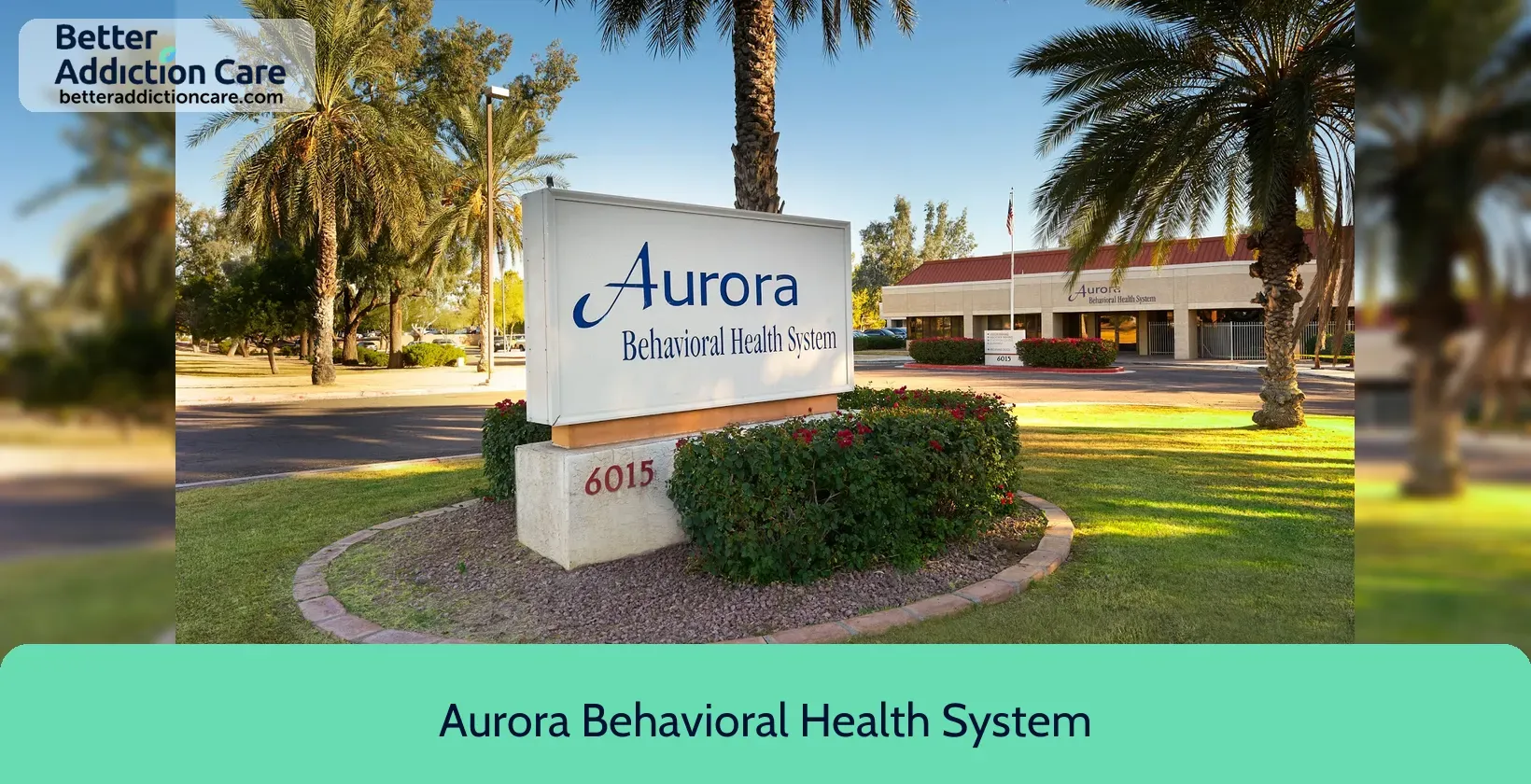
Aurora Behavioral Health System
Overview
Aurora Behavioral Health System is a substance abuse treatment center for people seeking treatment near Maricopa County. As part of their treatment modalities for recovery, Aurora Behavioral Health System provides cognitive behavioral therapy, integrated mental and substance use disorder treatment, and activity therapy during treatment. Aurora Behavioral Health System is located in Glendale, Arizona, accepting cash or self-payment for treatment.
Aurora Behavioral Health System at a Glance
Payment Options
- Cash or self-payment
- Medicaid
- Medicare
- State-financed health insurance plan other than Medicaid
- Private health insurance
Assessments
- Screening for tobacco use
- Comprehensive mental health assessment
- Comprehensive substance use assessment
- Screening for mental disorders
- Screening for substance use
Age Groups
- Seniors or older adults
- Adolescents
- Young adults
- Children/adolescents
- Adults
Ancillary Services
- Case management service
- Court-ordered outpatient treatment
- Integrated primary care services
- Psychosocial rehabilitation services
- Suicide prevention services
Highlights About Aurora Behavioral Health System
7.39/10
With an overall rating of 7.39/10, this facility has following balanced range of services. Alcohol Rehabilitation: 8.00/10, Drug Rehab and Detox: 7.85/10, Insurance and Payments: 6.00/10, Treatment Options: 7.70/10.-
Alcohol Rehabilitation 8.00
-
Drug Rehab and Detox 7.85
-
Treatment Options 7.70
-
Insurance and Payments 6.00
Accreditations
State department of health:

State Licenses, issued by government agencies, authorize rehabilitation organizations to legally operate within designated geographical areas. The specific licenses required for operation are typically determined by both the nature of the rehabilitation program provided by the facility and its physical location.
Hospital licensing authority:
The Hospital Licensing Authority is responsible for granting licenses to healthcare facilities, ensuring that they meet the standards and regulations set by the government. Accreditation is a process of evaluation and recognition by a third-party organization, confirming that the hospital meets specific quality and safety standards.
The Joint Commission:

The Joint Commission accreditation for addiction and behavioral health is a prestigious recognition signifying a facility's commitment to delivering high-quality care and safety for individuals dealing with substance abuse and mental health issues. It involves rigorous evaluations and assessments, ensuring patients receive evidence-based treatment and exceptional care. This accreditation demonstrates a facility's dedication to continuous improvement and ethical practices, building trust among patients and healthcare professionals seeking top-tier addiction and behavioral health services.
Treatment At Aurora Behavioral Health System
Treatment Conditions
- Mental health treatment
- Alcoholism
- Substance use treatment
- Co-occurring Disorders
Care Levels
- Hospital inpatient/24-hour hospital inpatient
- Partial Hospitalization Program
- Outpatient
- Outpatient day treatment or partial hospitalization
- Intensive outpatient treatment
Treatment Modalities
- Cognitive behavioral therapy
- Integrated Mental and Substance Use Disorder treatment
- Activity therapy
- Electroconvulsive therapy
- Telemedicine/telehealth therapy
Ancillary Services
Languages
- Sign language services for the deaf and hard of hearing
Additional Services
- Pharmacotherapies administered during treatment
- Mentoring/peer support
- Breathalyzer or blood alcohol testing
Special Programs
- Clients with co-occurring mental and substance use disorders
- Veterans
- Active duty military
- Members of military families
- Clients who have experienced trauma
Get Help Now
Common Questions About Aurora Behavioral Health System
Contact Information
Other Facilities in Glendale

7.58

7.58

6.65

6.68

6.59

7.14

6.92

7.17
DISCLAIMER: The facility name, logo and brand are the property and registered trademarks of La Frontera Arizona EMPACT SPC, and are being used for identification and informational purposes only. Use of these names, logos and brands shall not imply endorsement. BetterAddictionCare.com is not affiliated with or sponsored by La Frontera Arizona EMPACT SPC.