Cognitive Behavioral Therapy (CBT): Definition, Application, Types, Process, Risks and Benefits
Cognitive Behavioral Therapy (CBT) focuses on identifying and modifying the thought patterns and behaviors that lead to and sustain addictive behavior. It emphasizes active participation, practical skill development, and consistent practice through a structured form of therapy led by trained therapists.

Cognitive Behavioral Therapy (CBT) focuses on identifying and modifying the thought patterns and behaviors that lead to and sustain addictive behavior. It emphasizes active participation, practical skill development, and consistent practice through a structured form of therapy led by trained therapists.
CBT is primarily applied in addiction treatment to help patients recognize triggers, build emotional regulation, and develop long-term coping strategies to manage cravings and avoid relapse. According to the National Institute on Drug Abuse in 2020, CBT, when combined with other interventions, increases treatment retention and reduces substance use by over 40%.
The types of CBT used in addiction treatment include Cognitive Therapy, Exposure Therapy, Dialectical Behavior Therapy (DBT), Acceptance and Commitment Therapy (ACT), and Mindfulness-Based Cognitive Therapy (MBCT).
The CBT process involves ten structured steps: assessment and goal setting, identifying negative thought patterns, recognizing behavioral triggers, cognitive restructuring, developing coping strategies, behavioral activation, problem-solving, emotional regulation, applying skills in daily life, and reviewing progress.
CBT limitations include requiring high motivation, not addressing deep trauma alone, and being less effective without support or in cases of cognitive impairment. A study by the Substance Abuse and Mental Health Services Administration (SAMHSA) in 2021 notes that CBT must be paired with other therapies or medication to treat complex cases of addiction.
The benefits of CBT in addiction treatment include improved self-control, reduced relapse risk, better stress management, and enhanced ability to avoid triggering situations. The National Institute of Mental Health in 2022 confirms that CBT offers significant improvements in 70–80% of patients with co-occurring addiction and mental health disorders.
What Is Cognitive Behavioral Therapy (CBT)?
Cognitive Behavioral Therapy (CBT) is a structured form of psychotherapy that helps individuals recognize, challenge, and modify negative thought patterns and behaviors. It is grounded in the concept that psychological distress is largely influenced by cognitive distortions, faulty or unhelpful ways of thinking, and that by identifying and restructuring these thoughts, patients improve their emotional regulation and develop healthier coping mechanisms.
CBT was developed by Dr. Aaron T. Beck in the 1960s while he was conducting research on depression at the University of Pennsylvania. Unlike traditional approaches that focus extensively on past experiences, CBT is action-oriented and present-focused, requiring patients to participate actively in their own recovery through practical exercises, journaling, and sharing experiences during sessions with therapists.
What sets CBT apart from other therapeutic approaches is its collaborative and solution-focused structure, where the therapist and patient work together to set goals and implement evidence-based techniques.
According to a study by the National Institute of Mental Health (NIMH) titled "Cognitive Behavioral Therapy: An Evidence-Based Practice" (2022), CBT has been shown to reduce symptoms in 60–80% of patients with anxiety and depression after short-term treatment, making it one of the most effective forms of psychotherapy available today.
How Is Cognitive Behavioral Therapy Applied in Addiction Treatment?
Cognitive Behavioral Therapy is applied in addiction treatment by helping patients identify the triggers, thought patterns, and behaviors that lead to substance use, and replacing them with healthier coping strategies.
CBT teaches patients how to avoid high-risk situations, manage cravings, and respond to stress without relying on drugs or alcohol. It promotes long-term recovery by focusing on behavioral change through self-monitoring, problem-solving, and cognitive restructuring.
This structured form of psychotherapy requires active participation from the patient, who works collaboratively with trained therapists to track progress and practice new behaviors. CBT is also widely integrated with other treatments, such as medication-assisted treatment (MAT), group therapy, and 12-step programs, enhancing its effectiveness.
According to a study by the National Institute on Drug Abuse (NIDA) titled "Principles of Drug Addiction Treatment" in 2020), combining CBT with MAT improves abstinence rates by over 40%, especially in patients with opioid and alcohol use disorders. By sharing experiences and learning practical skills, individuals develop a toolkit for relapse prevention and long-term sobriety.
What Are the Types of Cognitive Behavioral Therapy?
The types of Cognitive Behavioral Therapy are Dialectical Behavior Therapy (DBT), Rational Emotive Behavior Therapy (REBT), Mindfulness-Based Cognitive Therapy (MBCT), and Acceptance and Commitment Therapy (ACT).
Each type focuses on different aspects of thought and behavior. DBT emphasizes emotional regulation and distress tolerance. All forms require active participation and are led by trained therapists in a structured form of psychotherapy.

The types of cognitive behavioral therapy are explained below:
Cognitive Therapy (CT)
Cognitive Therapy focuses on identifying and correcting distorted thinking patterns that contribute to mental health issues such as depression, anxiety, and low self-worth. Patients participate in sessions with therapists to examine the validity of their thoughts and develop more balanced thinking.
According to a study by the National Institute of Mental Health (2022), CT reduces depressive symptoms by 60–70% in patients with mild to moderate depression, particularly when used as part of a comprehensive psychotherapy plan.
Exposure Therapy
Exposure Therapy is primarily used to treat anxiety disorders and post-traumatic stress by gradually exposing patients to feared stimuli in a safe environment. This technique helps reduce avoidance behaviors and supports long-term recovery by preventing relapse.
Therapists guide patients through a structured form of confrontation that allows them to develop healthier responses to triggers. According to a study by the American Psychological Association (2021), 90% of individuals with phobias reported symptom reduction after consistent participation in exposure-based CBT.
Dialectical Behavior Therapy (DBT)
Dialectical Behavior Therapy is a specialized CBT form designed for patients who struggle with intense emotions, suicidal ideation, and borderline personality disorder (BPD). DBT combines acceptance and change strategies to help individuals build distress tolerance, improve relationships, and regulate mood.
According to a study by Linehan et al., published in the Archives of General Psychiatry (2006), DBT led to a 50% reduction in self-harm behaviors among individuals diagnosed with BPD after one year of treatment.
Acceptance and Commitment Therapy (ACT)
Acceptance and Commitment Therapy helps patients acknowledge difficult emotions and thoughts without judgment while committing to behavior aligned with their values. ACT is particularly effective in treating anxiety, addiction, and chronic pain.
Patients are encouraged to accept discomfort and focus on action rather than avoidance. According to a study by Hayes et al., titled "Acceptance and Commitment Therapy: Model, Processes, and Outcomes," published in Behaviour Research and Therapy (2006), ACT improves long-term functioning and reduces relapse risk by increasing psychological flexibility.
Mindfulness-Based Cognitive Therapy (MBCT)
Mindfulness-Based Cognitive Therapy integrates traditional CBT techniques with mindfulness practices to prevent relapse in patients with recurrent depression. It teaches patients to become more aware of negative thinking patterns and disengage from automatic reactions.
MBCT emphasizes sharing experiences in group settings led by trained therapists. According to a study by the National Institute for Health and Care Excellence (NICE) (2019), MBCT reduces the risk of depressive relapse by 43% among patients with three or more previous episodes.
What Is the Process During CBT?
The process during CBT involves identifying negative thought patterns, challenging their validity, and replacing them with healthier alternatives through structured sessions led by therapists. Patients are encouraged to participate actively by completing exercises, sharing experiences, and practicing skills between sessions, creating a consistent and goal-oriented psychotherapy experience.
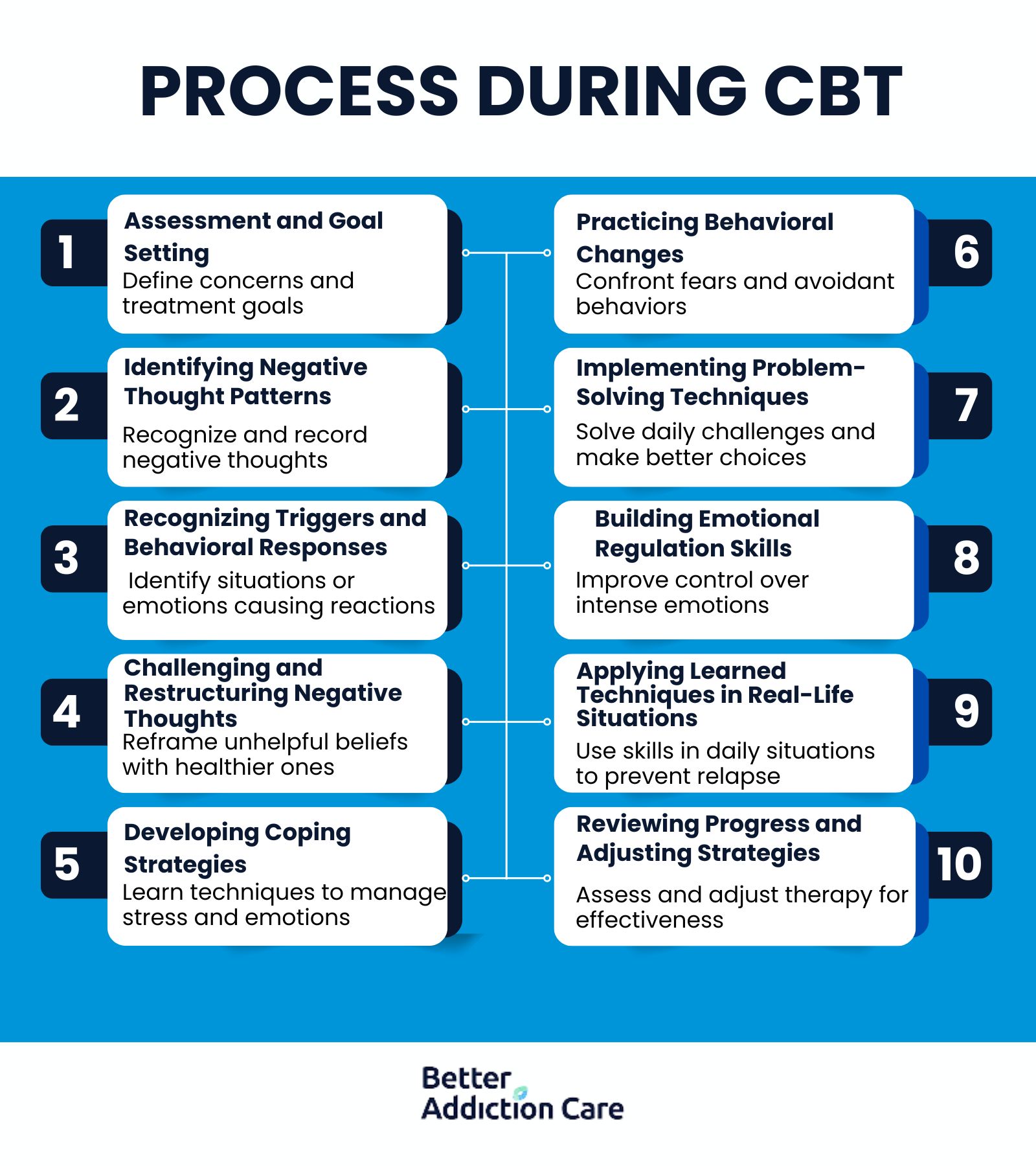
The process during CBT is explained below:
-
Assessment and goal setting: The CBT process begins with an in-depth assessment where the therapist and patient discuss current concerns, history, and symptoms. Together, they define clear and measurable treatment goals to guide therapy. This structured form of psychotherapy ensures sessions remain focused and outcome-driven.
-
Identifying negative thought patterns: Patients learn to observe automatic thoughts that contribute to distress and dysfunctional behavior. These patterns are recorded and discussed during sessions. This stage encourages sharing experiences and becoming more aware of internal dialogue.
-
Recognizing triggers and behavioral responses: Patients identify the external situations or emotional states that lead to unhelpful reactions. They work with therapists to trace connections between triggers and behavioral responses. This helps clarify the root of emotional and behavioral issues, such as intense emotions or cravings.
-
Challenging and restructuring negative thoughts: Therapists teach patients to evaluate the evidence behind their beliefs and consider alternative, balanced perspectives. This cognitive restructuring helps break patterns contributing to depression, anxiety, and relapse. The process promotes healthier thinking through repeated practice.
-
Developing coping strategies: CBT equips individuals with tools to handle stress, cravings, and emotional distress. Techniques such as relaxation training, thought-stopping, and distraction are commonly introduced. Patients participate by applying these methods between sessions.
-
Practicing behavioral changes: Behavioral activation and exposure techniques help patients gradually face avoided tasks or feared situations. Rehearsing new behaviors in a safe environment builds confidence and resilience. These activities are part of CBT’s action-oriented design.
-
Implementing problem-solving techniques: Patients are taught structured problem-solving steps to handle daily challenges. These include defining the issue, brainstorming solutions, and evaluating outcomes. The approach increases self-efficacy and decreases impulsive or emotional decisions.
-
Building emotional regulation skills: CBT integrates emotional awareness, labeling, and reframing exercises to manage intense emotions. This is especially useful for individuals with borderline personality disorder (BPD) or mood instability. Emotional regulation promotes stability and healthier relationships.
-
Applying learned techniques in real-life situations: As therapy progresses, patients are encouraged to use CBT skills in their daily routines. This includes managing triggers, avoiding high-risk environments, and maintaining structured thought practices. The application prevents relapse and supports long-term change.
-
Reviewing progress and adjusting strategies: Therapists and patients regularly assess goal achievement and therapy effectiveness. Techniques are adjusted based on outcomes and evolving needs. This ongoing review ensures CBT remains relevant and responsive throughout the treatment.
What Techniques Are Used in Cognitive Behavioral Therapy?
The techniques used in Cognitive Behavioral Therapy are cognitive restructuring, behavioral activation, exposure therapy, journaling, thought records, role-playing, and problem-solving. These activities involve challenging negative beliefs, practicing new behaviors, documenting thoughts and emotions, and simulating real-life situations in a safe environment with a therapist.
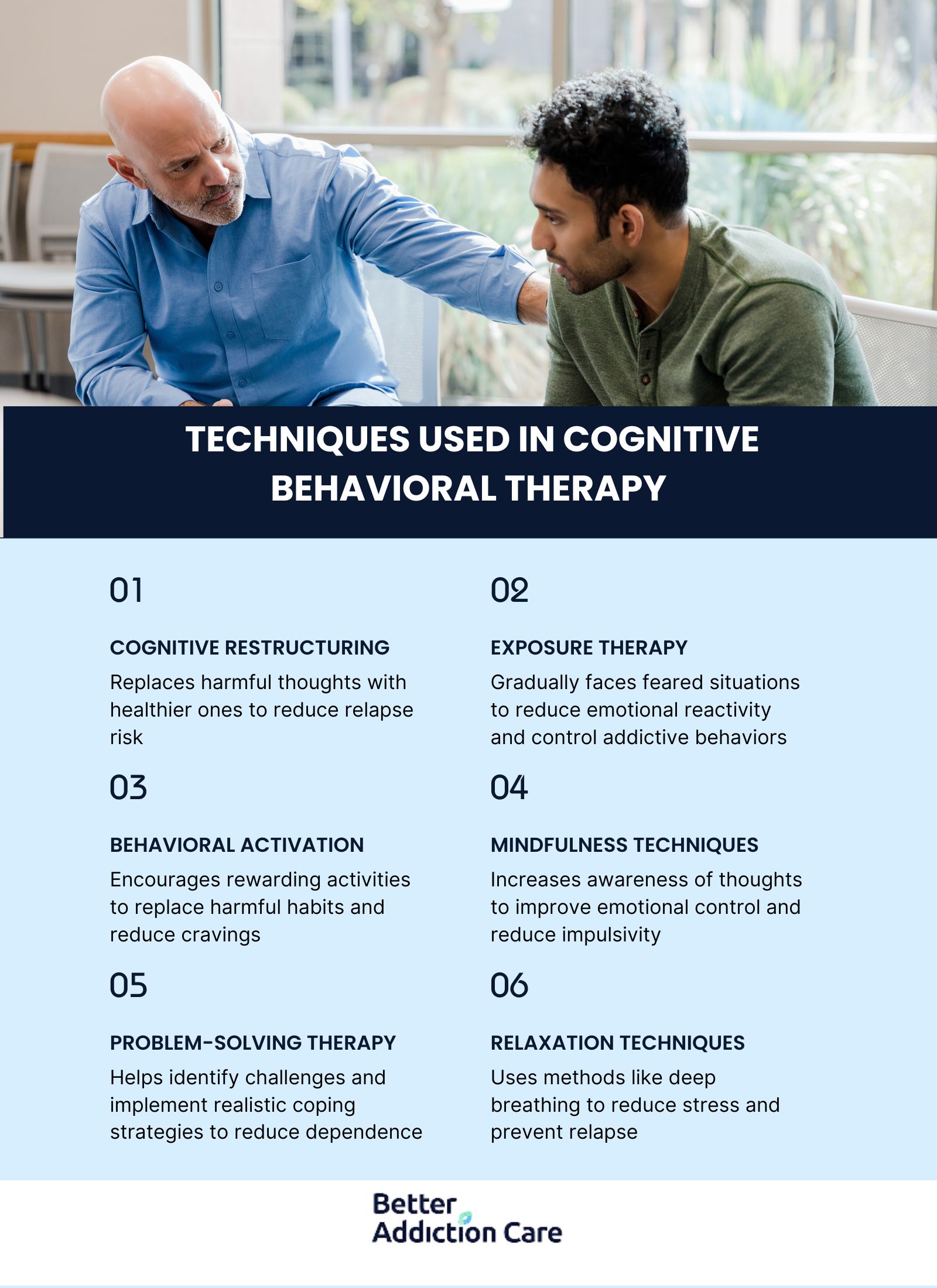
The techniques used in cognitive behavioral therapy are explained below:
-
Cognitive Restructuring (Reframing): This technique involves identifying distorted beliefs and questioning their accuracy to replace them with healthier thoughts. For example, a patient who believes, “I need alcohol to relax” is guided to challenge that belief and find alternative calming strategies. In addiction treatment, this helps individuals track thoughts that lead to addictive behavior and replace them with rational perspectives. According to a study by the National Institute on Drug Abuse (2020), cognitive restructuring significantly reduces relapse risk when patients recognize and modify harmful thinking patterns.
-
Exposure Therapy: Exposure therapy gradually introduces patients to feared environments or triggers in a controlled setting to reduce emotional reactivity. For instance, a person who fears social settings without using drugs is guided to face those situations while sober. This helps individuals develop confidence and emotional control, reducing the likelihood of addictive behavior as a coping mechanism.
-
Behavioral Activation: This approach encourages patients to engage in rewarding activities that align with their values, rather than avoiding them due to low motivation. For example, a recovering individual schedules regular exercise or hobbies instead of isolating, which helps overcome cravings tied to boredom or sadness. Behavioral activation replaces harmful habits with purposeful routines. A study by the National Institute of Mental Health (2017) shows that consistent activation reduces depressive symptoms, a major relapse trigger.
-
Mindfulness Techniques: Mindfulness teaches patients to observe their thoughts and feelings without judgment, improving emotional control and reducing impulsivity. For example, a person experiencing stress-related cravings learns to acknowledge the urge without acting on it. This awareness interrupts the automatic cycle of addictive behavior.
-
Problem-Solving Therapy: This technique involves identifying current challenges, brainstorming solutions, and evaluating outcomes logically. For instance, someone struggling with job stress leading to substance use is taught to define the problem and implement realistic coping strategies. This reduces dependency on substances by addressing root causes. A study by the Substance Abuse and Mental Health Services Administration (SAMHSA) in 2021 supports problem-solving as a critical skill for sustaining recovery.
-
Relaxation Techniques: Relaxation strategies such as deep breathing, progressive muscle relaxation, and guided imagery help reduce stress and anxiety that trigger addictive behavior. For example, a person with alcohol dependence practices deep breathing during moments of craving. These techniques help patients stay grounded and reduce emotional urges. According to a study by the National Center for Complementary and Integrative Health in 2020, relaxation methods improve emotional regulation and assist in relapse prevention.
What Are The Limitations of Cognitive Behavioral Therapy?
The limitations of cognitive behavioral therapy are its dependency on individual needs and reliance on patient effort. In addiction treatment, these limitations impact outcomes if patients face unresolved trauma, lack support systems, or experience cognitive barriers.
The limitations of cognitive behavioral therapy are explained below:
-
Requires active participation: CBT demands full involvement from the patient, including homework, sharing experiences, and practicing skills outside sessions. Individuals with low motivation or severe addiction find it difficult to participate consistently. Lack of engagement limits therapy effectiveness and slow progress.
-
Do not address deep-rooted trauma: CBT primarily targets current thought patterns and behaviors, but overlook underlying trauma. Patients with unresolved childhood abuse or complex PTSD require trauma-focused therapies. Without this, addictive behavior rooted in trauma persists despite surface-level improvements.
-
Not suitable for severe mental health conditions alone: For individuals with psychosis, severe bipolar disorder, or acute schizophrenia, CBT is not effective as a standalone approach. Such patients need medication and psychiatric stabilization first. CBT is a supplement but not the core treatment.
-
A structured approach does not fit everyone: CBT follows a structured form that feels rigid or impersonal to some patients. Creative or emotionally expressive individuals prefer more open-ended therapies. If the structure doesn’t align with their learning style, progress stagnates.
-
Emotionally challenging: CBT involves confronting distressing thoughts and habits, which initially intensify emotional discomfort. Discussing past failures, relapse events, or harmful beliefs evoke anxiety or shame. Patients need resilience and support to manage these reactions.
-
Results take time and consistency: CBT is not a quick fix—it requires regular sessions, consistent effort, and time to see lasting change. Individuals expecting fast results feel discouraged early in treatment. In addiction recovery, a lack of immediate improvement triggers relapse.
-
Limited effectiveness: Without social or familial backing, CBT is less successful in treating substance use disorders. Patients need reinforcement outside therapy to avoid triggers and sustain change. Lack of support systems has been linked to higher relapse rates.
-
Focuses on present issues rather than past experiences: CBT mainly targets current thought processes and doesn’t explore childhood experiences or unconscious motivations. Individuals seeking insight into their past feel the approach is shallow. In addiction recovery, neglecting historical context misses important relapse triggers.
-
Not always effective for individuals with cognitive impairments: Patients with dementia, intellectual disabilities, or brain injuries struggle to grasp CBT concepts. Tasks like tracking thoughts, analyzing beliefs, and questioning reasoning require cognitive functioning. In such cases, modified interventions or caregiver support is essential.
-
Relapse risk if coping strategies are not maintained: Even after completing CBT, patients face relapse if they stop applying learned strategies. Skills need long-term reinforcement to remain effective. Without ongoing practice or booster sessions, gains fade over time.
What Conditions Does CBT Treat?
The main conditions CBT treats are substance use disorders, behavioral addictions, anxiety/depression disorders, post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), bipolar disorder, and eating disorders. CBT’s focus on thought patterns, behavioral responses, and coping mechanisms makes it effective across a wide range of psychological and behavioral conditions.
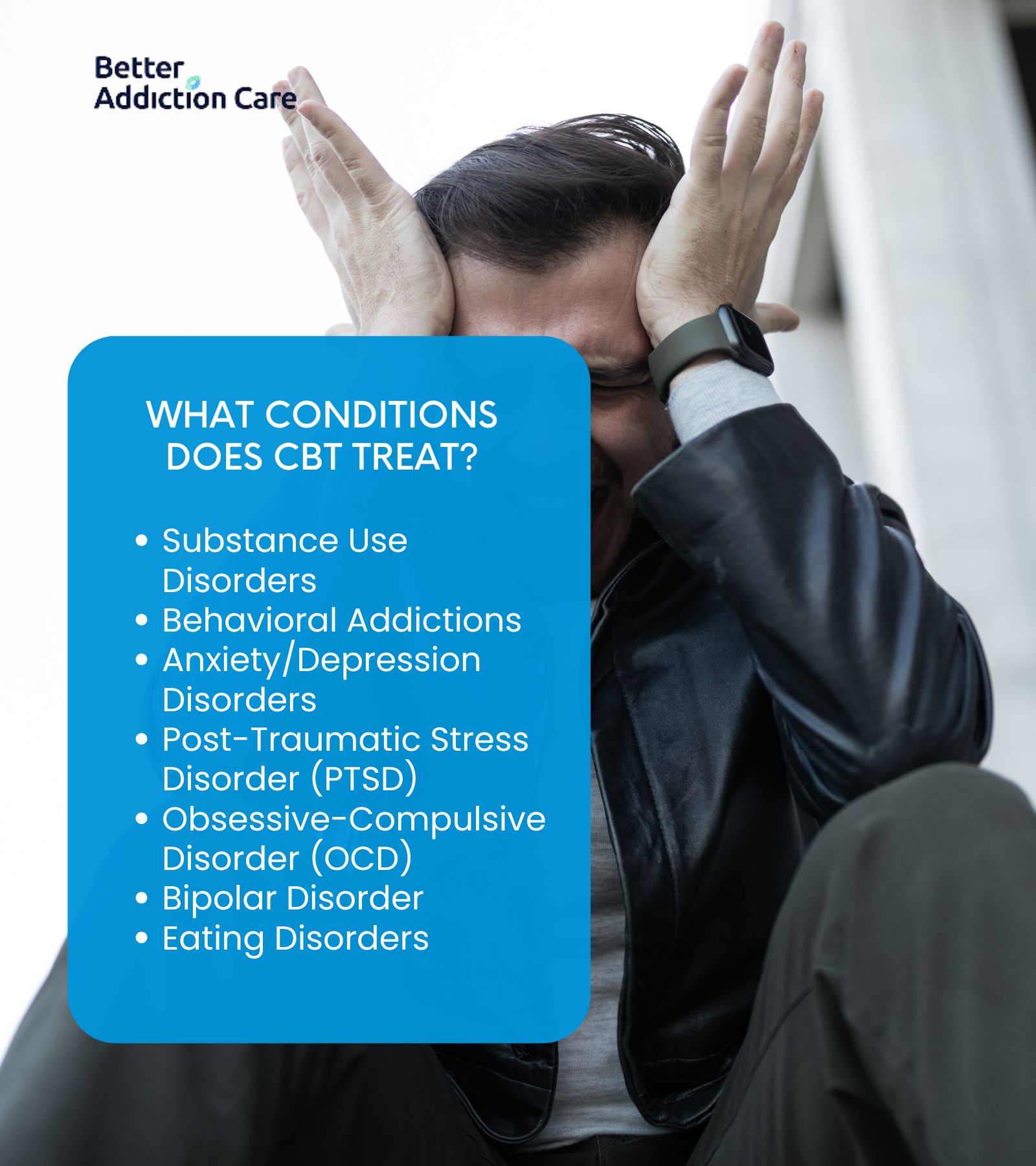
The conditions CBT treats are explained below:
-
Substance Use Disorders: These involve compulsive use of substances like alcohol or drugs, despite harmful consequences. CBT helps individuals overcome cravings, manage triggers, and replace addictive behavior with healthier coping mechanisms. According to a study by the National Institute on Drug Abuse (2020), CBT improves abstinence rates by over 40% when combined with medication-assisted treatment.
-
Behavioral Addictions: This includes addictions to behaviors such as gambling, gaming, or shopping that activate the brain's reward system. CBT helps individuals track thoughts, identify distorted beliefs, and use cognitive restructuring to disrupt compulsive patterns. Structured sessions support goal-setting and behavioral change through daily practice and exposure-based techniques.
-
Anxiety/Depression Disorders: These are characterized by persistent worry, fear, sadness, or loss of interest. CBT teaches patients to identify and question negative automatic thoughts and shift them toward rational alternatives. According to a study by the National Institute of Mental Health in 2022, CBT reduces symptoms in up to 80% of patients with generalized anxiety and major depressive disorder.
-
Post-Traumatic Stress Disorder (PTSD): PTSD arises from traumatic events, leading to flashbacks, avoidance, and hyperarousal. CBT, particularly trauma-focused methods, helps patients process trauma memories, reduce avoidance, and regain emotional control. The U.S. Department of Veterans Affairs in 2019 reports that CBT-based exposure therapy reduces PTSD symptoms by up to 60% in veterans and civilians.
-
Obsessive-Compulsive Disorder (OCD): OCD involves intrusive thoughts (obsessions) and repetitive behaviors (compulsions) performed to reduce distress. CBT, especially Exposure and Response Prevention (ERP), helps patients resist compulsions while confronting obsessive fears.
-
Bipolar Disorder: Though CBT doesn’t replace medication in treating bipolar disorder, it complements pharmacotherapy by addressing depressive episodes and improving medication adherence. CBT helps patients manage early warning signs, maintain routines, and restructure beliefs contributing to emotional instability. The American Psychological Association (2018) confirms CBT reduces relapse and improves daily functioning in bipolar patients.
-
Eating Disorders: Conditions like anorexia, bulimia, and binge-eating disorder involve unhealthy relationships with food and body image. CBT focuses on questioning distorted body image beliefs, regulating eating patterns, and confronting triggers for disordered behavior. According to a study by Fairburn et al., published in Behaviour Research and Therapy (2015), CBT led to full recovery in 45% of bulimia nervosa patients after 20 sessions
What Are The Benefits of Cognitive Behavioral Therapy?
The benefits of Cognitive Behavioral Therapy are long-lasting behavioral change, emotional regulation, and improved mental resilience. CBT equips patients with practical tools to manage difficult emotions, avoid triggering situations, and respond to stress with healthy choices. It empowers individuals to take control of their recovery through active participation, sharing experiences, and the consistent use of coping strategies that strengthen mental well-being.

The main benefits of Cognitive Behavioral Therapy are:
-
Improved self-control: CBT helps individuals recognize impulsive thoughts and behaviors, allowing them to pause and choose healthier responses. This is particularly useful in reducing addictive behavior and preventing relapse.
-
Development of coping strategies: Patients learn targeted skills to manage anxiety, handle stress, and deal with emotional triggers in day-to-day life. These strategies are reinforced through repetition and real-world application.
-
Ability to avoid triggering environments: CBT teaches patients to identify high-risk situations and plan responses ahead of time. This reduces the likelihood of exposure to stimuli that provoke cravings or relapse.
-
Better emotional regulation: Individuals learn to process intense emotions without becoming overwhelmed, especially in conditions like PTSD or borderline personality disorder. Emotional stability supports healthier relationships and day-to-day functioning.
-
Increased self-awareness and accountability: Through tracking thoughts and analyzing behavior patterns, patients gain insight into how their thinking affects their actions. This awareness is crucial for lasting transformation.
Where Can I Find a Rehab With a Cognitive Behavioral Therapy Program?
You can find a rehab with a cognitive behavioral therapy program by using verified national directories, local referrals, and professional treatment platforms. One reliable starting point is the Behavioral Health Treatment Services Locator by the Substance Abuse and Mental Health Services Administration (SAMHSA), which allows users to filter by therapy type, including CBT.
The Better Addiction Care (BAC) directory also offers a comprehensive list of rehab centers across the country that implement CBT in their recovery programs. Additionally, speaking with primary care physicians, licensed therapists, or addiction specialists provides personalized referrals based on your needs and location.
When exploring options, ensure the center uses evidence-based treatments, employs licensed professionals, and incorporates CBT in both group and individual sessions.
How Effective Is Cognitive Behavioral Therapy?
Cognitive Behavioral Therapy is highly effective, with numerous studies demonstrating consistent success rates in treating a wide range of mental health disorders. According to a study by the National Institute of Mental Health (2022), CBT leads to significant improvements in up to 80% of patients with anxiety and depression and is particularly effective when adapted to match individual needs.
In the context of substance use disorders, the National Institute on Drug Abuse (2020) reports that CBT, when combined with other interventions, improves recovery outcomes and reduces relapse risk by more than 40%.
Compared to traditional talk therapy or supportive counseling, CBT shows superior outcomes due to its structured approach, focus on practical skills, and use of measurable goals. These results make CBT one of the most evidence-backed treatments available for both behavioral and mental health disorders.
Is CBT Used in Outpatient Drug Rehab?
Yes, Cognitive Behavioral Therapy is widely used in outpatient drug rehab because it provides structure, flexibility, and practical tools for long-term recovery without requiring full-time residential care.
Outpatient programs integrate CBT to help patients identify triggers, develop coping strategies, and address underlying beliefs that contribute to addictive behavior. Since outpatient rehab allows individuals to continue their daily responsibilities while receiving treatment, CBT's structured form of psychotherapy fits seamlessly into weekly or biweekly sessions.
Therapists guide patients through goal-setting, tracking thoughts, and problem-solving exercises that improve self-awareness and support relapse prevention. According to a study by the National Institute on Drug Abuse in 2020, CBT-based outpatient programs significantly reduce drug use and improve retention rates when compared to non-CBT outpatient services.
How Does CBT Help With Alcohol Addiction?
Cognitive Behavioral Therapy helps with alcohol addiction by teaching individuals how to identify triggers, challenge distorted thinking, and apply healthier responses instead of turning to alcohol.
Through sessions with trained therapists, patients learn to develop coping strategies that reduce emotional vulnerability and build resilience in high-risk situations. CBT addresses the underlying beliefs that drive alcohol use, such as "I need a drink to handle stress," and replaces them with rational alternatives.
It also focuses on preventing relapse by equipping individuals struggling with alcohol addiction with techniques to manage cravings, avoid triggering environments, and maintain behavioral changes long after treatment ends.
According to a study by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) titled "Cognitive-Behavioral Therapy for Alcohol Dependence" (2021), patients who completed CBT programs reported a 58% reduction in heavy drinking episodes and significantly higher rates of long-term abstinence compared to those who received minimal intervention.
How Is CBT Combined With Medication-Assisted Treatment?
Yes, Cognitive Behavioral Therapy is effectively combined with Medication-Assisted Treatment (MAT) to enhance recovery outcomes in individuals with substance use disorders.
While MAT addresses the biological aspects of addiction using FDA-approved medications like buprenorphine, methadone, or naltrexone, CBT complements it by targeting the psychological and behavioral components. This integrated approach improves treatment retention, reduces cravings, and lowers the risk of relapse.
According to a study by the National Institute on Drug Abuse titled "Combined Behavioral and Pharmacological Treatment of Opioid Addiction" (2020), patients who received both MAT and CBT were 60% more likely to remain in treatment and achieve abstinence compared to those who received MAT alone. The combination ensures both physical stabilization and the development of long-term coping strategies.
How Long Does a CBT Session Last?
Cognitive Behavioral Therapy sessions last between 45 to 60 minutes and are conducted once or twice per week, depending on the patient’s condition and treatment goals. Most CBT programs are short-term and structured, running for an average of 12 to 20 weeks, although this extends based on individual needs and treatment progress.
During this period, patients work closely with therapists to develop and practice coping strategies, track thoughts, and address behavior patterns related to their specific mental health or substance use concerns. The consistent, time-limited nature of CBT makes it accessible, focused, and results-driven.
How Is CBT Different From Motivational Interviewing?
Cognitive Behavioral Therapy (CBT) and Motivational Interviewing (MI) differ in structure, goals, and therapeutic focus, though both are used effectively in addiction treatment.
CBT is a structured, goal-oriented psychotherapy that focuses on identifying and changing negative thought patterns and behaviors through coping strategies, behavioral experiments, and cognitive restructuring.
In contrast, Motivational Interviewing is a client-centered, non-directive approach that aims to enhance a person’s intrinsic motivation to change by resolving ambivalence through open-ended questions and reflective listening.
While CBT emphasizes active participation in problem-solving and behavior tracking, MI focuses more on sharing experiences, exploring values, and strengthening commitment to change.
According to a study by the National Institute on Drug Abuse titled "Comparing Cognitive Behavioral Therapy and Motivational Interviewing" (2020), CBT is more effective for long-term behavioral change, while MI is especially useful in the early stages of treatment when patients are uncertain about quitting their addictive behavior.
Is CBT Effective for Relapse Prevention?
Yes, Cognitive Behavioral Therapy is highly effective for relapse prevention because it equips individuals with long-term skills to recognize and manage triggers, challenge cravings, and maintain behavioral change.
CBT helps patients build personalized coping strategies, improve emotional regulation, and strengthen decision-making to avoid returning to addictive behavior. It also promotes tracking thoughts and questioning harmful beliefs that resurface after treatment causing relapse.
According to a study by the National Institute on Drug Abuse titled "Relapse Prevention and Cognitive Behavioral Approaches" in 2020, CBT-based relapse prevention programs reduce the likelihood of relapse by up to 60% within the first year of recovery.
Is CBT a Short-Term or Long-Term Therapy?
Cognitive Behavioral Therapy is primarily a short-term therapy, though it is extended for long-term support based on the patient’s needs. Standard CBT programs last between 12 to 20 weeks, offering focused, goal-driven interventions designed to produce measurable change in a limited time frame.
However, for chronic conditions or complex cases, such as co-occurring disorders or prolonged addiction, CBT is extended into a longer-term framework. According to a study by the American Psychological Association titled "CBT Duration and Treatment Outcomes in Clinical Practice" in 2019, short-term CBT leads to substantial improvement in most patients, while those with severe or recurring symptoms benefit from ongoing sessions to maintain gains and prevent relapse.
How Long Does CBT Take to Be Effective?
Cognitive Behavioral Therapy takes 4 to 6 weeks to be effective, with most patients experiencing significant improvement by the 12th to 20th session. The effectiveness and speed of results depend on the severity of the condition, consistency in attendance, and the patient’s willingness to participate, complete assignments, and apply coping strategies.
According to a study by the National Institute of Mental Health titled "CBT Outcomes in Clinical Settings" (2021), 75% of patients with depression or anxiety reported symptom reduction within the first six weeks of structured CBT. Early change is a predictor of long-term recovery, especially when the treatment is tailored to individual needs.
How Does CBT Help With Negative Thought Patterns?
Cognitive Behavioral Therapy helps with negative thought patterns by teaching individuals to identify, question, and replace distorted beliefs with more balanced and realistic alternatives.
Through cognitive restructuring, patients learn to track thoughts, evaluate the evidence behind them, and reframe harmful thinking that contributes to emotional distress or addictive behavior. This process promotes healthier decision-making and emotional responses, especially during high-risk situations.
According to a study by the National Institute of Mental Health in 2020, patients who engaged in cognitive restructuring during CBT experienced a 65% reduction in negative thinking, leading to improved emotional regulation and reduced relapse rates.
Can CBT be Done Online or Remotely?
Yes, Cognitive Behavioral Therapy can be done online or remotely through secure video sessions, digital platforms, and telehealth services. Online CBT follows the same structured form as in-person therapy, including goal-setting, tracking thoughts, cognitive exercises, and coping strategies, all guided by licensed therapists. Find drug rehab faciltiies with licensed CBT providers offering both in-person and virtual sessions across Georgia, Massachusetts, Oklahoma, Illinois, New York, Pennsylvania, California, Texas, and Florida through our comprehensive treatment directory.
It is particularly beneficial for individuals with limited access to in-person care or those seeking flexible scheduling. According to a study by the National Institute of Mental Health titled "Efficacy of Internet-Based Cognitive Behavioral Therapy" in 2021, remote CBT was found to be equally effective as face-to-face sessions for treating anxiety, depression, and substance use disorders, with over 70% of participants reporting significant improvements in symptoms.







