Drug Detox: Definition, Medications, Process, Side Effects
Drug detox is the first step in overcoming substance addiction, where the body clears itself of harmful toxins. This medically supervised process helps stabilize individuals physically and mentally, preparing them for ongoing addiction treatment and recovery. Detox addresses withdrawal symptoms and reduces immediate health risks. According to the Center for Substance Abuse Treatment (CSAT), 2006, "Detoxification and Substance Abuse Treatment," states that 40% to 60% of individuals relapse within the first year after detox.

Drug detox is the first step in overcoming substance addiction, where the body clears itself of harmful toxins. This medically supervised process helps stabilize individuals physically and mentally, preparing them for ongoing addiction treatment and recovery. Detox addresses withdrawal symptoms and reduces immediate health risks. According to the Center for Substance Abuse Treatment (CSAT), 2006, "Detoxification and Substance Abuse Treatment," states that 40% to 60% of individuals relapse within the first year after detox.
Medications used during drug detox include methadone, buprenorphine, and clonidine for opioids; benzodiazepines for alcohol withdrawal; and supportive medications for stimulants like cocaine and methamphetamines. These drugs help ease withdrawal symptoms, prevent complications, and make the detox process safer and more tolerable for patients.
The drug detox process involves an initial evaluation, stabilization through medical and psychological support, and preparation for further addiction treatment. Medical professionals monitor vital signs, administer necessary medications, and manage withdrawal symptoms to ensure a safe and more comfortable detoxification experience. Detox duration varies by substance: 4 to 10 days for opioids, 5 to 7 days for alcohol, and up to 4 weeks for benzodiazepines.
The side effects of drug detox include nausea, anxiety, sweating, insomnia, digestive issues, seizures, and intense cravings. These symptoms vary depending on the substance involved, the duration of use, and individual health factors, highlighting the need for professional medical supervision during detox.
What is Drug Detox?
Drug detox is a medically supervised process that helps individuals safely clear addictive substances from their bodies while managing acute withdrawal symptoms. It marks the first stage in the addiction recovery journey, laying the groundwork for ongoing treatment. The primary goal of drug detox is to stabilize the patient by alleviating withdrawal discomfort and preventing severe medical complications.
Detox protocols vary based on the substance involved, lasting about 4 to 10 days for opioids, 5 to 7 days for alcohol, and 2 to 4 weeks or longer for benzodiazepines. Medications such as benzodiazepines for alcohol withdrawal, methadone or buprenorphine for opioid dependence, and tapering strategies for benzodiazepines are commonly used to reduce withdrawal symptoms like seizures, anxiety, and cravings.
However, detox alone does not ensure lasting recovery; without follow-up care, 65% to 80% of individuals relapse within six months. Comprehensive addiction treatment following detox is important for sustained recovery, as highlighted in the study by Kosten, T. R., & O'Connor, P. G. et al. 2003, titled "Management of Drug and Alcohol Withdrawal."
What Medications Are Used in Drug Detox?
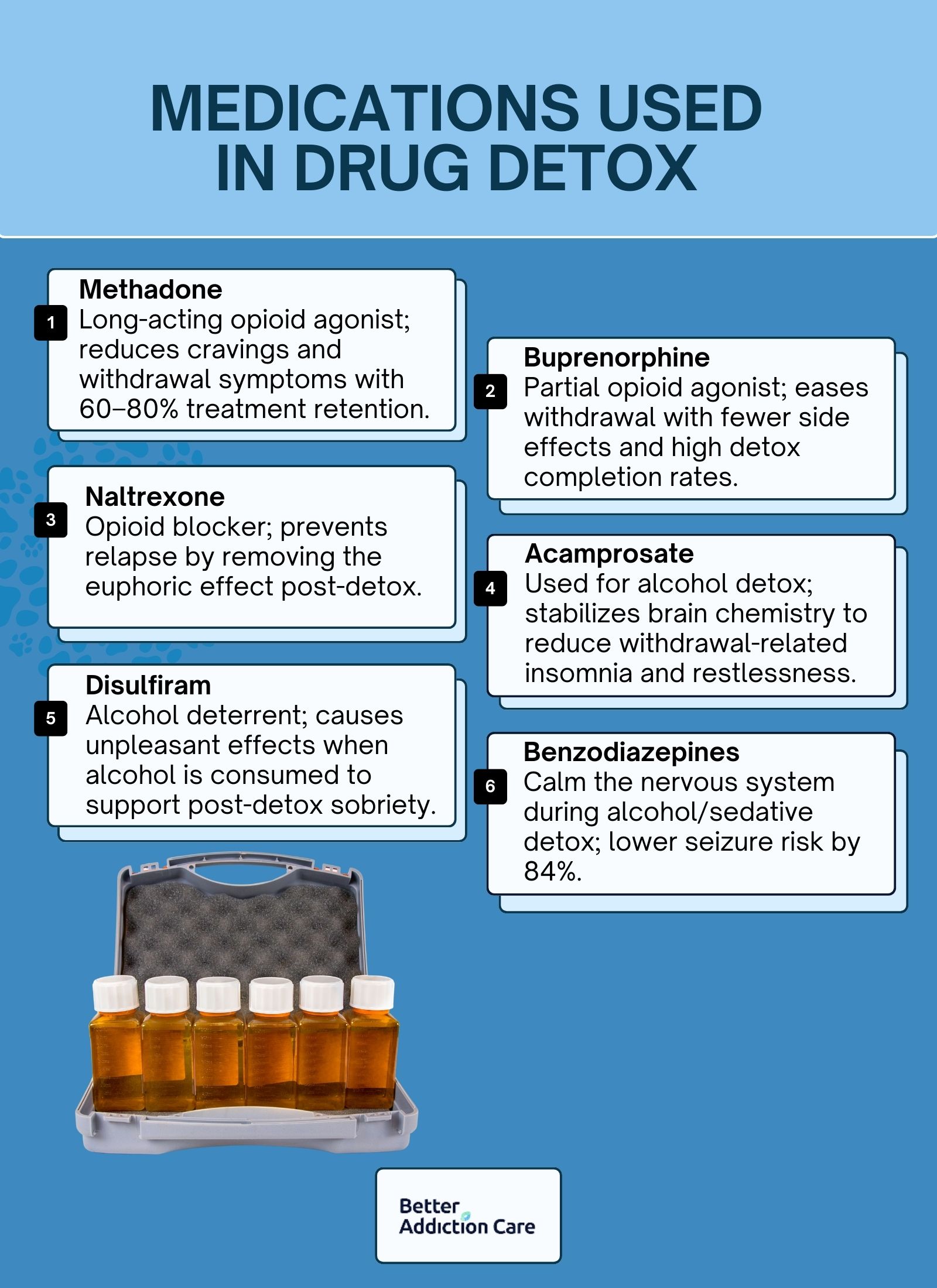
The medications used in drug detox are methadone, buprenorphine, naltrexone, acamprosate, disulfiram, and benzodiazepines. These medications are important tools in managing withdrawal symptoms, minimizing cravings, and preventing potentially life-threatening complications during the detox process. Used as part of Medication-Assisted Treatment (MAT), they support brain stabilization and increase the likelihood of long-term recovery when combined with psychosocial interventions. According to Lingford-Hughes, A. R. et al. 2012 in the study titled "BAP Updated Guidelines: Evidence-Based Guidelines for the Pharmacological Management of Substance Abuse, Harmful Use, Addiction, and Comorbidity," these medications significantly improve detox outcomes and reduce relapse rates.
Common medications used in drug detox are given below:
-
Methadone (Brand Name: Dolophine®): Methadone is a long-acting opioid agonist that binds to the brain's opioid receptors to reduce withdrawal symptoms and cravings without producing euphoria. It is widely used in opioid detox, particularly for heroin and prescription painkiller addiction. According to Schuckit, M. A. 2016 in the study titled "Treatment of Opioid-Use Disorders," methadone achieves retention rates of 60% to 80% in treatment programs over six months, demonstrating its effectiveness in opioid detoxification. It is administered daily in controlled settings to ensure safety and reduce misuse.
-
Buprenorphine (Brand Name: Subutex®, Suboxone® when combined with naloxone): Buprenorphine is a partial opioid agonist that partially activates opioid receptors, helping to relieve cravings and withdrawal symptoms with a reduced risk of respiratory depression. Compared to methadone, it offers similar efficacy with a better safety profile. A Cochrane review by Gowing, L., Ali, R., & White, J. M. 2014 in the study titled "Pharmacological Strategies for Detoxification," found that buprenorphine significantly increases detox completion rates when compared to non-opioid alternatives, making it a first-line treatment option in opioid withdrawal management.
-
Naltrexone (Brand Name: Vivitrol®, Revia®): Naltrexone is an opioid antagonist that blocks the effects of opioids at receptor sites, discouraging relapse by removing any euphoric effect. It is used after detox to prevent relapse but plays a role in detox planning, especially for those with high relapse risk. A randomized study by Krupitsky E, Zvartau E, Woody G. et al. 2010, titled "Use of naltrexone to treat opioid addiction in a country in which methadone and buprenorphine are not available," demonstrated that extended-release naltrexone significantly improved opioid abstinence rates compared to placebo, reinforcing its value in post-detox relapse prevention.
-
Acamprosate (Brand Name: Campral®): Acamprosate is explicitly used for alcohol detox and works by stabilizing chemical signaling in the brain that is disrupted during alcohol withdrawal. It reduces symptoms such as restlessness, insomnia, and dysphoria. Research by Mason BJ, Lehert P. et al. 2011, titled "Acamprosate for alcohol dependence: a sex-specific meta-analysis based on individual patient data," found that acamprosate significantly increased alcohol abstinence rates compared to placebo when used in combination with psychosocial support, making it a key medication in alcohol use disorder recovery.
-
Disulfiram (Brand Name: Antabuse®): Disulfiram is used as a deterrent in alcohol detox by causing unpleasant symptoms (such as nausea, flushing, and palpitations) when alcohol is consumed. It works by inhibiting aldehyde dehydrogenase, the enzyme involved in alcohol metabolism. While not used to manage withdrawal directly, disulfiram supports abstinence after detox. A meta-analysis by Skinner MD, Lahmek P, Pham H, Aubin HJ. et al. 2014, titled "Disulfiram efficacy in the treatment of alcohol dependence: a meta-analysis," showed that disulfiram is effective in promoting sobriety in highly motivated individuals when adherence is maintained.
-
Benzodiazepines (e.g., Valium®, Ativan®): Benzodiazepines, including diazepam (Valium®) and lorazepam (Ativan®), are central nervous system depressants commonly prescribed to treat withdrawal symptoms from alcohol and sedatives. They help control agitation, anxiety, and reduce the risk of seizures during the detox process. Considered the gold standard for managing alcohol withdrawal, benzodiazepines have been shown to reduce seizure risk by 84% compared to placebo. These medications are typically administered in carefully tapered doses under medical supervision to minimize the risk of dependency or misuse.
What Is the Process of Drug Detox?
The process of drug detox includes medically supervised steps aimed at managing withdrawal safely and preparing individuals for long-term recovery. It unfolds in three stages: evaluation, stabilization, and transition to treatment, each important to laying the foundation for successful addiction care.
The drug detoxification process includes the following steps:
-
Evaluation: This initial phase involves a thorough medical and psychological assessment. Healthcare professionals review the individual's substance use history, perform blood tests, evaluate withdrawal risk, and screen for co-occurring mental health conditions. These insights guide the creation of a personalized detox plan tailored to the individual's needs.
-
Stabilization: In this phase, medical interventions, such as medications, hydration, and supportive care, reduce withdrawal symptoms and restore physical and emotional balance. Stabilization lasts several days to weeks, depending on the substance involved, and ensures that the patient is safe and medically stable before proceeding.
-
Transition to Treatment: After stabilization, patients are introduced to the subsequent recovery phase, such as inpatient rehab, outpatient programs, or therapy-based interventions like Cognitive Behavioral Therapy (CBT) or Medication-Assisted Treatment (MAT). This step ensures continuity of care and helps prevent relapse. According to the CDC and NIDA (2024), approximately 75% of people who receive structured addiction treatment eventually recover.
What Are the Side Effects of Drug Detox?
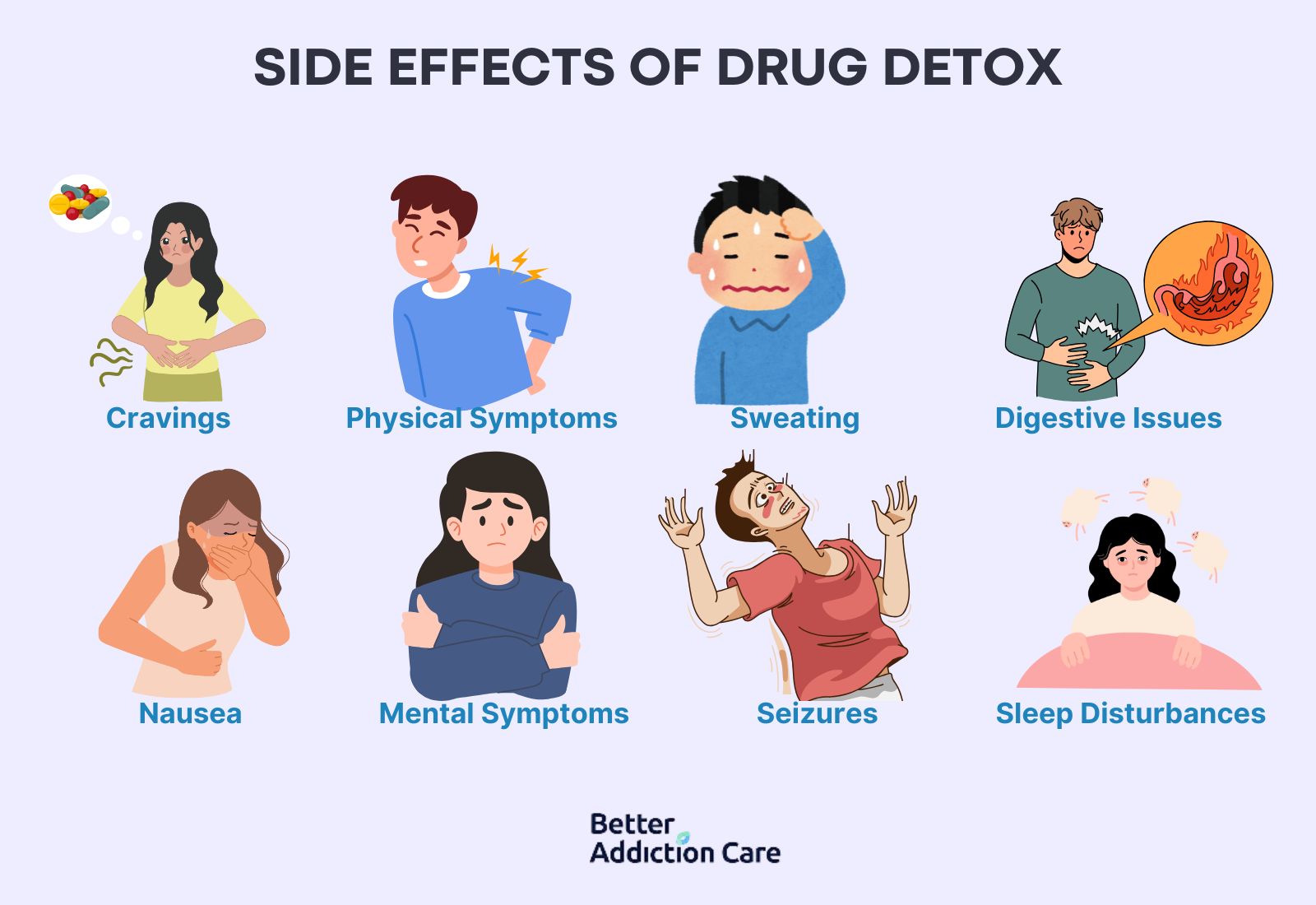
The side effects of drug detox are cravings, physical discomfort, mental health symptoms, digestive issues, sleep disturbances, sweating, nausea, and seizures. These symptoms arise as the body and brain react to the sudden absence of addictive substances, with intensity depending on the type of substance, usage duration, and individual health status.
The side effects of drug detox are given below:
-
Cravings: Cravings are intense urges or desires to use the drug again, triggered by physical discomfort or emotional distress during detox. They are persistent and powerful, making relapse a significant risk if cravings are not managed with medication or behavioral therapies.
-
Physical Symptoms: Physical symptoms such as muscle aches, sweating, chills, and tremors are common side effects during detox. These are caused by the body's attempt to regulate itself without the influence of addictive substances, particularly during opioid, alcohol, and benzodiazepine withdrawal.
-
Mental Symptoms: Mental health disturbances like anxiety, depression, irritability, and paranoia frequently emerge during detox. The brain's chemical balance is disrupted by long-term substance use, making psychological symptoms particularly challenging. Benzodiazepines, for instance, are used to manage anxiety and reduce seizure risks by up to 84% during alcohol detox, as studied by Bounds CG, Patel P. et al., 2024, titled "Benzodiazepines."
-
Digestive Issues: Digestive problems, including nausea, vomiting, diarrhea, and abdominal cramps, are common, especially in opioid and alcohol detox. These symptoms lead to dehydration and electrolyte imbalances if not adequately treated.
-
Sleep Disturbances: Difficulty falling asleep, staying asleep, or experiencing restful sleep occurs during withdrawal. Insomnia prolongs detox discomfort and heightens emotional instability, making recovery more difficult without appropriate interventions.
-
Sweating: Excessive sweating is a physical reaction to withdrawal, particularly common during alcohol and opioid detox. It is part of the body's autonomic instability response. During alcohol withdrawal, about 75% of individuals experience tremors, and approximately 25% develop an increased heart rate. Schuckit documents this, M. A. et al. 2016, in the study "Alcohol-Use Disorders."
-
Nausea: Nausea, a frequent detox side effect, emerges in the early stages of withdrawal and is severe enough to cause vomiting. Opioid withdrawal, in particular, is associated with intense gastrointestinal upset, which requires medical support to prevent complications such as dehydration.
-
Seizures: Seizures represent a severe and life-threatening risk during detox, particularly in alcohol and benzodiazepine withdrawal. Around 3% to 5% of patients undergoing alcohol detox experience seizures or delirium tremens if they do not receive proper medical care. The use of benzodiazepines reduces this risk by 84%, as cited by Lingford-Hughes, A. R. et al. 2012, titled "BAP Updated Guidelines: Evidence-Based Guidelines for the Pharmacological Management of Substance Abuse, Harmful Use, Addiction, and Comorbidity."
What Are the Side Effects of Drug Detoxification on Pregnant Women?
The side effects of drug detoxification on pregnant women are miscarriage, preterm labor, fetal distress, and stillbirth. Drug detox during pregnancy triggers severe withdrawal symptoms not only in the mother but also in the fetus, leading to complications such as uterine contractions, placental abruption, or restricted fetal growth. According to the American College of Obstetricians and Gynecologists (ACOG), abrupt withdrawal from substances like opioids causes fetal distress and increases the risk of pregnancy loss, highlighting the importance of medically supervised detox protocols.
What Drugs Are Required for a Medically Supervised Detox?
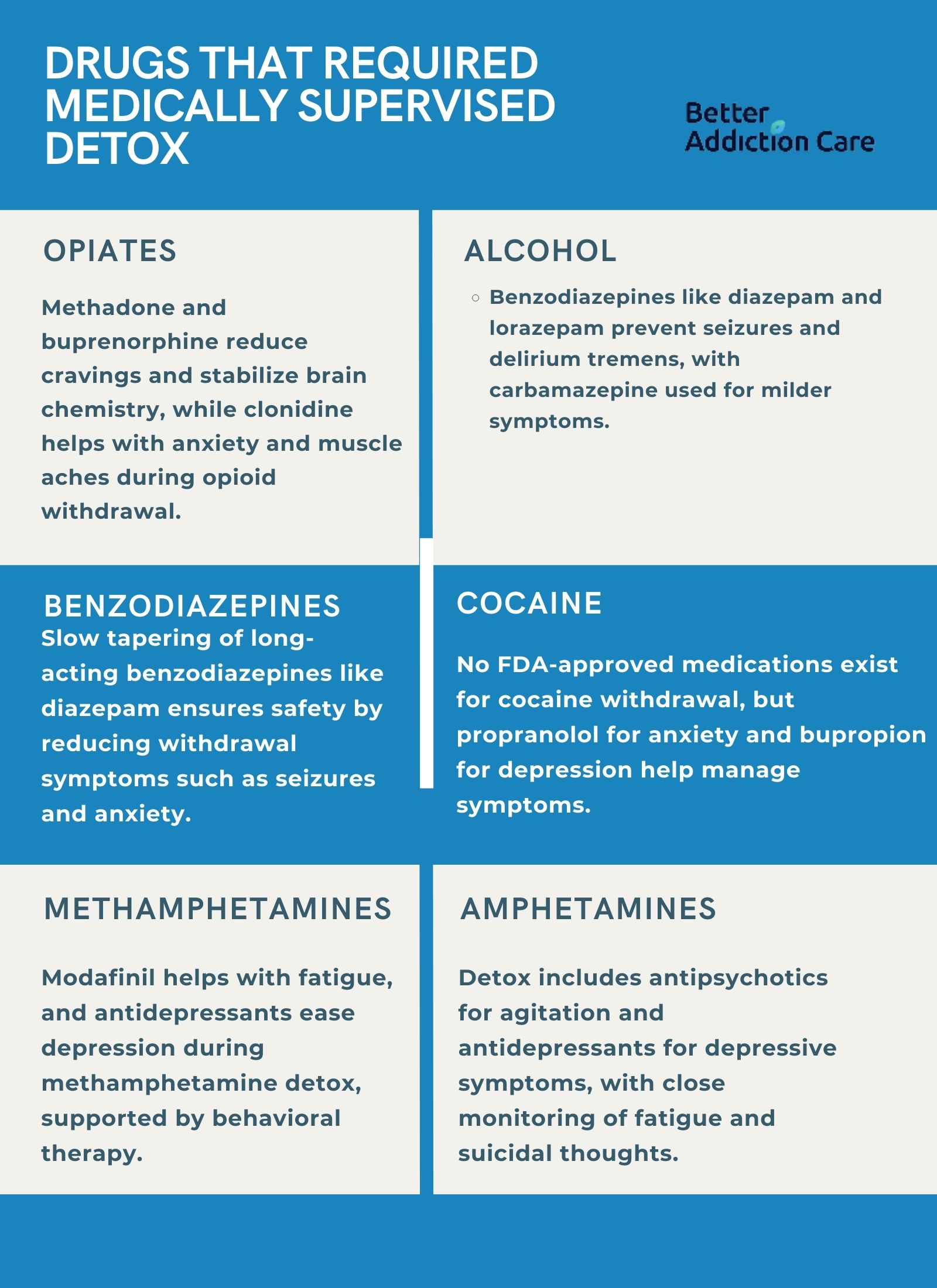
The drugs required for a medically supervised detox include methadone, buprenorphine, and clonidine for opioids; benzodiazepines and anticonvulsants for alcohol; tapering benzodiazepines for sedative withdrawal; and supportive medications for stimulant detox from cocaine, amphetamines, and methamphetamines. A medically supervised detox ensures safety by managing severe withdrawal symptoms and reducing the risks of complications like seizures, heart issues, or psychological crises.
The following drugs are required for a medically supervised detox:
-
Opiates: Medications like methadone (brand name: Methadose) and buprenorphine (brand name: Subutex, Suboxone) are used to manage opioid withdrawal symptoms. They reduce cravings, stabilize brain chemistry, and lower the risk of relapse. Clonidine is sometimes added to lessen anxiety, agitation, and muscle aches during detox.
-
Alcohol: Benzodiazepines such as diazepam (Valium) and lorazepam (Ativan) are the mainstay for alcohol detox to prevent seizures and delirium tremens. In some cases, anticonvulsants like carbamazepine are used as alternatives, especially for milder withdrawal symptoms.
-
Benzodiazepines: A slow tapering of long-acting benzodiazepines, such as diazepam, is used during detox to avoid severe withdrawal effects like seizures, psychosis, and intense anxiety. The goal is to gradually reducing the dose under medical supervision to ensure safety.
-
Cocaine: While there are no FDA-approved medications to specifically treat cocaine withdrawal, supportive drugs such as propranolol for anxiety or antidepressants like bupropion are used. These medications help manage mood swings, agitation, and cravings during early detox.
-
Amphetamines: Detox from amphetamines involves the use of supportive therapies, including antipsychotics for severe agitation or psychosis and antidepressants to manage depressive symptoms. Careful monitoring is important because withdrawal of opioids causes intense fatigue, depression, and suicidal thoughts.
-
Methamphetamines: Similar to amphetamine detox, there are no specific medications approved for methamphetamine withdrawal. However, doctors use medicines like modafinil to help with extreme sleepiness and antidepressants to ease depressive symptoms. Behavioral support is also significant during this process.
How Long Does Drug Detoxification Take?
It takes a few days to several weeks for drug detoxification, depending on the substance, the severity of dependence, and individual health factors. Each type of drug has a different withdrawal timeline, with symptoms ranging from mild to severe throughout the detox process. Medical supervision helps manage symptoms safely during this period.
The following are the timelines for drug detoxification for the following drugs:
-
Opiates: Opiate detox usually starts within 6 to 12 hours after the last use and peaks at around 72 hours. Most physical symptoms resolve within 5 to 7 days, though psychological cravings persist longer. Drugs like heroin and prescription opioids follow this general timeline.
-
Alcohol: Alcohol detox symptoms begin as early as 6 hours after the last drink. Acute withdrawal lasts between 5 and 7 days, but more severe cases like delirium tremens occur within 48 to 72 hours and require extended medical care.
-
Benzodiazepines: Benzodiazepine detox takes much longer, with withdrawal symptoms beginning within 1 to 4 days after stopping use. Acute withdrawal lasts 10 to 14 days, but protracted symptoms like anxiety and insomnia linger for several weeks or even months in some cases.
-
Cocaine: Cocaine detox symptoms emerge within hours of last use. The acute withdrawal phase, marked by intense cravings and mood disturbances, usually lasts around 7 to 10 days, though psychological symptoms like depression persist for weeks.
-
Amphetamines: Withdrawal from amphetamines begins within 24 hours after last use and peaks within 2 to 3 days. Most symptoms, including fatigue and depression, subside within 7 to 10 days, although some emotional symptoms continue for several weeks.
-
Methamphetamines: Methamphetamine detox follows a similar timeline to amphetamines, but is more intense. Symptoms start within 24 hours, peak at about 2 to 3 days, and diminish over 7 to 14 days. Depression, anxiety, and cravings linger longer and require ongoing support.
Can You Detox From Drugs at Home?
No, you cannot detox from drugs at home, as it is not recommended, especially for substances like alcohol, benzodiazepines, or opioids that cause life-threatening withdrawal symptoms. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), medical supervision during detox is essential to ensure safety, manage severe symptoms, and increase the chances of long-term recovery. Without professional care, individuals risk seizures, dehydration, psychiatric complications, or even death.
What Is Rapid Detox?
Rapid detox is a medical procedure where a person is sedated under anesthesia while medications flush drugs like opioids from their system quickly, within 4 to 6 hours. People seek rapid detox to avoid experiencing the intense discomfort of traditional withdrawal symptoms. However, while the physical detoxification is faster, the emotional and psychological recovery still requires ongoing therapy. Rapid detox takes less than a day, but complete stabilization needs additional days of observation.
Is Rapid Detox Safe?
No, rapid detox is not considered entirely safe. It carries serious risks, including heart attack, choking, aspiration pneumonia, paranoia, and even death. Studies cited by the American Society of Addiction Medicine (ASAM) report death rates associated with anesthesia-assisted rapid detox ranging from 1% to 3%, making it a high-risk procedure. Moreover, rapid detox does not address the underlying psychological aspects of addiction, leading to relapse.
What Are the Treatment Options After Drug Detox?
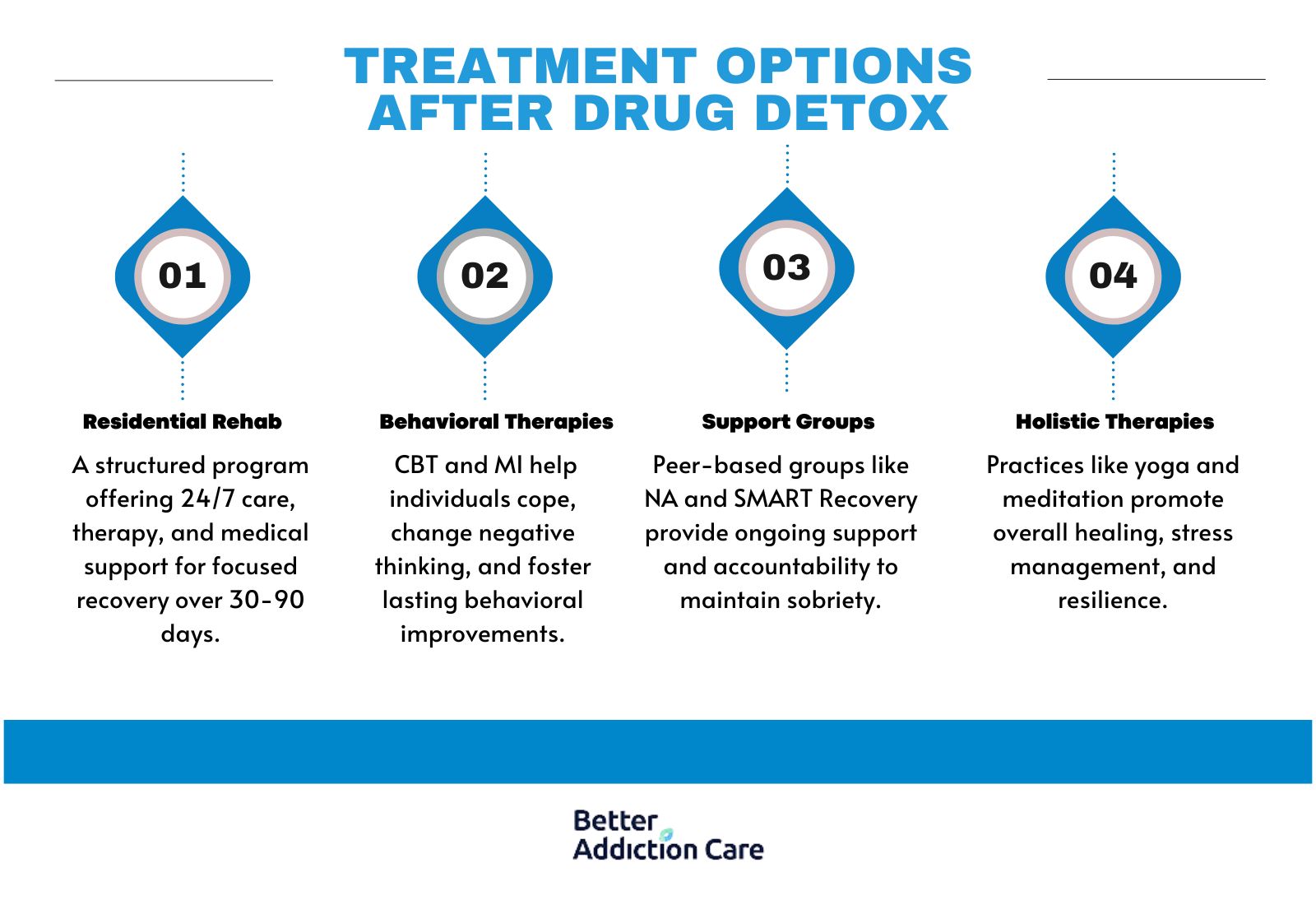
The treatment options after drug detox are inpatient rehab, behavioral therapies, holistic therapies, and support groups. These treatment options are important to prevent relapse and support long-term recovery. Detox alone only addresses the physical aspect of addiction; ongoing treatment helps individuals rebuild healthy habits, manage triggers, and strengthen mental health.
The treatment options after drug detox include:
-
Residential Rehab: Residential rehab provides 24/7 care in a structured, therapeutic environment. Programs last 30, 60, or 90 days, including therapy, medical care, and skill-building activities. This setting helps individuals focus entirely on recovery without outside distractions.
-
Behavioral Therapies: Behavioral therapies, such as Cognitive Behavioral Therapy (CBT) and Motivational Interviewing (MI), teach coping skills, address negative thought patterns, and encourage long-term behavior change. These therapies are important for understanding addiction triggers and building healthier responses.
-
Support Groups: Support groups like Narcotics Anonymous (NA) and SMART Recovery offer peer support, accountability, and a community of people who share similar struggles. Regular meetings provide encouragement and strategies to maintain sobriety over the long term.
-
Holistic Therapies: Holistic therapies include yoga, meditation, acupuncture, and art therapy. These treatments focus on healing the mind, body, and spirit, helping individuals manage stress, build resilience, and reconnect with themselves during recovery.
How to Find a Good Drug Detox Center?
To find a good drug detox center, search for licensed and accredited facilities in your state that offer medically supervised detox programs. Look for centers that provide personalized care plans, experienced staff, and transition support into ongoing treatment. You can also use a treatment locator of trusted online directories to find top-rated detox centers near you.
Does Insurance Cover Drug Detox?
Yes, most insurance plans do cover drug detox because it is considered a medically necessary service for treating substance use disorders. Coverage includes both inpatient and outpatient detox services, though the extent of coverage varies by provider and plan. You must verify your insurance coverage.
Related Articles
Treatment Centers in Virginia







