OxyContin Addiction: Effects, Causes, Dangers and Treatment
OxyContin addiction refers to a chronic disorder characterized by the compulsive use of OxyContin despite harmful consequences. According to the National Institute on Drug Abuse (NIDA), titled "Prescription Opioids and Addiction," published in 2020, OxyContin misuse is a significant factor in the opioid epidemic, with approximately 3.5 million people in the U.S. misusing prescription pain relievers, including OxyContin, in the past year.
OxyContin addiction refers to a chronic disorder characterized by the compulsive use of OxyContin despite harmful consequences. According to the National Institute on Drug Abuse (NIDA), titled "Prescription Opioids and Addiction," published in 2020, OxyContin misuse is a significant factor in the opioid epidemic, with approximately 3.5 million people in the U.S. misusing prescription pain relievers, including OxyContin, in the past year.
Key signs of oxycontin addiction include intense cravings, an inability to stop using the drug, and physical withdrawal symptoms like nausea, sweating, and agitation. According to a study by Rawson et al. titled "OxyContin Abuse: Who Are the Users?" published in the American Journal of Psychiatry (2007), addiction is marked by a history of repeated substance misuse.
The main causes of oxycontin addiction include prolonged use, genetic predisposition, and exposure to environments that normalize drug misuse. Aggressive marketing of OxyContin as a safe painkiller contributed significantly to its widespread misuse, as outlined in the study "The Promotion and Marketing of OxyContin: A Public Health Tragedy" by Van Zee in the American Journal of Public Health (2009).
The dangers of OxyContin addiction include severe respiratory depression, overdose, and a heightened risk of death when combined with other substances like alcohol or benzodiazepines. As reported in the study "Changing Patterns in Opioid Addiction" by Sproule et al., published in the Canadian Family Physician (2009), the drug’s manipulation for non-medical use increases these risks.
Treatment of oxycontin involves a combination of medical detoxification, behavioral therapies, and medication-assisted treatment such as methadone or buprenorphine. According to the National Institute on Drug Abuse (2020), these treatments help manage withdrawal and reduce cravings effectively.
What Is Oxycontin Addiction?
OxyContin addiction is defined as a substance use disorder characterized by the compulsive misuse of OxyContin, a controlled-release formulation of oxycodone, leading to significant impairment in daily life.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), addiction is marked by persistent cravings, inability to control usage, and continued use despite adverse consequences.
OxyContin is among the most commonly abused prescription opioids. In the United States, approximately 1.7 million individuals had substance use disorders involving prescription opioids in 2019, according to study by the Substance Abuse and Mental Health Services Administration (SAMHSA), titled "Key Substance Use and Mental Health Indicators in the United States," published in 2020.
The Centers for Disease Control and Prevention (CDC)also reported 70,630 drug overdose deaths in 2019, with 14,139 involving prescription opioids like OxyContin. This makes overdose one of the leading causes of death in opioids like oxycontin misuse.
Demographically, non-Hispanic whites in rural areas of the U.S. show the highest rates of OxyContin addiction, with males aged 25–44 being the most affected. According to a study by Katz and Hays titled "Adolescent OxyContin Abuse," published in the Journal of the American Academy of Child and Adolescent Psychiatry (2004), rural regions see higher addiction rates due to ease of access and cultural normalization of prescription drug use.
What Is Oxycontin?
OxyContin is a brand-name prescription medication containing oxycodone, a potent opioid analgesic. It is designed as a controlled-release tablet to manage moderate to severe chronic pain, particularly in cases requiring long-term, around-the-clock treatment. According to Purdue Pharma’s product information, OxyContin delivers pain relief over 12 hours.
The medication is classified as a Schedule II controlled substance under the Controlled Substances Act by the U.S. Drug Enforcement Administration (DEA). This classification indicates it has a high potential for abuse, leading to severe psychological or physical dependence.
On the streets, OxyContin is referred to as "Hillbilly Heroin," "Oxy," or "OC." A study by Sproule et al. titled "Changing Patterns in Opioid Addiction," published in the Canadian Family Physician (2009) found that street availability and manipulation for non-medical use significantly contribute to its widespread misuse
Why Is Oxycontin Addictive?
OxyContin is addictive because it interacts with the brain’s opioid receptors, triggering intense euphoria and a sense of well-being, which reinforces compulsive use. Its extended-release formula is manipulated—by crushing or snorting—to bypass its time-release mechanism, delivering a high dose rapidly and increasing its addictive potential.
According to the National Institute on Drug Abuse (2020), prescription opioids like OxyContin accounted for a significant portion of the 14,139 deaths caused by prescription opioid overdoses in the U.S.
The severity of addiction lies in the development of tolerance, where users require increasingly larger doses to achieve the same effect. This escalates the risk of overdose and life-threatening respiratory depression.
Who Is At Risk Of Oxycontin Addiction?
The individuals at risk for OxyContin addiction include those with a history of substance use disorders, individuals prescribed opioids for chronic pain, and people with untreated mental health conditions. The combination of genetic predisposition, environmental factors, and prolonged exposure to opioids also increases vulnerability.
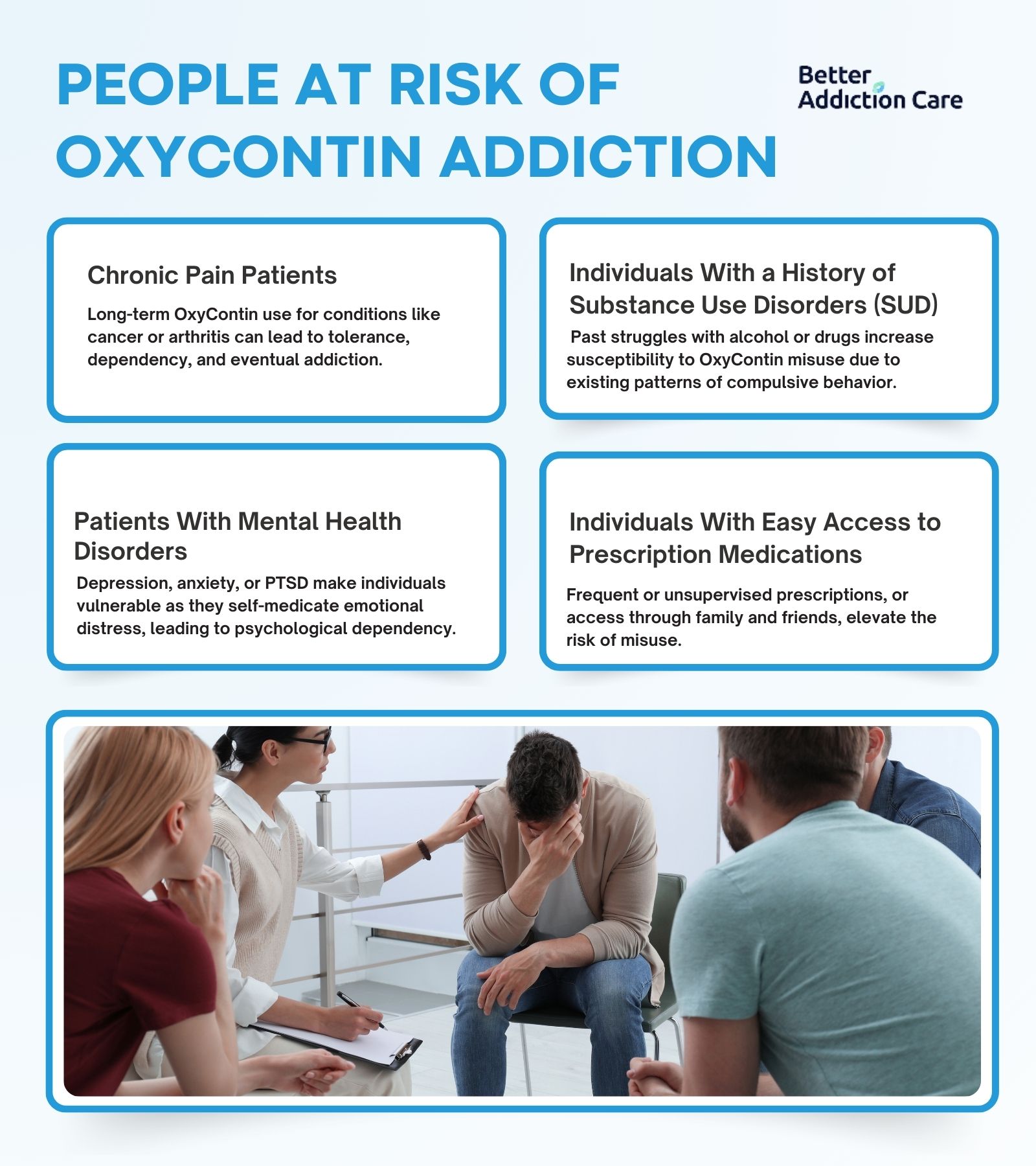
The people at risk of oxycontin addiction are explained below:
-
Chronic Pain Patients: Individuals managing long-term pain conditions such as cancer, arthritis, or severe injuries are at risk due to prolonged use of OxyContin. Over time, the body builds tolerance, requiring higher doses for the same effect, which leads to dependency and addiction. According to a study by Whelan et al. (2011) highlighted that chronic pain patients represent a significant portion of those prescribed OxyContin who develop misuse behaviors.
-
Individuals With a History of Substance Use Disorders (SUD): People with prior struggles with alcohol, tobacco, or illicit drugs are more susceptible to OxyContin addiction. Their existing patterns of compulsive behavior and chemical dependency increase the likelihood of misuse once they are introduced to opioids.
-
Patients With Mental Health Disorders: Depression, anxiety, and PTSD make individuals vulnerable, as they misuse OxyContin to self-medicate emotional distress. The drug's ability to temporarily numb emotional pain quickly leads to psychological dependence.
-
Individuals With Easy Access to Prescription Medications: Those with frequent prescriptions, unsupervised use, or access through family and friends are at higher risk. Accessibility leads to misuse, particularly in environments where medication diversion is common.
What Are The Symptoms And Effects Of Oxycontin Addiction?
The symptoms and effects of OxyContin addiction include intense cravings, physical dependence, and significant psychological and physiological harm. The drug's addictive nature stems from its ability to trigger the brain's reward system by releasing dopamine, reinforcing compulsive use and leading to dependency. Withdrawal symptoms further perpetuate the cycle of addiction, making it difficult for users to quit.
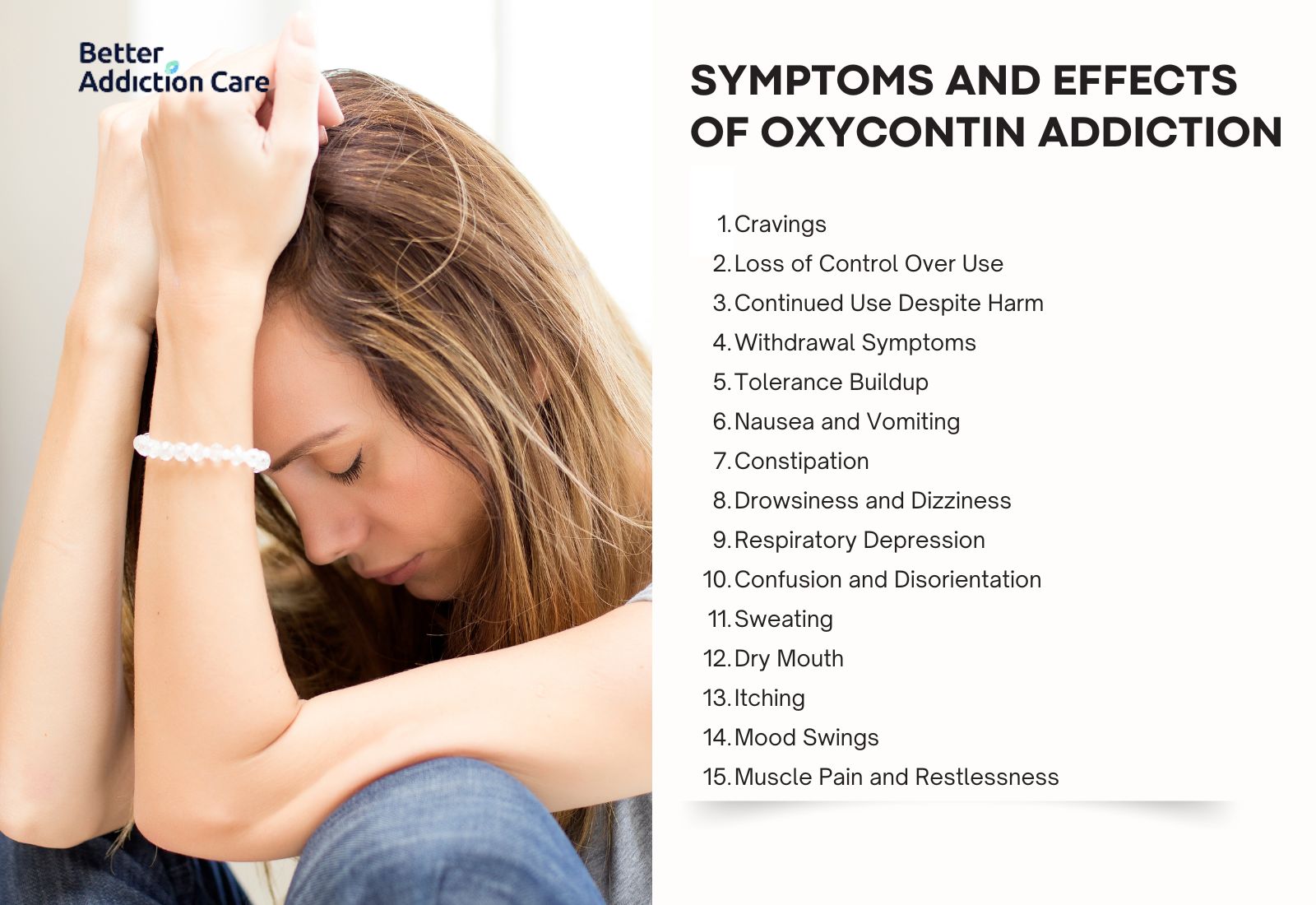
The symptoms and effects of OxyContin addiction are explained below:
-
Cravings: Strong, uncontrollable urges to use OxyContin, driven by the brain's reward system. This psychological symptom is central to addiction and leads to relapse without intervention.
-
Loss of Control Over Use: Individuals consume more OxyContin than prescribed or use it recreationally, unable to regulate their intake despite harmful consequences. This psychological sign reflects the compulsive nature of addiction.
-
Continued Use Despite Harm: Users persist in taking OxyContin even when it causes physical damage, relationship problems, or work-related issues. This behavioral symptom highlights the grip of addiction on decision-making.
-
Withdrawal Symptoms: When OxyContin use is reduced or stopped, individuals experience nausea, vomiting, sweating, and agitation. According to a study by Coplan et al. titled "The Effect of an Abuse-Deterrent Opioid Formulation on Addiction," published in Clinical Pharmacology and Therapeutics (2016), withdrawal is a hallmark sign of physical dependence.
-
Tolerance Buildup: The body adapts to OxyContin over time, requiring higher doses to achieve the same effect. This physical symptom increases overdose risk as users take dangerously large amounts.
-
Nausea and Vomiting: Common physical side effects of prolonged use or withdrawal. These symptoms occur due to OxyContin’s impact on the gastrointestinal tract and brainstem.
-
Constipation: A severe physical symptom resulting from OxyContin’s suppression of gastrointestinal motility. It also requires medical treatment.
-
Drowsiness and Dizziness: These physical symptoms result from the drug's depressant effects on the central nervous system and impair daily functioning.
-
Respiratory Depression: One of the most severe physical effects of OxyContin is slowing breathing to life-threatening levels. This effect is a leading cause of fatal overdoses, as reported by the CDC (2019).
-
Confusion and Disorientation: Psychological symptoms caused by OxyContin’s effects on cognitive function, seen during intoxication or withdrawal.
-
Sweating: A withdrawal symptom reflecting the body’s response to the absence of the drug. Chills and fever-like sensations accompany this physical symptom.
-
Dry Mouth: A common side effect of OxyContin, as it reduces saliva production and impacts oral health.
-
Itching: A mild physical side effect caused by histamine release, reported during intoxication.
-
Mood Swings: Psychological symptoms ranging from euphoria during use to depression during withdrawal, contributing to emotional instability.
-
Muscle Pain and Restlessness: Physical symptoms seen in withdrawal as the body adjusts to the absence of OxyContin.
What Are The Causes Of Oxycontin Addiction?
The causes of OxyContin addiction include chronic pain management, overprescription, genetic predisposition, and mental health disorders, among other factors. These causes intertwine, creating a complex pathway to dependency and addiction.
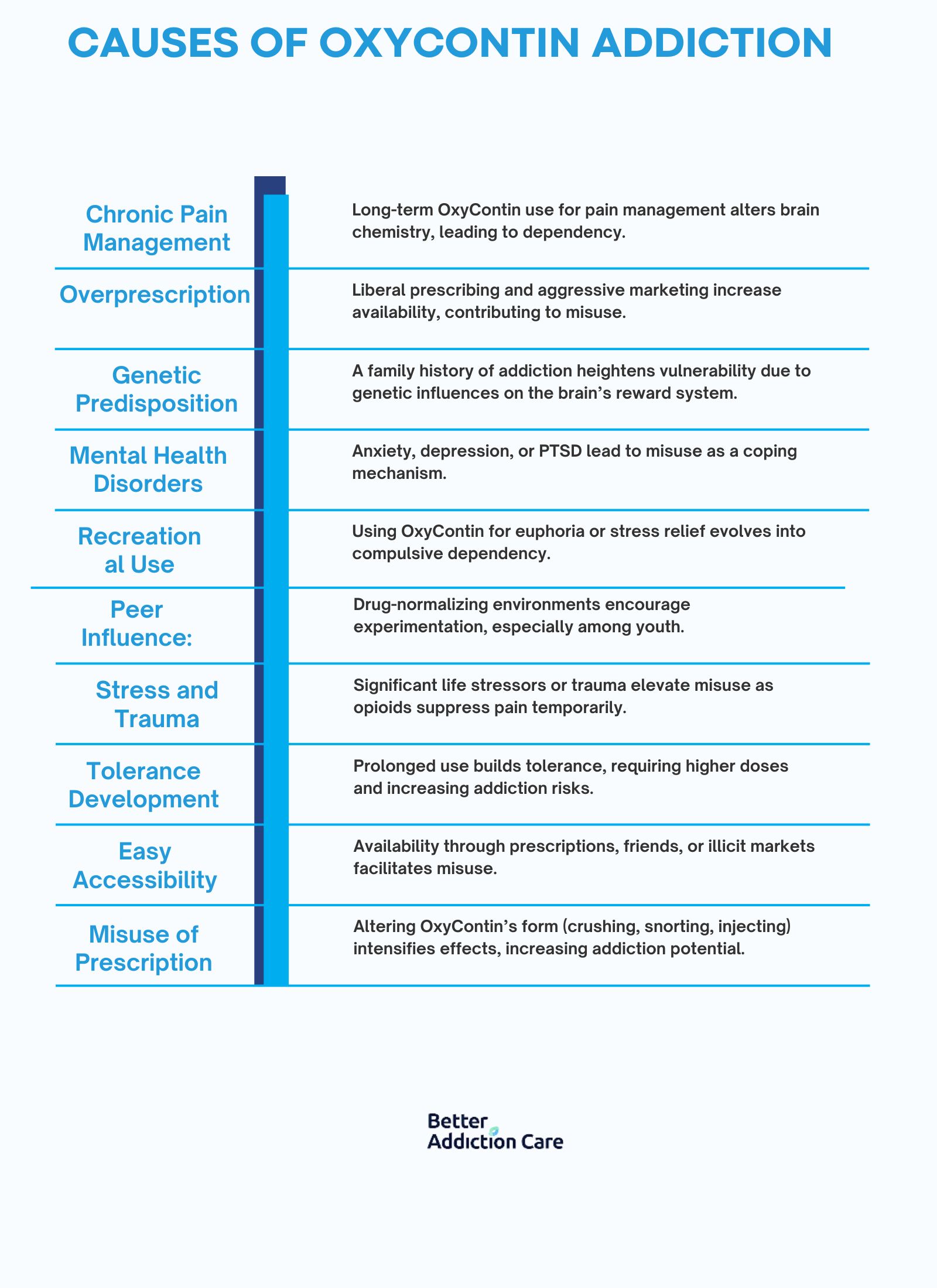
The causes of oxycontin addiction are explained below:
-
Chronic Pain Management: OxyContin is frequently prescribed for long-term pain management in conditions like cancer or severe injuries. Prolonged use alters the brain’s chemistry, leading to physical dependency. According to a study by Sproule et al. titled "Changing Patterns in Opioid Addiction," published in the Canadian Family Physician (2009), chronic pain patients prescribed opioids long-term are among the most vulnerable to addiction.
-
Overprescription: Aggressive marketing and liberal prescribing practices have made OxyContin widely available. Many individuals become addicted due to overprescription by healthcare providers, a factor emphasized in the study "The Promotion and Marketing of OxyContin: A Public Health Tragedy" by Van Zee, published in the American Journal of Public Health (2009).
-
Genetic Predisposition: Individuals with a family history of addiction are more likely to develop dependency. Genetic factors influence how the brain’s reward system responds to opioids, increasing the risk of compulsive use.
-
Mental Health Disorders: Conditions like anxiety, depression, and PTSD lead individuals to misuse OxyContin as a coping mechanism. This correlation of self-medication and coping mechanisms contributes to addiction.
-
Recreational Use: Some individuals use OxyContin recreationally to achieve euphoria or escape stress, initiating a cycle of misuse that can progress to addiction. The initial voluntary use evolves into compulsive dependency as tolerance develops.
-
Peer Influence: Social environments where drug use is normalized encourage experimentation with OxyContin. This external pressure is particularly impactful among younger populations.
-
Stress and Trauma: Experiencing significant life stressors or traumatic events increases the likelihood of OxyContin misuse. Stress elevates cravings, as opioids temporarily suppress emotional and physical pain.
-
Tolerance Development: With continued use, the body builds a tolerance to OxyContin, requiring larger doses to achieve the desired effect. This physiological change leads to misuse and escalates the risk of addiction.
-
Easy Accessibility: The widespread availability of OxyContin through prescriptions, friends, or illicit markets makes it easier for individuals to begin using and subsequently misusing the drug. As highlighted in the SAMHSA (2020) report, easy access is a significant driver of opioid addiction.
-
Misuse of Prescription: Crushing, snorting, or injecting OxyContin to bypass its time-release mechanism intensifies its effects, increasing both the addictive potential and the risk of overdose.
What Are The Dangers Of Oxycontin Addiction?
The dangers of OxyContin addiction are overdose, respiratory depression, and severe physical, psychological, and social consequences. Prolonged misuse of OxyContin impacts nearly every aspect of an individual's life, leading to life-threatening complications and long-term harm.
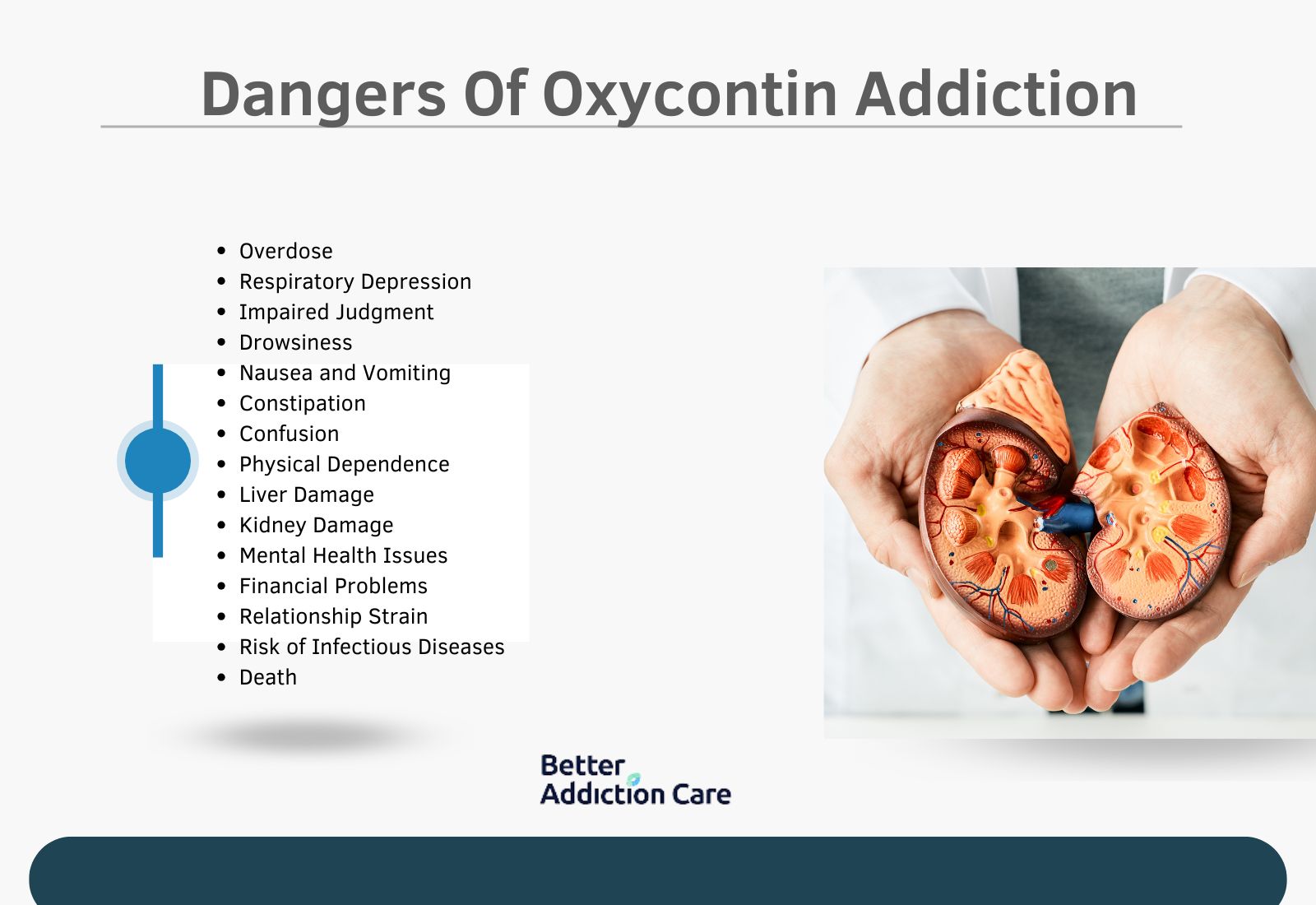
The risks of OxyContin addiction are explained below:
-
Overdose: Overdose occurs when excessive OxyContin intake suppresses vital functions, leading to unconsciousness, respiratory failure, or death. This is a critical short-term risk. According to the CDC (2019), prescription opioids, including OxyContin, were involved in over 14,000 overdose deaths in the U.S..
-
Respiratory Depression: OxyContin slows breathing, and in high doses, it halts it entirely, leading to oxygen deprivation and death. This is a short-term and potentially fatal risk during misuse or overdose.
-
Impaired Judgment: Cognitive impairment from OxyContin use leads to risky behaviors, including unsafe driving, neglect of responsibilities, or criminal activity. This is a short-term psychological effect that has long-term consequences.
-
Drowsiness: OxyContin’s sedative effects cause extreme sleepiness, impacting daily functioning. This is a short-term risk but leads to long-term issues like job loss and reduced productivity.
-
Nausea and Vomiting: Common short-term physical effects caused by OxyContin’s interaction with the digestive system. These symptoms also occur during withdrawal.
-
Constipation: A persistent long-term physical side effect due to OxyContin’s suppression of gastrointestinal motility. Chronic constipation leads to severe health complications like bowel obstruction.
-
Confusion: OxyContin disrupts cognitive clarity, resulting in disorientation and memory problems. This psychological effect is either short-term during intoxication or long-term with chronic misuse.
-
Physical Dependence: Prolonged use rewires the brain’s reward system, making the body reliant on OxyContin to function normally. This is a long-term danger that sustains addiction and complicates recovery.
-
Liver Damage: Chronic OxyContin misuse harms the liver, particularly when combined with other substances like alcohol or acetaminophen. This long-term physical risk develops unnoticed until significant damage occurs.
-
Kidney Damage: OxyContin impacts kidney function over time, especially in those with pre-existing conditions. This long-term physical harm increases the risk of renal failure.
-
Mental Health Issues: Depression, anxiety, and emotional instability develop or worsen with prolonged OxyContin use. These long-term psychological risks increase the likelihood of self-harm or suicide.
-
Financial Problems: Addiction leads to job loss and debt due to the high costs of obtaining OxyContin illicitly. This is a long-term social and economic impact of addiction.
-
Relationship Strain: Addiction erodes trust and stability in personal relationships, leading to isolation or familial estrangement. This is a long-term social consequence.
-
Risk of Infectious Diseases: Injecting OxyContin increases the risk of HIV, hepatitis, and other infections due to needle sharing. This is a long-term danger primarily associated with misuse of methods.
-
Death: The ultimate risk of prolonged OxyContin addiction, resulting from overdose or complications like respiratory failure. This fatal consequence is both a short-term and long-term risk.
What Are The Risks Of Mixing Oxycontin With Other Substances?
The risks of mixing oxycontin with other substances include life-threatening complications like overdose, respiratory depression, and death. Combining OxyContin with depressants like alcohol, benzodiazepines, or other opioids amplifies their sedative effects, impairing vital functions and overwhelming the central nervous system.
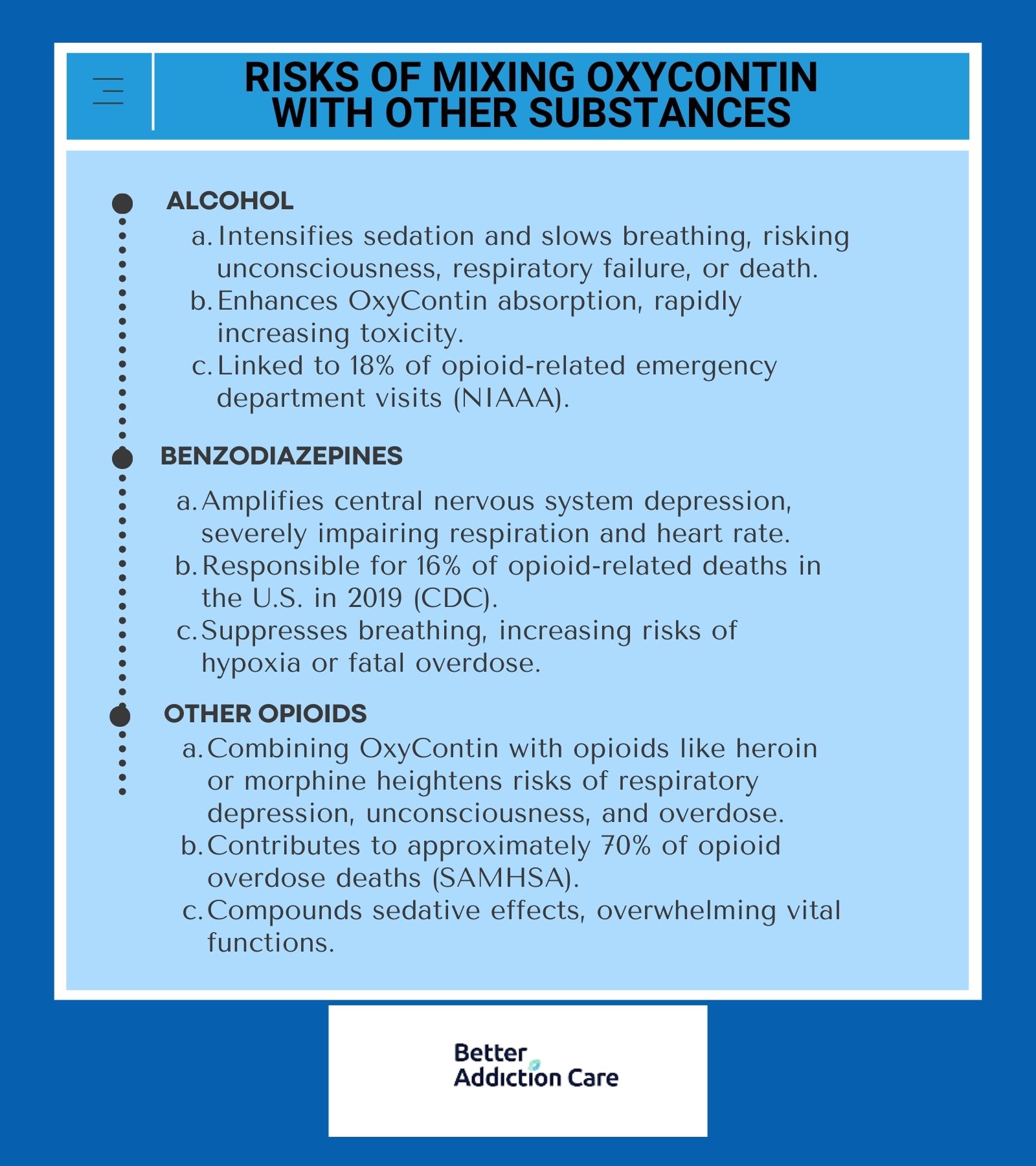
The risks of mixing oxyContin with other substances are explained below:
-
Alcohol: Alcohol combined with OxyContin intensifies sedation and slows breathing, which leads to unconsciousness, respiratory failure, and death. According to the National Institute on Alcohol Abuse and Alcoholism, approximately 18% of opioid-related emergency department visits involve alcohol use. Alcohol also increases the absorption of OxyContin, delivering higher doses more rapidly, further increasing toxicity levels.
-
Benzodiazepines: Mixing benzodiazepines (such as Xanax or Valium) with OxyContin amplifies central nervous system depression, severely impairing respiration and heart rate. The CDC reports that in 2019, benzodiazepines were involved in 16% of opioid-related deaths in the U.S., showing the dangers of this combination. This mix is particularly deadly as both substances suppress breathing, leading to hypoxia or fatal overdose.
-
Opioids: Using multiple opioids, like heroin or morphine, with OxyContin dramatically increases the risk of respiratory depression, unconsciousness, and overdose. According to SAMHSA (2020), approximately 70% of opioid overdose deaths involve the use of more than one opioid. This practice compounds the sedative effects, overwhelming the body’s ability to sustain vital functions.
How Is Oxycontin Addiction Diagnosed?
OxyContin addiction is diagnosed by assessing a patient’s behavior, physical symptoms, and medical history to determine patterns of misuse. Healthcare providers like psychiatrists use criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), which outlines substance use disorder as exhibiting at least two of eleven symptoms, such as cravings, inability to control use, and continued use despite negative consequences.
Diagnosis begins with a thorough patient interview to evaluate their history of OxyContin use, frequency, and dose. Healthcare providers also conduct physical exams to identify signs of addiction, such as withdrawal symptoms, tolerance buildup, and signs of respiratory or gastrointestinal complications.
Additional oxycontin diagnostic tools include urine toxicology screens to confirm the presence of OxyContin or other substances in the system. Self-assessment questionnaires like the Opioid Risk Tool (ORT) are also commonly used to identify individuals at risk of developing addiction based on their medical history and behavioral patterns.
What Are The Treatment Options For Oxycontin Addiction?
The treatment options for OxyContin addiction include medical detoxification, medication-assisted therapy (MAT), behavioral counseling, and support programs. These approaches address both the physical dependence and the psychological aspects of addiction, promoting long-term recovery and relapse prevention.
The treatment options for oxycontin addiction are explained below:
Medical Detoxification
Medical detoxification is a supervised process aimed at managing the acute physical symptoms of OxyContin withdrawal. This treatment uses medications like Clonidine or Methadone to reduce withdrawal symptoms such as nausea, anxiety, and muscle pain.
According to a study by Coplan et al. titled "The Effect of an Abuse-Deterrent Opioid Formulation on Addiction," published in Clinical Pharmacology and Therapeutics (2016), detoxification is essential for stabilizing patients during the critical withdrawal period.
Recovery typically takes 5 to 10 days, depending on the severity of the addiction, but it does not address the psychological components, requiring follow-up care for sustained recovery.
Cognitive Behavioral Therapy (CBT)
CBT is a structured psychotherapy that addresses the thought patterns and behaviors driving OxyContin addiction. It helps individuals identify triggers and develop healthier coping mechanisms. Initial therapy spans 12 to 16 weeks, with the benefits extending over time. While effective, CBT requires consistent participation and a commitment to long-term behavioral change.
Medication-Assisted Treatment (MAT)
MAT integrates FDA-approved medications like Buprenorphine, Methadone, and Naltrexone with counseling to treat both the physical and psychological aspects of OxyContin addiction. These medications alleviate cravings and withdrawal symptoms while blocking the euphoric effects of opioids.
According to the National Institute on Drug Abuse (2020), MAT reduces opioid misuse by 50% and improves treatment retention rates. Recovery duration varies, spanning several months to years, but MAT’s reliance on long-term medication use raises concerns about dependency.
Support Groups
Support groups like Narcotics Anonymous (NA) provide peer-led platforms for individuals to share experiences and gain emotional support. These groups are instrumental in building accountability and a sense of community, which are vital for maintaining sobriety.
Research by SAMHSA (2020) shows that individuals participating in peer support programs show significantly higher recovery rates compared to those who do not. While support groups are valuable, they rely heavily on an individual’s willingness to participate actively, and the outcomes vary depending on personal engagement.
Inpatient Treatment
Inpatient treatment involves living in a residential facility where individuals receive 24/7 care, combining detoxification, therapy, and skill-building.
According to a study by Sproule et al., titled "Changing Patterns in Opioid Addiction," published in the Canadian Family Physician (2009), inpatient treatment offers a distraction-free environment conducive to recovery, particularly for severe cases of addiction.
Recovery programs typically last 30 to 90 days, but the high cost and time commitment is a barriers for some individuals.
12-Step Programs
12-step programs, such as those used by Narcotics Anonymous, focus on spirituality, self-reflection, and community support. Participants work through structured steps aimed at maintaining sobriety and rebuilding their lives.
According to a 2020 SAMHSA report, 12-step programs have helped millions worldwide achieve and sustain recovery, mainly through their focus on peer support and accountability.
While highly structured, the spiritual framework only resonates with some, and its success depends on personal belief systems and consistent involvement.
What Is Oxycontin Withdrawal?
OxyContin withdrawal refers to the physical and psychological symptoms that occur when someone dependent on the drug abruptly reduces or stops its use. These symptoms arise because the body, having adjusted to OxyContin’s effects over time, struggles to regain equilibrium in the absence of the drug. Withdrawal reflects the central nervous system's attempt to recover from the suppressive effects of prolonged opioid use.
Common oxycontin withdrawal symptoms include nausea, vomiting, muscle aches, anxiety, sweating, insomnia, and intense cravings. According to the National Institute on Drug Abuse (NIDA, 2020), withdrawal symptoms begin as early as 12 hours after the last dose, peak within 48 to 72 hours, and gradually subside over 7 to 10 days.
The intensity of withdrawal depends on factors such as the duration of use, dosage, and individual health status.
Managing oxycontin withdrawal requires medical supervision to ensure safety and minimize discomfort. Without professional intervention, the severity of symptoms compels individuals to relapse in an attempt to alleviate distress, prolonging the cycle of addiction.
What Is The Withdrawal Timeline For Oxycontin?
The withdrawal timeline for OxyContin occurs in distinct phases, reflecting the body’s gradual adaptation to the absence of the drug. Symptoms begin within hours of the last dose, intensify during the peak phase, and gradually subside over the following days.
Protracted withdrawal symptoms, known as Post-Acute Withdrawal Syndrome (PAWS), persist for weeks or months, depending on the severity of addiction.
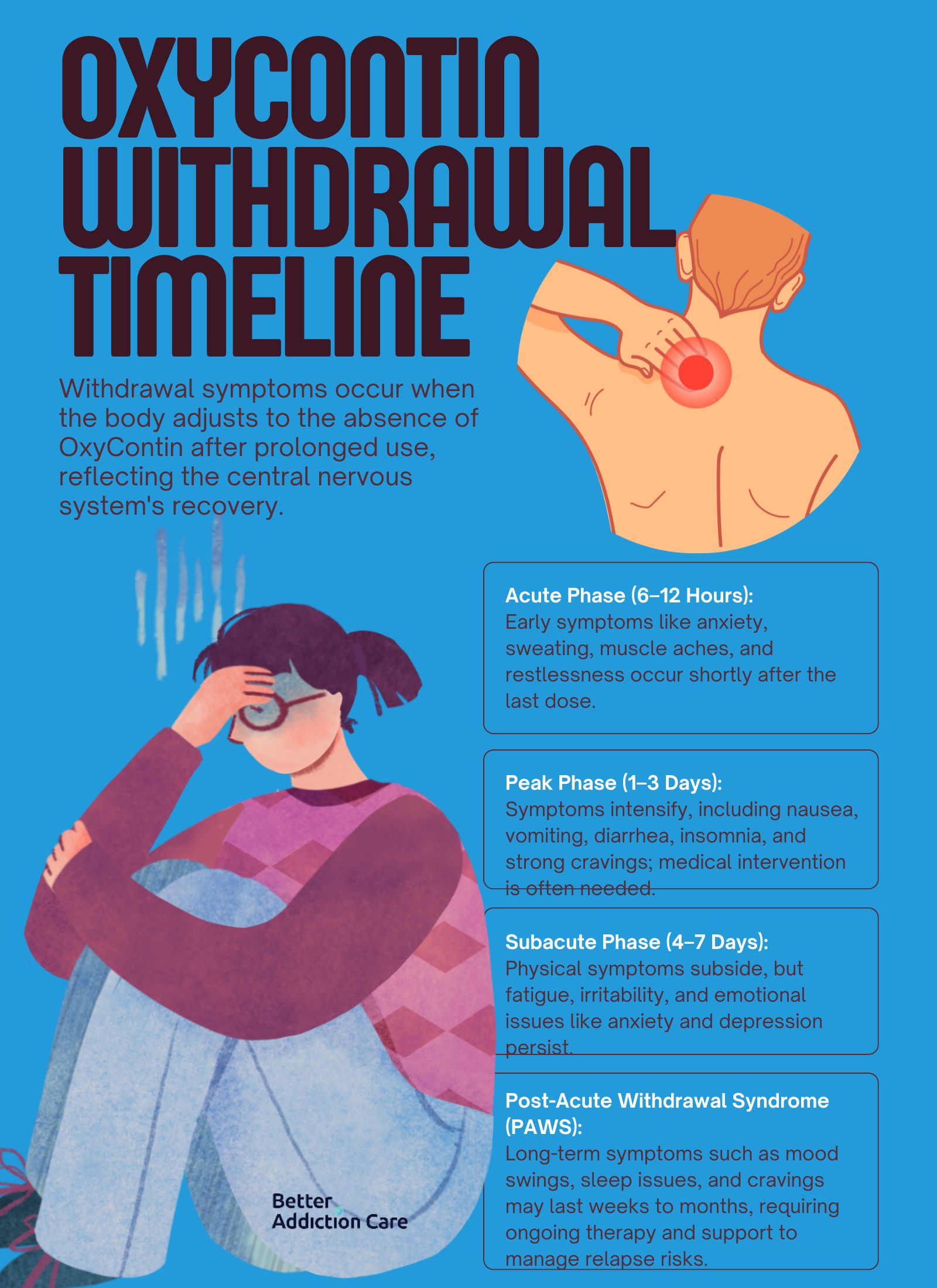
The withdrawal timeline for oxycontin is explained below:
-
Acute Phase (6–12 Hours): This phase begins shortly after the last dose. Symptoms include anxiety, sweating, yawning, muscle aches, and restlessness. These symptoms are early indicators of the body’s reaction to the absence of OxyContin.
-
Peak Phase (1–3 Days): During the peak phase, symptoms are at their most intense. Individuals experience nausea, vomiting, diarrhea, insomnia, and severe cravings. This is the most challenging phase to endure without medical intervention.
-
Subacute Phase (4–7 Days): Symptoms begin to subside but still include fatigue, irritability, and gastrointestinal discomfort. Emotional symptoms like anxiety and depression emerge as the body continues to recover.
-
Post-Acute Withdrawal Syndrome (PAWS): PAWS persists for weeks or even months after the acute withdrawal phases. Symptoms include mood swings, sleep disturbances, and persistent cravings. According to the National Institute on Drug Abuse (NIDA), PAWS is a major contributor to relapse and requires long-term management through therapy and support.
What Are The Withdrawal Symptoms Of Oxycontin?
The withdrawal symptoms of OxyContin encompass a wide range of physical and psychological effects, such as anxiety, restlessness, sweating, insomnia, and diarrhea, caused by the body’s dependence on the drug.
OxyContin interacts with opioid receptors in the brain, suppressing pain and creating a sense of euphoria. When use stops abruptly, the brain and body struggle to restore balance, leading to severe withdrawal symptoms.

The withdrawal symptoms of oxycontin include:
-
Anxiety: Anxiety arises because OxyContin disrupts the production of natural calming neurotransmitters like gamma-aminobutyric acid (GABA). Without the drug, the brain becomes hyperactive, resulting in heightened stress. According to the National Institute on Drug Abuse (NIDA, 2020), anxiety is one of the earliest and most persistent symptoms of opioid withdrawal.
-
Restlessness: Restlessness occurs as the nervous system becomes overstimulated in the absence of OxyContin's depressant effects. This symptom reflects the brain's overcompensation during withdrawal.
-
Muscle Aches: Muscle pain is a result of the body’s pain regulation system attempting to function without OxyContin. Opioids suppress pain perception, and withdrawal leads to a rebound effect where normal pain thresholds are heightened.
-
Sweating: The autonomic nervous system becomes hyperactive during withdrawal, causing excessive sweating as the body works to expel toxins and regulate its temperature. Sweating is accompanied by chills and fever-like sensations, as noted in the CDC report on opioid addiction and withdrawal complications.
-
Nausea and Vomiting: These symptoms occur because OxyContin disrupts the gastrointestinal tract’s natural motility. During withdrawal, this system becomes overactive, leading to nausea and frequent vomiting. The CDC highlights gastrointestinal symptoms as common and debilitating during the peak of opioid withdrawal.
-
Diarrhea: Similar to nausea, diarrhea results from the gut's hyperactivity when OxyContin's constipating effects are removed. This leads to dehydration if not managed properly.
-
Insomnia: Opioid withdrawal disrupts sleep patterns by increasing anxiety, restlessness, and physical discomfort. Insomnia often persists for several days, compounding other withdrawal symptoms and delaying recovery.
-
Irritability and Depression: OxyContin withdrawal significantly affects mood as the brain struggles to restore natural dopamine and serotonin levels. According to the National Institute on Drug Abuse (NIDA, 2020), depression and irritability are common, lasting beyond the acute withdrawal phase in many cases.
-
Dilated Pupils and Rapid Heartbeat: The autonomic nervous system, which controls involuntary functions like pupil size and heart rate, becomes overstimulated, leading to noticeable physical changes.
-
High Blood Pressure: The stress and agitation caused by withdrawal increase blood pressure levels. This symptom poses a serious risk, especially for individuals with pre-existing cardiovascular conditions.
-
Cravings: Intense cravings for OxyContin occur because the brain has become dependent on the drug for dopamine release. These cravings drive compulsive behavior and significantly increase the risk of relapse.
-
Fatigue and Tremors: Fatigue is caused by the physical and emotional strain of withdrawal, while tremors result from nervous system dysregulation during detoxification.
-
Chills and Runny Nose: These flu-like symptoms reflect the body’s attempt to restore equilibrium during the early stages of withdrawal. A runny nose and chills are particularly common during the first 24 to 48 hours.
-
Yawning: This seemingly minor symptom is a common response to nervous system overactivation and is often seen during the acute phase of opioid withdrawal.
How Is Oxycontin Consumed?
OxyContin is consumed in various ways, such as swallowing, snorting, chewing, smoking, and injecting, depending on whether it is used as prescribed or misused.
The most common method is swallowing the tablet whole, as intended for pain management. When taken this way, the drug’s controlled-release formulation provides extended pain relief over 12 hours.
In cases of misuse, individuals crush OxyContin tablets to snort the powder, bypassing the time-release mechanism and achieving an immediate euphoric effect. Others dissolve the crushed tablets in water and inject the solution directly into the bloodstream, leading to a rapid and intensified impact.
Chewing the tablets is another method that disrupts the controlled-release mechanism, delivering a concentrated dose quickly. Some individuals even smoke the crushed powder, further enhancing its effects by inhaling the drug into the lungs.
These alternative consumption methods dramatically increase the risk of addiction, overdose, and severe health complications, as they deliver higher doses of the drug to the body than intended. Misusing OxyContin in these ways bypasses the drug’s safety mechanisms and amplifies its dangerous effects on the central nervous system.
Does Oxycontin Get You High?
Yes, OxyContin gets you high when it is misused. When taken as prescribed, OxyContin releases oxycodone slowly over time, providing consistent pain relief without significant euphoric effects.
However, misuse delivers a large dose of oxycodone into the bloodstream all at once. This leads to an intense euphoria, described as a "high." The euphoric effect occurs because OxyContin stimulates the brain’s opioid receptors, releasing large amounts of dopamine, the neurotransmitter associated with pleasure and reward.
According to the National Institute on Drug Abuse (NIDA, 2020), this surge in dopamine not only creates the high but also reinforces drug-taking behavior, making misuse highly addictive.
How Long Does Oxycontin Stay In Your System?
OxyContin stays in your system for 24 hours to 90 days, depending on the biological sample tested, dosage taken, frequency of use, metabolism rate, and overall health of the individual. Due to its relatively short plasma half-life of 3 to 4.5 hours, it can be detected in blood up to 24 hours after the last dose.
OxyContin is detected in urine for up to 3 to 4 days as the kidneys process and eliminate the drug. Hair tests detect it for up to 90 days or longer, as traces of the drug become embedded in the hair follicles over time.
According to the National Institute on Drug Abuse (NIDA), opioid detection timelines are influenced by the type of test used and whether the drug was misused or taken as prescribed.
Can Oxycontin Misuse Lead To Overdose?
Yes, OxyContin misuse leads to overdose. Overdose occurs when excessive amounts of the drug overwhelm the central nervous system, causing life-threatening symptoms such as severe respiratory depression, unconsciousness, and cardiac arrest.
Misused consumption methods bypass the drug's controlled-release mechanism, delivering a dangerously high dose to the body all at once.
According to the Centers for Disease Control and Prevention (CDC), there were 14,139 deaths involving prescription opioids like OxyContin in 2019, accounting for nearly one-third of all opioid overdose deaths that year.
Overdose risk is particularly high when OxyContin is combined with other depressants like alcohol or benzodiazepines, as these substances increase their effects on the respiratory system.
What Are Oxycontin Overdose Symptoms?
OxyContin overdose symptoms include shallow breathing, blue lips, drowsiness, shallow breathing, weak pulse, nausea, and seizures. These symptoms occur when the drug is taken in excessive quantities, overwhelming the body’s ability to process it. Symptoms escalate quickly, requiring immediate medical intervention.
Symptoms of OxyContin overdose include:

-
Slow or shallow breathing
-
Unresponsiveness or unconsciousness
-
Blue lips or fingertips
-
Extreme drowsiness
-
Pinpoint pupils
-
Weak pulse
-
Cold or clammy skin
-
Nausea or vomiting
-
Seizures
According to the National Institute on Drug Abuse (NIDA), recognizing these symptoms early and administering interventions like naloxone can save lives.
Is Oxycontin Stronger Than Oxycodone?
No, OxyContin is not stronger than oxycodone. Both medications contain the same active ingredient, oxycodone, and have the same potency in terms of milligram strength. The primary difference lies in their formulations.
OxyContin is a controlled-release version of oxycodone designed to provide extended pain relief over 12 hours. In contrast, regular oxycodone is an immediate-release medication that delivers effects more quickly but requires more frequent dosing.
The controlled-release formulation of OxyContin creates the perception of greater strength because misusing the drug (e.g., crushing and snorting it) allows the entire dose to enter the bloodstream at once.
How Is Oxycontin Different From Percocet?
Yes, OxyContin is different from Percocet, though both contain the opioid oxycodone. OxyContin is a brand-name medication that contains only oxycodone in a controlled-release form, providing extended pain relief for up to 12 hours.
In contrast, Percocet combines oxycodone with acetaminophen, an over-the-counter pain reliever, and is formulated for immediate release, offering shorter-term pain relief.
These differences affect how the medications are prescribed. OxyContin is used for managing chronic, severe pain, while Percocet is prescribed for acute, moderate-to-severe pain. The acetaminophen content in Percocet also presents additional risks, such as liver damage, especially when taken in high doses or with alcohol.
According to the National Institute on Drug Abuse (NIDA), medications like Percocet contribute to the widespread misuse of prescription opioids, with nearly 9.3 million people in the U.S. misusing prescription pain relievers in 2020
Is Mixing Oxycontin And Alcohol Dangerous?
Yes, mixing OxyContin and alcohol is extremely dangerous. Both substances are central nervous system depressants, and their combined effects significantly increase the risk of respiratory depression, unconsciousness, and death. Alcohol enhances the sedative properties of OxyContin, leading to greater suppression of vital functions like breathing and heart rate.
This combination is a leading cause of fatal overdoses. According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), approximately 18% of emergency department visits involving prescription opioids also involve alcohol misuse.
Is Oxycontin Legal?
Yes, OxyContin is legal when prescribed by a licensed healthcare provider for legitimate medical use. It is classified as a Schedule II controlled substance under the U.S. Controlled Substances Act, meaning it is approved for medical use. Still, it has a high potential for abuse and dependence.
The U.S. Food and Drug Administration (FDA) regulates OxyContin as a prescription medication primarily intended for managing severe, chronic pain that requires long-term opioid treatment. However, its legal status is limited to appropriate medical use, and any misuse—such as taking it without a prescription, in larger doses, or through methods like snorting or injecting—constitutes illegal activity.
What Does Oxycontin Look Like?
Oxycontin looks like a round or oval tablet in various colors, depending on the dosage strength. The tablets are imprinted with specific markings that identify the brand and dosage, such as "OC" or "OP" on one side and the milligram dosage (e.g., 10, 20, 40, 80) on the other.
The colors of the 10 mg tablets vary by dosage: 10 mg tablets are white, 20 mg pink, 40 mg yellow, and 80 mg green. These visual differences help patients and healthcare providers easily distinguish between strengths.
Counterfeit OxyContin tablets, sold illegally, mimic the appearance of the genuine product but contain dangerous substances like fentanyl, increasing the risk of overdose. The U.S. Drug Enforcement Administration (DEA) has issued warnings about these counterfeit pills, which contribute to the growing opioid crisis.
Is Oxycontin An Opioid?
Yes, OxyContin is an opioid. It contains oxycodone, a synthetic opioid that binds to the brain’s opioid receptors to alleviate moderate to severe pain. Classified as a Schedule II controlled substance, OxyContin is highly effective for pain management but carries a significant risk of addiction and misuse.
Opioid use and addiction have reached epidemic levels in the United States. According to the National Institute on Drug Abuse (NIDA), over 2 million Americans suffered from opioid use disorder in 2020, and prescription opioids like OxyContin contributed to nearly 14,000 deaths from opioid overdoses in 2019.
What Is The Chemical Composition Of Oxycontin?
OxyContin's chemical composition is centered around its active ingredient, oxycodone hydrochloride, a semi-synthetic opioid derived from thebaine, an alkaloid found in the opium poppy.
Inactive ingredients include excipients such as lactose, magnesium stearate, and hypromellose, which contribute to the controlled-release formulation. This design allows the drug to deliver oxycodone steadily over 12 hours.
What Is The Typical Dosage Of Oxycontin?
The typical dosage of OxyContin depends on the patient's pain severity, medical history, and opioid tolerance. For opioid-naïve patients, the starting dose is generally 10 mg every 12 hours.
For patients already using opioids, dosages range from 20 mg to 80 mg every 12 hours, with adjustments made based on the patient’s response and tolerance.
The U.S. Food and Drug Administration (FDA) states that dosages above 80 mg are only prescribed for opioid-tolerant patients due to the heightened risk of life-threatening respiratory depression.
Related Articles
Treatment Centers in Virginia









