Drug Interaction: Definition, Types, Symptoms
Drug interactions occur when one drug affects the way another drug works, potentially altering its effectiveness or increasing the risk of side effects. These interactions involve prescription medications, over-the-counter drugs, supplements, or even certain foods and beverages, making awareness necessary for safe medication use.

Drug interactions occur when one drug affects the way another drug works, potentially altering its effectiveness or increasing the risk of side effects. These interactions involve prescription medications, over-the-counter drugs, supplements, or even certain foods and beverages, making awareness necessary for safe medication use.
A study by Hughes JE, Bennett KE, Cahir C. et al. 2024, titled “Drug-Drug Interactions and Their Association with Adverse Health Outcomes in the Older Community-Dwelling Population: A Prospective Cohort Study” found that the prevalence of potentially clinically important drug-drug interactions (DDIs) in older adults increased from 23.3% to 45.2% over two years, with DDI exposure associated with a 26% increase in adverse drug events (ADEs) and a decline in health-related quality of life (HRQoL).
There are several types of drug interactions, including drug-drug interactions, where two or more medications interact; drug-food interactions, where certain foods impact drug absorption or metabolism; and drug-supplement interactions, where herbal or dietary supplements interfere with medication effects. Each type either enhances, reduces, or causes unintended side effects of a drug.
The main symptoms of drug interactions vary but include nausea, dizziness, confusion, irregular heartbeat, and changes in blood pressure. In severe cases, interactions lead to life-threatening conditions such as respiratory depression or seizures. Recognizing these symptoms early and consulting a healthcare provider help prevent complications.
What Is a Drug Interaction?
A drug interaction is when a drug's effects are altered by the presence of another substance, such as another drug, food, beverage, or supplement. These interactions enhance or reduce the intended effect of a medication, leading to potential health risks or reduced efficacy. Some drug interactions cause harmful side effects, while others increase the therapeutic benefits of a medication.
According to the U.S. Food and Drug Administration (FDA), nearly 2 million adverse drug reactions (ADRs) occur each year in the United States, with many resulting from drug interactions. A study published in the Journal of the American Medical Association (JAMA) found that hospitalized patients have a 20% to 30% risk of experiencing a drug interaction, and this risk increases with the number of medications taken.
Drug interactions can be classified into three main types: drug-drug interactions, where two or more medications interact; drug-food interactions, where certain foods affect medication absorption or effectiveness (e.g., grapefruit interfering with statins); and drug-supplement interactions, where vitamins or herbal products alter drug metabolism. The consequences of these interactions range from mild discomfort to life-threatening complications, such as organ failure, increased toxicity, or reduced treatment effectiveness.
High-risk populations include elderly individuals, patients with chronic conditions, and those taking multiple medications (polypharmacy). The World Health Organization (WHO) estimates that medication-related errors, including drug interactions, contribute to thousands of preventable deaths each year globally. Healthcare providers emphasize the importance of medication reconciliation, patient education, and regular drug interaction screenings to minimize risks.
How Does a Drug Interaction Occur?
A drug interaction occurs when the body processes multiple substances simultaneously, leading to changes in how a drug is absorbed, distributed, metabolized, or excreted. This happens through several mechanisms, such as metabolic interference, competition for receptor sites, or altered enzyme activity in the liver. Some interactions slow down drug clearance, increasing toxicity, while others reduce absorption, making the medication less effective. Food, beverages, and supplements also impact how a drug functions by affecting digestive enzymes or altering pH levels in the stomach.
Can Recreational Drugs Interact with Prescription Medications?
Yes, recreational drugs can interact with prescription medications, leading to dangerous health effects. Many recreational substances, including alcohol, cannabis, and stimulants, affect the central nervous system and amplify or counteract the effects of prescribed drugs. For example, mixing opioids with alcohol causes severe respiratory depression, according to the National Institute of Alcohol Abuse and Alcoholism (NIAAA). Stimulants like cocaine increase heart rate and blood pressure when combined with certain medications, as studied by Schwartz BG et al. 2010, titled “Cardiovascular Effects of Cocaine.” Some recreational drugs interfere with liver enzymes responsible for drug metabolism, leading to unexpected and potentially harmful reactions.
MDMA (ecstasy) combined with antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), significantly increases the risk of serotonin syndrome, a life-threatening condition characterized by confusion, rapid heart rate, and high fever, as studied by Dobry Y, Rice T, Sher L., et al. 2013, titled “Ecstasy use and serotonin syndrome: a neglected danger to adolescents and young adults prescribed selective serotonin reuptake inhibitors.” Another example is marijuana interacting with blood thinners like warfarin, which increases the risk of excessive bleeding due to the way cannabinoids affect drug metabolism in the liver, according to a study by Damkier P, Lassen D, Christensen MMH, Madsen KG, Hellfritzsch M, Pottegård A., et al. 2019, titled “Interaction between warfarin and cannabis.” These interactions highlight the importance of discussing recreational drug use with a healthcare provider to avoid potentially severe complications.
What Are the Types of Drug Interactions?
The types of drug interactions are drug-drug, drug-food, and drug-condition interactions. Drug interactions occur when a medication's effects are altered by another substance, leading to enhanced, reduced, or unintended effects. These interactions happen between two or more drugs, between drugs and food or beverages, or between drugs and pre-existing medical conditions. Some interactions are beneficial, while others are harmful or even fatal.
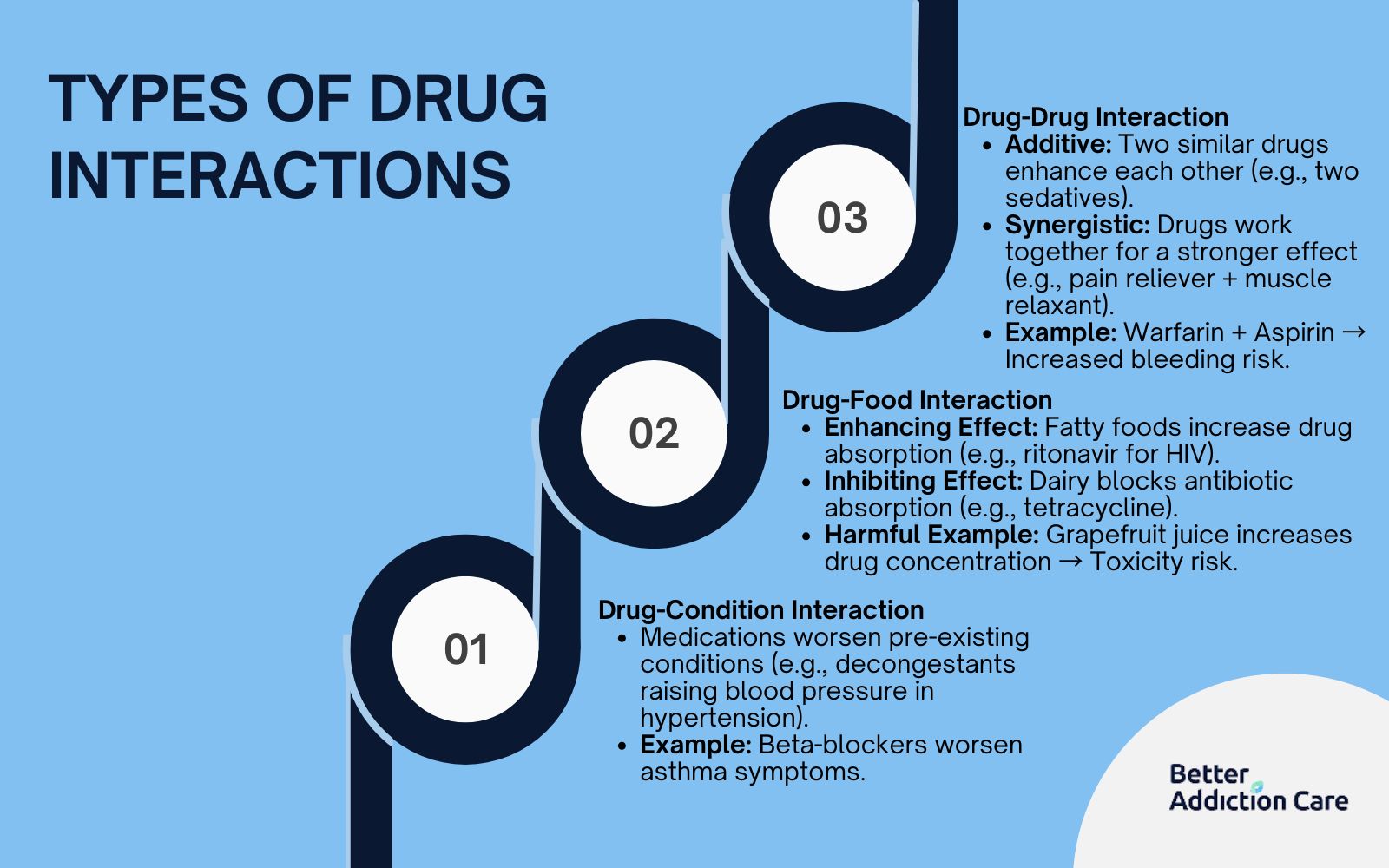
The types of drug interactions are as follows:
1. Drug-Drug Interaction
A drug-drug interaction occurs when two or more medications interact in the body, altering their effectiveness or causing unintended side effects. These interactions are classified as additive, synergistic, or antagonistic. Additive interactions occur when two drugs with similar effects combine, leading to an increased response, such as taking two sedatives that amplify drowsiness. Synergistic interactions happen when drugs work together to produce a stronger effect than either alone, like using pain relievers with muscle relaxants. Antagonistic interactions occur when one drug reduces or blocks the effect of another, such as certain antibiotics decreasing the efficacy of birth control pills.
The mechanism behind drug-drug interactions depends on how medications are metabolized. Many drugs are processed in the liver by enzymes like cytochrome P450. If two drugs compete for the same enzyme, one builds up in the bloodstream, increasing toxicity risks. Some medications also alter absorption by changing stomach acidity or binding with other drugs in the intestines, preventing proper uptake.
Symptoms and side effects of drug-drug interactions vary widely, ranging from mild discomfort like nausea and dizziness to severe complications such as internal bleeding, irregular heartbeats, or respiratory depression. Some interactions are fatal, especially when combining central nervous system depressants like opioids and benzodiazepines, which lead to overdose and death.
In some cases, drug-drug interactions are beneficial. For example, using a beta-blocker with a diuretic helps control high blood pressure more effectively than either drug alone. A beneficial drug-drug interaction is the combination of levodopa and carbidopa for Parkinson’s disease, as studied by According to Muranova A, Shanina E. et al. 2023, titled "Levodopa/Carbidopa/Entacapone Combination Therapy." Levodopa converts into dopamine in the brain but breaks down too soon when taken alone, reducing its effectiveness and causing side effects. Carbidopa prevents this early breakdown, allowing more levodopa to reach the brain while minimizing side effects like nausea. This enhances treatment efficacy, making the combination more effective than levodopa alone.
Harmful interactions occur when medications are taken without proper medical supervision, leading to dangerous side effects. A harmful drug-drug interaction occurs between warfarin and aspirin, as studied by Turan B, Demir H, Mutlu A, Daşlı T, Erkol A, Erden İ. Et al. 2016, titled “Inappropriate combination of warfarin and aspirin.” Warfarin is an anticoagulant that prevents blood clots, while aspirin is an antiplatelet drug that also affects blood clotting. When taken together, they significantly increase the risk of excessive bleeding, including internal bleeding and hemorrhagic stroke. This interaction is dangerous, especially without medical supervision, as it leads to life-threatening bleeding complications.
Treating drug-drug interactions involves stopping or adjusting the dosage of the interfering medication, switching to alternative drugs, or using antidotes in severe cases, such as naloxone for opioid overdoses.
2. Drug-Food Interaction
A drug-food interaction happens when the nutrients in food or beverages interfere with the absorption, metabolism, or excretion of a drug. Some foods enhance drug effectiveness, while others inhibit it, leading to suboptimal treatment outcomes. Common examples include grapefruit juice increasing the concentration of certain medications, dairy products reducing the absorption of antibiotics like tetracycline, and leafy greens counteracting blood thinners like warfarin.
The mechanism behind drug-food interactions depends on how food components affect drug processing. Some foods inhibit liver enzymes, slowing down drug metabolism and increasing toxicity risks. Others alter stomach acidity, delaying or reducing drug absorption. Certain beverages, like alcohol, intensify the sedative effects of medications, making them more potent than intended.
Symptoms and side effects of drug-food interactions range from mild digestive discomfort to severe complications such as internal bleeding, liver toxicity, or dangerously high blood pressure. Some interactions, like consuming tyramine-rich foods while taking monoamine oxidase inhibitors (MAOIs), cause life-threatening hypertensive crises. While most drug-food interactions are not fatal, they significantly reduce treatment effectiveness or cause harmful reactions.
In some cases, drug-food interactions are beneficial. Taking some medications with food helps reduce stomach irritation, as seen with nonsteroidal anti-inflammatory drugs (NSAIDs). According to Ibarra M et al. (2012) in their study titled "Impact of Food Administration on Lopinavir–Ritonavir Bioequivalence Studies," consuming fatty foods with certain medications, such as the antiviral drug ritonavir, enhances its absorption, increases bioavailability, and improves effectiveness in treating HIV by maintaining consistent drug levels in the body.
However, harmful interactions occur when food or drink inhibits medication absorption or enhances side effects. One harmful example of a drug-food interaction is the combination of warfarin and leafy green vegetables. Leafy greens, such as spinach and kale, are high in vitamin K, which counteracts the blood-thinning effects of warfarin, increasing the risk of blood clots and reducing the medication’s effectiveness.
Managing drug-food interactions involves dietary modifications, such as avoiding specific foods, taking medications at the recommended times, or consulting a doctor for alternative treatment options.
3. Drug-Condition Interaction
A drug-condition interaction occurs when a medication negatively affects a pre-existing health condition, leading to worsened symptoms or new complications. These interactions are particularly concerning for individuals with chronic illnesses such as heart disease, diabetes, or kidney disorders. For example, decongestants containing pseudoephedrine raise blood pressure in people with hypertension, corticosteroids spike blood sugar levels in diabetics, and certain painkillers worsen kidney disease.
The mechanism behind drug-condition interactions involves the way medications influence bodily functions already affected by a disease. Some drugs exacerbate symptoms by interfering with natural regulatory processes, such as increasing fluid retention in heart failure patients. Others reduce the effectiveness of medications used to manage chronic conditions, leading to unstable health status.
Symptoms and side effects vary depending on the condition being affected. A person with asthma taking a beta-blocker experiences worsening breathing difficulties, while someone with acid reflux using a nonsteroidal anti-inflammatory drug (NSAID) develops severe gastrointestinal irritation. Some interactions are fatal, such as blood pressure medications triggering dangerously low blood pressure in individuals with underlying cardiovascular conditions.
In some cases, drug-condition interactions are beneficial if medications are carefully tailored to complement existing treatments. For instance, a diabetic patient benefits from an adjusted insulin regimen when prescribed corticosteroids. However, harmful interactions occur when medications are prescribed without considering the patient’s medical history. Managing drug-condition interactions requires personalized treatment plans, regular monitoring, and adjustments in medication choices to minimize risks while ensuring effective therapy.
What are the Symptoms of Drug Interactions?
The symptoms of drug interactions are nausea, vomiting, headache, dizziness, confusion, drowsiness, difficulty breathing and seizures. These symptoms are varied and range from mild discomfort to severe, life-threatening conditions. These reactions occur when one drug affects the way another works, leading to unintended side effects. The severity of symptoms depends on the type of interaction, the medications involved, and individual health factors.
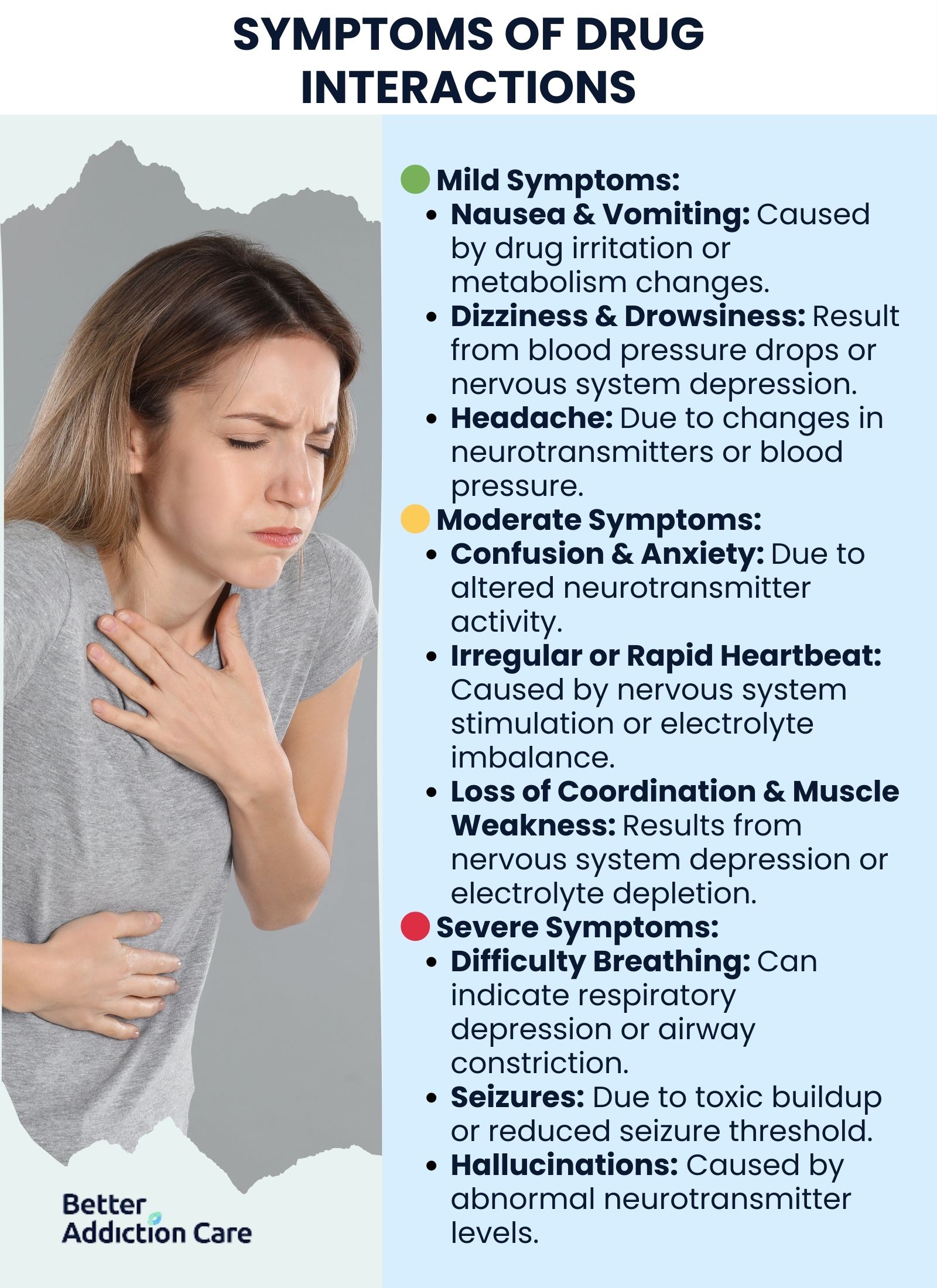
The symptoms of drug interactions are as follows:
-
Nausea: Nausea is a feeling of discomfort in the stomach that precedes vomiting. Drug interactions cause nausea when medications irritate the gastrointestinal tract or alter the body's metabolism of a drug. To manage nausea, patients must take medications with food if allowed, stay hydrated, and consult a doctor for alternative treatments if symptoms persist. According to a study by Drugs.com, the interaction between methadone and rifampin reduces methadone plasma levels, which trigger withdrawal symptoms, including nausea and vomiting, in 21 out of 30 patients undergoing methadone maintenance therapy while receiving rifampin for tuberculosis.
-
Vomiting: Vomiting is the forceful expulsion of stomach contents through the mouth. It occurs due to drug interactions that irritate the stomach lining, overstimulate the brain’s vomiting center, or alter neurotransmitter activity. Managing vomiting involves stopping the offending drug, drinking clear fluids to prevent dehydration, and using anti-nausea medications if necessary.
-
Dizziness: Dizziness refers to a sensation of lightheadedness or unsteadiness. Drug interactions lower blood pressure, affect inner ear balance, or alter brain function, leading to dizziness. Patients must avoid sudden movements, stay hydrated, and consult a doctor if dizziness persists. According to the FDA Drug Safety and Availability document titled “FDA Drug Safety Communication: FDA warns about serious risks and death when combining opioid pain or cough medicines with benzodiazepines; requires its strongest warning,” combining opioids with benzodiazepines cause severe dizziness, profound sedation, respiratory depression, and even death.
-
Headache: A headache is a pain or discomfort in the head or neck region. Drug interactions cause headaches due to changes in blood pressure, increased brain neurotransmitter activity, or dehydration. Managing headaches includes staying hydrated, avoiding medication triggers, and taking pain relievers under medical supervision.
-
Rapid Heartbeat: A rapid heartbeat (tachycardia) occurs when the heart beats faster than normal. Drug interactions stimulate the nervous system, increase adrenaline levels, or affect electrolyte balance, leading to an increased heart rate. To manage this, patients must rest, avoid stimulants like caffeine, and seek medical help if symptoms persist. According to a study by Carlson RW et al. 2009, titled “Intoxication with street drugs: Cocaine and amphetamines,” the interaction between cocaine and amphetamines causes severe tachycardia, significantly increasing heart rate and the risk of life-threatening cardiovascular complications. Both drugs stimulate the central nervous system, leading to excessive catecholamine release, which dangerously elevates heart rate and blood pressure.
-
Irregular Heartbeat: An irregular heartbeat (arrhythmia) refers to abnormal heart rhythms, which are too fast, too slow, or erratic. Drug interactions interfere with heart electrical signals or electrolyte levels. Patients experiencing arrhythmias must avoid triggers, monitor heart rate, and seek immediate medical attention if severe.
-
Confusion: Confusion is a state of disorientation and difficulty in thinking clearly. Drug interactions affect brain neurotransmitters, reduce oxygen supply, or cause toxic buildup in the body. Patients seek medical advice, avoid self-medication, and ensure proper hydration and nutrition. A combination of fluoxetine (an antidepressant) and tramadol leads to serotonin syndrome, causing severe confusion, agitation, and even life-threatening complications. According to a study by Spies PE, Pot JLWH, Willems RPJ, Bos JM, Kramers C. et al. 2017, titled “Interaction between tramadol and selective serotonin reuptake inhibitors: are doctors aware of potential risks in their prescription practice?” only 20 to 30% of prescribers in a general hospital were aware of the potential interaction between fluoxetine (an SSRI) and tramadol, yet tramadol was prescribed at similar rates to SSRI/SNRI users (23.8%) and non-users (24.6%), despite the risk of serotonin syndrome.
-
Drowsiness: Drowsiness is excessive sleepiness or fatigue that affects alertness. Drug interactions enhance sedative effects or depress nervous system activity. Patients must avoid operating machinery, get adequate rest, and consult a doctor about alternative medications if needed.
-
Difficulty Breathing: Difficulty breathing (dyspnea) is a sensation of breathlessness. Specific drug interactions cause airway constriction, fluid buildup in the lungs, or depressed respiratory function. Patients must seek emergency medical attention, avoid allergens, and use prescribed respiratory treatments.
-
High or Low Blood Pressure: Changes in blood pressure occur when drug interactions affect vascular tone or fluid balance. High blood pressure (hypertension) increases heart strain, while low blood pressure (hypotension) causes dizziness and fainting. Managing these symptoms requires monitoring blood pressure, adjusting medication doses, and following a doctor’s recommendations.
-
Seizures: Seizures are sudden, uncontrolled electrical disturbances in the brain. Drug interactions lower the seizure threshold, interfere with anticonvulsant medications, or cause toxic buildup. Patients with a history of seizures must follow medication instructions closely and seek emergency care if a seizure occurs.
-
Muscle Weakness: Muscle weakness refers to reduced strength and difficulty in movement. Drug interactions disrupt nerve signals, deplete essential electrolytes, or cause muscle toxicity, as studied by Jones JD, Mogali S, and Comer SD. et al. 2012, titled “Polydrug abuse: a review of opioid and benzodiazepine combination use.” Managing this symptom includes resting, staying hydrated, and discussing alternative medications with a healthcare provider.
-
Loss of Coordination: Loss of coordination (ataxia) affects balance and movement. Drug interactions that depress the central nervous system or impair nerve function cause this symptom. Patients must avoid alcohol, be cautious when walking, and consult a doctor if coordination problems persist. Research by Drugs.com titled “Drug Interactions between gabapentin and methadone” found the interaction between methadone and gabapentin causes serious ataxia, leading to an increased risk of falls and impaired motor function. This occurs due to their combined depressant effects on the central nervous system, significantly impairing balance and movement.
-
Anxiety or Agitation: Anxiety or agitation involves feelings of nervousness, restlessness, or excessive worry. Drug interactions affect neurotransmitter levels or overstimulate the nervous system. Managing this symptom includes practicing relaxation techniques, avoiding caffeine, and consulting a doctor about medication adjustments.
-
Hallucinations: Hallucinations are sensory perceptions of things that are not present, such as seeing or hearing things that do not exist. Drug interactions cause hallucinations by affecting dopamine or serotonin levels in the brain. Patients experiencing hallucinations must seek medical help immediately to adjust their medication regimen.
What Drugs Should Not Be Taken Together?
Opioids like oxycodone and benzodiazepines such as Xanax should not be taken together because their combined effects dangerously suppress breathing, leading to overdose and death. Certain drug interactions cause severe health risks, including excessive sedation, irregular heart rhythms, dangerously high or low blood pressure, or fatal respiratory depression. For example, cocaine and heroin (speedballing) significantly increase the risk of sudden cardiac arrest, while alcohol and benzodiazepines lead to blackouts and life-threatening respiratory failure.

The following drugs should not be taken together:
Alcohol + Benzodiazepines (e.g., Xanax, Valium)
Alcohol and benzodiazepines are not recommended to be taken together because both depress the central nervous system (CNS), leading to extreme drowsiness, respiratory depression, and an increased risk of overdose. Benzodiazepines like Xanax (alprazolam) and Valium (diazepam) are prescribed for anxiety and insomnia, but when combined with alcohol, they cause dangerous sedation, confusion, memory loss, and even death due to suppressed breathing. Since both substances suppress respiratory activity and increase sedation, the combined impact has severe respiratory effects, as studied by NIAAA in research titled “Alcohol-Medication Interactions: Potentially Dangerous Mixes.”
Prescription Opioids + Opioids (e.g., Oxycodone, Heroin)
Combining prescription opioids like oxycodone, hydrocodone, or morphine with illicit opioids like heroin or fentanyl results in life-threatening respiratory depression, leading to coma or death. Since all opioids work by binding to the brain’s opioid receptors and suppressing pain signals, taking multiple opioids together significantly increases overdose risk, especially with highly potent opioids like fentanyl, which is 50 to 100 times stronger than morphine.
Benzodiazepines + Sleep Medications (e.g., Ambien)
Benzodiazepines such as lorazepam (Ativan) or clonazepam (Klonopin) should not be mixed with sleep aids like zolpidem (Ambien) because both enhance the effects of gamma-aminobutyric acid (GABA) in the brain, leading to excessive sedation, impaired coordination, and an increased risk of falls, blackouts, and overdose. According to GoodRx, titled “7 Clonazepam Interactions You Should Know About,” this combination also dangerously slows breathing, potentially leading to death.
MDMA + LSD ("Candy Flipping")
MDMA (Ecstasy) and LSD are not recommended to be taken together because the combination, called "candy flipping," causes severe serotonin syndrome, leading to dangerously high body temperature, confusion, muscle rigidity, and seizures. MDMA increases serotonin release, while LSD also affects serotonin receptors, creating an overstimulated nervous system that results in hallucinations, panic attacks, and cardiovascular issues.
Cocaine + Heroin (Speedball)
It is not recommended to take cocaine and heroin together because they have opposite effects on the body, which mask overdose symptoms. Cocaine is a stimulant that increases heart rate and blood pressure, while heroin is a depressant that slows breathing. This dangerous combination leads to sudden cardiac arrest, respiratory failure, and overdose, making speedballs one of the deadliest drug interactions, as studied by van Amsterdam J et al. 2024, titled “Explaining the high mortality among opioid-cocaine co-users compared to opioid-only users. A systematic review.”
Adderall + Cocaine
Adderall (amphetamine) and cocaine should not be taken together because both are powerful stimulants that overload the cardiovascular system, leading to dangerously high blood pressure, irregular heart rhythms, and increased risk of heart attack or stroke. Additionally, this combination causes severe anxiety, paranoia, and psychosis due to excessive dopamine stimulation.
Marijuana + Alcohol
Marijuana and alcohol should not be taken together because they both affect coordination, judgment, and cognitive function, increasing the risk of accidents and blackouts. Alcohol enhances the absorption of THC, the psychoactive compound in marijuana, leading to extreme dizziness, nausea, vomiting (a phenomenon known as "greening out"), and even panic attacks.
Opioids + Benzodiazepines
Opioids like morphine, oxycodone, or fentanyl and benzodiazepines like Xanax or Valium should never be combined because they both depress the central nervous system, leading to profound sedation, respiratory depression, and a high risk of fatal overdose. The FDA has issued its strongest warning against this combination due to the severe danger of accidental death.
MDMA (Ecstasy) + MAOIs
MDMA and monoamine oxidase inhibitors (MAOIs), which are used to treat depression (e.g., phenelzine, tranylcypromine), must not be mixed because this combination dramatically increases serotonin levels, leading to serotonin syndrome. Symptoms include high fever, rapid heart rate, muscle breakdown, and seizures, which are fatal without immediate medical intervention.
Suboxone + Benzodiazepines
Suboxone (buprenorphine/naloxone), used for opioid addiction treatment, should not be combined with benzodiazepines like clonazepam or alprazolam because both drugs cause severe respiratory depression and sedation. This combination is particularly dangerous for individuals with a history of opioid use disorder, as it increases overdose risk despite Suboxone’s partial opioid agonist properties.
Methamphetamine + Opioids
Methamphetamine and opioids should not be taken together because their opposing effects on the body create unpredictable and dangerous reactions. Methamphetamine is a stimulant that increases heart rate and blood pressure, while opioids slow down breathing and heart function. This leads to sudden cardiac arrest, respiratory failure, and an increased risk of overdose, as the stimulant masks opioid-induced respiratory depression, as studied by Meyer D, Athota P, Gowen A, Nguyen NM, Schaal VL, Yelamanchili SV, Pendyala G. et al. 2022, titled “Effect of Combined Methamphetamine and Oxycodone Use on the Synaptic Proteome in an In Vitro Model of Polysubstance Use.”
Does Grapefruit Juice Interact with Drugs?
Yes, grapefruit juice interacts with drugs because it inhibits the cytochrome P450 3A4 (CYP3A4) enzyme in the small intestine. This leads to increased drug absorption and higher blood concentrations, which enhance side effects or toxicity.
A study published in Clinical Pharmacokinetics by Bailey DG et al., 2013, titled “Grapefruit–medication interactions: Forbidden fruit or avoidable consequences?” found that grapefruit juice significantly increases the bioavailability of certain medications, including statins (e.g., atorvastatin), calcium channel blockers (e.g., felodipine), and immunosuppressants (e.g., cyclosporine). The furanocoumarins in grapefruit juice block CYP3A4, preventing drug breakdown and leading to dangerously high drug levels. This interaction causes severe complications such as excessive sedation, muscle toxicity, irregular heart rhythms, and increased bleeding risk when combined with anticoagulants. Due to these risks, patients taking CYP3A4-metabolized drugs avoid grapefruit juice or consult their healthcare provider.
How Does Alcohol Addiction Affect Drug Interactions?
Alcohol addiction affects drug interactions by significantly increasing the risk of harmful drug interactions. A study by the National Institutes of Health found that nearly 42% of U.S. adults who consume alcohol also use medications known to interact adversely with alcohol. This risk is even higher among older adults with alcohol addiction; approximately 78% of those over 65 who drink alcohol report using such medications. These interactions lead to severe health issues, including liver damage, heart problems, and impaired breathing.
How Does Alcohol Interact with Drugs?
Alcohol interacts with drugs by altering their metabolism, increasing side effects, and potentially leading to dangerous health risks. According to a study published in Alcohol Research: Current Reviews by Weathermon R, Crabb DW, et al. 1999, titled “Alcohol and medication interactions,” alcohol affects drug metabolism by inhibiting or inducing liver enzymes, particularly cytochrome P450 2E1 (CYP2E1). This either intensifies drug effects, leading to excessive sedation, dizziness, or respiratory depression or reduces drug efficacy. For example, alcohol enhances the sedative effects of benzodiazepines and opioids, increasing overdose risk. It also interferes with medications like warfarin, leading to blood clotting or excessive bleeding. Chronic alcohol consumption further complicates drug interactions by inducing liver enzymes and altering the way medications are processed over time.
The common drug interactions with alcohol are as follows:
-
Benzodiazepines (e.g., Xanax, Valium): Combining alcohol with benzodiazepines significantly increases sedation and the risk of respiratory depression. Both substances act as central nervous system (CNS) depressants, slowing brain activity and leading to extreme drowsiness, dizziness, confusion, and impaired coordination. In severe cases, this combination causes life-threatening breathing difficulties, coma, or even death. Due to these dangers, doctors strongly advise against using alcohol while taking benzodiazepines. According to a study by Jones CM, Paulozzi LJ, Mack KA; CDC. et al. 2016, titled “Alcohol involvement in opioid pain reliever and benzodiazepine drug abuse-related emergency department visits and drug-related deaths—United States, 2010,” alcohol was involved in 27.2% of benzodiazepine-related visits and 21.4% of benzodiazepine-related deaths in US emergency departments.
-
Opioids (e.g., oxycodone, heroin): Alcohol and opioids are both potent CNS depressants, and their combined use intensifies sedative effects, slowing down breathing and heart rate. This leads to fatal respiratory depression, particularly in individuals taking high doses of opioids or those with reduced tolerance, according to a study by Witkiewitz K, Vowles KE. et al. 2018, titled “Alcohol and Opioid Use, Co-Use, and Chronic Pain in the Context of the Opioid Epidemic: A Critical Review.” The U.S. Centers for Disease Control and Prevention (CDC) warns that alcohol consumption alongside prescription opioids increases the risk of overdose and death, making this interaction especially dangerous.
-
Antidepressants (e.g., SSRIs, MAOIs): Alcohol worsens the side effects of antidepressants, leading to excessive drowsiness, dizziness, and impaired coordination. In the case of monoamine oxidase inhibitors (MAOIs), alcohol triggers dangerously high blood pressure (hypertensive crisis) due to its interaction with certain compounds, such as tyramine, found in some alcoholic beverages. Alcohol counteracts the benefits of antidepressants, worsening symptoms of depression and anxiety, according to the Mayo Clinic.
-
Blood Thinners (e.g., warfarin): Alcohol interferes with the metabolism of blood thinners like warfarin, altering their effectiveness and increasing the risk of excessive bleeding or clot formation. Chronic alcohol use enhances warfarin’s anticoagulant effects, leading to internal bleeding, while binge drinking reduces its effectiveness, increasing the risk of blood clots and strokes. Patients on warfarin are advised to limit alcohol consumption and undergo regular monitoring to prevent complications.
-
Diabetes Medications (e.g., insulin, metformin): Alcohol consumption dangerously lowers blood sugar levels in individuals taking diabetes medications like insulin and sulfonylureas, increasing the risk of hypoglycemia (low blood sugar). According to research by the American Diabetes Association, this causes dizziness, confusion, fainting, and even seizures. Additionally, mixing alcohol with metformin increases the risk of lactic acidosis, a potentially life-threatening condition caused by a buildup of lactic acid in the bloodstream.
-
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs, e.g., ibuprofen, aspirin): NSAIDs, when taken with alcohol, raise the risk of gastrointestinal bleeding and stomach ulcers. Alcohol irritates the stomach lining, and NSAIDs further reduce the stomach’s protective mucus, making it more vulnerable to damage. Long-term use of both substances together increases the likelihood of internal bleeding, stomach pain, and even perforation of the stomach or intestines.
-
Antibiotics (e.g., metronidazole, cefotetan): Certain antibiotics, such as metronidazole and cefotetan, interact negatively with alcohol, leading to severe nausea, vomiting, flushing, rapid heartbeat, and low blood pressure. According to Healthline, this reaction, known as the disulfiram-like effect, occurs because alcohol inhibits the breakdown of acetaldehyde, a toxic byproduct of alcohol metabolism. Patients prescribed these antibiotics are strongly advised to avoid alcohol during and for several days after completing treatment.
What Supplements Interact with Drugs?
Supplements that interact with drugs include Ginseng, Ginkgo biloba, Garlic supplements, and Vitamin K. These supplements interact with drugs by altering their absorption, metabolism, or effectiveness, which lead to reduced efficacy or increased risk of side effects. Many herbal and dietary supplements contain active compounds that interfere with prescription medications, sometimes causing dangerous interactions. Some supplements enhance drug effects, increasing toxicity, while others block drug activity, making treatments less effective.
The following supplements interact with drugs:
-
St. John’s Wort: St. John’s Wort is known for its antidepressant properties. However, it significantly reduces the effectiveness of various medications by increasing the activity of liver enzymes that break down drugs. It lowers the levels of antidepressants, birth control pills, blood thinners, and immunosuppressants, making them less effective.
-
Ginseng: Ginseng interferes with blood sugar control in diabetic patients and reduces the effectiveness of anticoagulants like warfarin. It also causes insomnia and rapid heartbeat when taken with stimulants or certain antidepressants, as studied by Chen W, Balan P, and Popovich DG. et al. 2019, titled “Review of Ginseng Anti-Diabetic Studies.”
-
Ginkgo Biloba: Ginkgo biloba is used to enhance memory and circulation, but it increases the risk of bleeding when combined with blood thinners like warfarin, aspirin, or NSAIDs. This interaction leads to excessive bruising or internal bleeding.
-
Garlic Supplements: Garlic supplements have natural blood-thinning properties, which enhance the effects of anticoagulants and antiplatelet drugs, increasing the risk of bleeding. A study by Lawn A, Sains P. et al. 2012, titled “Comment on: Not just a vampire repellent: the adverse effects of garlic supplements in surgery,” also lowers blood pressure excessively when taken with hypertension medications.
-
Vitamin K: Vitamin K plays an important role in blood clotting and counteracts the effects of blood thinners like warfarin. Patients on anticoagulants must maintain a consistent intake of Vitamin K to avoid fluctuations in drug effectiveness.
-
Calcium and Magnesium: Calcium and magnesium supplements interfere with the absorption of certain antibiotics, reducing their effectiveness. These minerals also interact with osteoporosis medications and thyroid medications, preventing proper absorption.
-
Iron Supplements: Iron supplements decrease the effectiveness of certain antibiotics and thyroid medications by binding to them in the stomach, reducing their absorption. According to GoodRx, taking iron separately from these medications helps avoid this interaction.
-
Echinacea: Echinacea is used to boost immunity but interferes with immunosuppressant medications, potentially reducing their ability to prevent organ rejection in transplant patients.
-
Fish Oil (Omega-3 Fatty Acids): Fish oil supplements have natural anticoagulant properties, but when combined with blood thinners or non-steroidal anti-inflammatory drugs (NSAIDs), they increase the risk of bleeding.
Who Is at Risk for Drug Interactions?
People who take multiple medications, have chronic health conditions or belong to specific age groups are at higher risk for drug interactions. Drug interactions lead to reduced effectiveness, increased side effects, or serious health complications. Understanding who is at risk helps prevent harmful interactions through careful monitoring and medical supervision.
The following individuals are at risk for drug interactions:
-
Older Adults: As people age, their metabolism slows down, making it harder for the body to break down and eliminate drugs. Older adults are also more likely to take multiple medications, increasing the risk of interactions. According to Johns Hopkins Medicine, people over 60 who take daily medications for multiple chronic conditions are at risk for overmedication and other complications of polypharmacy. Complications include sedation, increased risk for falls, and side effects.
-
Individuals Taking Multiple Medications (Polypharmacy): People who take several prescription or over-the-counter medications, including supplements, have a higher chance of drug interactions. Some drugs interfere with the effectiveness of others, leading to unintended side effects or reduced therapeutic benefits.
-
Individuals with Chronic Health Conditions: People with conditions such as diabetes, heart disease, liver disease, or kidney disease are more prone to drug interactions because their organs do not process medications efficiently. This leads to drug buildup in the body, increasing toxicity risks.
-
Individuals with Liver or Kidney Impairment: The liver and kidneys play a key role in metabolizing and eliminating drugs. According to a study by Susa ST, Hussain A, Preuss CV. et al. 2023, titled “Drug Metabolism,” these organs are not functioning correctly, and medications accumulate in the body, leading to a higher risk of toxicity and adverse effects.
-
People Who Consume Alcohol or Use Recreational Drugs: Alcohol and recreational drugs interact with prescription medications, altering their effects and increasing the risk of side effects such as drowsiness, dizziness, or respiratory depression, as studied by NIAAA titled “Alcohol-Medication Interactions: Potentially Dangerous Mixes.”
-
Individuals Taking Herbal Supplements: Many herbal supplements contain active compounds that interfere with prescription drugs. For example, St. John’s Wort reduces the effectiveness of antidepressants and birth control, while ginkgo biloba increases the risk of bleeding when taken with blood thinners.
-
Pregnant or Breastfeeding Women: Certain drug interactions affect fetal development or pass into breast milk, potentially harming the baby. According to the Mayo Clinic, pregnant and breastfeeding women must consult a healthcare provider before taking any medications or supplements.
-
Individuals with Genetic Variations in Drug Metabolism: Some people have genetic differences that affect how their bodies metabolize medications. These variations lead to either excessive drug accumulation or rapid elimination, affecting drug efficacy and safety.
How to Avoid Drug Interaction?
To avoid drug interactions, it is important to be aware of potential conflicts between medications, supplements, and foods while taking preventive measures to minimize risks. Careful monitoring, consulting healthcare professionals, and using reliable tools help prevent dangerous interactions and ensure medications work as intended.
To avoid drug interactions, the following ways are employed:
-
Use a Drug Interaction Checker: Online drug interaction checkers or pharmacy databases help identify potential conflicts between medications, supplements, and foods. These tools provide instant alerts about possible side effects or reduced drug effectiveness, allowing you to take precautions before combining substances.
-
Wait Between Medications That Interact: Some medications require a time gap between doses to prevent interactions. For example, certain antibiotics are not recommended to be taken with dairy products, and some medications need to be spaced apart to avoid reducing absorption or effectiveness. Always follow prescribed dosing schedules.
-
Talk to Your Doctor: Consulting your doctor or pharmacist before starting new medications, supplements, or over-the-counter drugs helps prevent interactions. Healthcare professionals review your medication list and adjust dosages or recommend safer alternatives if needed.
-
Read Medication Labels and Instructions Carefully: Drug labels and package inserts provide important warnings about potential interactions with other medications, foods, or alcohol. Reading and following these instructions helps you avoid combinations that lead to harmful effects.
-
Keep a List of All Medications and Supplements: Maintaining an updated list of all prescription medications, over-the-counter drugs, vitamins, and supplements you take helps healthcare providers identify potential interactions. This is especially important for individuals seeing multiple doctors or specialists.
-
Avoid Alcohol and Recreational Drugs: Alcohol and recreational drugs significantly alter how medications work in the body, increasing the risk of side effects such as drowsiness, dizziness, or life-threatening reactions. Always check if alcohol consumption is safe with your prescribed medications.
-
Be Cautious with Herbal Supplements: Many herbal supplements contain active compounds that interfere with prescription medications. For example, St. John’s Wort reduces the effectiveness of antidepressants, and ginseng affects blood sugar levels. Always inform your doctor about any supplements you take.
-
Monitor for Unusual Symptoms: If you experience side effects such as dizziness, nausea, irregular heartbeat, or confusion after starting a new medication, report them to your healthcare provider immediately. Early detection of interactions prevents serious complications.
-
Stick to One Pharmacy: Filling all prescriptions at the same pharmacy allows pharmacists to track your medications and identify potential interactions. Many pharmacies offer medication review services to ensure safe combinations.
How Do I Know If My Medications Interact with Each Other?
To know if your medications interact with each other it's important to use a drug interaction checker, consult with healthcare professionals, and monitor for unusual symptoms. According to a study by Budnitz DS, Lovegrove MC, Shehab N, Richards CL. et al. 2011, titled “Emergency hospitalizations for adverse drug events in older Americans,” from 2007 to 2009, an estimated 99,628 emergency hospitalizations per year in U.S. adults aged 65+ were due to adverse drug events, with nearly half (48.1%) occurring in those 80+, and 65.7% caused by unintentional overdoses, primarily involving warfarin (33.3%), insulins (13.9%), antiplatelet agents (13.3%), and hypoglycemic agents (10.7%).
Drug databases such as those provided by the FDA and the National Library of Medicine help identify harmful interactions. Symptoms like dizziness, nausea, confusion, or irregular heartbeat indicate an interaction requiring immediate medical attention. Regular medication reviews with a doctor or pharmacist also help prevent adverse effects.
Why Do Some Drugs Interact Differently for Different People?
Drugs interact differently for different people due to differences in genetics, metabolism, age, organ function, and other personal factors. Research by the American Academy of Family Physicians suggests that genetic variations in liver enzymes, such as CYP450, significantly affect how drugs are metabolized, leading to different responses in different people. For example, some individuals metabolize drugs more slowly, causing higher blood levels and increased side effects, while others process them rapidly, reducing drug effectiveness. Age-related changes, pre-existing health conditions, and concurrent medications influence how the body reacts to drug combinations. Personalized medicine approaches, including genetic testing, help predict drug interactions and optimize treatment plans.
How Do Drug Interactions Impact The Effectiveness Of Treatment Programs In Drug Rehab Facilities?
Drug interactions impact the effectiveness of treatment programs in drug rehab facilities by fundamentally altering how medications work in the body and compromising therapeutic outcomes. When individuals take multiple substances, whether prescription medications, over-the-counter drugs, or recreational substances, these interactions reduce treatment efficacy, intensify side effects, or create dangerous health complications that derail recovery progress. Drug interactions impact treatment success by interfering with medication absorption, metabolism, and therapeutic action, making it essential for rehab facilities to carefully monitor and manage all substances in a patient's system. Effective management of drug interactions is crucial for successful treatment and recovery. Our local drug and alcohol rehab locator connects you with tailored treatment centers, from rehabs in California to rehabs in Texas, offering confidential assessments and support to help navigate potential drug interactions and ensure safe, effective care.
Related Articles
Treatment Centers in Texas








