Drug Addiction: Definition, Types, Signs and Symptoms
What is Drug Addiction?
Drug addiction, also known as substance use disorder, involves an overwhelming drive to repeatedly use substances, even when the negative impact on health, relationships, and daily life becomes evident. This drug addiction condition alters the brain's reward system, leading individuals to continuously seek and use substances, even when it disrupts their health, relationships, and overall well-being. It encompasses a wide range of addictive substances, each causing serious physical, social, and emotional damage. According to the “2022 National Survey on Drug Use and Health Data” published by the Substance Abuse and Mental Health Services Administration, in 2022, 48.7 million people aged 12 or older (or 17.3%) had a substance use disorder (SUD) in the past year, including 29.5 million who had an alcohol use disorder (AUD), 27.2 million who had a drug use disorder (DUD), and 8.0 million people who had both an AUD and a DUD.
The types of drug addiction include both physical and psychological dependencies on substances such as alcohol, pain medications, and illegal drugs. Alcohol addiction affects millions through the use of beer, wine, and hard liquor. Alcohol addiction is the most common form of substance use disorder (SUD). According to the 2022 National Survey on Drug Use and Health (NSDUH), approximately 29.5 million people aged 12 or older in the U.S. suffer from alcohol use disorder (AUD), accounting for 10.2% of the population. Pain medication addiction is another growing concern, involving physically addictive prescription drugs like oxycodone, morphine, and fentanyl. Illegal drugs such as cocaine, heroin, and methamphetamine also cause severe physical and psychological dependency, leading to devastating health consequences.
The effects of drug addiction include physical risks to the body, emotional dysregulation, and negative effects on the social aspects of life. Physically, it leads to damage to organs, overdose, and other severe health issues. Socially, it disrupts relationships, causes isolation, and results in job loss. Emotionally, it creates anxiety, depression, and loss of control, further perpetuating the cycle of substance use. According to a study written by Eske, J. et. al. 2023 titled “What are the effects of drug misuse?” and published by Medical News Today, SUD also exacerbates the symptoms of other mental disorders, and early drug use is a strong risk factor for the later development of substance use disorders. Drug addiction is a risk factor for developing other mental illnesses. These effects demonstrate the broad-reaching consequences of drug addiction on every aspect of life.
What is the Definition of Drug Addiction?
The definition of drug addiction is a chronic relapsing disorder characterized by compulsive drug seeking, continued use despite harmful consequences, and long-lasting changes in the brain according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5, 2013) and highlighted by the National Institute of Drug Abuse.
Addiction is similar to other diseases, such as heart disease, type 2 diabetes and HIV/AIDS, in the way they disrupt the normal, healthy function of organs, leading to severe harm. These conditions (heart disease, type 2 diabetes, HIV/AIDS and drug addiction) are preventable and treatable, but without intervention, they will result in life-threatening outcomes.
What are the Types of Drug Addictions?

The types of drug addictions are wide ranging and include legal and illegal substances that are categorized into several classes, including stimulants, depressants, opioids, and hallucinogens.
The types of drug addictions are listed below:
-
Alcohol Use Disorder (Alcohol Addiction)
-
Lean Addiction
-
Crystal Meth Addiction
-
Heroin Addiction
-
PCP (Phencyclidine) Addiction
-
Hashish Addiction
-
Marijuana Addiction
-
Tramadol Addiction
-
Benzodiazepine Addiction
-
Fentanyl Addiction
-
Opioid Use Disorder
-
Tobacco Addiction
-
Xanax (Alprazolam) Addiction
-
Shatter Addiction
-
Pregabalin (Lyrica) Addiction
-
Ketamine Addiction
-
Antihistamine Addiction
-
Librium Addiction
-
Oxazepam Addiction
-
Methadone Addiction
-
Codeine Addiction
-
Cocaine Addiction
-
Polysubstance Addiction
-
Remeron Addiction
-
Morphine Addiction
-
Benadryl Addiction
-
Kratom Addiction
-
Methocarbamol (Robaxin) Addiction
-
Percocet Addiction
-
Suboxone Addiction
-
Ativan Addiction
-
Fentanyl Addiction
-
OxyContin Addiction
-
NyQuil Addiction
-
Ecstasy Addiction
-
Ritalin Addiction
-
Clobazam Addiction
-
Restoril Addiction
Alcohol Use Disorder (Alcohol Addiction)
Alcohol addiction, also known as alcohol use disorder, is a chronic condition where individuals (for example: professionals with high stress jobs, college students, adults coping with trauma) lose control over their drinking, continuing to consume alcohol despite its harmful effects on health, relationships, and daily responsibilities. The human body builds a tolerance, requiring individuals to consume up to 2 to 3 times the original amount of alcohol to achieve the desired effect, leading to physical dependence and compulsive use. The severity stems from alcohol's legal status, making it easily accessible and socially accepted, which contributes to the progression of addiction in many cases. 140,557 Americans die from the effects of alcohol in an average year showing the severity of the addiction according to The National Center for Drug Abuse Statistics survey titled “Alcohol Abuse Statistics” . Alcohol addiction is both physical and psychological in nature. Physically, the body becomes dependent on alcohol to function normally, while psychologically, the individual develops an emotional attachment to drinking as a coping mechanism.
Alcohol is classified as a depressant because it slows down the central nervous system, impairing cognitive functions, coordination, and decision-making. Alcohol addiction is severe, particularly when individuals experience withdrawal symptoms like tremors, anxiety, or seizures when attempting to quit. The general withdrawal timeline for alcohol ranges from 5 to 7 days, with symptoms peaking within 24 to 72 hours. In more severe cases, symptoms last longer, especially for heavy, long-term drinkers. Factors like the amount of alcohol consumed and the length of the addiction influence the withdrawal period. Alcohol is legal in the United States, contributing to its widespread use and potential for alcohol addiction.
Lean Addiction
Lean addiction is a substance use disorder dependent on a recreational drug mixture made from codeine cough syrup, soda, and sometimes candy, leading to a highly addictive substance use disorder. Lean is a downer due to the depressant effects of codeine, which slows down the central nervous system, leading to relaxation and euphoria. As an opioid-based drug, Lean addiction is considered severe because it often leads to compulsive use, and the risk of overdose is high. The addictive properties of codeine make this addiction both physical and psychological; users develop a physical need for the drug to avoid withdrawal, while also relying on its sedative effects to cope with stress or emotional issues.
The withdrawal timeline for Lean, influenced by its codeine content, lasts from 5 to 10 days. The symptoms of lean withdrawal peak within the first few days. Individuals with long-term or heavy use experience prolonged withdrawal symptoms. The drug is not legal in the U.S. for recreational use, as codeine is a controlled substance. Lean addiction poses significant health risks and legal consequences. According to Ware, O. et. al. 2024 “Codeine and promethazine: Exploratory study on “lean” or “sizzurp” using national survey data and an online forum”published by the National Library of Medicine, the NSDUH data indicated that lean use was most prevalent among teenagers and young adults (ages 13–21), accounting for 66% showing the concerning popularity of lean addiction among a particularly vulnerable demographic, highlighting the potential public health risks associated with its use in this age group.
Crystal Meth Addiction
Crystal Meth addiction,known as methamphetamine addiction, is a substance use disorder involving the compulsive use of a powerful stimulant that affects the central nervous system. Crystal Meth falls under the category of stimulant addictions due to its ability to increase dopamine levels, leading to heightened energy and euphoria. The severity of Crystal meth addiction is classified as severe, mainly because of its rapid and extreme impact on the brain's reward system, making it highly addictive after just a few uses. Methamphetamine elevates oxidative stress and disrupts receptor function over time, reducing their sensitivity to the drug. Individuals who are addicted to crystal meth include people with anxiety disorders, people who need to stay awake, or someone with chronic pain, who requires increasing amounts of methamphetamine to experience the same level of pleasure, leading to dependence and eventual addiction according to a 2017 study by Hedges et al., published in Neuropsychopharmacology.
Crystal Meth addiction is primarily psychological, as users develop an intense craving for the euphoric effects rather than relying on the drug for physical stability. The withdrawal timeline for Crystal Meth addiction ranges from one to two weeks, with symptoms like fatigue, depression, and intense drug cravings. Factors like the duration of use and the quantity consumed extend this period by up to a month. Methamphetamine is illegal in the U.S., except for specific medical conditions in rare cases. Methamphetamine addiction is a growing concern and needs comprehensive treatment options to address the dangers.
Heroin Addiction
Heroin addiction, a severe form of substance addiction, is the compulsive use of an opioid that produces intense euphoria and pain relief. Classified as a depressant addiction, heroin slows down the body's functions by binding to opioid receptors in the brain. The severity of heroin addiction is classified as severe because of its highly addictive nature, leading to rapid physical and psychological dependence. A 2011 article by Sándor Hosztafi in Acta Pharmaceutica Hungarica noted that heroin is a highly addictive, illegal substance and one of the most commonly misused opioids. It delivers a fast-acting "rush" or euphoric sensation, which is why individuals turn to heroin, especially as a cheaper alternative to prescription opioids.
Heroin addiction is both physical and psychological, as individuals experience withdrawal symptoms such as nausea and muscle pain, as well as intense cravings for the drug to achieve emotional relief. The withdrawal timeline for heroin starts within 6 to 12 hours after the last dose and lasts up to 10 days, with the most intense heroin addiction symptoms occurring within the first 48 to 72 hours. Factors such as frequency of use and dosage extend withdrawal by several days. Heroin is illegal in the U.S. for any purpose. Heroin addiction is life-threatening and requires multi-faceted treatment options due to its dangers.
PCP (Phencyclidine) Addiction
PCP addiction is the compulsive use of Phencyclidine, a dissociative drug that causes hallucinations, distorted perceptions, and detachment from reality. It is classified as a substance addiction and considered a depressant because it slows brain activity and alters sensory processing. The severity of PCP addiction is considered moderate to severe due to its strong psychological effects, which lead to dangerous behaviors and long-term mental health issues. A 2018 study by De Berardis et al., published in the International Journal of Molecular Sciences, explained that prolonged use of PCP amplifies its impact on the nervous system, worsening these impairments and potentially leading to suicidal thoughts. This is significant because PCP directly affects glutamate and NMDA activity.
PCP addiction is primarily psychological, as the intense effects on perception and mental state drive continued use. Withdrawal from PCP lasts from a few days to several weeks, with symptoms like confusion, depression, and cravings. Withdrawal duration depends on the frequency and amount of drug use. PCP is illegal in the U.S., and due to its potent effects, PCP (Phencyclidine) addiction poses significant risks for users. PCP addiction is risky and requires the necessary treatment to help support recovery.
Hashish Addiction
Hashish addiction is the chronic use of hashish, a concentrated form of cannabis resin, leading to a substance addiction that stimulates the brain's reward centers. Hashish is classified as a stimulant due to its psychoactive effects that elevate mood and perception. The severity of addiction is moderate because while hashish addiction develops over time, it is associated with long-term use.
Physical and psychological dependence occurs with hashish addiction, with symptoms such as cravings and mood disturbances. It not only alters the brain’s chemistry but also becomes a way to cope with life’s challenges, making it difficult to break free from the cycle of dependence. Withdrawal symptoms usually appear within 1to 2 days of stopping use and lasts for up to two weeks, with changes in intensity based on the length and quantity of use. Hashish is illegal in most U.S. states, and as such, Hashish addiction remains a growing concern in regions where cannabis products are widely available.
Marijuana Addiction
Marijuana addiction, also called cannabis use disorder, is a substance addiction which involves the chronic use of cannabis. Marijuana addiciton is classified as a mild stimulant addiction, with effects such as euphoria and altered perception. The severity of marijuana addiction is mild to moderate because, although users develop a dependence, it takes frequent, long-term use to lead to addiction. A 2015 study by Hasin et al., published in JAMA Psychiatry, found that 30% of cannabis users develop marijuana use disorder. The likelihood of addiction or dependence increases with higher cannabis consumption.
Cannabis use disorder is primarily psychological, as users crave the calming and euphoric effects rather than developing severe physical withdrawal symptoms. Withdrawal symptoms begin within 24 to 48 hours and last about two weeks, though stress and anxiety levels extend this period. Marijuana remains illegal at the federal level in the U.S., although many states have legalized it for medical and recreational use, contributing to the rise in marijuana addiction cases.
Tramadol Addiction
Tramadol addiction occurs when individuals develop a dependence to this prescription painkiller, a synthetic opioid used to treat moderate to severe pain. Tramadol addiction is classified as a substance addiction under the opioid category because it binds to opioid receptors in the brain to provide pain relief. The severity of tramadol addiction is considered moderate to severe, as users quickly build a tolerance, requiring higher doses for the same effect. According to the U.S. Department of Health and Human Services' 2022 report on “Opioid Overdose Prevention,” approximately 2.1 million people in the U.S. struggle with opioid use, including tramadol addiction. The severity of the problem is emphasized by the sharp increase in opioid overdose deaths, which doubled from over 21,000 in 2010 to 42,000 in 2016.
Tramadol addiction is both physical and psychological because the body becomes dependent on tramadol to function normally while the brain is altered and relied upon to deal with life’s struggles, making it tough to break free from addiction. Tramadol addiction has withdrawal symptoms like sweating, anxiety, and muscle aches beginning within 12 hours of the last dose and lasting up to two weeks. Long-term use extends withdrawal symptoms. Tramadol is legal in the U.S. with a prescription, but misuse of the drug has led to increased instances of tramadol addiction.
Benzodiazepine Addiction
Benzodiazepine addiction is the compulsive use of sedative medications like Xanax or Valium, commonly prescribed for anxiety and sleep disorders. It is a substance addiction and classified as a depressant addiction because it slows down brain activity to create a calming effect. The severity of benzodiazepine addiction is severe due to the high risk of dependency, especially for those who use benzodiazepines for more than 3 to 6 months.
Benzodiazepine addiction is a physical addiction as withdrawal symptoms like seizures, insomnia, and anxiety make quitting difficult. Withdrawal starts within 1 to 4 days and lasts several weeks or longer, depending on the dosage and duration of use. Benzodiazepines are legal with a prescription in the U.S., but their addictive potential has led to a high rate of misuse and addiction. A study by Votaw et al., published in the July 2019 issue of Drug and Alcohol Dependence, found that benzodiazepine addiction is widespread, with benzodiazepines and other tranquilizers being the third most commonly misused or prescribed drugs in the U.S., affecting about 2.2% of the population in 2017. Benzodiazepine addiction is life-threatening if it gets out of control and requires medical treatment.
Fentanyl Addiction
Fentanyl addiction involves the chronic abuse of fentanyl, a powerful synthetic opioid that is 50-100 times more potent than morphine. Classified as a substance addiction, it falls under the depressant category due to its strong impact on slowing the central nervous system. The severity of fentanyl addiction is extremely high, as even small amounts will lead to overdose and death, making it one of the most dangerous addictions.
Addiction to fentanyl is both physical and psychological because the substance alters brain chemistry and helps cope with daily struggles, it also deepens the dependency, making it harder to quit., The withdrawal symptoms of fentanyl begin within a few hours and last 1 to 2 weeks, depending on the level of dependency. Because fentanyl is mixed with other substances, withdrawal is unpredictable and more intense. Fentanyl is legal in the U.S. for medical use, but its illicit production and distribution have caused a spike in fentanyl addiction cases. According to the 2022 National Survey on Drug Use and Health highlights from the Substance Abuse and Mental Health Services Administration (SAMHSA), fentanyl addiction is widespread, with 991,000 individuals aged 12 or older (0.4% of the population) having either misused prescription fentanyl or used illegally made fentanyl (IMF) in the past year. Fentanyl addiction is a life-threatening condition that necessitates robust treatment options.
Opioid Use Disorder
Opioid use disorder (OUD), or opioid addiction, is a substance addiction that encompasses the misuse of both prescription and illegal opioids, such as heroin, fentanyl, and prescription painkillers. OUD is classified as a depressant addiction, as opioids slow down the body's systems and create feelings of relaxation and euphoria. The severity of opioid use disorder is severe due to the high risk of dependence and the potential for overdose. According to the 2021 National Survey on Drug Use and Health (NSDUH) conducted by the Substance Abuse and Mental Health Services Administration (SAMHSA), an estimated 2.5 million people aged 18 years or older in the United States had opioid use disorder in the past year. This represents about 1% of the adult population in the country.
OUD is physical and psychological because it is associated with chronic pain and changes brain chemistry while also offering a temporary escape from life’s hardships, making it even harder to overcome the addiction. Opioid withdrawal symptoms such as nausea, vomiting, and intense cravings beginning within 6 to 12 hours of the last dose and lasting up to two weeks. The withdrawal timeline is extended depending on the type of opioid and the frequency of use. While some opioids are legal with a prescription in the U.S., opioid use disorder remains a widespread public health issue compounded by the high potential for addiction and the extreme lengths individuals will go to in order to obtain the substance. Opioid Use Disorder is hazardous and must be tackled with a full spectrum of treatment methods.
Tobacco Addiction
Tobacco addiction is the regular use of nicotine, a stimulant found in cigarettes and other tobacco products. Classified as a substance addiction, tobacco stimulates the release of dopamine in the brain, creating feelings of pleasure and relaxation. The severity of tobacco addiction is moderate, but its long-term health impacts make it dangerous, especially due to the risk of cancer and respiratory diseases.
The effects of tobacco addiction are both physical and psychological, as users become dependent on nicotine to function normally. Withdrawal symptoms like irritability, anxiety, and difficulty concentrating begin within hours of the last cigarette and will last several weeks. Tobacco products, including cigarettes, are legal in the U.S., contributing to the widespread prevalence of tobacco addiction. According to Cornelius ME et.al. 2021 “Tobacco Product Use Among Adults - United States” published by the Morbidity Mortality Weekly Report, approximately 46 million U.S. adults (18.7%) reported using some form of tobacco, including cigarettes (11.5%), e-cigarettes (4.5%), cigars (3.5%), smokeless tobacco (2.1%), and pipes, including hookah (0.9%). Among tobacco users (male and female), 77.5% reported using combustible products like cigarettes, cigars, or pipes, while 18.1% reported using two or more types of tobacco products. Tobacco addiction is dangerous and needs comprehensive education programs for young minds.
Xanax (Alprazolam) Addiction
Xanax addiction occurs when individuals become dependent on alprazolam, a benzodiazepine commonly prescribed to treat anxiety and panic disorders. Classified as a depressant addiction, Xanax slows brain activity, producing a calming effect. The severity of Xanax addiction is severe, as users quickly develop a tolerance, leading to higher doses and risk of overdose. According to a 2018 study by Ait-Daoud et al., titled "A Review of Alprazolam Use, Misuse, and Withdrawal," Xanax is highly addictive due to its rapid processing and short half-life, meaning it leaves the body quickly. This leads to a higher likelihood of misuse, as its effects wear off more rapidly.
Alprazolam addiction is both physical and psychological because it is used as a way to cope with stress, anxiety, or emotional pain. Xanax also has withdrawal symptoms such as seizures, tremors, and intense anxiety starting within 1 to 4 days and lasting up to several weeks. Factors like long-term use and high doses prolong withdrawal. Xanax is legal in the U.S. with a prescription, but it's addictive potential makes Xanax addiction a significant issue among users. Alprazolam addiction is a severe problem requiring a well-rounded approach to treatment.
Shatter Addiction
Shatter addiction occurs when individuals become dependent on a potent cannabis concentrate. Classified as a stimulant addiction, shatter induces strong psychoactive effects that heighten sensory perception and euphoria. The severity of shatter addiction is moderate to severe, as its potency increases the likelihood of developing dependence and mental health issues like anxiety or paranoia. Shatter is notable for its high THC concentration, around 80%, making it far more potent and dangerous compared to dried cannabis, which has an average THC content of about 15%, according to a 2023 update from the Canadian Government. The significantly higher THC levels in shatter increase the risk of severe psychological effects, including anxiety, paranoia, and addiction, as noted by the Alcohol and Drug Foundation.
Shatter addiction is primarily psychological because it involves cravings, compulsive drug-seeking behavior, and an inability to stop using despite knowing the harmful consequences. Shatter withdrawal symptoms such as irritability, insomnia, and mood swings occurring within a few days of cessation and lasting up to two weeks. The highly concentrated THC content makes shatter use illegal in many states, contributing to the growing concern over its misuse. Shatter addiction is dangerous and needs a complete, well-rounded treatment approach.
Pregabalin (Lyrica) Addiction
Pregabalin addiction involves dependency on Lyrica, a prescription medication used to treat nerve pain and seizures. Classified as a depressant addiction, Pregabalin slows brain activity, reducing pain signals but leading to a high potential for misuse. The severity of Pregabalin addiction ranges from moderate to severe, as users develop tolerance quickly and require higher doses for the same effect. Pregabalin addiction is common, with a 1.6% gabapentinoid abuse prevalence observed in the general population, as reported by the researchers of the 2017 study “Abuse and Misuse of Pregabalin and Gabapentin,” published in the Drugs journal. Among opioid abusers, gabapentinoid abuse rates range from 3% to 68%. An international adverse event database identified 11,940 cases of gabapentinoid abuse between 2004 and 2015, with over 75% of these reports occurring since 2012.
Pregabalin (lyrica) addiction is both physical and psychological because while individuals develop a physical dependence it also alters their brain chemistry making them believe they need it and making it difficult to quit. Lyrica withdrawal symptoms like anxiety, dizziness, and insomnia starting within 24 to 48 hours of the last dose and last up to a week or more. While Pregabalin is legal with a prescription in the U.S., its misuse has led to increased rates of addiction and dependence. Pregabalin (lyrica) addiction is harmful, and addressing it requires full-scale treatment solutions.
Ketamine Addiction
Ketamine addiction occurs when individuals misuse ketamine, a dissociative anesthetic known for its hallucinogenic effects. Classified as a depressant addiction, ketamine disrupts brain activity, leading to altered perceptions and dissociation. The severity of ketamine addiction is moderate to severe, as frequent use leads to tolerance, dependence, and long-term cognitive impairment. A 2021 study by Palamar et al., published in the American Journal of Public Health, revealed that less than 1% of people in the U.S. use ketamine. However, recreational use of ketamine has been on the rise in recent years, with a notable increase starting in 2019 when the FDA approved the use of Ketamine nasal spray for unmanageable depression.
Special K addiction is both physical and psychological due to its effects on the brain and body. While the primary dependence is psychological, leading to cravings, confusion, and agitation within 24 hours of the last dose, physical symptoms also develop, with withdrawal symptoms such as confusion, agitation, and cravings starting within 24 hours of the last dose and lasting several days. Although ketamine is legal for medical use in the U.S., its recreational use is illegal and has been associated with significant health risks. Ketamine addiction is risky and calls for a broad and complete treatment strategy.
Antihistamine Addiction
Antihistamine addiction develops when individuals misuse medications used to treat allergies, such as diphenhydramine (Benadryl), for their sedative effects. Classified as a depressant addiction, antihistamines slow down bodily functions and induces relaxation or drowsiness when taken in high doses. The severity of antihistamine addiction is mild to moderate but becomes more severe with long-term misuse. According to the Centers for Disease Control and Prevention (CDC)’s October 2022 Morbidity and Mortality Weekly Report (MMWR), antihistamine addiction is prevalent. Of the 92,033 overdose fatalities recorded between 2019 and 2020, 13,574 (14.7%) tested positive for antihistamines, while 3,345 (3.6%) were directly linked to antihistamine use.
Addiction to antihistamines is both physical and psychological, with withdrawal symptoms like anxiety, insomnia, and irritability occurring within 24 to 48 hours of cessation and lasting up to a week, users also depend on its sedative effects to manage stress or sleep. While antihistamines are legal and available over-the-counter, their potential for misuse raises concerns about dependency. Antihistamine addiction requires in-depth, multi-faceted treatment options.
Librium Addiction
Librium addiction refers to the misuse of chlordiazepoxide, a benzodiazepine commonly prescribed for anxiety and alcohol withdrawal. Classified as a depressant addiction, Librium calms brain activity, making it highly addictive with long-term use. The severity of Librium addiction is severe due to the risk of developing both tolerance and physical dependence, leading to higher doses and withdrawal complications. According to a paper by Blanco et al., published in the October 2018 issue of The Journal of Clinical Psychiatry, approximately 2.1% of American adults have abused benzodiazepines at some point in their lives. Among those prescribed benzodiazepines, the rate of abuse increases significantly to 17.1%.
Librium addiction is both physical and psychological due to the body's dependence and withdrawal symptoms, and psychological, as users become emotionally reliant on it to manage anxiety and stress. Librium, also known as chlordiazepoxide, has withdrawal symptoms such as seizures, tremors, and intense anxiety beginning within 1 to 4 days and lasting several weeks. Librium is legal in the U.S. with a prescription, but its high potential for addiction makes careful medical supervision essential during use. Librium addiction is difficult to recover from and requires a tailored treatment approach.
Oxazepam Addiction
Oxazepam addiction occurs when individuals misuse the benzodiazepine, prescribed for alcohol withdrawal, anxiety or insomnia. As tolerance builds, higher doses are required to achieve the same calming effects, leading to compulsive use and physical dependence. The severity of oxazepam addiction is tied to its ability to slow brain activity, which results in both cognitive and emotional detachment. Oxazepam, like other benzodiazepines, works by calming the central nervous system, enhancing the effects of gamma-aminobutyric acid (GABA), a natural substance in the body, according to a Medscape patient handout on "oxazepam (Rx)," revised in February 2023. While effective for certain conditions, prolonged use leads to dependence. Medsafe’s New Zealand Data Sheet, updated in February 2022, notes that extended use of oxazepam results in a barbiturate-alcohol type of dependence, increasing the risk of benzodiazepine addiction.
Oxazepam addiction is both physical and psychological. Physically, the body relies on the drug to function, with withdrawal symptoms like tremors, seizures, and intense anxiety. Psychologically, individuals become emotionally dependent on the drug to manage stress or anxiety. Withdrawal lasts 1 to 2 weeks, with symptoms starting 24 to 48 hours after the last dose. Oxazepam is legal with a prescription but carries a high risk of misuse. Addressing oxazepam addiction is important and involves comprehensive care and treatment.
Methadone Addiction
Methadone addiction is when individuals misuse this synthetic opioid, prescribed to treat opioid addiction. Over time, tolerance increases, leading to higher doses and physical dependence. Methadone addiction is considered severe as it is linked to powerful, long-lasting effects, making it challenging to stop once dependence develops. Methadone addiction is a significant issue, with around 261,000 Americans aged 12 and older (0.1%) reporting methadone misuse in 2017, according to the 2017 National Survey on Drug Use and Health by the Substance Abuse and Mental Health Services Administration. Additionally in 2023, the National Institute on Drug Abuse reported that overdose deaths involving prescription opioids like methadone rose from 3,442 in 1999 to 17,029 in 2017.
Meth addiction involves both physical and psychological dependence. Physically, the body needs methadone to avoid withdrawal symptoms like nausea, muscle pain, and cravings. Psychologically, individuals rely on methadone for emotional stability and pain relief. Withdrawal begins 24 to 36 hours after the last dose and lasts for several weeks. Methadone is legally prescribed but requires careful monitoring to avoid addiction. Methadone addiction poses serious risks and needs an all-encompassing treatment plan.
Codeine Addiction
Codeine addiction refers to an individual's misuse of the opioid, commonly used in pain relief medications and cough syrups. Over time, the body develops tolerance, requiring higher doses, which leads to physical dependence and compulsive use. The widespread availability of codeine in over-the-counter products makes misuse more accessible, making codeine addiction much more severe. According to the publication titled “United States Dispensing Rate Maps,” last reviewed in December 2023 by the Centers for Disease Control and Prevention (CDC), a total of 131,778,501 opioid prescriptions were issued in 2022. Codeine remains one of the most commonly prescribed opioids in the U.S.
Codeine addiction is both physical and psychological. Physically, withdrawal symptoms like muscle pain, sweating, and irritability occur when use stops. Psychologically, individuals become emotionally reliant on codeine for managing stress or discomfort. Withdrawal begins 12 to 24 hours after the last dose and lasts up to a week. Codeine is legal with a prescription but has a high potential for abuse. Overcoming codeine addiction is difficult and requires an extensive approach to treatment.
Cocaine Addiction
Cocaine addiction is a substance use disorder marked by the compulsive use of the stimulant, which increases dopamine levels and produces intense euphoria. Over time, individuals require more frequent or larger doses, leading to both physical and psychological dependence. Cocaine's fast-acting nature makes its addiction particularly severe, with dire consequences for brain function. According to a study by Schwartz et al., published in the September 2022 issue of Substance Abuse and Rehabilitation, approximately 2.2 million people in the United States regularly use cocaine, in contrast to 600,000 methamphetamine users. Of those, 1.5 million meet the criteria for cocaine use disorder (CUD) as outlined in the Diagnostic and Statistical Manual for Mental Disorders (DSM-5).
Cocaine addiction is primarily psychological, with strong physical effects. Although physical withdrawal symptoms of cocaine addiction are less severe than with opioids, intense cravings, depression, and anxiety occur when use stops. Withdrawal begins within hours and lasts for days to weeks. Cocaine is illegal, making its use both risky and highly addictive. Cocaine addiction is a serious issue that calls for thorough treatment strategies.
Polysubstance Addiction
Polysubstance addiction occurs when individuals become addicted to multiple substances at once, combining alcohol, opioids, and stimulants. This type of substance use addiction is dangerous due to the compounded effects on the body and mind, increasing the risk of overdose and making treatment more complex. Poly substance addiction is severe however the height of the severity stems from the interactions between different drugs, which leads to more extreme dependence. A 2014 report by the Substance Abuse and Mental Health Services Administration (SAMHSA), titled “Benzodiazepines in Combination with Opioid Pain Relievers or Alcohol: Greater Risk of More Serious ED Visit Outcomes,” revealed that nearly a million emergency department visits related to benzodiazepines or their combination with alcohol or opioids occurred between 2005 and 2011. The report noted a 24-55% increase in the risk of severe outcomes when opioids or alcohol were combined with benzodiazepines compared to using BZD alone.
Polysubstance addiction is both physical and psychological. The body becomes reliant on multiple substances, resulting in severe withdrawal symptoms like nausea, tremors, and mood swings. Psychologically, individuals develop compulsive drug-seeking behaviors to manage stress or trauma. Withdrawal timelines vary depending on the substances involved, but symptoms of polysubstance addiction start within hours to days after the last use and are severe and require medical treatment. Polysubstance addiction is serious and requires immediate treatment.
Remeron Addiction
Remeron (mirtazapine) addiction occurs when individuals develop a dependency on this antidepressant, commonly prescribed to treat depression and anxiety. As a substance addiction, Remeron impacts neurotransmitters in the brain, altering mood and emotional balance. The severity of Remeron addiction is mild to moderate, as it does not create the same compulsive use patterns as more addictive substances like opioids or benzodiazepines. However, misuse or long-term use leads to dependency.
Remeron addiction is primarily psychological, as the body doesn’t develop a significant physical dependence, but users become emotionally reliant on its calming effects. According to a 2023 article titled, “Remeron Addiction: Signs and Symptoms of Mirtazapine Abuse” from Addiction Resource, mirtazapine causes psychological effects such as hallucinations, disorientation, and impaired memory function. These effects heighten the risk of developing mental health issues or exacerbate existing ones. Withdrawal symptoms begin within 1 to 3 days of cessation, including insomnia, nausea, and irritability, and lasts up to a week. Remeron is legal in the U.S. with a prescription. Remeron addiction is feasible at home but the root of the addiction such as mental health disorders need therapeutic interventions.
Morphine Addiction
Morphine addiction is a substance addiction involving the misuse of this powerful opioid, prescribed for severe pain management. Classified as a depressant, morphine slows down the central nervous system, which leads to physical dependence after prolonged use. The severity of morphine addiction is high due to its potent effects and the rapid development of tolerance, requiring increased doses to achieve pain relief. Morphine addiction is widespread, affecting over 16 million people worldwide and more than 2.1 million in the United States. This contributes to over 120,000 opioid-related deaths annually, according to a July 2023 update from StatPearls Publishing titled “Opioid Use Disorder.”
Morphine addiction is both physical and psychological. The body becomes dependent on the drug, leading to withdrawal symptoms such as nausea, sweating, and severe cravings when use is stopped. Withdrawal begins within 6 to 12 hours of the last dose and lasts 1 to 2 weeks. Morphine is legal in the U.S. with a prescription, but its high potential for addiction makes it a controlled substance. Morphine addiction is dangerous and necessitates medical treatment.
Benadryl Addiction
Benadryl (diphenhydramine) addiction occurs when individuals misuse this over-the-counter antihistamine for its sedative effects. As a substance addiction, Benadryl affects the central nervous system, causing drowsiness and relaxation. The severity of Benadryl addiction is usually mild to moderate, as it is less likely to result in compulsive use compared to controlled substances, but long-term misuse leads to dependency. Benadryl addiction is relatively rare, but misuse and dependence have been documented. A 2021 study by Nemanich A. et al., titled “Increased Rates of Diphenhydramine Overdose, Abuse, and Misuse in the United States, 2005-2016,” reported a 63% rise in intentional diphenhydramine exposures, including Benadryl, over 12 years.
Benadryl addiction is both physical and psychological. Physically, the body becomes reliant on its sedative properties, while psychologically, users rely on it for relief from anxiety or insomnia. Withdrawal symptoms of Benadryl addiction, such as irritability and sleep disturbances occur within 24-48 hours and last up to a week. Benadryl is legal and widely available over the counter in the U.S., but its misuse does lead to addiction. Benadryl addiction is manageable without treatment, however with any addiction, the psychological aspect requires some form of therapy.
Kratom Addiction
Kratom addiction develops when individuals misuse this herbal substance, commonly used for pain relief or its stimulant effects. Classified as a substance addiction, kratom impacts opioid receptors in the brain, leading to dependency similar to opioids. The severity of kratom addiction varies from moderate to severe, depending on the frequency and dosage of use, with higher doses causing stronger opioid-like effects. Kratom addiction is notably widespread. According to the 2021 National Survey on Drug Use and Health, published by the Substance Abuse and Mental Health Services Administration in December 2022, approximately 1.7 million people, or 0.6% of individuals aged 12 and older, reported using kratom in the past year.
Kratom addiction is both physical and psychological. Physical dependence develops as the body adjusts to the substance, leading to withdrawal symptoms like muscle aches, irritability, and nausea. Psychological dependence occurs when users rely on kratom for mood enhancement or pain relief. Withdrawal symptoms of Kratom addiction start within 12-24 hours after cessation and lasts 3-7 days. Kratom is currently legal in the U.S., though it remains unregulated. While recovering from Kratom addiction is possible to manage on your own, but treatment is necessary if the addiction has become too severe.
Methocarbamol (Robaxin) Addiction
Methocarbamol addiction develops when individuals misuse this muscle relaxant, commonly prescribed to alleviate pain from muscle spasms. As a substance addiction, methocarbamol impacts the central nervous system, leading to physical relaxation and drowsiness. The severity of methocarbamol addiction is mild to moderate, as it doesn’t produce euphoria but is still misused, particularly in combination with other drugs. In 2011, approximately 53,000 emergency department visits were due to the misuse or abuse of muscle relaxants, with 18% involving alcohol consumption, according to a 2014 study by Witenko C. et al., titled "Considerations for the Appropriate Use of Skeletal Muscle Relaxants for the Management of Acute Low Back Pain."
Methocarbamol addiction is primarily psychological, as individuals develop an emotional reliance on its calming effects. Physically, the drug does not cause strong withdrawal symptoms, but discontinuation after misuse leads to mild discomfort, such as headaches or fatigue. The withdrawal timeline is short, lasting a few days. Methocarbamol is legal in the U.S. with a prescription, making it easily accessible for those who misuse it. Due to its effects on the central nervous system, Methocarbamol (Robaxin) addiction still poses risks, especially when misused.
Percocet Addiction
Percocet addiction occurs when individuals misuse this combination of oxycodone and acetaminophen, a prescription opioid for pain relief. Classified as a substance addiction, Percocet is highly addictive due to its opioid component, which produces pain relief and euphoria. The severity of Percocet addiction is high, as tolerance develops quickly, leading to the need for larger doses and an increased risk of overdose. According to the article titled, “Key Substance Use and Mental Health Indicators in the United States: Results from the 2022 National Survey on Drug Use and Health,” published by the Substance Abuse and Mental Health Services Administration in November 2023, Percocet addiction affected 2.5 million individuals and accounted for 30.7% of prescription painkiller abuse in 2022.
Percocet addiction is both physical and psychological. The body becomes dependent on the opioid to avoid withdrawal symptoms like nausea, sweating, and intense cravings. Psychological dependence manifests as an emotional reliance on the drug to cope with pain or stress. Withdrawal symptoms of Percocet addiction begin within 6-12 hours after the last dose and lasts 1-2 weeks, with symptoms peaking in the first few days. Percocet is legal in the U.S. with a prescription, but it's opioid component makes Percocet addiction a serious public health issue.
Suboxone Addiction
Suboxone addiction occurs when individuals misuse this medication, which is prescribed to treat opioid dependence. Suboxone contains buprenorphine and naloxone, making it a partial opioid agonist that reduces withdrawal symptoms without producing the same high as stronger opioids. Suboxone is classified as a substance addiction because, despite its use in treating opioid addiction, it is still misused in high doses. The severity of Suboxone addiction tends to be moderate because of its design to prevent misuse, though dependence develops with prolonged use. According to the National Institute on Drug Abuse, approximately 16.1 million people, or 5.8% of the U.S. population over the age of 12, misused prescription psychotherapeutic drugs in 2020. Due to this, the Substance Abuse and Mental Health Services Administration (SAMHSA) advises that individuals seeking to use Suboxone should do so under the care of a doctor experienced in treating Suboxone use disorder.
Suboxone addiction is primarily psychological, though some physical dependence occurs, especially if the drug is misused. Withdrawal symptoms start within 1 to 3 days after discontinuation and lasts up to a week, though cravings and psychological symptoms persist longer. Suboxone is legal in the U.S. with a prescription, but its misuse contributes to the rising concern over opioid addiction treatments. Despite its role in recovery, Suboxone addiction still occurs if not carefully monitored.
Ativan Addiction
Ativan addiction occurs when individuals become dependent on this benzodiazepine, commonly prescribed for anxiety or sleep disorders. Classified as a substance addiction, Ativan works by slowing brain activity, producing a calming effect. The severity of Ativan addiction is severe, as users develop tolerance quickly, leading to higher doses and an increased risk of overdose. Ativan (Lorazepam) is one of the five most frequently prescribed benzodiazepines and is commonly found in illicit drug markets, according to a 2023 article from the Drug Enforcement Administration. The 2020 National Survey on Drug Use and Health by the Substance Abuse and Mental Health Services Administration estimated that 4.8 million individuals aged 12 and older misused prescription benzodiazepines, including lorazepam, in 2020.
Ativan addiction is both physical and psychological. Physically, the body becomes dependent on the drug to function normally, and withdrawal symptoms such as seizures, tremors, and anxiety occur when use is stopped. Psychologically, individuals rely on Ativan to manage stress or anxiety, deepening their dependence. Withdrawal symptoms of Ativan addiction begins within 1-4 days after the last dose and lasts several weeks. Ativan is legal in the U.S. with a prescription, but it's addictive potential makes Ativan addiction a serious concern.
OxyContin Addiction
OxyContin addiction occurs when individuals misuse this extended-release form of oxycodone, a powerful opioid prescribed for chronic pain relief. As a substance addiction, OxyContin binds to opioid receptors in the brain, producing euphoria and pain relief. The severity of OxyContin addiction is severe due to the drug’s high potential for tolerance and dependence, requiring larger doses over time to achieve the same effect. According to Carise, D. et. al. 2009 “Prescription OxyContin Abuse Among Patients Entering Addiction Treatment”, around 5% of individuals admitted to 157 addiction treatment programs reported prior use of OxyContin. Of those, 4.5% had used the drug regularly for at least a year, and 2% had used it within the 30 days before admission. Additionally, 78% of those who reported using OxyContin said it hadn’t been prescribed for any medical reason, 86% used it to "get high," and 78% had previously received treatment for a substance use disorder.
Addiction to OxyContin is physical and psychological. Physically, users develop a dependence on the drug, experiencing withdrawal symptoms like nausea, muscle pain, and intense cravings when attempting to quit. Psychologically, individuals rely on OxyContin to manage pain or stress. Withdrawal symptoms usually begin within 6 to 12 hours after the last dose and lasts 1 to 2 weeks. OxyContin is legal in the U.S. with a prescription, but its high risk of misuse makes OxyContin addiction a critical issue.
NyQuil Addiction
NyQuil addiction occurs when individuals misuse this over-the-counter cold and flu medication, for its sedative or psychoactive effects. As a substance addiction, NyQuil contains ingredients like dextromethorphan and doxylamine, which cause drowsiness and, at high doses, dissociative effects. The severity of NyQuil addiction is mild to moderate, but misuse in large quantities or for prolonged periods leads to dependency. In a 2021 paper by S.H.F. Lam et al., published in the Journal of the American College of Emergency Physicians Open, it was reported that around 3.1 million individuals in the U.S. aged 12 to 25 had used over-the-counter cough and cold medicine to achieve a "high."
NyQuil addiction is primarily psychological, as users become reliant on its calming effects to cope with insomnia or stress. However, long-term misuse leads to physical symptoms such as dizziness and digestive issues upon cessation. Withdrawal symptoms are mild, with a timeline of a few days to a week. NyQuil is legal and available over the counter in the U.S., but its potential for misuse contributes to NyQuil addiction in some cases.
Ecstasy Addiction
Ecstasy addiction occurs when individuals develop a dependence on MDMA, a synthetic stimulant and hallucinogen used recreationally for its euphoric effects. As a substance addiction, ecstasy stimulates the release of serotonin and dopamine in the brain, leading to enhanced mood and sensory perception. The severity of ecstasy addiction ranges from moderate to severe, as frequent use causes significant psychological dependence and long-term cognitive damage. In 2021, 0.8% of individuals above the age of 12 (or over 2.2 million) reported using MDMA (Ecstasy) within the previous 12 months, according to a 2017 publication from the National Institute on Drug Abuse titled, “What is the scope of MDMA use in the United States?”.
Ecstasy addiction is primarily psychological, with users craving the euphoric and social effects of the drug. Withdrawal symptoms like depression, fatigue, and anxiety begin within 24 to 48 hours and lasts up to a week. Ecstasy is illegal in the U.S., which further exacerbates the dangers associated with its misuse. Ecstasy addiction severely impacts both mental health and neurological functioning if not addressed.
Ritalin Addiction
Ritalin addiction occurs when individuals misuse the stimulant, prescribed for attention-deficit hyperactivity disorder (ADHD). As a substance addiction, Ritalin affects dopamine levels in the brain, enhancing focus and energy. The severity of Ritalin addiction is moderate to severe, as users quickly develop a tolerance, leading to larger doses for the same effects and a higher risk of dependency. In 2016, close to 2 million young Americans aged 12 and older reported misusing prescription stimulants such as Ritalin. Additionally, the National Institute on Drug Abuse (NIDA)’s Monitoring the Future survey revealed that over 50% of students who used Ritalin and other prescription stimulants non-medically obtained them from family members or friends.
Ritalin addiction is both physical and psychological. Physically, users experience withdrawal symptoms such as fatigue, depression, and cravings when the drug is stopped. Psychologically, individuals become reliant on Ritalin to improve focus or manage daily tasks. Withdrawal symptoms start within a few hours to a day after the last dose and lasts several days to a week. Ritalin is legal in the U.S. with a prescription, but its potential for misuse makes Ritalin addiction a growing concern needing holistic treatment methods for recovery.
Clobazam Addiction
Clobazam addiction develops when individuals misuse this benzodiazepine, often prescribed for seizures and anxiety. Classified as a substance addiction, clobazam enhances the calming effects of gamma-aminobutyric acid (GABA) in the brain, leading to relaxation. The severity of clobazam addiction is moderate to severe, as tolerance builds quickly, and users require higher doses over time, increasing the risk of dependency.
Clobazam addiction is both physical and psychological. Physically, the body becomes dependent according to a study by Tolbert et al., published in the April 2012 issue of Neurology, stating that the most frequently reported adverse effects following the abrupt discontinuation of clobazam included tremors, anxiety, insomnia, and headaches. Psychologically, users rely on clobazam to manage stress or anxiety. Withdrawal begins within 1 to 4 days of stopping use and lasts several weeks. Clobazam is legal in the U.S. with a prescription, but its addictive potential makes clobazam addiction a serious risk for long-term users needing comprehensive treatment options.
Restoril Addiction
Restoril addiction occurs when individuals misuse this benzodiazepine, commonly prescribed for insomnia. As a substance addiction, Restoril works by slowing brain activity, inducing sleep and reducing anxiety. The severity of Restoril addiction is severe, as users develop a tolerance quickly, requiring higher doses to achieve the same sedative effects. According to the ClinCalc DrugStats Database report on “Temazepam: Drug Usage Statistics, United States, 2013 – 2020,” benzodiazepine abuse frequently arises from accessing these drugs through medical prescriptions. In 2020, around 551,311 patients in the United States were prescribed Restoril, accounting for approximately 2,143,561 prescriptions.
Restoril addiction is both physical and psychological. Physically, dependence on the drug results in withdrawal symptoms like insomnia, anxiety, and seizures when use is stopped. Psychologically, individuals become reliant on Restoril to manage sleep disorders, deepening their emotional dependence. Withdrawal begins within 1 to 3 days after the last dose and lasts several weeks. Restoril is legal in the U.S. with a prescription, but its addictive potential makes Restoril addiction a serious concern for long-term users.
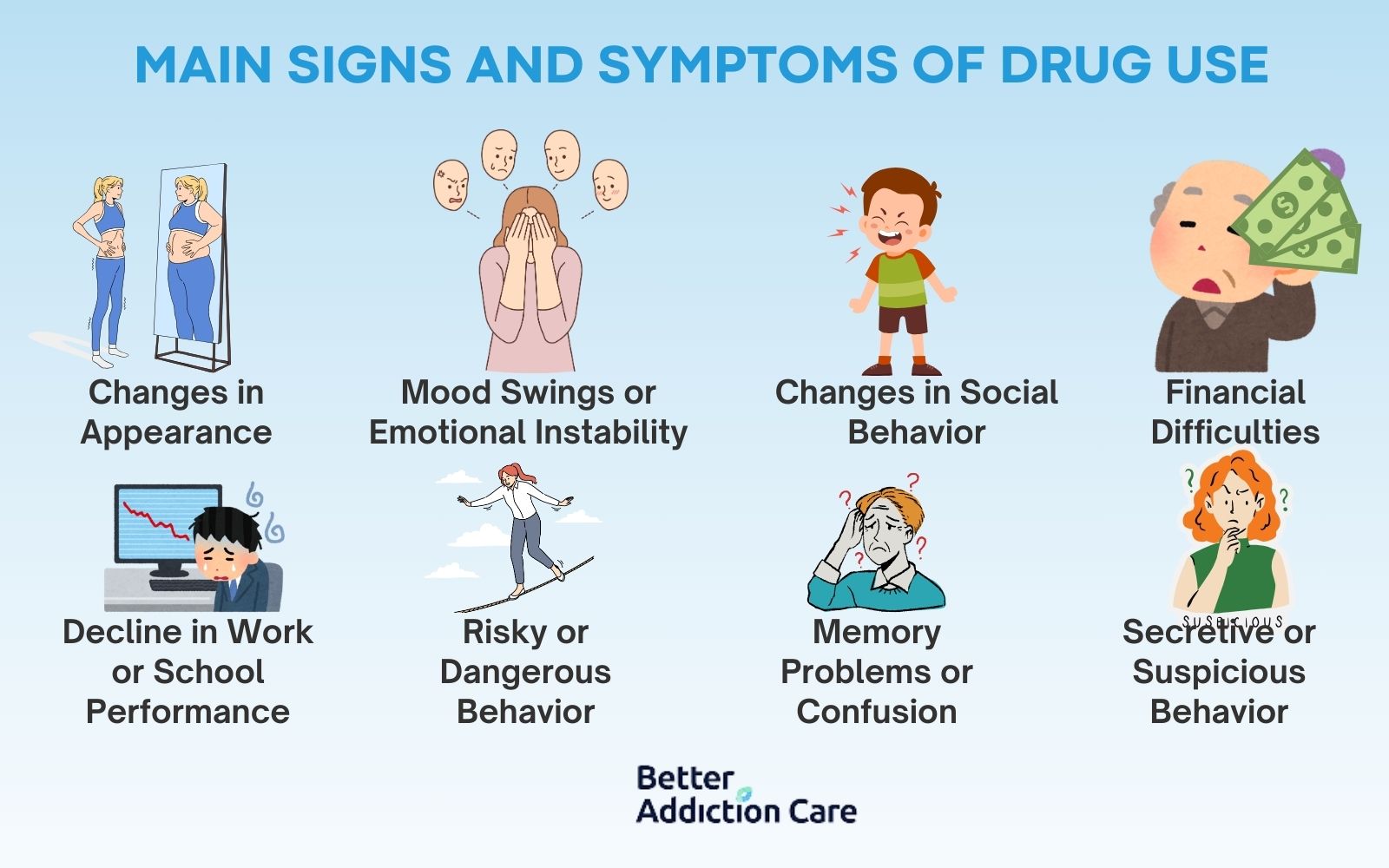
What are the Main Signs and Symptoms of Drug Use?
The main signs of drug use include a multitude of symptoms dependent upon the type of drug used and how severe the addiction to the drug is. While each individual will experience different physical, emotional, and behavioral changes, there are common patterns that signal drug misuse. These signs range from subtle changes to more pronounced symptoms as the addiction progresses.
Here is a list of the signs and symptoms of drug use:
-
Changes in Appearance
A noticeable decline in personal grooming or hygiene, such as weight loss, bloodshot eyes, or neglected clothing, indicates drug use. These are short-term signs, but if the drug use persists, these physical changes worsen and become more pronounced over time. -
Mood Swings or Emotional Instability
Sudden shifts in mood, such as irritability, agitation, or extreme euphoria, is a symptom of drug use. Drugs alter brain chemistry, leading to unpredictable emotional responses. This is a short-term sign, but long-term use results in chronic emotional instability. -
Changes in Social Behavior
Withdrawal from family and friends or a shift in social circles, especially toward individuals with a history of drug use, are a sign. In the short term, this involves avoiding social gatherings, but over time, it leads to isolation and the loss of meaningful relationships. -
Financial Difficulties
An increase in borrowing money, selling personal items, or unexplained financial struggles suggest drug use. This is a longer-term symptom, as individuals begin to prioritize obtaining drugs over financial responsibilities. -
Decline in Work or School Performance
Drug use impairs concentration, motivation, and energy, leading to missed deadlines, lower grades, or poor job performance. This is both a short-term and long-term sign, as early use causes immediate decline, but persistent use leads to serious academic or career consequences. -
Risky or Dangerous Behavior
Engaging in unsafe activities, such as driving under the influence or getting into physical altercations, are a sign of drug use. These behaviors are short-term responses to the disinhibition caused by drugs but leads to long-term legal or personal consequences. -
Memory Problems or Confusion
Drug use impairs cognitive function, causing memory loss, confusion, or difficulty concentrating. These are short-term effects that will worsen with continued use, potentially leading to long-term cognitive decline. -
Secretive or Suspicious Behavior
Individuals using drugs start lying about their whereabouts, hiding substances, or avoiding conversations about their activities. This is a short-term sign that becomes a persistent issue as drug use escalates and secrecy becomes a necessity to cover their addiction.
What are the Main Signs and Symptoms of K2 (Spice)?

The main signs and symptoms of K2 (Spice) are listed below:
-
Paranoia and Hallucinations: One of the most common symptoms of K2 use is intense paranoia and vivid hallucinations. The synthetic cannabinoids in K2 affect the brain more than regular marijuana, leading to severe mental disorientation. These symptoms are short-term but result in dangerous behaviors, as users act irrationally or harm themselves due to their altered perception of reality.
-
Aggressive or Violent Behavior: K2 triggers aggressive or even violent outbursts in users. This happens because of the drug’s unpredictable effects on brain chemicals, leading to heightened agitation and loss of impulse control. These behaviors are short-term but escalate quickly, especially with continued or higher doses.
-
Physical Symptoms (Rapid Heart Rate, Nausea): K2 use leads to physical symptoms such as a racing heart, dizziness, and nausea. These reactions occur due to the toxic chemicals in synthetic cannabinoids, leading to severe health problems if use is prolonged. Short-term use results in these symptoms almost immediately, while long-term use causes more serious cardiovascular issues.
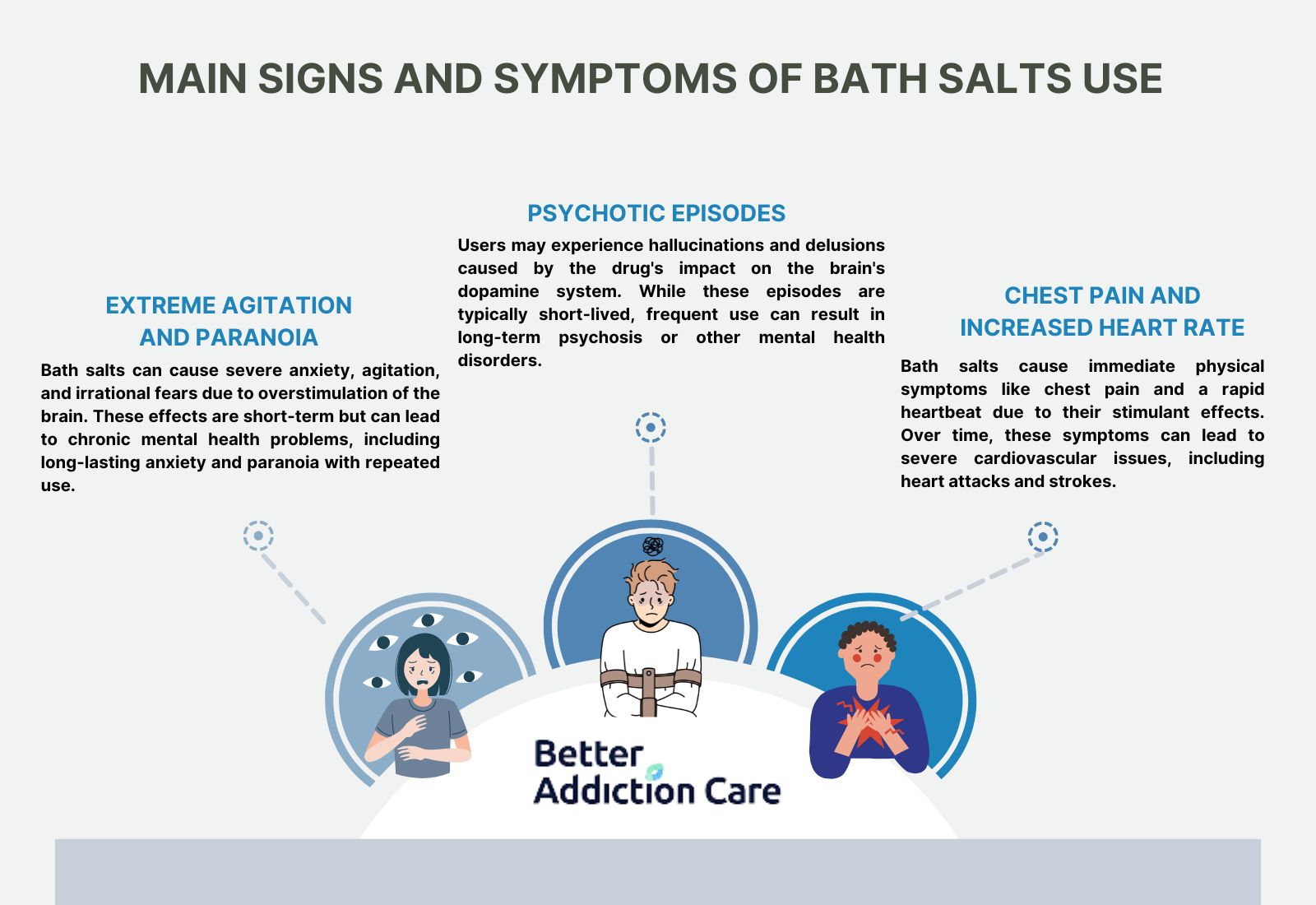
What are the Main Signs and Symptoms of Bath Salts?
The main signs and symptoms of bath salts include:
-
Extreme Agitation and Paranoia: Bath salts cause extreme agitation, anxiety, and paranoia. These synthetic stimulants over-stimulate the brain, leading to delusions and irrational fears. This symptom is short-term, occurring shortly after ingestion, but repeated use results in chronic mental health issues like anxiety and paranoia.
-
Psychotic Episodes: Bath salts induce psychotic episodes, where users experience severe hallucinations and delusions. The drug’s potent effect on the brain's dopamine system leads to significant mental disturbances. These episodes are short-term, but repeated use results in long-lasting psychosis or other mental health disorders.
-
Chest Pain and Increased Heart Rate: Immediate physical symptoms of bath salts include chest pain accompanied by a rapid heart rate. This occurs due to the drug’s stimulant effects, which put immense strain on the cardiovascular system. These symptoms are short-term but lead to heart attacks, strokes, or other long-term heart issues with repeated use.
What are the Main Signs and Symptoms of Barbiturates, Benzodiazepines, and Hypnotics?
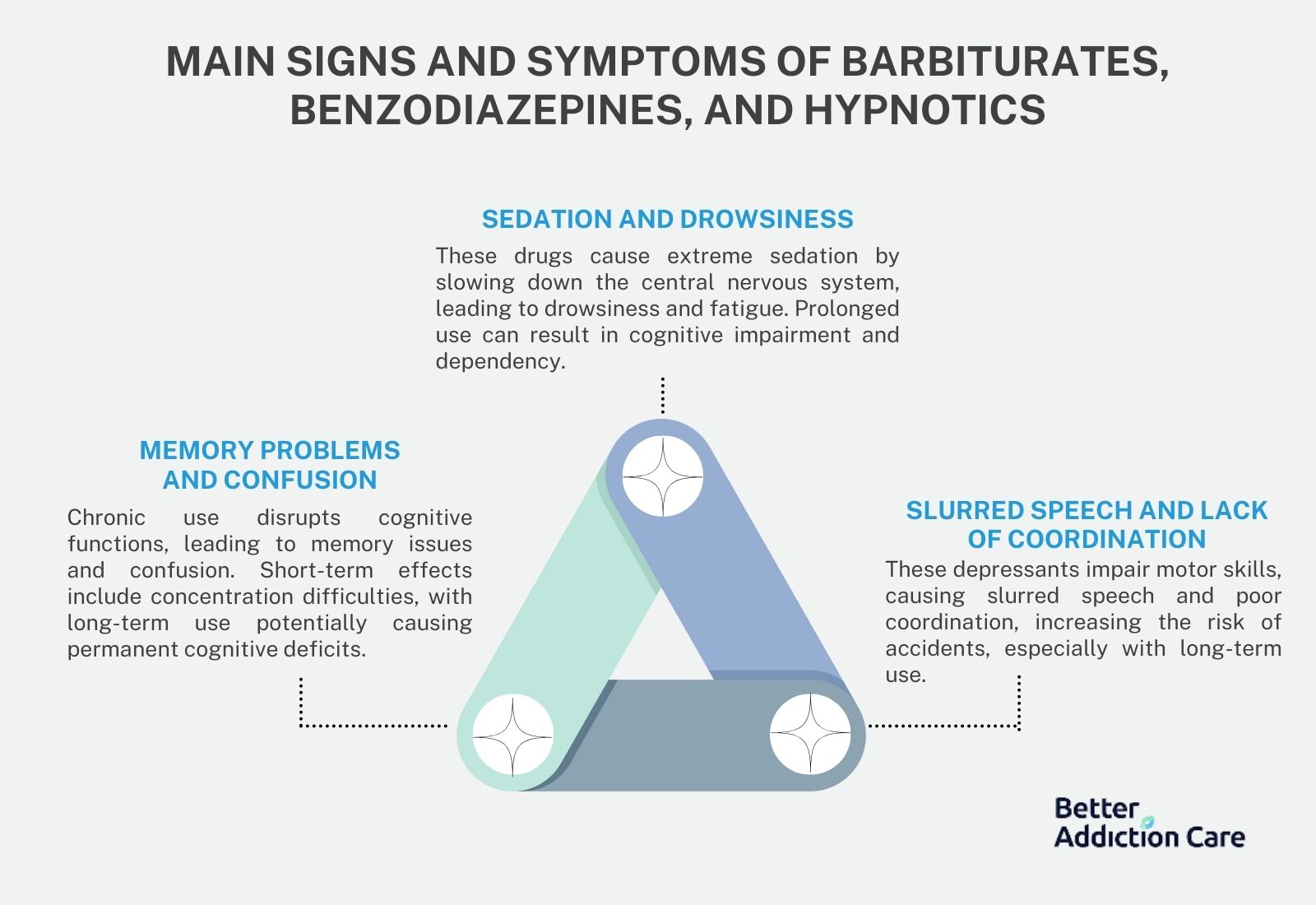
The main signs and symptoms of barbiturates, benzodiazepines, and hypnotics are listed below:
-
Sedation and Drowsiness: The primary effect of barbiturates, benzodiazepines, and hypnotics is extreme sedation. These drugs slow down the central nervous system, leading to drowsiness and fatigue. This is a short-term symptom while the drugs are active, but long-term use results in cognitive impairment and dependency.
-
Memory Problems and Confusion: Chronic use of these depressants results in memory issues and confusion, as they disrupt brain function related to cognitive tasks. Over time, users struggle with short-term memory and experience difficulty concentrating. While confusion is a short-term side effect, prolonged use leads to permanent cognitive deficits.
-
Slurred Speech and Lack of Coordination: Barbiturates, benzodiazepines, and hypnotics impair motor functions, causing slurred speech and poor coordination. This results from their depressant effects on the brain, which slow down the body's physical responses. These symptoms are short-term but increase the risk of accidents or injuries, especially in long-term users who experience these effects regularly.
What are the Main Signs and Symptoms of Meth, Cocaine, and Other Stimulants?
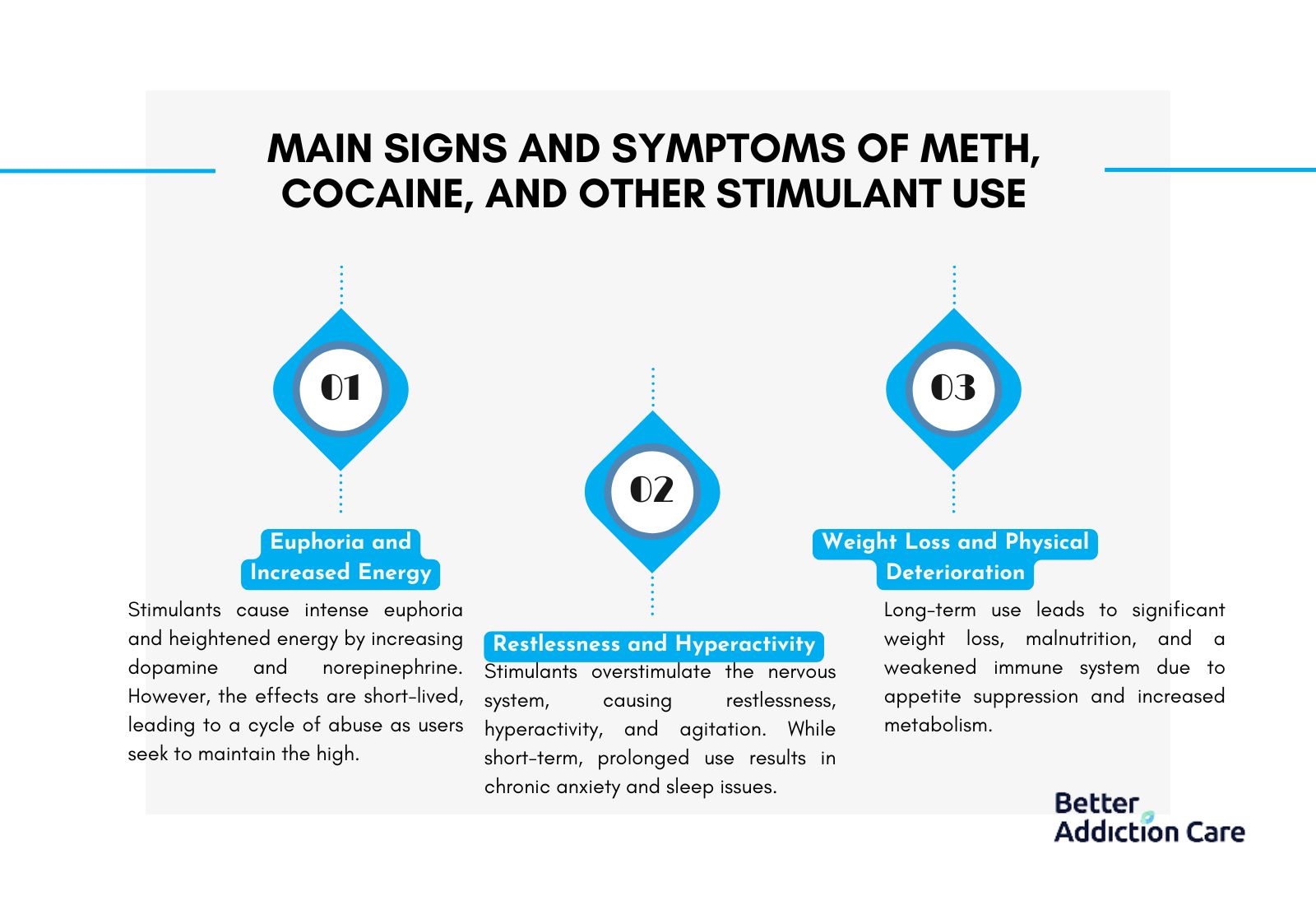
The main signs and symptoms of meth, cocaine and other stimulants include:
-
Euphoria and Increased Energy: Meth, cocaine, and other stimulants cause an intense feeling of euphoria and energy due to their effect on dopamine and norepinephrine in the brain. This leads to heightened alertness and activity in the short term. However, this feeling is short-lived, and frequent users take more to maintain the high, leading to a cycle of abuse.
-
Restlessness and Hyperactivity: Users of stimulants experience extreme restlessness and hyperactivity. These drugs over-stimulate the brain’s nervous system, leading to constant movement, agitation, and an inability to relax. This is a short-term symptom while under the drug’s influence, but prolonged use causes chronic anxiety and sleep disturbances.
-
Weight Loss and Physical Deterioration: Long-term stimulant use, especially meth and cocaine, results in significant weight loss due to appetite suppression and increased metabolism. Over time, this leads to malnutrition, weakened immune systems, and other health problems. This symptom becomes more pronounced with long-term use and is difficult to reverse without medical intervention.
What are the Main Signs and Symptoms of Club Drugs?
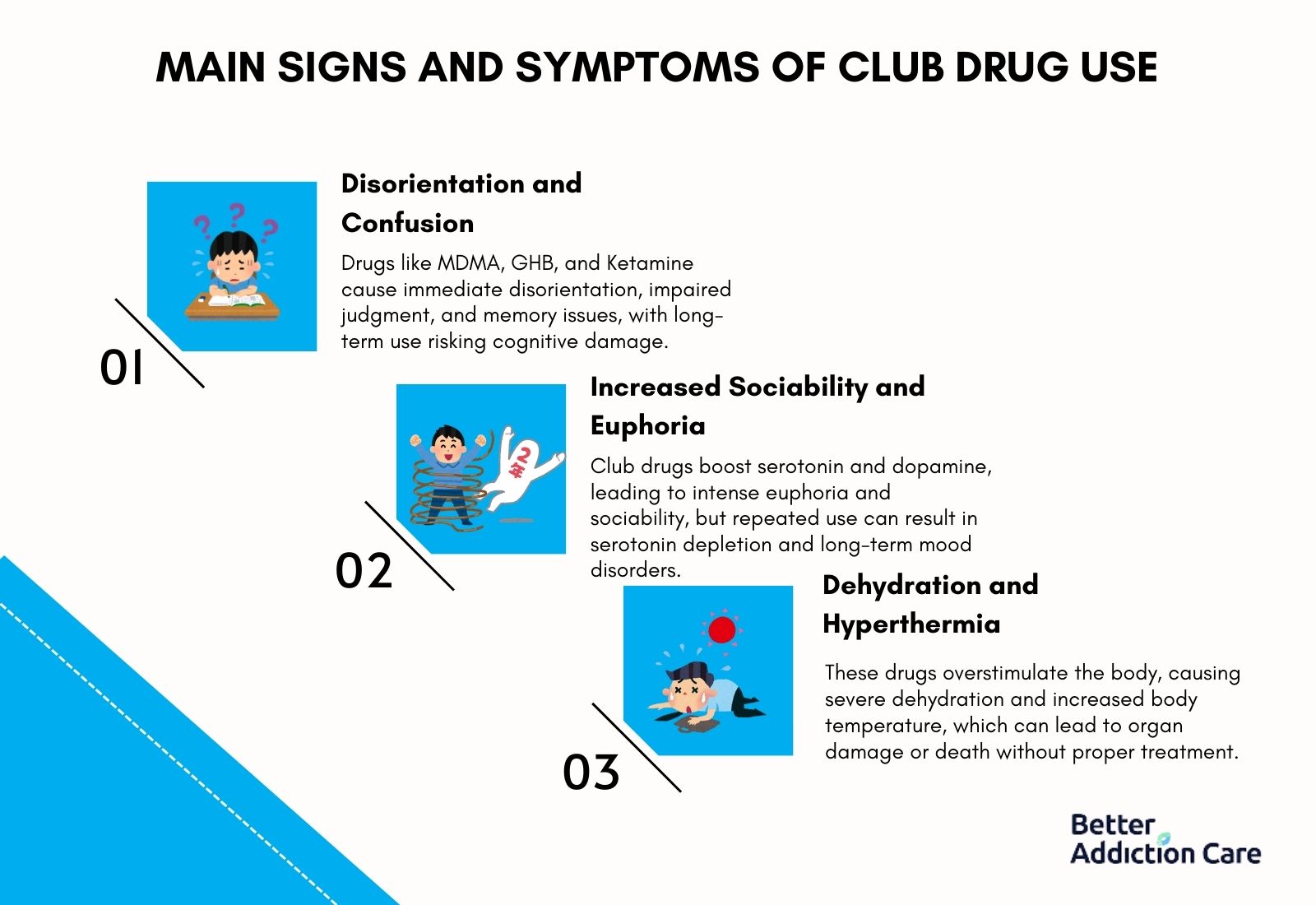
The main signs and symptoms of club drugs are listed below:
-
Disorientation and Confusion: Club drugs such as MDMA, GHB, and Ketamine frequently cause severe disorientation and confusion. These drugs alter brain chemistry, leading to impaired judgment, memory issues, and difficulty focusing. Disorientation occurs immediately after ingestion and risks lasting cognitive damage with repeated use.
-
Increased Sociability and Euphoria: Club drugs induce heightened sociability and intense euphoria by boosting serotonin and dopamine levels. Emotional closeness and extreme happiness are typical short-term effects, but frequent use results in serotonin depletion, causing long-term mood disorders and depression.
-
Dehydration and Hyperthermia: Severe dehydration and elevated body temperature are common with club drug use. These drugs overstimulate the body, leading to excessive sweating and overheating. Without treatment, long-term organ damage or even death is possible.
What are the Main Signs and Symptoms of Hallucinogens?
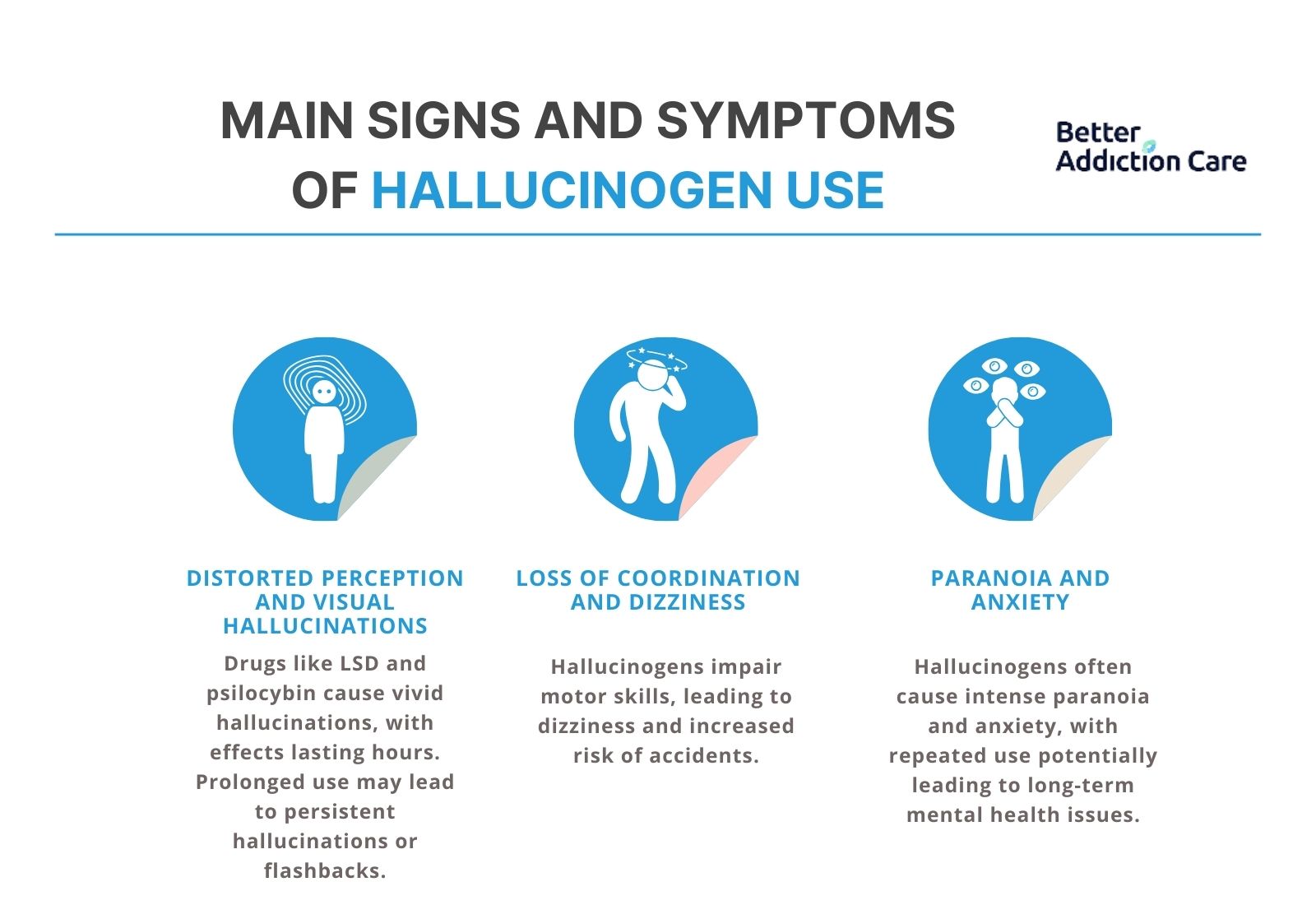
The main signs and symptoms of hallucinogens are listed below:
-
Distorted Perception and Visual Hallucinations: Drugs like LSD and psilocybin cause profound distortions in perception, leading to vivid visual and auditory hallucinations. These effects last for several hours, but prolonged use risks persistent hallucinations or flashbacks.
-
Loss of Coordination and Dizziness: Hallucinogens impair motor functions, causing loss of coordination and dizziness by disrupting brain signals that control movement and balance. This short-term symptom increases the likelihood of falls and injuries during intoxication.
-
Paranoia and Anxiety: Many hallucinogens frequently trigger intense paranoia and anxiety. Distorted reality leads to fear and panic. Repeated use risks long-term mental health issues such as chronic anxiety.
What are the Main Signs and Symptoms of Inhalants?
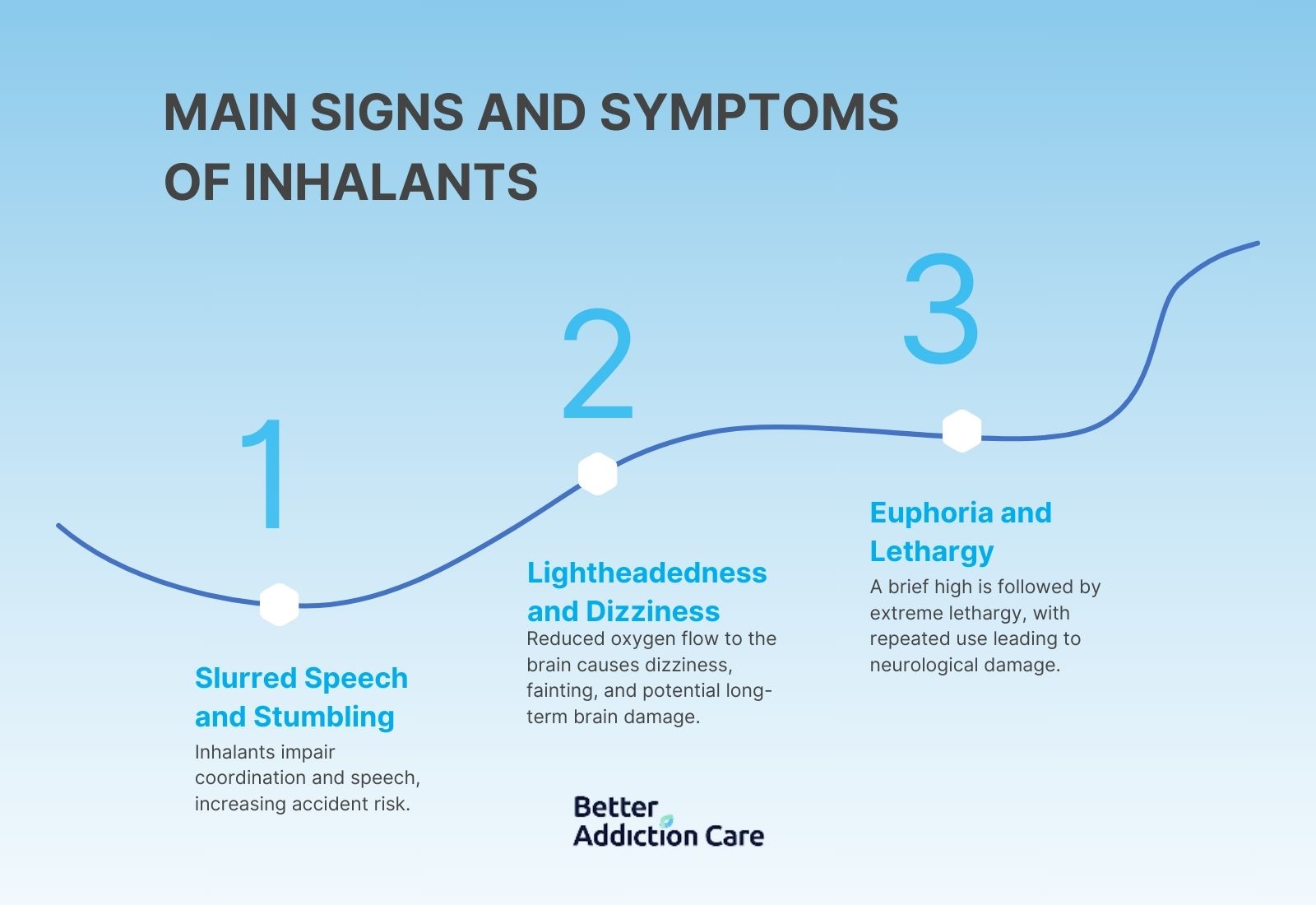
The main signs and symptoms of inhalants are listed below:
-
Slurred Speech and Stumbling: Drugs like paint thinners and aerosols immediately depress the central nervous system, causing slurred speech and stumbling. The user is more prone to accidents or injuries during use.
-
Lightheadedness and Dizziness: Inhalant use rapidly leads to lightheadedness and dizziness due to reduced oxygen flow to the brain. Short-term use leads to fainting or sudden death, while long-term use results in brain damage and organ failure.
-
Sudden Euphoria Followed by Lethargy: Inhalants trigger a brief period of euphoria followed by intense lethargy. The cycle of stimulation and sedation is a sign of inhalant abuse, with repeated use leading to neurological damage and other serious health issues.
What are the Main Signs and Symptoms of Opioid Painkillers?
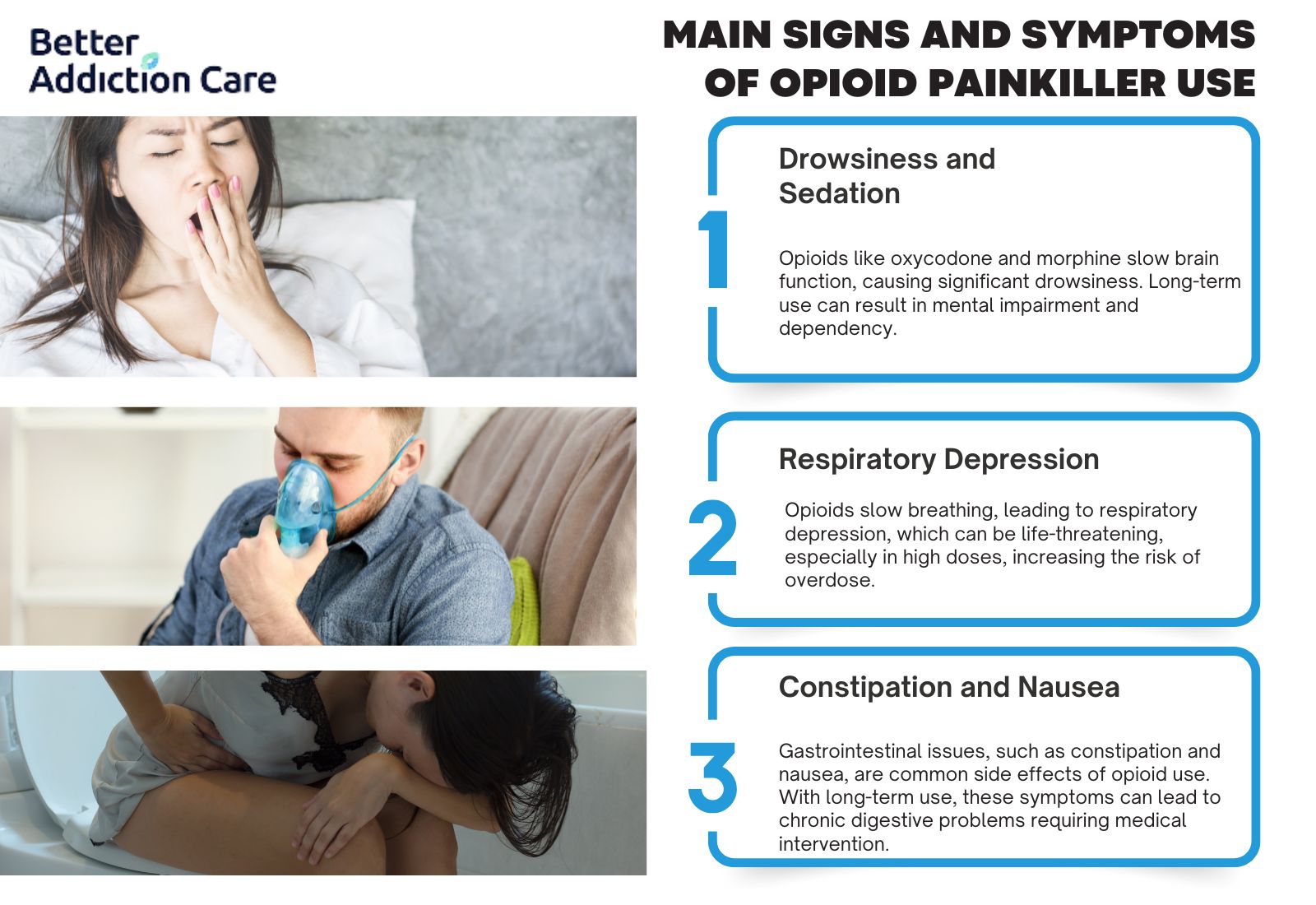
The main signs and symptoms of opioid painkillers are listed below:
-
Drowsiness and Sedation: Opioid painkillers like oxycodone and morphine induce significant drowsiness and sedation by slowing brain function. Long-term use results in dependency and reduced mental sharpness.
-
Respiratory Depression: Opioid use slows down breathing, leading to respiratory depression. In high doses, this short-term symptom causes life-threatening oxygen deprivation, increasing the risk of fatal overdose.
-
Constipation and Nausea: Most opioids cause gastrointestinal issues such as constipation and nausea. These short-term symptoms lead to chronic digestive problems with long-term use, requiring medical treatment.
Can Drug Rehab Cure Drug Addiction?
Yes, drug rehab can help individuals overcome drug addiction for several key reasons. First, rehab provides a structured environment with medical and psychological support, which is important for managing withdrawal symptoms and preventing relapse. Second, rehab programs include behavioral therapies, such as Cognitive Behavioral Therapy (CBT), that address the root causes of addiction, helping individuals develop coping strategies to maintain sobriety. According to a meta-review published in the journal Psychological Medicine in 2021, CBT has more evidence supporting it than any other psychological therapy across various physical and mental conditions Finally, drug rehab offers aftercare support, such as counseling and peer support groups, which helps individuals stay committed to their recovery long after completing the program.
What is Drug Abuse?
Drug abuse is the misuse of legal or illegal substances in a way that is harmful to the individual. It involves taking larger doses or using drugs for non-medical purposes, leading to dangerous behaviors and health risks. The difference between drug abuse and addiction is that abuse involves harmful use without dependency, whereas addiction is characterized by a compulsive need to use drugs, despite negative consequences. Addiction involves both physical and psychological dependence, while abuse may or may not lead to addiction.
What are Risk Factors for Substance Abuse?
The risk factors for substance abuse are genetic predisposition, environmental influence and mental health disorders. One key risk factor is genetics, as individuals with a family history of addiction are more prone to developing similar issues. According to the National Institute on Drug Abuse (NIDA), genetics account for approximately 40% to 60% of a person’s vulnerability to drug addiction. Another significant risk factor is environmental influence, such as growing up in an unstable home or being surrounded by peer pressure, which makes drug experimentation more likely. Lastly, mental health disorders such as anxiety or depression significantly increase the risk of substance abuse, as individuals turn to drugs as a way to self-medicate or escape emotional pain.
Is Drug Addiction a Disease?
Yes, drug addiction is a disease according to the American Medical Association (AMA). It iis classified as a disease because it changes the brain's structure and function, affecting behavior and making it a chronic, relapsing condition. This classification aligns with the understanding that addiction disrupts normal brain functions, similar to other chronic diseases like heart disease or diabetes as written by the American Medical Association, in a study titled "Addiction as a Disease." There are several reasons it is considered a disease. First, it alters brain function, particularly in areas related to reward, motivation, and decision-making, which is a hallmark of chronic diseases. Second, addiction is progressive, meaning it worsens over time if untreated, similar to other chronic illnesses like diabetes or heart disease. Lastly, like other diseases, addiction requires ongoing treatment and management, as relapses are common, and recovery is a lifelong process.
What Celebrities Suffer from Drug Addiction?
These celebrities that suffer from drug addiction have been open about their struggles. Drug addiction affects individuals from all walks of life, including high-profile celebrities. Many well-known figures are using their platform to raise awareness about addiction and recovery. Here is a list of celebrities who have battled drug addiction:
-
Robert Downey Jr. – Struggled with drug addiction in the 1990s, impacting his acting career until he sought rehabilitation.
-
Demi Lovato – Battled addiction to cocaine and alcohol, which led to multiple stints in rehab and an overdose in 2018.
-
Elton John – Overcame a long-term addiction to alcohol and cocaine, now advocates for addiction recovery.
-
Jamie Lee Curtis – Openly discussed her recovery from an addiction to painkillers.
-
Matthew Perry – Struggled with addiction to opioids and alcohol during the height of his Friends fame.
-
Lindsay Lohan – Battled with substance abuse issues, leading to numerous legal troubles and rehab stints.
-
Eminem – Faced a long-term addiction to prescription drugs, particularly Vicodin and Valium, before seeking treatment.
-
Ozzy Osbourne – Has faced long-term battles with alcohol and drugs throughout his career.
What are the Most Important Research Papers About Drug Addiction?
The most imporant research papers about drug addiciton incude writings from Nora D. Volkow, Kenneth Kendler and George Koob. Drug addiction has been a subject of extensive research, and several important studies have shaped the understanding of its causes, consequences, and treatments. Below are three significant research papers, each contributing valuable insights into addiction:
-
"Addiction as a Brain Disease" by Nora D. Volkow (National Institute on Drug Abuse, NIDA)
This pivotal study highlights the conclusion that addiction fundamentally alters brain structure and function, particularly in areas controlling reward and decision-making. The study was conducted through neuroimaging techniques to observe changes in brain activity. It underscored addiction as a chronic disease rather than a behavioral choice. -
"Risk Factors for Addiction: A Twin Study" by Kenneth Kendler (Virginia Commonwealth University)
This research paper concluded that genetics play a significant role in addiction risk, estimating that about 40 to 60% of susceptibility to drug addiction is inherited. The study utilized twin data to assess the impact of genetic factors on addiction across various substance use disorders. -
"The Impact of Environmental and Social Factors on Addiction" by George Koob (National Institute on Alcohol Abuse and Alcoholism, NIAAA)
This paper found that environmental and social factors, such as childhood trauma and socioeconomic status, significantly influence addiction risk. The study conducted a longitudinal analysis of individuals from different socio-economic backgrounds to explore the relationship between environment and drug use behaviors.