Dialectical Behavior Therapy (DBT): Definition, Application, Process, Risks and Benefits
Dialectical Behavior Therapy (DBT) helps individuals regulate emotions, tolerate distress, and improve behaviors, making it highly effective for mental health and addiction treatment. According to a study by Linehan et al. titled "Dialectical Behavior Therapy for Substance Use Disorders," published in the American Journal of Psychiatry (2019), individuals undergoing DBT for addiction had a 63% higher likelihood of maintaining sobriety compared to those in traditional treatment programs.

Dialectical Behavior Therapy (DBT) helps individuals regulate emotions, tolerate distress, and improve behaviors, making it highly effective for mental health and addiction treatment. According to a study by Linehan et al. titled "Dialectical Behavior Therapy for Substance Use Disorders," published in the American Journal of Psychiatry (2019), individuals undergoing DBT for addiction had a 63% higher likelihood of maintaining sobriety compared to those in traditional treatment programs.
DBT is applied in addiction and mental health therapy by teaching individuals distress tolerance, emotional regulation, and mindfulness skills to manage impulsive behaviors and relapse triggers.
The process of a DBT session involves skills training, behavioral reinforcement, and real-life application of coping mechanisms. According to a study by Neacsiu et al. titled "The Impact of DBT on Emotional Dysregulation," published in the Journal of Affective Disorders (2020), individuals completing DBT reported a 50% decrease in emotional reactivity and a 35% improvement in distress tolerance compared to other therapy approaches.
The DBT limitations include its time-intensive nature, high dropout rates, and the need for trained therapists, which limits accessibility. Patients enrolled in DBT programs fail to complete treatment due to its rigorous structure.
DBT offers significant benefits, such as improved emotional regulation, reduced self-harm behaviors, and better interpersonal relationships, making it highly effective for long-term mental health stability.
According to a study by Stoffers-Winterling et al. titled "Effectiveness of DBT for Borderline Personality Disorder," published in the Cochrane Database of Systematic Reviews in 2020, DBT was 77% more effective in reducing self-harm and impulsive behaviors compared to traditional talk therapy.
What Is Dialectical Behavior Therapy (DBT)?
Dialectical Behavior Therapy (DBT) is an evidence-based therapy that combines cognitive-behavioral techniques with mindfulness strategies to help individuals regulate emotions, manage distress, and improve interpersonal behaviors.
Originally developed by psychologist Marsha M. Linehan in the late 1980s, DBT was designed to treat individuals with mental health conditions such as borderline personality disorder (BPD) by addressing self-destructive tendencies, impulsive actions, and extreme negative thoughts. Unlike traditional talk therapy, DBT incorporates structured skill-building exercises to enhance emotional regulation and distress tolerance.
The roots of DBT are traced back to psychodynamic therapy, which emphasizes the role of unconscious conflicts and early life experiences in shaping current emotions and behaviors. While psychodynamic therapy focuses on exploring past experiences, DBT takes a structured and skills-based approach, aiming to modify immediate responses to distress.
This makes it distinct from other therapeutic models, including Cognitive Behavioral Therapy (CBT), which primarily targets dysfunctional thinking patterns without the mindfulness-based interventions seen in DBT.
According to a study by the National Institute of Mental Health (NIMH) titled "Effectiveness of Dialectical Behavior Therapy in Treating Borderline Personality Disorder," published in 2019, individuals undergoing DBT showed a 50% reduction in self-harm behaviors and an improvement in overall emotional regulation compared to those receiving standard psychiatric care.
What Is Dialectical Behavior Therapy (DBT) Used For?
Dialectical Behavior Therapy is used for treating a range of mental health conditions, including borderline personality disorder (BPD), depression, anxiety disorders, substance use disorders, and post-traumatic stress disorder (PTSD).
Originally designed to focus on suicidal behavior and BPD, DBT has since been adapted to help individuals struggling with negative thoughts, self-destructive behaviors, and emotional dysregulation. As an evidence-based therapy, it integrates cognitive-behavioral techniques with mindfulness practices to enhance distress tolerance and improve overall psychological well-being.
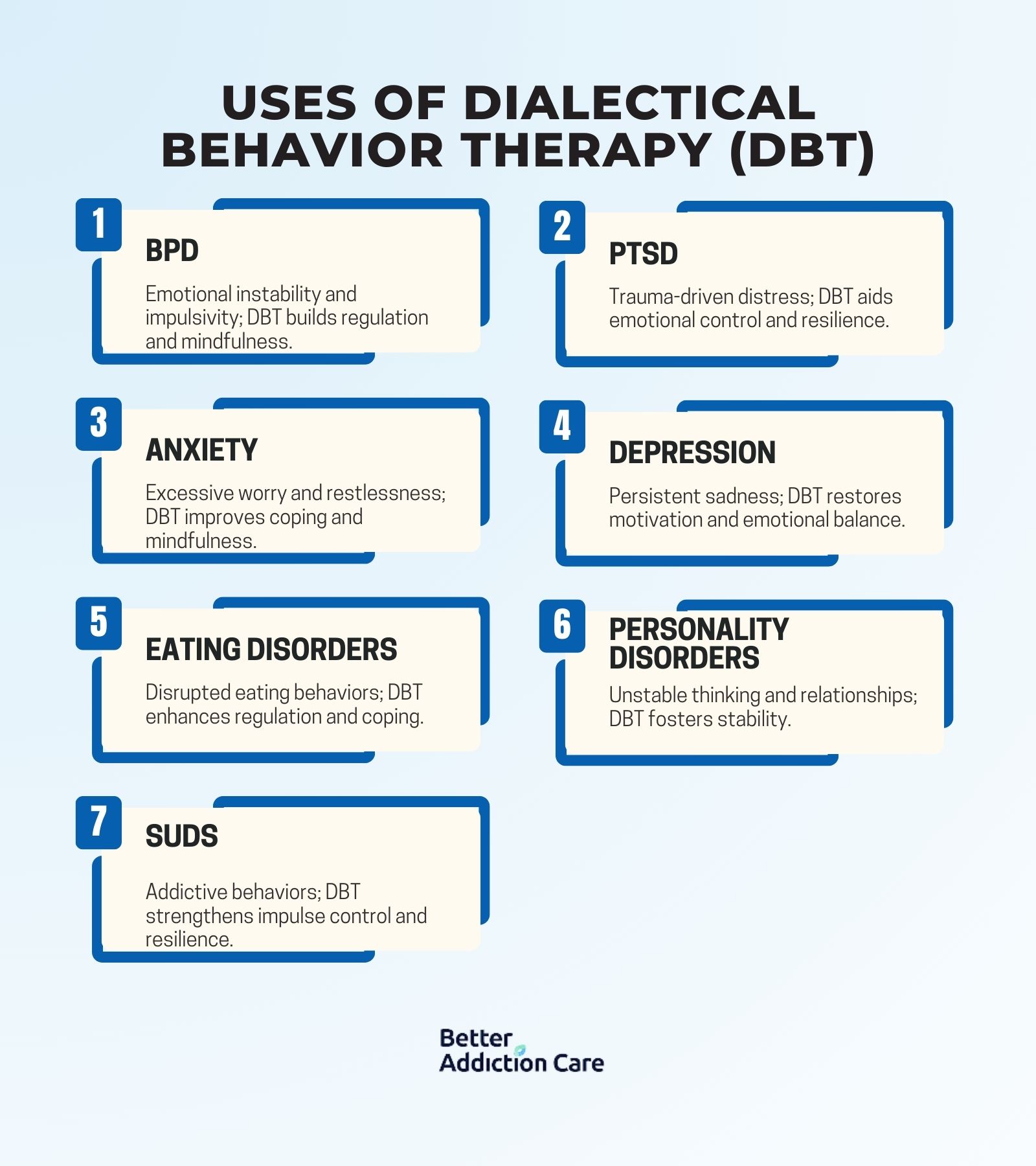
The disorders of dialectal behavior therapy are explained below:
Borderline Personality Disorder (BPD)
BPD is a personality disorder characterized by unstable relationships, emotional instability, impulsive behaviors, and intense fears of abandonment. Individuals with BPD struggle with self-harm, suicidal tendencies, and extreme negative thoughts that impact their daily functioning. DBT helps by teaching emotional regulation, distress tolerance, interpersonal effectiveness, and mindfulness techniques to manage overwhelming emotions. According to a study by the National Institute of Mental Health (NIMH), approximately 1.6% of adults in the U.S. are diagnosed with BPD, with up to 75% of affected individuals engaging in self-harming behaviors.
Post-Traumatic Stress Disorder (PTSD)
PTSD is a psychiatric disorder that develops after experiencing or witnessing a traumatic event, leading to intrusive memories, nightmares, emotional numbness, and hypervigilance. People with PTSD struggle with intense emotions, distressing flashbacks, and difficulty regulating their behaviors. DBT helps by improving distress tolerance, reducing emotional reactivity, and using mindfulness-based skills to process traumatic experiences. Research from the National Center for PTSD shows that 6% of the U.S. population will experience PTSD at some point in their lives, with higher rates in veterans and first responders.
Anxiety Disorders
Anxiety disorders involve excessive worry, fear, and nervousness that interfere with daily life. Individuals experience negative thoughts, restlessness, difficulty concentrating, and physical symptoms like rapid heartbeat or shortness of breath. DBT helps by incorporating mindfulness techniques to reduce anxiety, improving emotion regulation, and teaching distress tolerance strategies to manage overwhelming stress. According to the Anxiety and Depression Association of America (ADAA), anxiety disorders affect 19.1% of adults in the U.S. annually, making it one of the most prevalent mental health conditions.
Depression
Depression is a mood disorder characterized by persistent sadness, loss of interest in activities, fatigue, and suicidal ideation. Individuals with depression struggle with negative thoughts, emotional numbness, and difficulties in daily functioning. DBT provides structure through behavioral activation, emotion regulation techniques, and interpersonal effectiveness skills to help individuals regain motivation and improve their emotional well-being. According to the National Institute of Mental Health (NIMH), depression affects 8.4% of U.S. adults annually, with higher rates among women.
Eating Disorders
Eating disorders, including anorexia nervosa, bulimia nervosa, and binge-eating disorder, involve severe disturbances in eating behavior, body image distortions, and unhealthy coping mechanisms. These disorders stem from emotional distress, negative thoughts, and an inability to regulate emotions effectively. DBT helps by targeting emotional dysregulation, improving distress tolerance, and teaching coping strategies to replace maladaptive behaviors like food restriction, bingeing, or purging. According to the National Eating Disorders Association (NEDA), nearly 9% of the U.S. population will develop an eating disorder in their lifetime.
Personality Disorders
Personality disorders involve long-term patterns of unhealthy thinking, behaviors, and interpersonal difficulties. Individuals with these disorders struggle with emotional instability, impulsivity, and challenges in relationships. DBT is particularly effective for treating personality disorders as it enhances self-awareness, emotional control, and social functioning. Research from the American Psychiatric Association (APA) suggests that up to 10% of the general population have a personality disorder, with varying severity levels.
Substance Use Disorders/Drug Addiction
Substance use disorders (SUDs) involve the compulsive use of drugs or alcohol despite negative consequences. Individuals with drug addiction and AUD turn to substances as a way to cope with distress, emotional pain, or unresolved trauma. DBT helps by teaching distress tolerance skills, reducing impulsivity, and enhancing coping mechanisms to prevent relapse. According to the National Institute on Drug Abuse (NIDA), approximately 21 million Americans struggle with a substance use disorder, with alcohol and opioid addiction being the most common.
How Is DBT Applied In Rehab Programs?
DBT is applied in rehab programs by incorporating talk therapy, mindfulness techniques, and structured behavioral interventions to help individuals manage negative thoughts, distress, and impulsive behaviors.
It is delivered through individual therapy sessions, group skills training, and phone coaching, ensuring that individuals with mental health conditions such as substance use disorders, BPD, and PTSD develop long-term coping strategies for emotional regulation and relapse prevention.
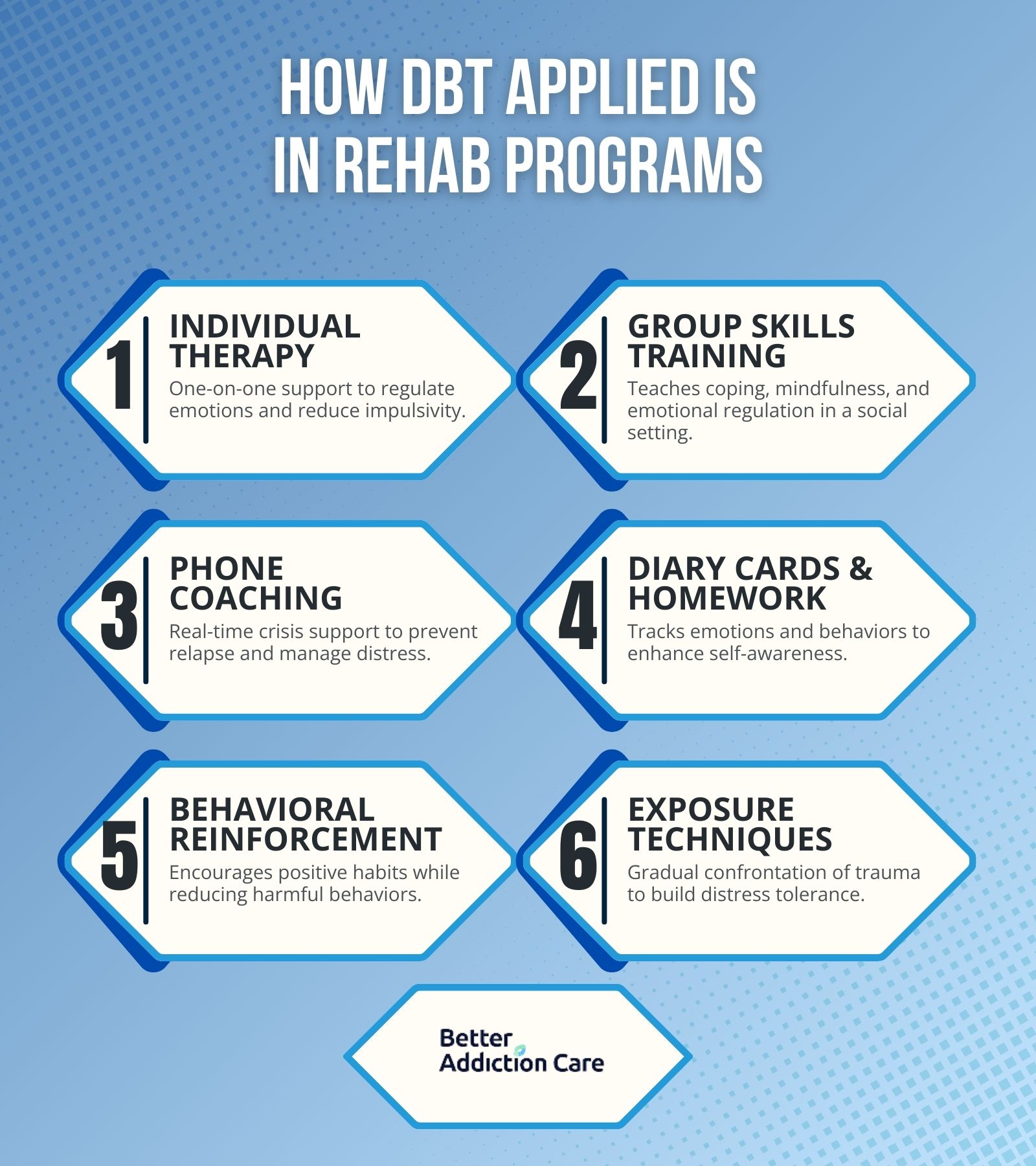
Ways DBT applied in rehab are explained below:
-
Individual Therapy: Individual therapy sessions provide one-on-one support to help patients identify negative thoughts, emotional triggers, and destructive behaviors. This component is particularly beneficial for individuals with BPD, PTSD, and substance use disorders, as it focuses on emotion regulation and distress tolerance strategies. Therapists use problem-solving approaches and cognitive restructuring to reduce impulsive actions and self-harm tendencies. According to a study by the National Institute of Mental Health (NIMH), DBT-based individual therapy reduces suicidal behaviors by 50% in individuals diagnosed with BPD compared to traditional therapy.
-
Group Skills Training: Group DBT sessions teach essential coping skills, including mindfulness, interpersonal effectiveness, emotional regulation, and distress tolerance. These skills help individuals with anxiety disorders, depression, and personality disorders develop healthier communication methods and manage overwhelming emotions. Group training reinforces social support and accountability while allowing patients to practice new strategies in a controlled environment. Research from the American Psychiatric Association (APA) found that 60% of individuals undergoing DBT group therapy experienced improved emotional regulation and reduced self-harming behaviors.
-
Phone Coaching: Phone coaching offers real-time support for individuals facing emotional crises, allowing them to apply DBT techniques outside therapy sessions. It is particularly effective for individuals with substance use disorders, PTSD, and eating disorders, as it helps prevent relapse and impulsive decision-making. Patients contact their therapists for guidance on managing distressing situations and applying learned DBT strategies. A study by the National Institute on Drug Abuse (NIDA) found that individuals who had access to DBT phone coaching were 40% less likely to relapse into substance abuse than those without it.
-
Diary Cards & Homework: Diary cards and homework assignments encourage self-monitoring by having patients track their emotional responses, triggers, and behavioral patterns. This component is particularly useful for individuals with BPD, depression, and eating disorders, as it promotes self-awareness and helps therapists tailor interventions. Patients record distressing emotions, impulsive actions, and coping mechanisms to identify progress and areas for improvement.
-
Behavioral Reinforcement: Behavioral reinforcement in DBT helps individuals replace maladaptive coping mechanisms, such as self-harm, substance use, or avoidance, with healthier alternatives. This technique is widely used in treating personality disorders, PTSD, and anxiety disorders, as it reinforces positive behaviors through rewards and encouragement. Therapists use contingency management techniques, reinforcing behaviors that align with treatment goals while discouraging harmful patterns. According to a study by the National Center for PTSD, behavioral reinforcement combined with DBT techniques led to a 45% reduction in PTSD-related symptoms.
-
Exposure Techniques: Exposure techniques help individuals gradually confront distressing thoughts, emotions, or traumatic memories in a controlled manner. This method is particularly effective for individuals with PTSD, anxiety disorders, and depression, as it reduces avoidance behaviors and increases distress tolerance. DBT incorporates mindfulness-based exposure strategies, allowing patients to process emotions without feeling overwhelmed.
What Is The Process During Dialectical Behavior Therapy?
The process during Dialectical Behavior Therapy includes assessment and goal setting, skills training, exposure therapy, behavioral reinforcement, and continuous progress monitoring. Individuals work with therapists to identify emotional triggers, practice talk therapy techniques, and apply mindfulness-based strategies to regulate negative thoughts and impulsive behaviors, ensuring long-term management of their mental health condition.
The process during dialectical behavior therapy is explained below:
-
Assessment and Goal Setting: Therapists evaluate the individual’s emotional challenges, triggers, and negative thoughts while establishing treatment goals tailored to their specific needs.
-
Learning DBT Skills: Patients are introduced to core DBT techniques, including mindfulness, distress tolerance, and emotional regulation, to help them manage mental health conditions effectively.
-
Practicing Mindfulness: Individuals engage in guided breathing exercises, meditation, and self-awareness practices to stay present and reduce impulsive behaviors.
-
Managing Emotions: Therapy sessions focus on identifying emotional triggers, restructuring thought patterns, and learning coping mechanisms to regulate intense emotions.
-
Building Distress Tolerance: Patients develop crisis management strategies, including grounding techniques and radical acceptance, to navigate distressing situations without harmful reactions.
-
Improving Relationships: Interpersonal effectiveness training teaches individuals how to set boundaries, communicate assertively, and build healthier social connections.
-
Applying Skills in Daily Life: Patients practice learned DBT strategies in real-world situations, such as handling conflicts, avoiding relapse, and maintaining emotional balance.
-
Tracking Progress: Diary cards and self-monitoring tools help individuals document emotional responses, skill usage, and behavioral changes over time.
-
Adjusting Treatment as Needed: Therapists review progress, modify interventions, and introduce new strategies based on the individual’s evolving needs and challenges.
What Are The Common Worksheets Used In Dialectical Behavior Therapy?
The common worksheets used in Dialectical Behavior Therapy are mindfulness exercises, emotion regulation logs, distress tolerance worksheets, interpersonal effectiveness sheets, and thought tracking journals. These worksheets help individuals identify negative thoughts, monitor emotional triggers, practice talk therapy techniques, and apply learned DBT strategies to improve their mental health condition and daily behaviors.
The common worksheets used in Dialectical Behavior Therapy include:
-
Chain Analysis: Helps individuals identify triggers, emotional responses, and the chain of events leading to maladaptive behaviors. It is used to break negative patterns and develop healthier coping strategies.
-
Diary Cards: Used for tracking daily emotions, distress levels, and the application of DBT skills. Patients record their emotional responses and negative thoughts to monitor progress and adjust their coping mechanisms.
-
Emotion Regulation Worksheets: Focuses on recognizing, labeling, and modifying emotional responses. These worksheets help individuals develop strategies to manage overwhelming emotions and maintain emotional stability.
What Are The Limitations Of Dialectical Behavior Therapy?
The limitations of Dialectical Behavior Therapy are time-intensive treatment, the need for highly trained therapists, and its limited effectiveness for certain mental health conditions.
While DBT is an evidence-based therapy, it requires long-term commitment, is not suitable for individuals struggling with severe cognitive impairments, and relies on structured support, which is not always accessible.
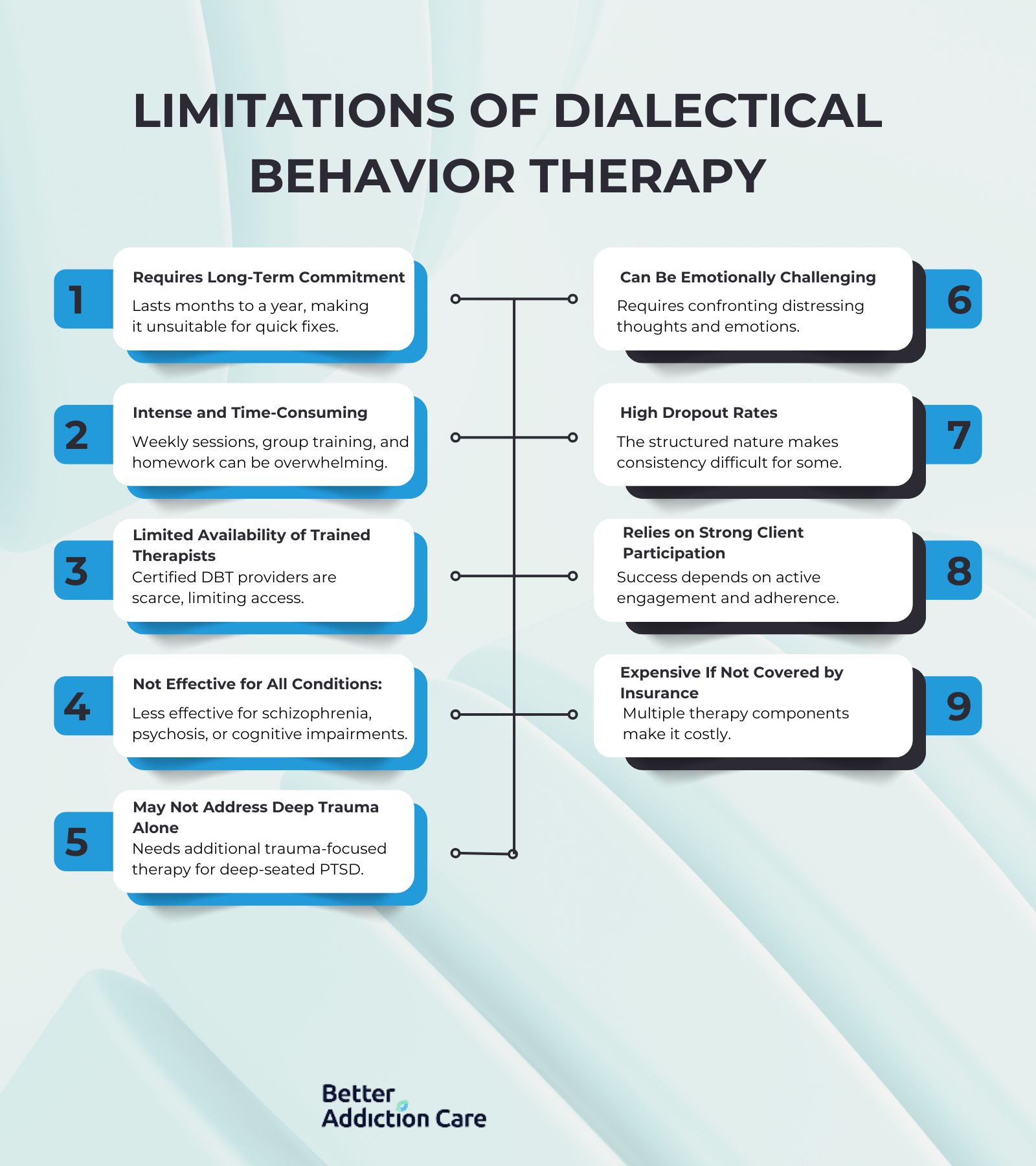
The limitations of dialectical behavior therapy include:
-
Requires Long-Term Commitment: DBT is a structured therapy that lasts several months to a year, making it difficult for individuals seeking quick solutions. Patients must actively engage in ongoing therapy sessions and practice skills consistently for lasting benefits.
-
Intense and Time-Consuming: DBT involves weekly individual therapy, group skills training, and additional homework assignments, which are overwhelming for individuals with busy schedules or severe emotional distress. The high time demand makes it difficult for some to complete the full program.
-
Limited Availability of Trained Therapists: DBT requires specialized training, and not all therapists are certified to provide it. This limits access, particularly in rural areas or regions with fewer mental health professionals trained in DBT.
-
Not Effective for All Mental Health Conditions: While DBT is highly beneficial for BPD, PTSD, and substance use disorders, it is not as effective for severe schizophrenia, psychosis, or cognitive impairments. Some individuals require additional treatments, such as medication management or alternative therapies.
-
May Not Address Deep-Rooted Trauma Alone: Although DBT helps individuals manage distress and emotional regulation, it does not fully resolve deep-seated trauma. Individuals with significant PTSD or childhood trauma need additional trauma-focused therapy, such as Eye Movement Desensitization and Reprocessing (EMDR).
-
Can Be Emotionally Challenging: DBT requires patients to confront negative thoughts, regulate intense emotions, and change maladaptive behaviors, which is distressing. Some individuals struggle with the emotional demands and find the process overwhelming.
-
High Dropout Rates Due to Rigorous Structure: The structured nature of DBT is challenging for individuals who struggle with consistency or commitment.
-
Relies on Strong Client Participation: DBT success depends on the individual's willingness to actively engage in therapy, complete assignments, and apply learned skills. Those who struggle with motivation or adherence do not experience the full benefits of the treatment.
-
Expensive If Not Covered by Insurance: DBT involves multiple therapy components, including individual sessions, group therapy, and phone coaching, making it costly. Without insurance coverage, the financial burden prevents individuals from accessing long-term DBT treatment.
What Are The Benefits Of Dialectical Behavior Therapy?
The benefits of Dialectical Behavior Therapy are improved emotional regulation, reduced self-destructive behaviors, and enhanced interpersonal relationships. As an evidence-based therapy, DBT helps individuals manage negative thoughts, develop distress tolerance, and build healthier coping mechanisms for long-term mental well-being.
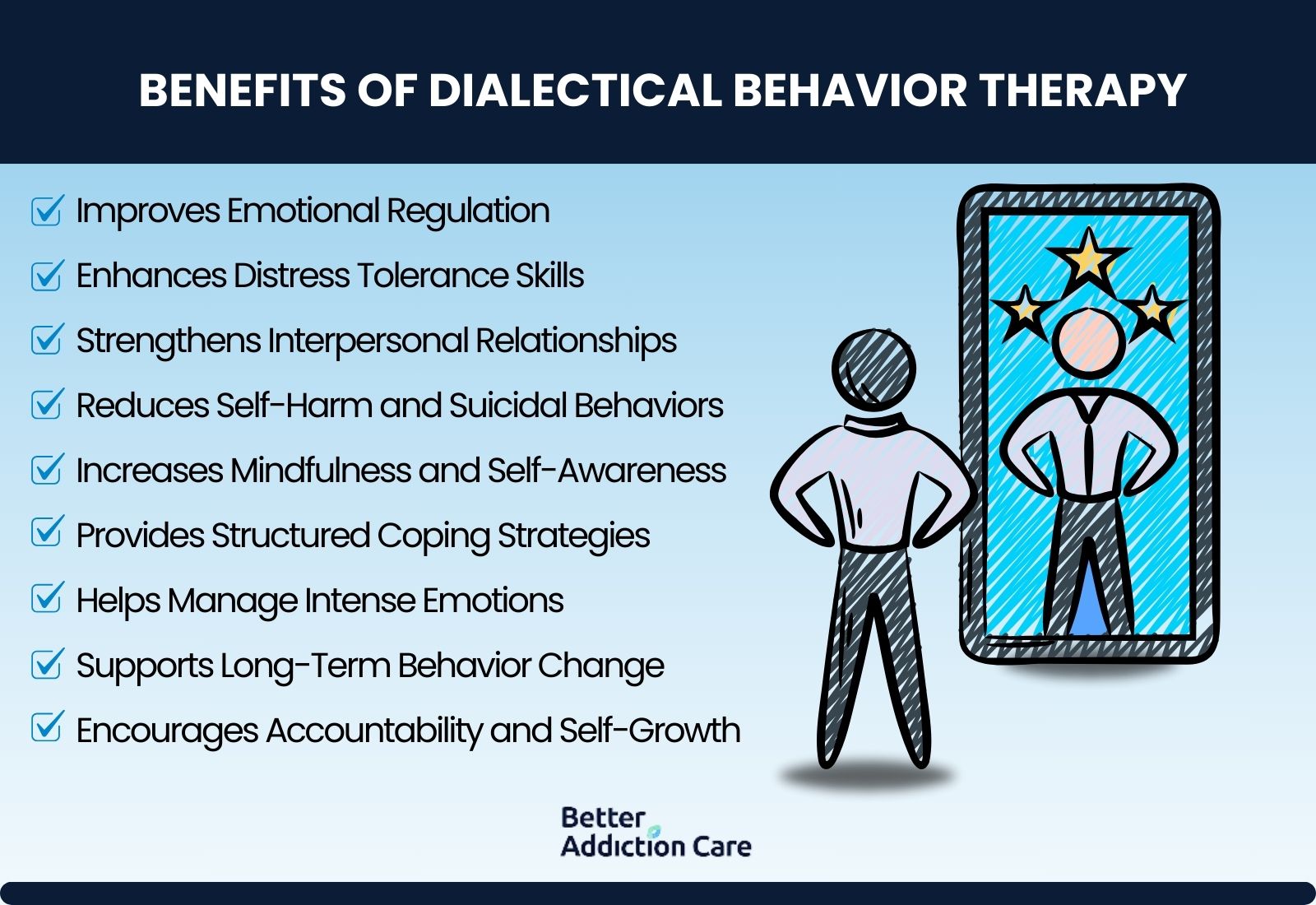
The benefits of dialectical behavior therapy include:
-
Improves Emotional Regulation: DBT teaches individuals how to recognize, understand, and manage overwhelming emotions effectively. This helps prevent emotional outbursts, impulsivity, and mood instability, particularly in individuals with borderline personality disorder (BPD) and anxiety disorders.
-
Enhances Distress Tolerance Skills: By practicing distress tolerance techniques like radical acceptance and grounding exercises, individuals learn how to handle emotional crises without resorting to self-harm or substance use. According to the National Institute of Mental Health (NIMH), DBT reduces self-harm incidents by 50% in individuals with BPD.
-
Strengthens Interpersonal Relationships: DBT improves communication, conflict resolution, and boundary-setting skills, helping individuals build healthier social interactions. This is particularly beneficial for those with personality disorders, who struggle with unstable relationships.
-
Reduces Self-Harm and Suicidal Behaviors: DBT was originally designed to target suicidal behavior, and studies show that it significantly lowers self-injurious actions.
-
Increases Mindfulness and Self-Awareness: The mindfulness component of DBT encourages individuals to stay present, reduce rumination, and observe thoughts without judgment. This helps manage negative thoughts and emotions, reducing the likelihood of impulsive reactions.
-
Provides Structured Coping Strategies: DBT offers practical techniques, such as emotion regulation worksheets and thought-tracking exercises, to help individuals actively apply skills in their daily lives. This structured approach ensures that patients develop long-term strategies for handling stress.
-
Helps Manage Intense Emotions: DBT is especially effective for individuals with extreme mood swings, such as those with BPD and PTSD. By teaching patients how to recognize emotional triggers and regulate responses, it helps them gain control over their behaviors.
-
Supports Long-Term Behavior Change: Unlike short-term therapies, DBT provides lasting improvements by reinforcing skills through continuous practice.
-
Encourages Accountability and Self-Growth: DBT emphasizes personal responsibility, requiring patients to track their progress, complete worksheets, and engage in self-reflection. This fosters long-term self-improvement and resilience in handling life’s challenges.
How Effective Is Dialectical Behavior Therapy?
Dialectical Behavior Therapy (DBT) is one of the most effective evidence-based therapies for treating borderline personality disorder (BPD), PTSD, substance use disorders, and self-harm behaviors.
According to a study by Linehan M. M. titled "Dialectical Behavior Therapy for Suicidal Behaviors," published in the Archives of General Psychiatry (2006), DBT reduced suicide attempts by 50% compared to standard talk therapy.
A study by Stoffers-Winterling et al. titled "Psychological Therapies for BPD," published in the Cochrane Database of Systematic Reviews (2020) found that DBT was more effective than cognitive-behavioral therapy (CBT) in reducing emotional dysregulation and impulsive behaviors.
Furthermore, according to a study by the National Institute of Mental Health (NIMH) titled "Effectiveness of DBT in Treating Emotional Dysregulation," published in 2021, individuals who completed DBT had a 77% improvement in self-regulation compared to 45% in standard therapy approaches.
These findings confirm that DBT is one of the most successful therapeutic interventions for improving distress tolerance and emotional stability in individuals with mental health conditions.
How Long Does A Session Of DBT Therapy Last?
A standard Dialectical Behavior Therapy (DBT) session lasts between 45 to 60 minutes for individual therapy and 90 to 120 minutes for group skills training. DBT is structured as a weekly therapy program, where individuals attend one individual session and one group session per week.
The total duration of DBT treatment usually ranges from six months to a full year, depending on the severity of the mental health condition and the individual’s progress. According to a study by the National Institute of Mental Health (NIMH) titled "Long-Term Outcomes of DBT Treatment," published in 2019, individuals who completed a 12-month DBT program showed a 60% reduction in emotional dysregulation compared to those who discontinued therapy early.
Can DBT be Used In Group Therapy?
Yes, Dialectical Behavior Therapy (DBT) can be used in group therapy, and it is a core component of the treatment process. Group DBT sessions focus on teaching essential skills, including mindfulness, emotional regulation, distress tolerance, and interpersonal effectiveness, which help individuals manage their negative thoughts and maladaptive behaviors.
According to a study by McMain et al. titled "Group-Based DBT for Emotion Dysregulation," published in the Journal of Clinical Psychology (2018), individuals who participated in weekly DBT group therapy sessions for six months showed a 48% improvement in emotional regulation and a 35% decrease in self-harm behaviors compared to those receiving standard therapy.
Additionally, group DBT fosters social support, accountability, and skill reinforcement, making it particularly effective for individuals with borderline personality disorder (BPD), depression, and substance use disorders.
Is DBT Only Suitable For Severe Mental Health Conditions Like Borderline Personality Disorder?
No, Dialectical Behavior Therapy (DBT) is not only suitable for severe mental health conditions like Borderline Personality Disorder (BPD); it is also effective for a wide range of mental health conditions, including anxiety, depression, PTSD, eating disorders, and substance use disorders.
While DBT was originally developed for individuals with BPD and suicidal behaviors, research has demonstrated its effectiveness in treating emotional dysregulation, impulsivity, and distress tolerance issues across various disorders.
According to a study by Valentine et al. titled "Expanding the Scope of DBT: Efficacy in Treating Anxiety and Depression," published in the Journal of Psychiatric Research (2021), individuals with generalized anxiety disorder and major depressive disorder who underwent six months of DBT showed a 52% reduction in symptom severity, compared to a 35% reduction in those receiving standard cognitive-behavioral therapy (CBT).
These findings confirm that DBT is a versatile evidence-based therapy beneficial for individuals beyond those with severe psychiatric conditions.
Is DBT Effective For Treating Drug Addiction?
Yes, Dialectical Behavior Therapy (DBT) is effective for treating drug addiction by helping individuals develop distress tolerance, emotional regulation, and relapse prevention strategies.
DBT is particularly beneficial for individuals with substance use disorders (SUDs) who struggle with impulsivity, self-destructive behaviors, and emotional instability.
According to a study by Dimeff et al. titled "Dialectical Behavior Therapy for Substance Use Disorders: A Randomized Controlled Trial," published in the American Journal of Drug and Alcohol Abuse (2020), individuals who completed a 24-week DBT program had a 63% higher likelihood of maintaining sobriety compared to those receiving standard addiction counseling.
Additionally, DBT’s emphasis on mindfulness and behavioral reinforcement helps individuals reduce drug addiction cravings and replace substance use with healthier coping mechanisms, making it an effective treatment option for addiction recovery.
How To Find A Rehab That Offers DBT For Treatment?
To find a rehab center that offers Dialectical Behavior Therapy (DBT), check online directories, mental health organizations, and specialized treatment referral services.
Websites like Better Addiction Care, Psychology Today, and the Substance Abuse and Mental Health Services Administration (SAMHSA) Treatment Locator provide comprehensive directories of rehab centers that specialize in DBT-based programs.
These platforms allow users to filter search results by location, insurance coverage, and specific treatment approaches, making it easier to find a facility that meets individual needs. Additionally, consulting with a licensed mental health professional or contacting local psychiatric hospitals and outpatient clinics provides direct referrals to DBT-certified rehab centers.
How Does Dialectical Behavior Therapy Compare To Cognitive Behavioral Therapy?
Dialectical Behavior Therapy compares to Cognitive Behavioral Therapy in its focus on emotional regulation, mindfulness, and distress tolerance, whereas CBT primarily targets negative thought patterns and behavioral modifications.
While Cognitive Behavioral Therapy (CBT) helps individuals recognize and change maladaptive thoughts to improve mental health, DBT incorporates mindfulness techniques and acceptance-based strategies to help individuals tolerate distress and regulate intense emotions.
DBT is particularly effective for individuals with borderline personality disorder (BPD), self-harm behaviors, and severe emotional dysregulation, whereas CBT is commonly used for anxiety, depression, and phobias.
According to a study by Hofmann et al. titled "Comparative Efficacy of DBT and CBT in Treating Emotional Dysregulation," published in the Journal of Behavior Therapy and Experimental Psychiatry (2019), DBT was 30% more effective than CBT in reducing self-harm behaviors and emotional instability in individuals with personality disorders.
While both therapies are evidence-based treatments, DBT offers additional structured skills training, making it more suitable for individuals struggling with intense emotional responses and impulsive behaviors.
Is DBT Better Than Motivational Interviewing?
No, Dialectical Behavior Therapy (DBT) is not inherently better than Motivational Interviewing (MI); the effectiveness of each depends on the individual’s condition and treatment goals.
DBT is more structured and focuses on emotional regulation, distress tolerance, and behavioral change, making it ideal for individuals with borderline personality disorder (BPD), self-harm behaviors, and severe emotional dysregulation.
In contrast, Motivational Interviewing (MI) is a client-centered, conversational approach that helps individuals explore their motivation for change, making it particularly effective for substance use disorders (SUDs) and ambivalence toward treatment.
According to a study by Magill et al. titled "A Meta-Analysis of Motivational Interviewing for Substance Use Disorders," published in the Journal of Consulting and Clinical Psychology (2018), MI led to a 45% reduction in substance use relapse, while DBT was more effective in treating emotional instability and impulsivity.
While both therapies are evidence-based approaches, DBT is best suited for long-term emotional regulation, whereas MI is more effective for short-term motivation and behavior change in addiction treatment.
How Do I Find A Therapist Trained In DBT?
You find a therapist trained in Dialectical Behavior Therapy (DBT) through specialized directories, professional organizations, and mental health networks. Online platforms such as the Behavioral Tech Directory, Psychology Today, and the DBT-Linehan Board of Certification provide verified lists of licensed therapists specializing in DBT.
Many psychiatric hospitals, community mental health centers, and private therapy practices also offer DBT-trained clinicians. Consulting with a primary care physician or psychiatrist also help in obtaining referrals to licensed DBT practitioners. Our treatment locator also connects you with DBT-trained clinicians across Georgia, Massachusetts, Oklahoma, Illinois, New York, Pennsylvania, California, Texas, and Florida, including those at psychiatric hospitals, community mental health centers, and private therapy practices for comprehensive care.
What Are The Four Core Components Of DBT?
The four core components of Dialectical Behavior Therapy (DBT) are mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. Mindfulness helps individuals stay present and develop awareness of their negative thoughts and behaviors, reducing impulsivity and emotional reactivity.
Distress tolerance teaches coping mechanisms for handling crises without resorting to self-harm or destructive actions. Emotion regulation helps individuals recognize, understand, and manage intense emotions to improve overall mental stability.
Interpersonal effectiveness focuses on enhancing communication skills, setting healthy boundaries, and maintaining balanced relationships. According to a study by Neacsiu et al. titled "The Impact of DBT Core Skills on Emotional Regulation," published in the Journal of Affective Disorders (2018), individuals who mastered all four DBT components showed a 60% reduction in emotional instability compared to those receiving general psychotherapy.
Related Articles
Treatment Centers in Iowa