Drug Withdrawal: Definition, Signs and Symptoms, Causes, and Treatment
Drug withdrawal occurs when a person who has developed a dependence on a substance abruptly reduces or stops use. It is a natural physiological reaction to the absence of a drug the body has adapted to, creating uncomfortable or even dangerous symptoms.
Drug withdrawal occurs when a person who has developed a dependence on a substance abruptly reduces or stops use. It is a natural physiological reaction to the absence of a drug the body has adapted to, creating uncomfortable or even dangerous symptoms.
According to the 2023 NSDUH, approximately 2.3 million Americans aged 12 and older (0.8% of the population) received addiction treatment involving medications for opioid use disorder (MOUD) within the past year.
Signs and symptoms of drug withdrawal vary widely depending on the substance but commonly include anxiety, nausea, sweating, muscle pain, and tremors. Both physical and psychological symptoms range from mild discomfort to severe, life-threatening reactions without proper management.
The causes of drug withdrawal stem from neurochemical changes in the brain due to repeated substance use. Over time, the brain adapts to the presence of the drug, and when it is removed, neurotransmitter imbalances trigger withdrawal symptoms as the body struggles to regain equilibrium.
Treatment for drug withdrawal involves medically supervised drug detox programs, symptom management through medications, and emotional support. Professional care is important to ensure safety, ease symptoms, and prepare individuals for further recovery, such as therapy, inpatient rehab, or outpatient support services.
What Is Drug Withdrawal?
Drug withdrawal is the physical and psychological response that occurs when a person abruptly reduces or stops using a substance they have developed dependence on. Withdrawal happens because the body adapts to the presence of a drug over time, disrupting natural brain chemistry. When the substance is removed, the body struggles to regain balance, leading to what is known as withdrawal syndrome.
Common substances that cause withdrawal include alcohol, opioids, benzodiazepines, stimulants like cocaine and methamphetamine, and nicotine. Withdrawal symptoms range from mild discomfort to severe, life-threatening conditions, especially in individuals with a substance use disorder.
What Are the Signs and Symptoms of Drug Withdrawal?
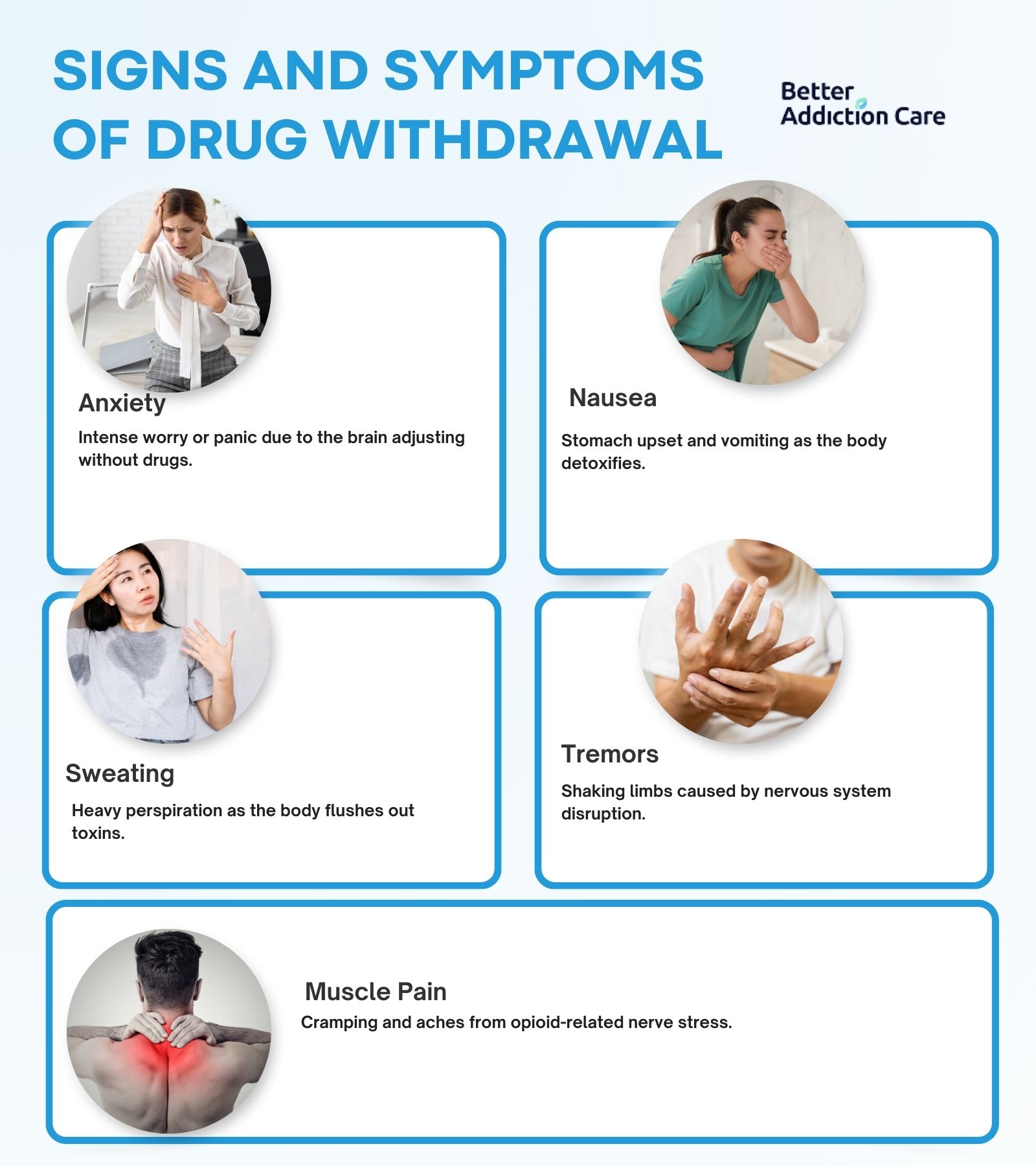
The signs and symptoms of drug withdrawal are anxiety, nausea, sweating, tremors, and other physical and psychological changes. These symptoms vary depending on the type of substance used, the length of use, and the severity of dependence. Withdrawal involves acute symptoms that appear within hours and protracted symptoms that linger for weeks.
The signs and symptoms of drug withdrawal are as follows:
1. Anxiety
Anxiety is a feeling of intense nervousness, worry, or fear that commonly arises during drug withdrawal. It is a psychological symptom caused by the brain's difficulty adjusting to the absence of substances that previously regulated mood. Anxiety appears as restlessness, panic attacks, and obsessive worrying, especially during acute withdrawal from alcohol, opioids, and benzodiazepines. This is highlighted in the study by Caetano R, Clark CL, and Greenfield TK. et al. 1998, titled "Prevalence, trends, and incidence of alcohol withdrawal symptoms: analysis of general population and clinical samples," 86% of Americans experience symptoms of depression and anxiety during alcohol withdrawal.
2. Nausea
Nausea is a queasy or unsettled sensation in the stomach, leading to vomiting during withdrawal. It is a physical symptom that occurs because drug use disrupts the gastrointestinal system, and the body struggles to stabilize during detox. Nausea is especially common in opioid and alcohol withdrawal and persists during protracted withdrawal if left untreated. As reported in the study by Caetano R, Clark CL, and Greenfield TK. et al. 1998, titled "Prevalence, trends, and incidence of alcohol withdrawal symptoms: analysis of general population and clinical samples," 61% of white Americans experience nausea and vomiting symptoms during alcohol withdrawal.
3. Sweating
Sweating is the excessive release of perspiration as the body tries to eliminate toxins and stabilize temperature during withdrawal. It is a physical symptom most associated with opioid, alcohol, and stimulant withdrawal. Heavy sweating accompanies other signs such as chills, shaking, and increased heart rate during acute withdrawal phases. As reported in the study by Caetano R, Clark CL, and Greenfield TK, 75% of white Americans experience excessive sweating and chills when going through alcohol withdrawal.
4. Tremors
Tremors are involuntary shaking or trembling movements, seen in the hands, arms, or legs during drug withdrawal. Tremors occur due to disruptions in the nervous system after prolonged substance use. Alcohol withdrawal is particularly known for causing hand tremors, but tremors also occur with opioid, benzodiazepine, and stimulant withdrawal, indicating severe physical dependence.
5. Muscle Pain and Cramping
Muscle pain and cramping are common symptoms during opioid withdrawal, persisting for extended periods. Research indicates that severe musculoskeletal pain rises from 24.5% to 53.4% among methadone users, consistent with findings from Kamali-Sarvestani F, Motiallah T, Ghaffarinejad F. et al. 2014, titled "The Prevalence of Musculoskeletal Pain and Forward Head Posture among Heroin Users during their Withdrawal with Methadone."
What Does Drug Withdrawal Feel Like?
Drug withdrawal feels like a combination of intense physical discomfort and emotional turmoil. Individuals experience muscle aches, nausea, chills, and relentless cravings, comparable to battling a severe flu while enduring extreme anxiety or depression. Emotional sensations like agitation, hopelessness, and mood swings amplify the distress, making withdrawal a deeply taxing experience marked by both physical and psychological discomfort.
What Causes Drug Withdrawal?
The causes of drug withdrawal are rooted in the brain's adaptation to prolonged substance use. Repeated drug exposure alters neurotransmitter activity, forcing the brain to adjust its normal functions. When the substance is suddenly removed, the brain struggles to regain balance, leading to withdrawal symptoms. This mechanism, driven by tolerance and dependence, underlies the intense physical and emotional reactions individuals experience during withdrawal.
What Are the Stages and Timeline for Drug Withdrawal?
The stages and timeline for drug withdrawal include onset, peak symptoms, and eventual resolution. Withdrawal begins within hours after stopping drug use, peaks in severity around days 2 to 3, and gradually improves over the following days. For opioids, withdrawal lasts about 5 to 10 days; alcohol withdrawal spans 7 to 10 days; and stimulants usually cause withdrawal symptoms for 5 to 7 days. Some individuals also experience post-acute withdrawal syndrome (PAWS), where symptoms linger for weeks or months.
How Long Do Drug Withdrawal Symptoms Last?
The duration of withdrawal symptoms ranges from a few days to several months, depending on the substance. Opioid withdrawal symptoms usually persist for 5 to 10 days, alcohol withdrawal lasts around 7 to 10 days, benzodiazepine withdrawal extends for several weeks to months, and stimulant withdrawal lasts 5 to 7 days. While acute symptoms resolve relatively quickly, some individuals face longer-term emotional and cognitive challenges during recovery.
What Is the Treatment for Drug Withdrawal?
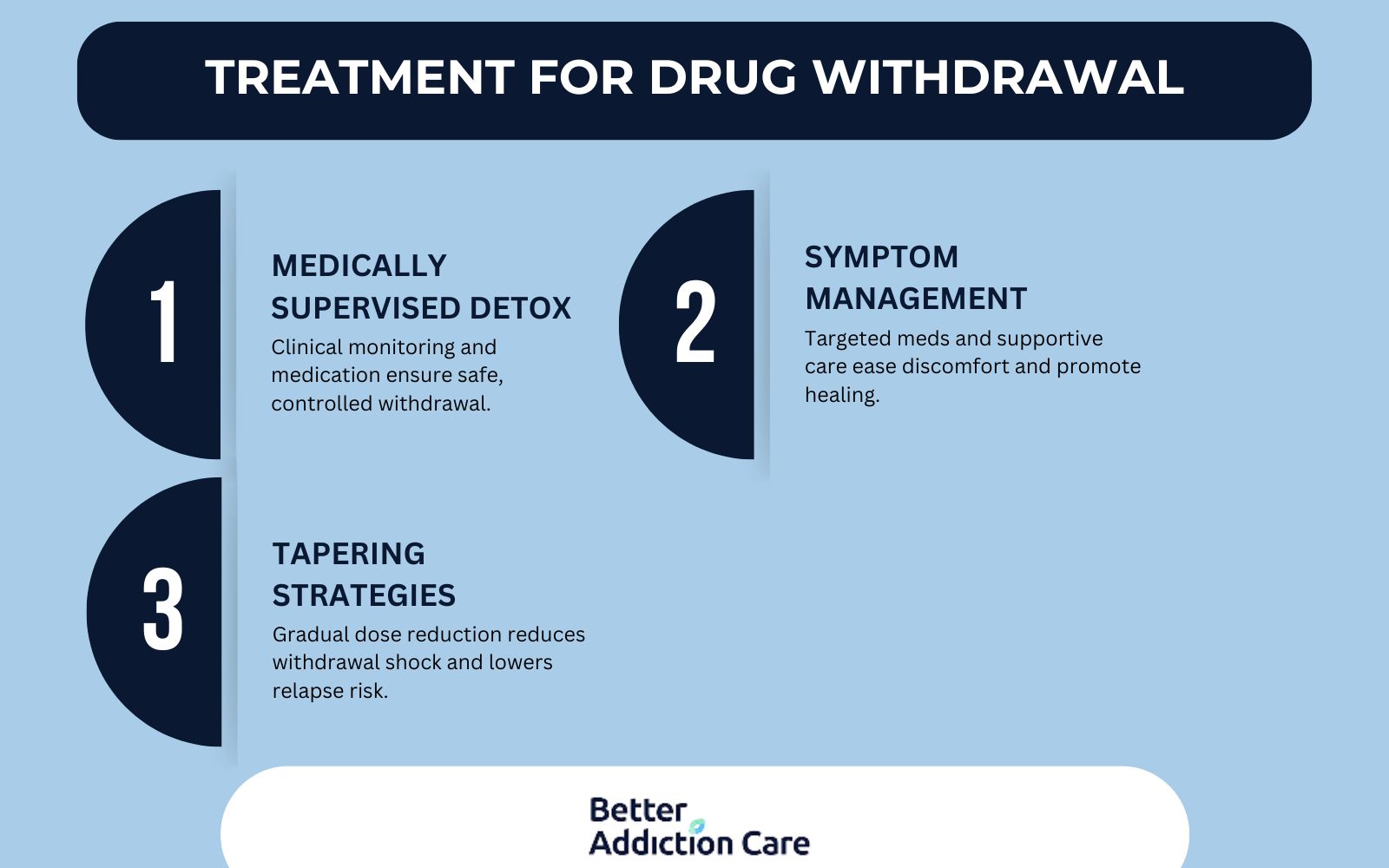
The treatment for drug withdrawal includes medically supervised detoxification, symptom management strategies, and gradual tapering approaches to ensure safe recovery. Professional treatment is important to minimize complications, ease discomfort, and support long-term sobriety through clinical care and therapeutic interventions.
The treatment for drug withdrawal includes:
-
Medically Supervised Detox: Medically supervised detox involves monitoring individuals in a clinical setting to manage withdrawal symptoms safely. Medical teams administer medications to stabilize vital signs, prevent complications like seizures, and ease severe symptoms. This structured environment provides immediate intervention if emergencies arise, making it the safest first step in recovery, according to Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Settings.
-
Symptom Management: Symptom management focuses on alleviating the physical and psychological discomforts of withdrawal. Doctors prescribe medications like benzodiazepines for alcohol withdrawal or clonidine for opioid withdrawal to control anxiety, agitation, nausea, and muscle aches. Supportive care, such as hydration, nutrition, and rest, is also important in helping the body heal during this phase.
-
Tapering Strategies: Tapering is the gradual reduction of drug dosage to minimize withdrawal shock to the body. This method is especially important for substances like benzodiazepines or opioids, where abrupt cessation is dangerous. A professionally managed tapering schedule lowers dependency slowly, reducing both the intensity of withdrawal symptoms and the risk of relapse.
How to Find Treatment for Drug Withdrawal?
To find treatment for drug withdrawal, individuals should start by exploring reputable resources that connect them with trusted care providers. A helpful tool is our treatment locator, which allows users to find rehabs in Florida and rehabs in New York, as well as many other locations, based on specific needs. Inpatient treatment offers 24/7 medical supervision for severe withdrawal cases, while outpatient programs provide flexible support for milder symptoms. Accessing the right level of care through a professional network ensures a safer detox process and better long-term recovery outcomes.
What Medications Are Used to Treat Drug Withdrawal?

The medications used to treat drug withdrawal are Methadone, Benzodiazepines, and Clonidine. These medications help ease withdrawal symptoms, reduce cravings, and provide stabilization during detox. They are important in medically supervised detox programs to improve comfort and increase the likelihood of successful recovery.
The medications used to treat drug withdrawal are as follows:
-
Methadone (Opioids): Methadone is a long-acting opioid agonist used to manage withdrawal symptoms in individuals detoxing from heroin or prescription opioids. It reduces cravings and minimizes withdrawal severity by acting on the same brain receptors without producing the same high. According to the National Institute on Drug Abuse (NIDA), methadone is an opioid medication that has been used for more than 50 years to treat opioid use disorder.
-
Benzodiazepines (Alcohol): Benzodiazepines are the primary medications for managing alcohol withdrawal. They help prevent severe complications like seizures and delirium tremens by calming the central nervous system and reducing hyperactivity during withdrawal, as studied by Sachdeva A, Choudhary M, Chandra M. et al. 2015, titled "Alcohol Withdrawal Syndrome: Benzodiazepines and Beyond."
-
Clonidine (general withdrawal): Clonidine is used to treat a variety of withdrawal symptoms across multiple substances, including opioids and alcohol. It helps alleviate anxiety, sweating, muscle aches, and agitation by regulating the body's stress response.
What Is the Difference Between Drug Withdrawal and Detox?
The difference between drug withdrawal and detox lies in their focus and purpose. Drug withdrawal refers to the physical and psychological symptoms that occur when a person suddenly reduces or stops using a substance after developing dependence. These symptoms range from mild discomfort to severe medical emergencies. In contrast, drug detox is the medically supervised process of managing withdrawal symptoms safely and effectively. Detox focuses on stabilizing the individual, relieving symptoms, and preparing them for long-term addiction treatment as part of the recovery process.
What Are the Risks of Untreated Drug Withdrawal?
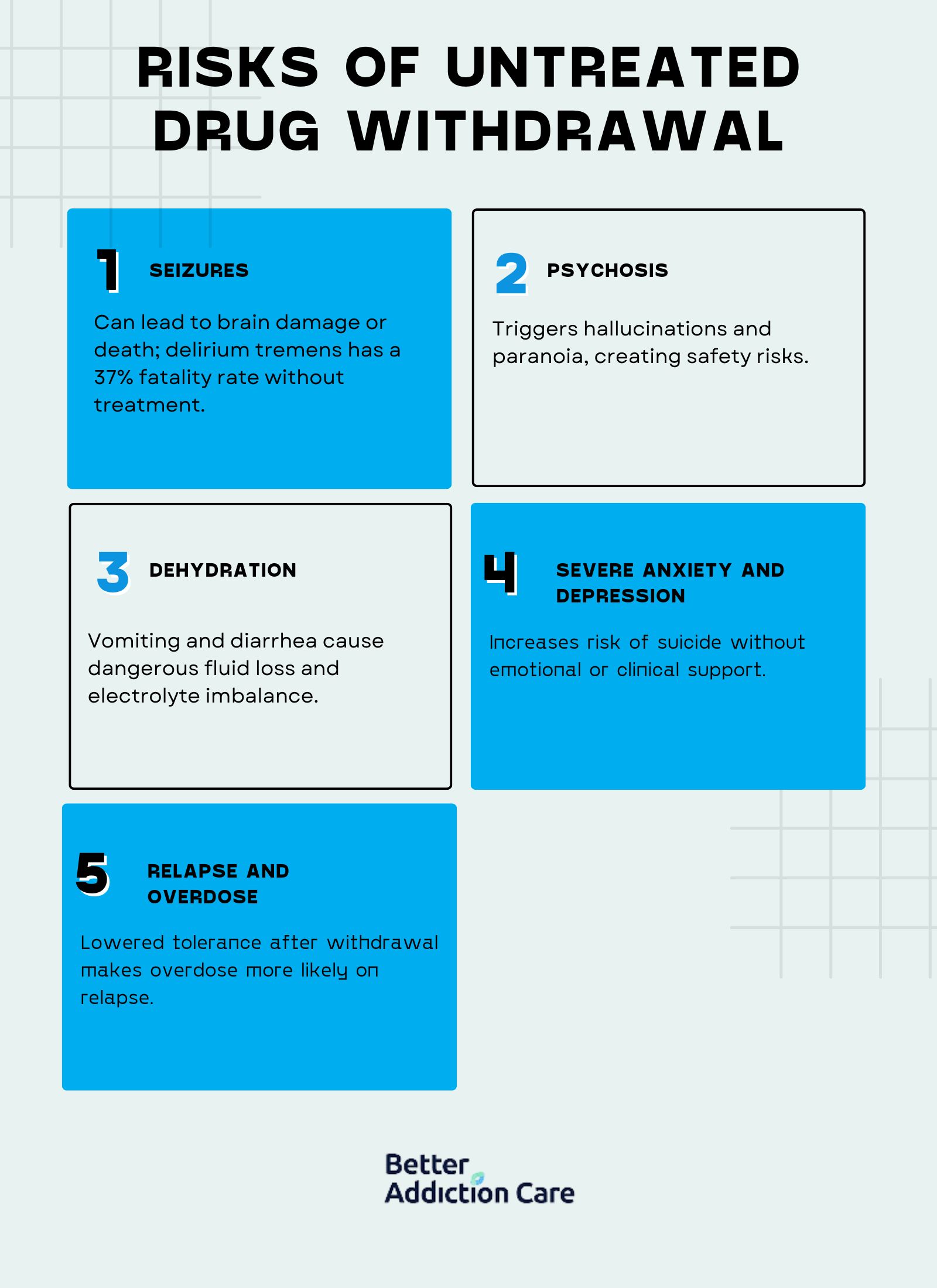
The risks of untreated drug withdrawal lead to severe health complications and even life-threatening emergencies. Without proper medical supervision, individuals are vulnerable to intense physical and psychological symptoms that quickly spiral out of control, increasing the chances of relapse, hospitalization, or death.
The risks of untreated drug withdrawal are as follows:
-
Seizures (Alcohol Withdrawal): Untreated alcohol withdrawal causes dangerous seizures, particularly in individuals with a long history of heavy drinking. Seizures occur suddenly and lead to brain damage or death if not medically managed. According to Medical News Today, "Can alcohol withdrawal be fatal?" The mortality rate for delirium tremens, the most severe form of alcohol withdrawal, reaches approximately 37% without treatment. However, this rate drops to around 5% with timely and proper medical care.
-
Psychosis (Stimulant Withdrawal): Stimulant drugs like cocaine and methamphetamines cause acute psychosis during withdrawal. This involves hallucinations, paranoia, and severe agitation, posing risks to both the individual and others around them.
-
Dehydration (Opioid Withdrawal): Opioid withdrawal leads to vomiting and diarrhea, which cause rapid dehydration and electrolyte imbalance. Without medical intervention, this results in heart problems, kidney failure, or other important health issues.
-
Severe Anxiety and Depression: Psychological symptoms like overwhelming anxiety and depression are common during withdrawal and increase the risk of suicidal thoughts and behaviors without proper therapeutic support.
-
Relapse and Overdose: Individuals who attempt to withdraw without supervision are at a higher risk of relapsing. After a period of abstinence, their tolerance drops, making overdose far more likely if they resume drug use.
Is Medical Intervention Always Required for Drug Withdrawal?
No, medical interventions are not always required for drug withdrawals, but it depends on the substance and the severity of dependence. High-risk withdrawals, such as those from alcohol and benzodiazepines, need medical detox due to the danger of seizures, delirium tremens, or even death.
In contrast, withdrawal from substances like cannabis or mild stimulant use is sometimes managed safely at home under careful monitoring. However, even low-risk withdrawals carry potential complications, and professional guidance is recommended to minimize discomfort, prevent relapse, and ensure safety throughout the process.
What Is the Process of Managing Drug Withdrawal?
The process of managing drug withdrawal involves several carefully coordinated steps to ensure the person's safety, comfort, and long-term recovery. Proper management includes physical stabilization, emotional support, and monitoring for complications.
The process of managing drug withdrawal is as follows:
-
Evaluation and Assessment: This initial phase involves a comprehensive medical and psychological evaluation to determine the severity of withdrawal, history of substance use, co-occurring conditions, and immediate risks. It helps tailor the detox and treatment plan to the individual's needs.
-
Stabilization: Stabilization focuses on helping the patient achieve a medically stable and substance-free state. This involves administering medications to relieve withdrawal symptoms, prevent complications, and manage cravings while offering emotional reassurance.
-
Tapering (When Applicable): For certain drugs like benzodiazepines and opioids, a tapering schedule is used to reduce the substance instead of abrupt cessation, gradually. This reduces the severity of withdrawal symptoms and lowers the risk of serious medical events.
-
Medical Monitoring: Continuous monitoring of vital signs, mental health status, and symptom progression is significant during withdrawal management. In inpatient settings, medical staff respond immediately to emergencies such as seizures or cardiac issues.
-
Emotional and Psychological Support: Managing withdrawal also requires addressing the emotional challenges, such as anxiety, depression, and cravings. Counseling, therapy sessions, and motivational support are offered to prepare individuals for ongoing addiction treatment.
-
Transition to Further Treatment: Detox is just the beginning. Once stabilized, individuals are transitioned to inpatient or outpatient rehab programs to continue their recovery journey through therapy, education, and support services.
Do All Drugs Cause Withdrawal Symptoms?
No, not all drugs cause withdrawal symptoms after stopping use. Substances that create physical dependence, such as opioids, alcohol, benzodiazepines, and stimulants, are well-known for triggering withdrawal syndromes because they alter brain chemistry and bodily functions over time. However, not every drug leads to classic withdrawal symptoms.
For example, psychedelics like LSD or psilocybin do not cause physical dependence or significant withdrawal because they do not impact the brain's reward and tolerance pathways in the same way. Whether or not withdrawal occurs largely depends on the substance's potential to cause dependence and the brain's adaptation to regular exposure.
Is Withdrawal a Sign of Drug Addiction?
Yes, withdrawal is a sign of drug addiction, as it reflects the body's physical dependence on a substance through symptoms like cravings, nausea, and anxiety. However, it's important to distinguish between dependence and addiction. Physical dependence involves tolerance and withdrawal, while addiction also includes compulsive drug use, loss of control, and continued use despite harmful consequences. Experiencing withdrawal indicates a deeper issue, like a drug addiction, especially when combined with behavioral symptoms of addiction.







