Contingency Management (CM): Definition, Application, Process, Risks, and Benefits
Contingency management (CM) uses operant conditioning and reinforcement techniques to encourage positive behavioral changes, such as abstinence or treatment adherence. According to a study by Higgins et al. titled "Contingency Management in the Treatment of Substance Use Disorders," published in Psychiatry (2008), CM programs led to a 2.4x higher abstinence rate compared to standard treatment.

Contingency management (CM) uses operant conditioning and reinforcement techniques to encourage positive behavioral changes, such as abstinence or treatment adherence. According to a study by Higgins et al. titled "Contingency Management in the Treatment of Substance Use Disorders," published in Psychiatry (2008), CM programs led to a 2.4x higher abstinence rate compared to standard treatment.
CM is applied in addiction and mental health settings by rewarding verified behaviors like negative drug tests, medication compliance, or therapy attendance. The National Institute on Drug Abuse (2018) reports that voucher-based CM improved retention by 31% and increased abstinence by 55% in outpatient drug treatment.
The CM process involves setting behavioral goals, objectively monitoring behavior, and delivering immediate rewards once the target behavior is confirmed.
Limitations of CM include the cost of rewards, logistical challenges, and reduced effectiveness once incentives stop. According to a study by Petry et al. titled "Do the Effects of Contingency Management Diminish Over Time?" (2008), treatment effects declined within three months after reward discontinuation, indicating a need for supplemental long-term strategies.
CM offers key benefits such as increased treatment retention, reduced relapse, and higher patient engagement, especially in early recovery. A meta-analysis by Benishek et al., published in Addiction (2014) found that CM led to a 61% greater likelihood of abstinence compared to control interventions.
What Is Contingency Management?
Contingency Management (CM) is a behavioral therapy approach in healthcare that uses reinforcement techniques to encourage positive behavior change, particularly in substance use and mental health treatment. It operates on the principle of operant conditioning, where desirable behaviors are immediately followed by tangible rewards to increase the likelihood of repetition.
Developed from behavior modification theories, CM is grounded in the work of B.F. Skinner, a psychologist, emphasized the impact of environmental consequences on behavior. Skinner's research in the mid-20th century established the foundation for using incentives to shape behaviors through positive reinforcement rather than punishment.
CM remains a core strategy in modern behavioral therapy due to its measurable impact. It is particularly relevant in treating substance use disorders, where consistent reinforcement can increase treatment adherence and drug-free urine samples.
According to a study by the National Institute on Drug Abuse titled "Principles of Drug Addiction Treatment," published in 2018, CM interventions have led to a 31% improvement in treatment retention rates compared to standard care, proving its utility in structured treatment programs.
What Are the Four Pillars of Contingency Management?
The four pillars of contingency management applied during treatment include incentivizing drug-free test results, rewarding therapy attendance, and reinforcing medication adherence.
In addiction treatment, CM involves providing patients with vouchers, prizes, or privileges when they meet predefined behavioral targets—most commonly, producing clean urine samples. According to a study by Stephen T. Higgins titled "Contingency Management in the Treatment of Substance Use Disorders," published in Psychiatry (2008), patients receiving CM were 2.4 times more likely to remain abstinent during treatment compared to those receiving standard care.
In mental health treatment, CM supports behaviors like regular participation in therapy sessions, medication compliance, and reduction in self-harming behavior. This approach is especially useful in treating patients with schizophrenia, bipolar disorder, or co-occurring conditions.
A study by the National Institute of Mental Health (NIMH) titled "Behavioral Treatments for Severe Mental Illness" (2020) reported that CM led to a 22% improvement in patient engagement rates and reduced dropout rates across community-based mental health programs.
How Is Contingency Management Applied During Treatment?
Contingency management is applied during treatment by incentivizing drug-free test results, rewarding therapy attendance, and reinforcing medication adherence. In addiction treatment, CM involves providing patients with vouchers, prizes, or privileges when they meet predefined behavioral targets—most commonly, producing clean urine samples.
According to a study by Stephen T. Higgins titled "Contingency Management in the Treatment of Substance Use Disorders," published in Psychiatry (2008), patients receiving CM were 2.4 times more likely to remain abstinent during treatment compared to those receiving standard care.
In mental health treatment, CM supports behaviors like regular participation in therapy sessions, medication compliance, and reduction in self-harming behavior. This approach is especially useful in treating patients with schizophrenia, bipolar disorder, or co-occurring conditions.
A study by the National Institute of Mental Health (NIMH), titled "Behavioral Treatments for Severe Mental Illness" (2020), reported that CM led to a 22% improvement in patient engagement rates and reduced dropout across community-based mental health programs.
What Techniques Are Used in Contingency Management?
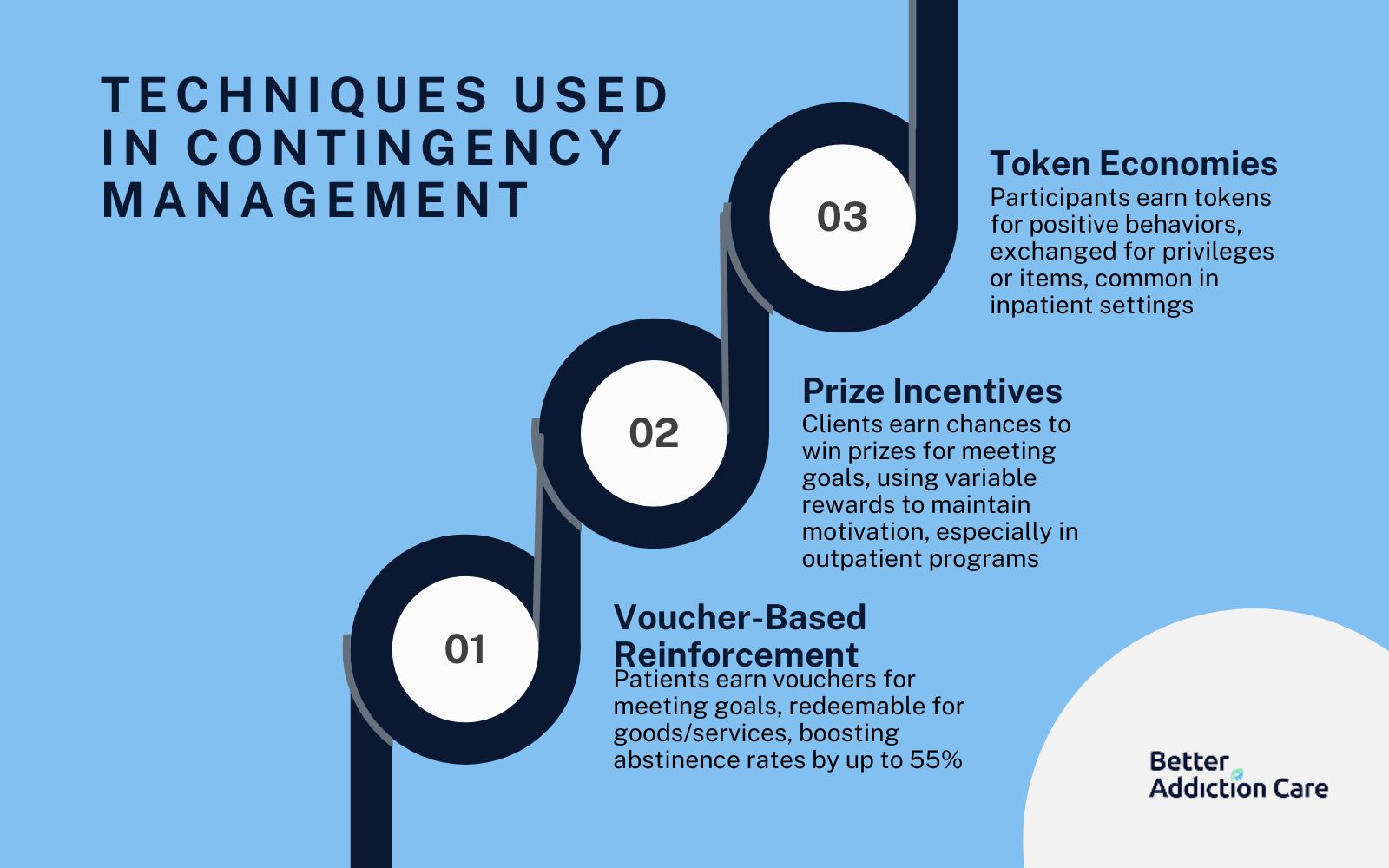
The techniques used in contingency management include voucher-based reinforcement, prize-based incentives, and level systems. These methods involve providing rewards—monetary or symbolic—immediately after the desired behavior to strengthen consistency and improve treatment outcomes.
The techniques used in contingency management are explained below:
-
Voucher-Based Reinforcement Programs: This technique provides patients with vouchers each time they meet a behavioral goal, such as submitting a drug-free urine sample. These vouchers are exchanged for goods or services like food, clothing, or transportation. According to a study by the National Institute on Drug Abuse titled "Contingency Management Interventions/Motivational Incentives" (2018), voucher-based programs increased abstinence rates by up to 55% during treatment.
-
Prize Incentives for Goal Achievement: Clients draw for a chance to win prizes when they meet a targeted behavior, such as attending therapy or remaining abstinent. The system uses variable reinforcement, with each draw offering a chance at different reward sizes to maintain motivation. This method has proven cost-effective while still improving engagement and compliance, especially in outpatient addiction programs.
-
Token Economies in Group Settings: Participants earn tokens for engaging in positive behaviors, such as participating in group discussions or following program rules. These tokens act as currency and are traded for privileges or items within the treatment facility. Token economies are especially useful in residential or inpatient settings where structured group dynamics are part of daily therapy.
What Is the Process During a Contingency Management Session?
The process during a contingency management session includes behavior assessment, objective verification, and immediate reward delivery. Clients are evaluated for target behaviors (e.g., abstinence), verified through tools like drug tests or attendance records, and reinforced with rewards immediately upon meeting criteria to strengthen the behavior-response connection.
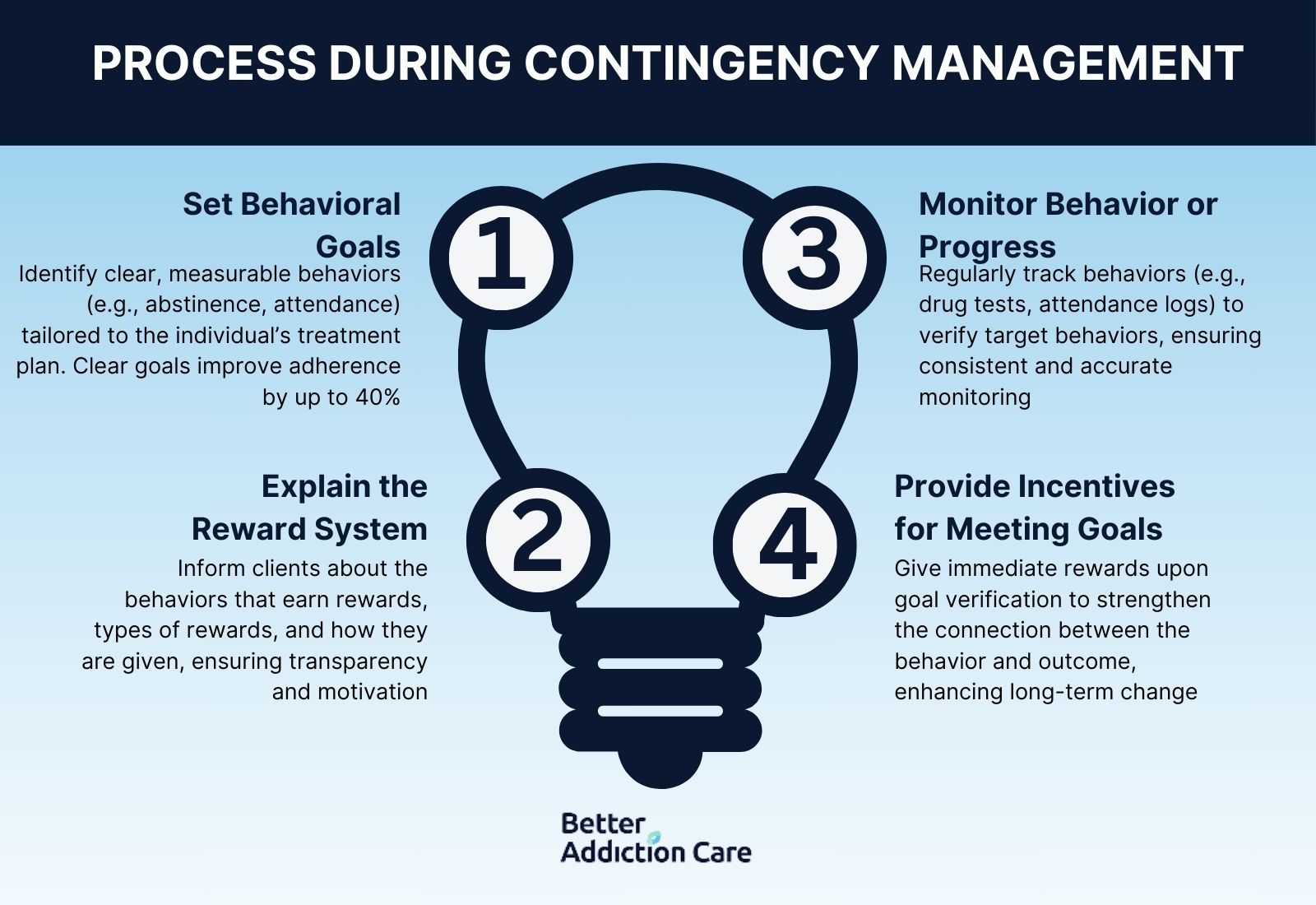
The process during contingency management is as follows:
-
Set Behavioral Goals: The first step involves identifying specific, measurable behaviors to target, such as abstinence from substances, therapy attendance, or medication adherence. These goals must be tailored to the individual’s treatment plan and clearly defined to avoid ambiguity. According to a study by Petry et al. 2005 titled "Contingency Management Improves Retention and Abstinence," published in the Journal of Consulting and Clinical Psychology, programs with clearly defined behavioral goals saw a 40% increase in treatment adherence.
-
Explain the Reward System: Patients are informed of what behaviors will earn rewards, the types of rewards available, and how rewards will be distributed. This step ensures transparency and boosts motivation by linking desired behaviors to meaningful incentives. A predictable and fair reward system is essential to maintaining client engagement.
-
Monitor Behavior or Progress: Regular, objective monitoring—such as urine drug screens, attendance logs, or therapist check-ins—is conducted to verify that the target behavior has occurred. Monitoring must be consistent and accurate to preserve the integrity of the program. Reliable tracking is key to reinforcing behavior promptly.
-
Provide Incentives for Meeting Goals: Once behavior is verified, the appropriate reward is given without delay to strengthen the connection between action and outcome. Delayed rewards reduce the effectiveness of reinforcement. Immediate distribution increases the likelihood of behavior repetition and long-term change.
What Types of Rewards Are Used in Contingency Management?
The types of rewards used in contingency management are monetary vouchers, prize draws, and privilege-based incentives. These rewards vary by program but are selected for their ability to offer immediate, tangible reinforcement that aligns with the client’s motivation and treatment goals.
The types of rewards used in contingency management are explained below:
-
Monetary Incentives: Patients receive vouchers or direct cash equivalents for meeting treatment goals, such as maintaining sobriety or attending sessions. These are exchanged for essentials like groceries, transportation, or hygiene products. According to a study by the National Institute on Drug Abuse titled "Principles of Drug Addiction Treatment" (2018), voucher-based CM programs improved abstinence rates by up to 55% during treatment.
-
Tangible Prizes: Clients earn the opportunity to draw for physical prizes ranging from small items like snacks to high-value rewards such as electronics or gift cards. This variable reinforcement system sustains engagement through excitement and unpredictability. It is cost-effective and widely used in outpatient programs.
-
Privileges or Access-Based Rewards: Individuals gain access to preferred activities, extended curfews, or social outings when behavioral goals are met. These are especially effective in residential or adolescent treatment settings where freedom and social access are valued. Privilege-based rewards help reinforce structure while respecting personal motivators.
All rewards in CM programs are customized to fit individual preferences, increasing the likelihood of response and long-term behavior change.
What Are the Benefits of Contingency Management?
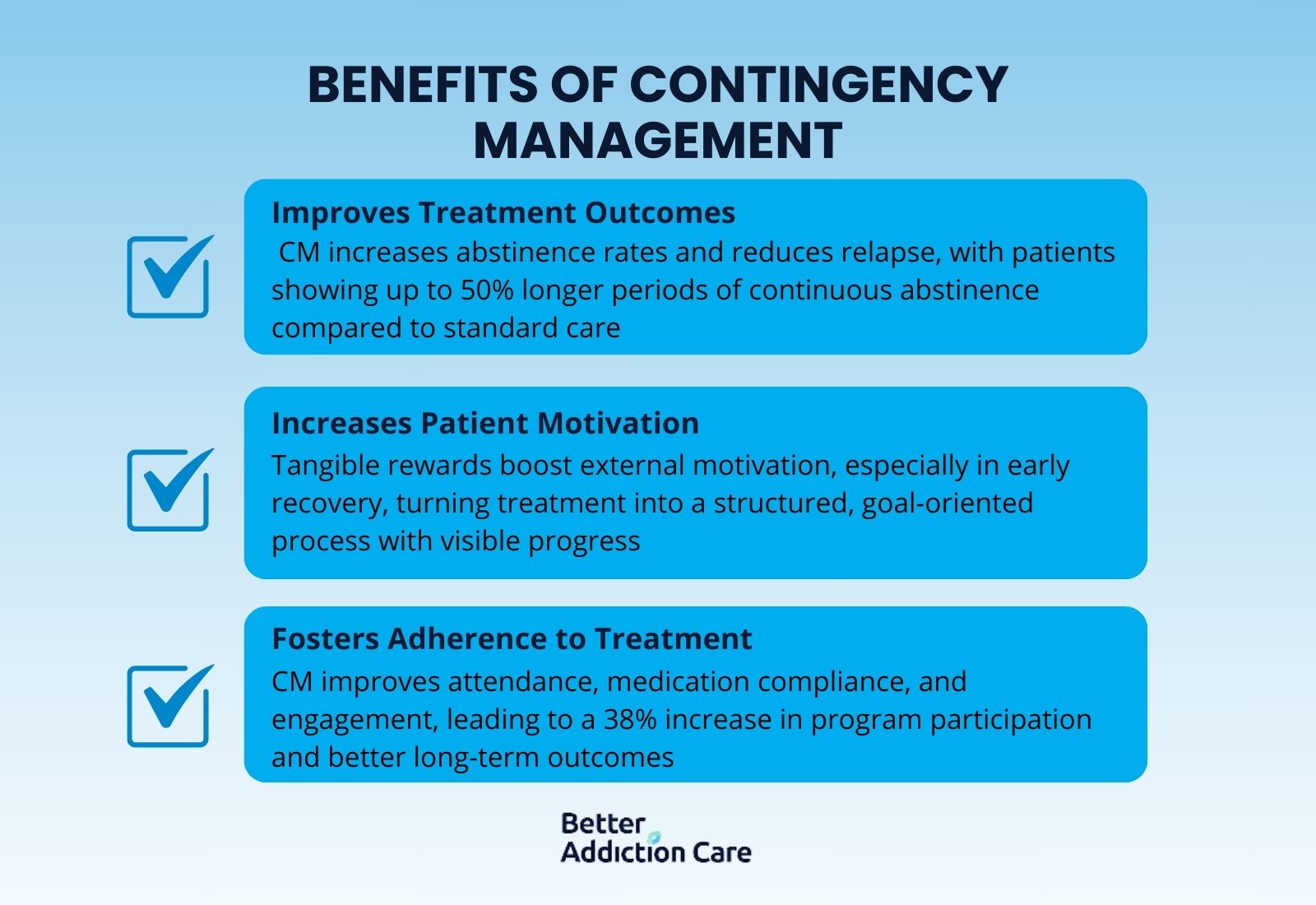
The benefits of contingency management are increased treatment retention, higher abstinence rates, and improved patient engagement. CM interventions improve abstinence outcomes and significantly reduce dropout rates in both addiction and mental health programs.
The benefits of contingency management are explained below:
-
Improves Treatment Outcomes: CM significantly enhances abstinence rates and reduces relapse during and after treatment. According to a study by Higgins et al. titled "Incentives Improve Outcomes in Cocaine Dependence Treatment," published in the Archives of General Psychiatry (2000), patients in CM programs showed a 50% longer period of continuous abstinence compared to those in standard care. Long-term success was also observed at 6-month follow-up evaluations.
-
Increases Patient Motivation: Tangible rewards create immediate, external motivation that drives consistent participation in therapy and recovery routines. This is especially effective in early recovery stages when internal motivation is still low. CM transforms treatment into a structured, goal-oriented experience with visible progress.
-
Fosters Adherence to Treatment Programs: CM boosts attendance, medication compliance, and overall engagement by tying accountability directly to reinforcement. According to a study by Petry et al. titled "Contingency Management Enhances Adherence to Treatment," published in the Journal of Substance Abuse Treatment (2006), attendance increased by 38% among CM participants. Consistent adherence improves long-term health outcomes and program success rates.
Who Can Benefit from Contingency Management?
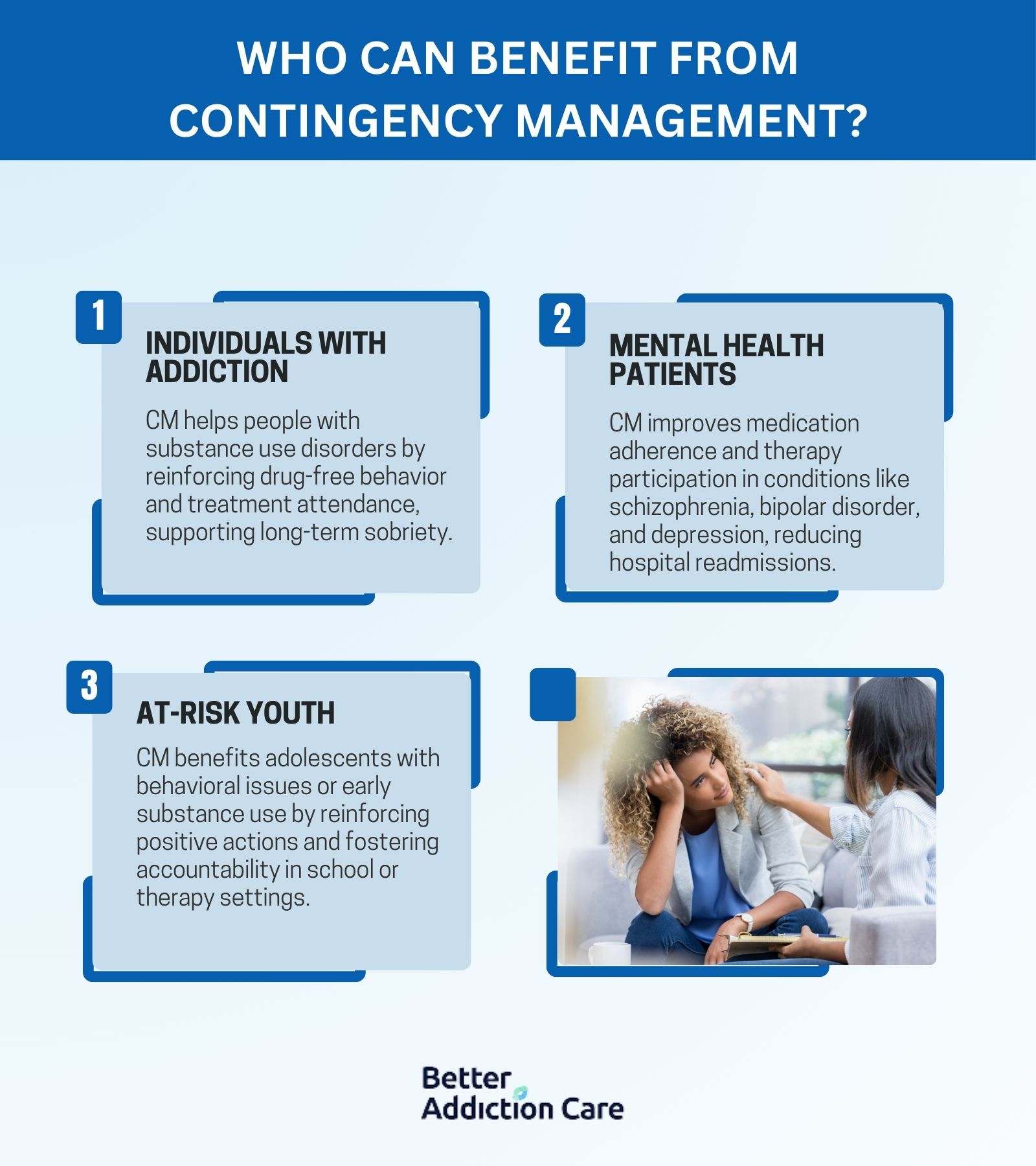
Individuals with addiction, mental health patients, and at-risk youth can benefit from contingency management. These groups respond positively to structured reinforcement systems, which improve behavioral control, increase program engagement, and reduce relapse or dropout rates across diverse treatment settings.
The people who can benefit from contingency management include the following:
-
Individuals with Addiction: People struggling with substance use disorders benefit from CM by receiving immediate reinforcement for remaining drug-free or attending treatment. The structure helps reduce impulsive behavior and supports long-term sobriety. CM is especially effective for stimulant, opioid, and alcohol dependence.
-
Mental Health Patients: Individuals managing conditions like schizophrenia, bipolar disorder, or depression benefit from CM through improved medication adherence and therapy participation. The reinforcement system provides motivation and structure, which are often lacking due to symptom-related barriers. CM also helps reduce hospital readmission rates.
-
At-Risk Youth: Adolescents with behavioral issues, truancy, or early substance use respond well to reward-based systems that reinforce positive actions. CM helps build responsibility and accountability in a developmentally appropriate way. It is commonly used in school-based programs, juvenile justice interventions, and family therapy settings.
What Are the Limitations of Contingency Management?
The limitations of contingency management are the cost of implementation, short-term behavior focus, and dependency on external rewards. Without proper transition planning, individuals struggle to maintain behavior change once incentives are removed, making long-term sustainability a concern in some settings.
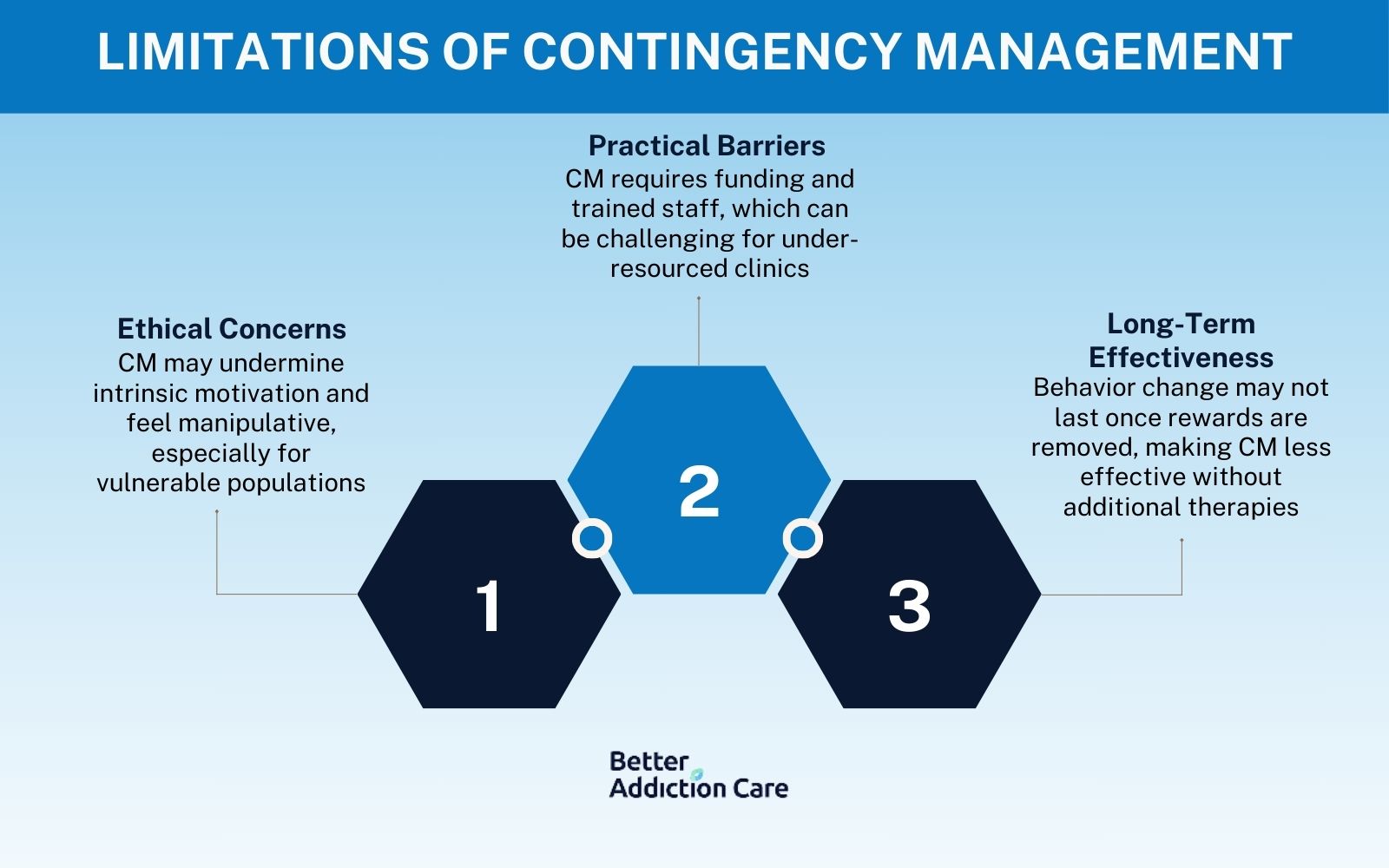
The limitations of contingency management are explained below:
-
Ethical Concerns: Critics argue that CM places too much emphasis on material rewards, potentially undermining intrinsic motivation for recovery. Some view it as manipulative, especially when used in vulnerable populations who feel coerced by the incentive structure. These concerns raise questions about fairness, autonomy, and long-term behavioral ownership.
-
Practical Barriers to Implementation: CM programs require funding for rewards, which can be a barrier for under-resourced clinics or public health systems. Additionally, effective implementation depends on trained staff who consistently monitor progress and manage reward systems. Program logistics, including tracking behaviors and distributing incentives, demand administrative time and infrastructure.
-
Limitations in Long-Term Effectiveness: Several studies indicate that once rewards are removed, behavior change is not always sustained, especially without supplementary therapies. This highlights the need for CM to be paired with other long-term behavioral or cognitive treatments. Overreliance on external reinforcement without internalization of goals limits its durability.
According to a study by Petry et al. titled "Do the Effects of Contingency Management Diminish Over Time?" published in the Journal of Consulting and Clinical Psychology (2008), benefits began to drop within three months after incentives were withdrawn. This finding highlights the importance of combining CM with long-term behavioral therapies for lasting results.
How to Find a Rehab That Includes Contingency Management?
To find a rehab that includes contingency management, use online directories like Better Addiction Care, SAMHSA’s Behavioral Health Treatment Services Locator, or the National Institute on Drug Abuse’s treatment-finder tools.
These platforms allow users to filter rehab facilities based on evidence-based approaches, including CM programs, ensuring access to structured, incentive-based therapies. It’s also recommended to contact centers directly to confirm that CM is actively integrated into their treatment protocols and delivered by trained professionals.
How Does Contingency Management Differ from Cognitive Behavioral Therapy?
Contingency management differs from cognitive behavioral therapy in its use of external rewards to reinforce behavior, while CBT focuses on identifying and restructuring negative thought patterns to drive internal behavioral change.
CM relies on operant conditioning principles, using tangible incentives like vouchers or privileges to shape observable behaviors directly. In contrast, CBT equips patients with coping skills and cognitive strategies to manage triggers and avoid relapse.
"According to a study by Petry et al. titled 'Contingency management versus cognitive-behavioral therapy for substance use disorders: A meta-analysis,' published in Psychology of Addictive Behaviors in 2017, contingency management showed a 61% higher rate of treatment retention compared to cognitive behavioral therapy across 22 clinical trials." This distinction makes them complementary rather than competing approaches in comprehensive treatment plans.
What Conditions Is Contingency Management Used for?
The conditions contingency management is used for are drug addiction, alcohol use disorder, mental health disorders, gambling addiction, obesity and weight management, and behavioral issues in adolescents. These diverse applications reflect CM’s effectiveness in reinforcing positive behaviors across clinical and community-based treatment settings.
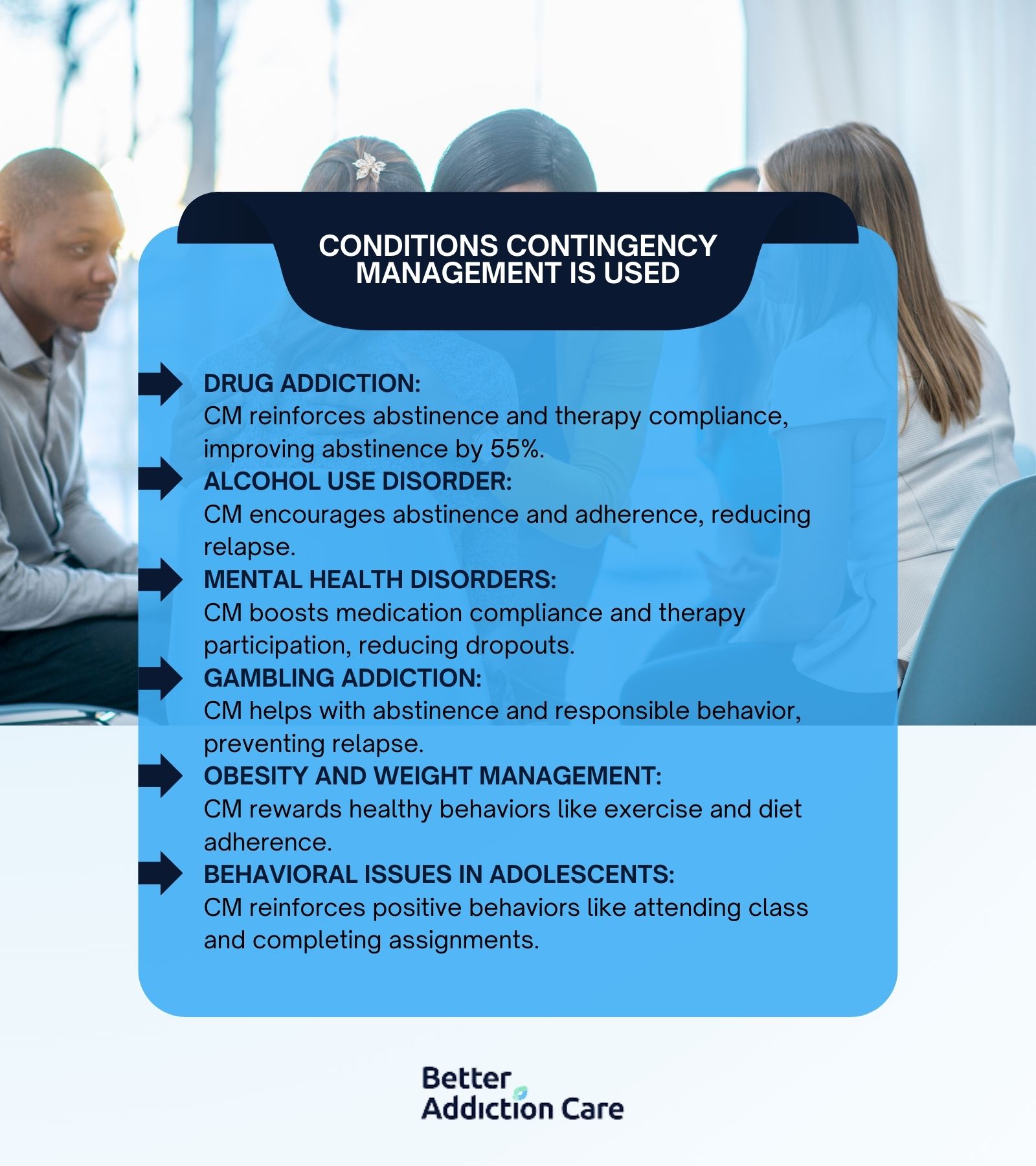
The conditions contingency management is used for are explained below:
Drug Addiction
Contingency management is widely used in the treatment of drug addiction, particularly for stimulant, opioid, and cannabis use disorders. It reinforces abstinence by providing immediate rewards for negative drug tests, program attendance, or therapy compliance.
According to a study by the National Institute on Drug Abuse titled "Principles of Drug Addiction Treatment" (2018), CM interventions led to a 55% increase in drug abstinence compared to standard care. Drug addiction remains a widespread issue, with an estimated 20.4 million people in the U.S. aged 12 or older reporting a substance use disorder in the past year (SAMHSA, 2022).
CM's structured reward system helps build consistent recovery habits, especially in the early stages of drug addiction treatment when relapse risk is highest.
Alcohol Use Disorder
Contingency management is used in alcohol use disorder (AUD) treatment by reinforcing abstinence, treatment attendance, and medication adherence with immediate, tangible rewards. CM is integrated with breathalyzer testing or biomarker tracking to verify alcohol-free behavior before rewards are distributed.
According to a study by the National Institute on Alcohol Abuse and Alcoholism titled "Alcohol Facts and Statistics" (2023), approximately 29.5 million people aged 12 and older in the U.S. had AUD in the past year.
CM has been shown to increase engagement and reduce relapse rates in both outpatient and residential alcohol addiction programs.
Mental Health Disorders
In mental health treatment, contingency management is applied to conditions like schizophrenia, bipolar disorder, and depression to promote medication compliance, therapy participation, and reduction of self-injurious behavior.
Reinforcements are given for behaviors such as attending appointments or maintaining symptom-tracking logs. According to the National Institute of Mental Health (2022), 57.8 million U.S. adults experienced a mental illness in the past year, underscoring the importance of interventions that promote treatment continuity.
CM is particularly effective in reducing dropout rates and improving daily functioning among patients with severe mental illnesses.
Gambling Addiction
Contingency management supports recovery from gambling addiction by reinforcing abstinence from gambling activities, financial responsibility, and participation in therapy. Monitoring tools like spending reports or self-report logs are verified before incentives are awarded.
The National Council on Problem Gambling (2023) estimates that about 2 million U.S. adults meet the criteria for severe gambling problems, with another 4-6 million showing mild to moderate gambling issues. CM provides external accountability and structure, which are critical in rebuilding self-regulation and preventing relapse.
Obesity and Weight Management
In weight management programs, contingency management is used to encourage behaviors like exercise adherence, healthy meal tracking, and weight monitoring. Participants earn rewards for achieving physical activity goals or dietary milestones, which strengthens commitment to lifestyle changes.
According to the Centers for Disease Control and Prevention (CDC, 2023), over 41.9% of U.S. adults are classified as obese, contributing to rising rates of heart disease, diabetes, and other chronic conditions. CM offers a practical strategy to support behavioral change in both clinical and community wellness programs.
Behavioral Issues in Adolescents
Contingency management is used in school and clinical settings to address adolescent issues such as defiance, truancy, and early substance use. Rewards are provided for meeting behavioral targets like attending class, completing assignments, or following therapy routines.
The CDC’s Youth Risk Behavior Survey (2021) reports that 29% of high school students experienced persistent sadness or hopelessness, while 16% engaged in risky substance use behaviors. CM helps create structure, reinforce positive behavior, and engage families in the treatment process.
How Effective Is Contingency Management?
Contingency management is most effective for stimulant use disorders, opioid addiction, and co-occurring substance use and mental health conditions, where consistent behavior reinforcement is critical.
According to a meta-analysis by Benishek et al. titled "Prize-Based Contingency Management for the Treatment of Substance Abusers," published in the Addiction Journal (2014), CM interventions produced a 61% greater likelihood of abstinence compared to control conditions.
Similarly, a report by the National Institute on Drug Abuse (2020) confirmed CM as one of the most empirically supported treatments for cocaine and methamphetamine use, where traditional therapies often show limited effectiveness.
Its success in increasing treatment adherence and reducing relapse makes it a key component in integrated behavioral health strategies.
How Is Progress Tracked in CM?
Progress is tracked in CM by using objective, verifiable measures such as urine drug screens, breathalyzer tests, attendance records, medication logs, and behavioral checklists.
Yes- this structured tracking is essential because it ensures that rewards are only given when clearly defined goals are met, preserving the integrity and fairness of the program.
According to a study by Petry et al. titled "Contingency Management in Substance Abuse Treatment," published in Psychiatric Clinics of North America (2008), accurate monitoring improved program compliance by over 40%, especially when tied to immediate reinforcement. This method helps clinicians measure short-term gains while encouraging consistent behavior over time.
How Long Does Contingency Management Last?
Contingency management lasts between 8 to 24 weeks on average, depending on the treatment setting, target behavior, and clinical goals. Short-term CM programs, typically 8 to 12 weeks, are common in outpatient addiction treatment where the focus is on initial abstinence and program engagement.
Longer durations—up to 6 months—are used for patients with chronic conditions or co-occurring disorders to reinforce sustained behavioral change. According to a study by Petry et al. titled "Longer-Term Outcomes with Contingency Management," published in Psychology of Addictive Behaviors (2012), extending CM beyond 12 weeks resulted in greater maintenance of abstinence at 6- and 12-month follow-ups.
Duration is strategically aligned with the behavior being targeted and the individual’s progress trajectory.
Is CM Covered by Insurance?
Yes, contingency management is covered by insurance, but coverage is limited and varies by plan and location. While CM is recognized as an evidence-based practice, it is not universally reimbursed due to challenges in billing for non-traditional therapeutic incentives.
Medicaid has begun funding pilot CM programs in certain states, and some private insurers offer partial reimbursement when CM is bundled within comprehensive behavioral treatment plans. Patients are encouraged to verify coverage directly with their provider or through trusted directories.
To confirm whether your insurance covers contingency management programs, use Better Addiction Care to check eligibility and explore accredited facilities.
How Do Rewards in CM Prevent Relapse?
Rewards in CM prevent relapse by strengthening the association between sobriety and positive outcomes, which reinforces healthy behavior patterns over time. By delivering immediate, consistent incentives for abstinence or treatment compliance, CM helps rewire the brain’s reward system—shifting focus from substance-related gratification to constructive reinforcement.
According to a study by the National Institute on Drug Abuse titled "Contingency Management: Incentives for Sobriety" (2020), individuals in CM programs experienced a 50% reduction in relapse rates compared to those receiving standard treatment alone. This immediate feedback loop helps build momentum during early recovery, where relapse risk is highest, and provides a structured foundation for long-term behavior change.







