Drug Withdrawal Medication: Definition, Types, Side Effects
Drug withdrawal medications play an important role in managing the symptoms associated with substance withdrawal. These medications are designed to ease both physical and psychological symptoms, facilitating a safer and more comfortable detox process. According to Gupta M, Gokarakonda SB, Regina AC, et al. 2024 in a study titled "Withdrawal Syndromes,” the estimated global prevalence of withdrawal in adults is 18.4% for heavy episodic alcohol use, 15.2% for daily tobacco smoking, 0.77% for amphetamines, 0.37% for opioids, and 0.35% for cocaine.
Drug withdrawal medications play an important role in managing the symptoms associated with substance withdrawal. These medications are designed to ease both physical and psychological symptoms, facilitating a safer and more comfortable detox process. According to Gupta M, Gokarakonda SB, Regina AC, et al. 2024 in a study titled "Withdrawal Syndromes,” the estimated global prevalence of withdrawal in adults is 18.4% for heavy episodic alcohol use, 15.2% for daily tobacco smoking, 0.77% for amphetamines, 0.37% for opioids, and 0.35% for cocaine.
Common types of drug withdrawal medication include buprenorphine, methadone, benzodiazepines, and naltrexone. Each type of drug withdrawal medication is designed to address specific symptoms and substances based on individual needs. For opioid withdrawal, medications such as Methadone, Naltrexone, Clonidine, and Suboxone help reduce cravings, stabilize mood, and prevent severe withdrawal symptoms during recovery. In oxycodone withdrawal, Buprenorphine and Methadone are used to ease cravings and withdrawal effects by targeting the same receptors as oxycodone but with a safer profile.
The side effects of drug withdrawal medication include drowsiness, nausea, dizziness, sweating, and occasionally respiratory depression or liver toxicity. For example, opioids and alcohol withdrawal medications cause dizziness, nausea, and fatigue, while benzodiazepine medications might lead to confusion or blurred vision. These effects vary based on the substance being treated and individual response.
What Are Drug Withdrawal Medications?
Drug withdrawal medications are pharmaceutical treatments that help manage the symptoms individuals experience when they stop using addictive substances. These medications are for easing both physical and psychological discomfort, minimizing cravings, and reducing the risk of serious complications during detox.
Drug withdrawal medications include options like methadone and buprenorphine for opioid withdrawal, benzodiazepines for alcohol withdrawal, and clonidine for general withdrawal symptoms. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), medications such as buprenorphine and methadone are highly effective in alleviating withdrawal symptoms and supporting sustained recovery efforts.
What Is Drug Withdrawal?
Drug withdrawal is a set of physical and psychological symptoms that occur when a person who has developed dependence on a substance suddenly reduces or stops its use. Drug withdrawal happens because the body and brain have adapted to the presence of the drug, and without it, normal functioning is disrupted. This condition, known as withdrawal syndrome, causes a wide range of effects, including pain, anxiety, cravings, and mood swings, depending on the substance involved.
What Are the Types of Drug Withdrawal Medications?
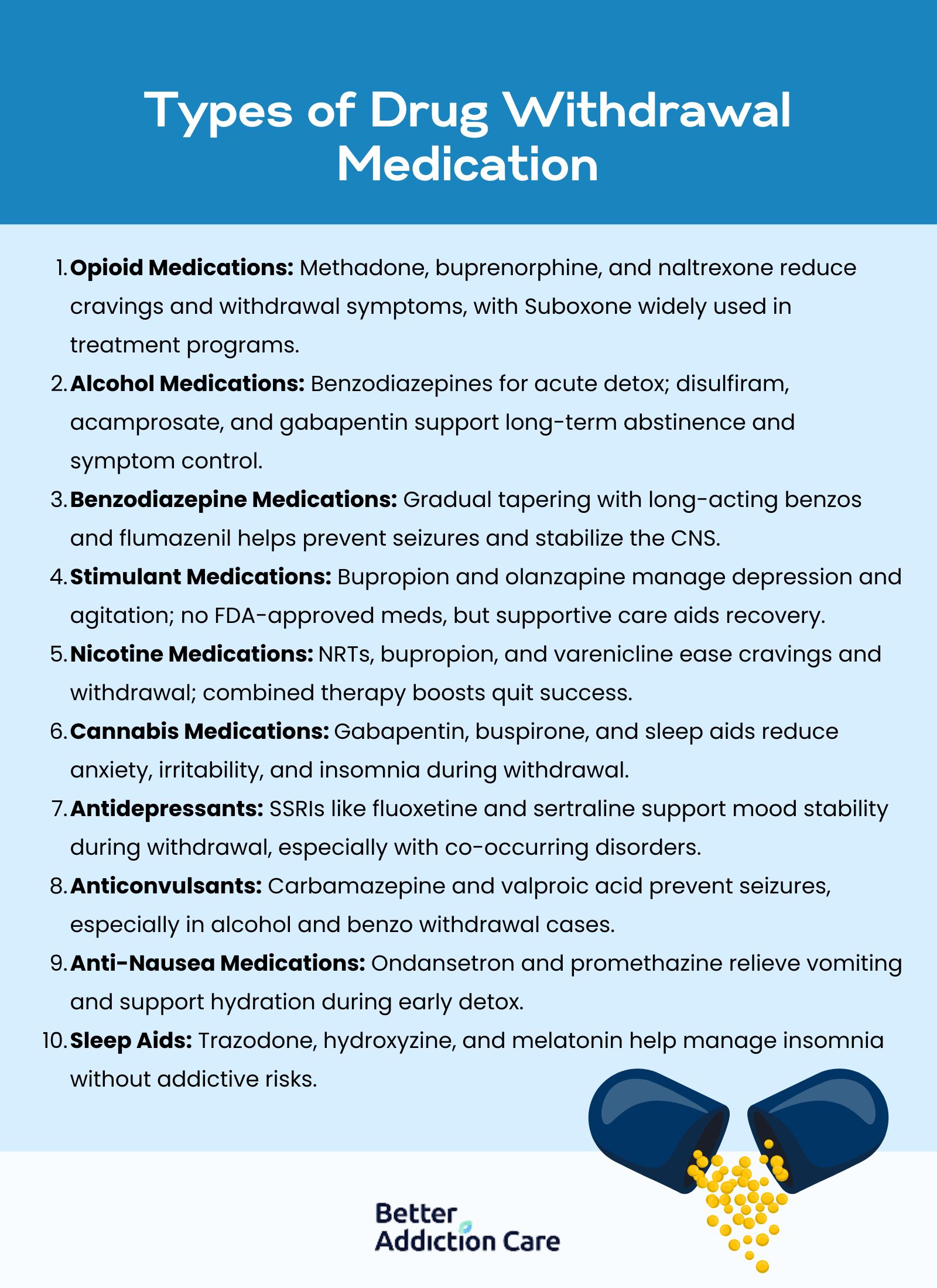
The types of drug withdrawal medications are treatments designed to relieve symptoms, promote stability during detox, and enhance recovery outcomes. These medications support both physical and emotional stabilization, depending on the substance involved and the severity of dependence.
The types of drug withdrawal medications are as follows:
Opioid Withdrawal Medications
Opioid withdrawal medications, such as methadone, buprenorphine, and naltrexone, are used to treat symptoms of opioid dependence by targeting opioid receptors in the brain. Methadone is a full opioid agonist that reduces cravings and withdrawal symptoms without producing significant euphoria. In the U.S., methadone is dispensed through about 1,800 certified opioid treatment programs, serving around 400,000 individuals, just 19% of the estimated 2.1 million people with opioid use disorder, according to the Washington State Standard.
Buprenorphine is a partial agonist, offering a safer ceiling effect to prevent overdose. Naltrexone acts as an opioid antagonist, blocking the effects of opioids entirely. Suboxone is a widely used opioid withdrawal medication that contains buprenorphine and naloxone. Availability remains limited, with only 1 in 4 adolescent addiction centers offering Suboxone, as reported by the NIH. A study by Anton RF et al. 2008, titled "Naltrexone for the Management of Alcohol Dependence," found that 73.7% of participants on naltrexone experienced positive clinical outcomes compared to 58.2% on placebo.
Opioid withdrawal symptoms peak within 72 hours and improve over 5 to 10 days, though maintenance treatment with methadone or buprenorphine extends for months to years, depending on individual recovery needs.
Alcohol Withdrawal Medications
Alcohol withdrawal medications are important for preventing life-threatening complications such as seizures, tremors, and delirium tremens (DTs), while also supporting the path to long-term abstinence. During the acute detox phase, benzodiazepines like diazepam (Valium) and lorazepam (Ativan) are the primary treatments, working by enhancing GABAergic neurotransmission to calm the hyperactive brain activity caused by alcohol cessation.
According to ClinCalc data from 2022, diazepam accounted for approximately 3.09 million prescriptions and lorazepam for 8.5 million, highlighting their central role in withdrawal management. Beyond detox, other medications play significant roles in maintaining recovery. Disulfiram (Antabuse) discourages alcohol consumption by triggering unpleasant reactions like nausea and flushing if alcohol is ingested, promoting sobriety after detox; a 2010 study by Ulrichsen, J., Nielsen, M.K., and Ulrichsen, M., et al. 2010, titled “Disulfiram in Severe Alcoholism—An Open Controlled Study," showed that 26% of patients maintained abstinence with disulfiram compared to 20% in the control group.
Acamprosate (Campral) stabilizes disrupted brain chemistry to reduce cravings, with research by Yahn SL, Watterson LR, Olive MF. et al. 2013, titled "Safety and efficacy of acamprosate for the treatment of alcohol dependence," demonstrating that it decreased the risk of returning to drinking by 86%.
Gabapentin, primarily known for treating nerve pain and seizures, has proven effective in reducing alcohol cravings, anxiety, and insomnia during withdrawal; Furieri FA, Nakamura-Palacios EM. et al. 2007, titled "Gabapentin reduces alcohol consumption and craving: a randomized, double-blind, placebo-controlled trial," found that 75% of studies using gabapentin alone showed positive outcomes.
Clinicians use tools like the Clinical Institute Withdrawal Assessment for Alcohol Scale (CIWA-Ar) to monitor symptom severity and guide medication dosing throughout the 7 to 10-day detox process, ensuring both safety and stability for long-term treatment engagement.
Benzodiazepine Withdrawal Medications
Benzodiazepine withdrawal medications focus on carefully supervised tapering strategies to prevent life-threatening complications like seizures, severe rebound anxiety, and destabilization of the central nervous system. Long-acting benzodiazepines such as diazepam and lorazepam are commonly used to gradually reduce dependence, allowing the brain's GABA receptors to adjust slowly without triggering dangerous hyperexcitability.
In some clinical detox settings, flumazenil, a benzodiazepine receptor antagonist, is administered intravenously to help reverse sedation effects and stabilize withdrawal; a 2022 study by MacDonald T. et al. 2022 titled “Outcomes of patients treated with low-dose flumazenil for benzodiazepine detoxification: A description of 26 participants,” reported that 73.1% of patients treated with low-dose flumazenil remained abstinent at one month, 65.4% at two months, and 61.5% at three months.
Tapering schedules are highly individualized, spanning several weeks or months depending on the intensity and duration of prior benzodiazepine use. Close medical monitoring throughout the taper is important to adjust dosages safely and avoid destabilization. When properly managed, benzodiazepine withdrawal treatment significantly reduces health risks and helps individuals transition toward sustained recovery without developing new dependencies.
Stimulant Withdrawal Medications
Stimulant withdrawal medications, although less standardized, include antidepressants like bupropion and antipsychotics like olanzapine to address acute psychiatric symptoms. Stimulant withdrawal primarily causes psychological distress such as depression, fatigue, and agitation rather than life-threatening physical symptoms.
Medications act by stabilizing dopamine and serotonin levels, which are disrupted by chronic stimulant use. Although no FDA-approved drug exists specifically for stimulant withdrawal, supportive pharmacotherapy improves comfort and reduces relapse risk. Symptoms peak within several days and resolve within 1 to 2 weeks, though medications for mood stabilization are needed for longer periods.
Nicotine Withdrawal Medications
Nicotine withdrawal medications, including nicotine replacement therapies (NRTs), bupropion, and varenicline, assist individuals in managing cravings and withdrawal symptoms by targeting nicotinic acetylcholine receptors in the brain. NRTs deliver small, controlled amounts of nicotine to prevent withdrawal distress, while bupropion acts on dopamine and norepinephrine pathways, and varenicline partially stimulates nicotine receptors to ease cravings.
Combining pharmacotherapy with behavioral interventions has been shown to double or even triple smoking cessation success rates. Withdrawal symptoms peak within 3 days and gradually subside over 2 to 4 weeks, with medications continued for 8 to 12 weeks for best results.
Cannabis Withdrawal Medications
Cannabis withdrawal medications such as gabapentin, buspirone, and sleep aids are used to manage symptoms like irritability, anxiety, and insomnia that occur when heavy cannabis use is stopped. Gabapentin regulates GABA and glutamate neurotransmission, while buspirone addresses anxiety without sedating side effects.
Although cannabis withdrawal is less dangerous than alcohol or opioid withdrawal, the psychological discomfort is significant enough to hinder recovery. Research shows that medications like gabapentin significantly reduce the severity of withdrawal symptoms. Symptoms usually peak within the first week of cessation and diminish over two to three weeks.
Antidepressants for Withdrawal Support
Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs) like fluoxetine and sertraline, are prescribed to support individuals experiencing depressive symptoms during withdrawal. Withdrawal destabilizes serotonin and dopamine systems, leading to mood disturbances that increase relapse risk.
Antidepressants work by correcting these chemical imbalances, promoting emotional stability during early recovery. Scientific evidence supports their use, particularly in individuals with co-occurring mood disorders or substance-induced depression. Therapeutic effects emerge within 4 to 6 weeks, and antidepressants are continued for several months as part of comprehensive addiction treatment plans.
Anticonvulsants for Withdrawal Symptoms
Anticonvulsants such as carbamazepine and valproic acid play an important role in preventing seizures during withdrawal from alcohol and benzodiazepines. These medications stabilize neuronal activity by modulating sodium and calcium channels, reducing the risk of excessive excitatory firing in the brain.
Anticonvulsants are particularly useful in patients where benzodiazepine treatment is risky or insufficient. Carbamazepine is as effective as benzodiazepines in managing mild to moderate alcohol withdrawal. Anticonvulsants are administered during the acute detox phase, lasting about 5 to 10 days, but continued use is necessary based on seizure risk.
Anti-Nausea Medications for Withdrawal
Anti-nausea medications like ondansetron and promethazine are prescribed during withdrawal to manage vomiting, nausea, and gastrointestinal distress. These medications block serotonin or dopamine receptors in the brain's vomiting centers.
Proper nausea management is important for maintaining hydration and nutritional intake, which directly impacts physical recovery during detox. Anti-nausea treatments are most needed in the first few days of withdrawal, but are extended as necessary based on patient needs and symptom persistence.
Sleep Aids for Withdrawal Recovery
Sleep aids, including trazodone, hydroxyzine, and melatonin, are frequently utilized during withdrawal to address severe insomnia, a common symptom of many types of substance discontinuation. These medications promote natural sleep cycles without the dependency risks associated with sedative-hypnotics like benzodiazepines.
Sleep disturbances not only impair healing but also increase emotional instability and cravings, so addressing them is important for successful recovery. Sleep aids are used during the initial weeks of withdrawal and, if needed, into the post-acute withdrawal phase lasting several months.
What Medications Are Used for Opioid Use Disorder?
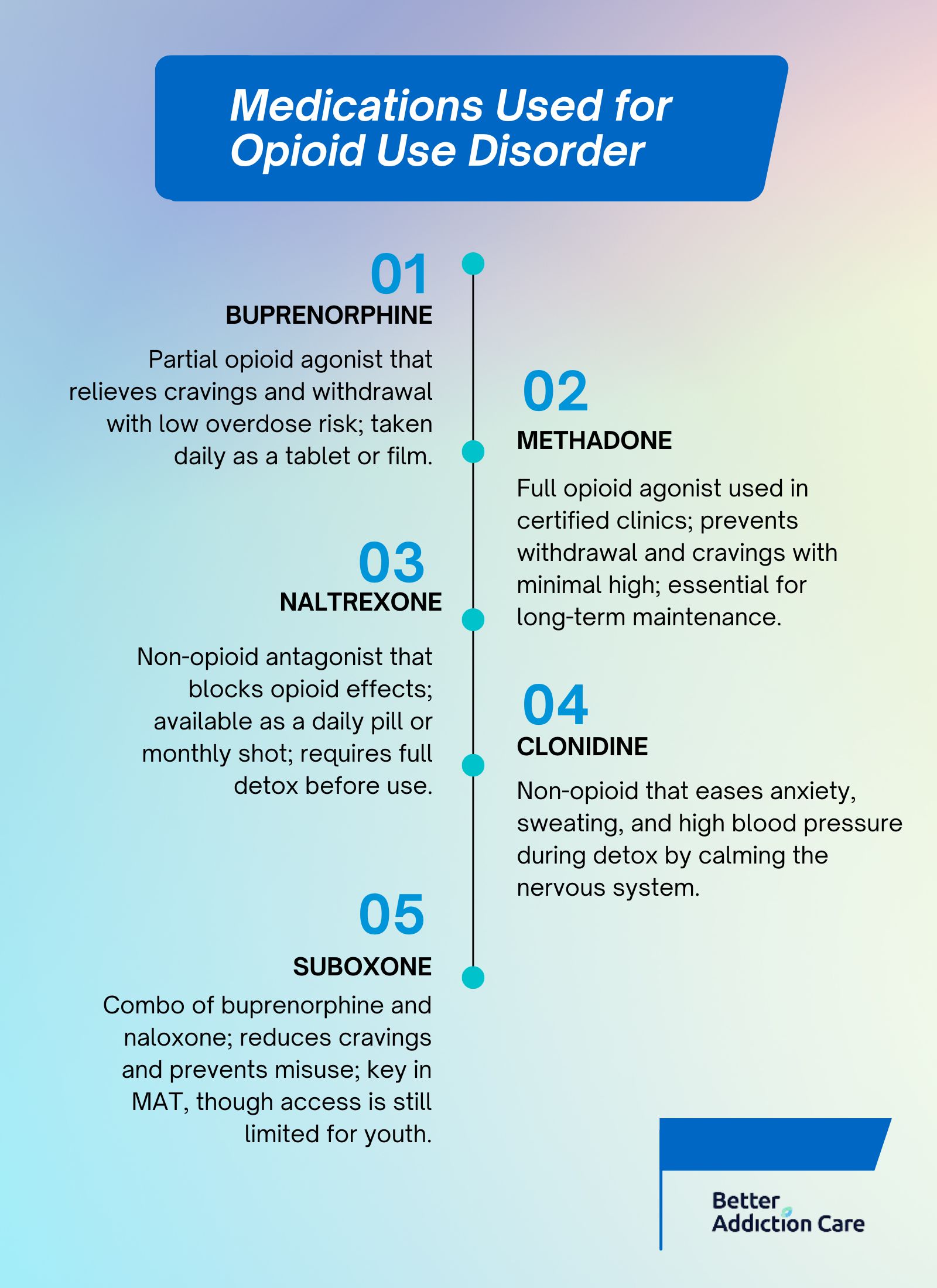
The medications used for opioid withdrawal and opioid use disorder include buprenorphine, methadone, naltrexone, clonidine, and Suboxone. These FDA-approved and widely recognized MAT (medication-assisted treatment) options are significant for managing opioid detox symptoms, minimizing cravings, and promoting long-term recovery. Depending on the phase of treatment, detoxification or maintenance, and individual patient needs, these medications provide different mechanisms of action to support safer transitions away from opioid use disorder.
The medications used for opioid withdrawal are as follows:
-
Buprenorphine: Buprenorphine is a partial opioid agonist that binds to opioid receptors with lower intensity compared to full opioids. It helps relieve withdrawal symptoms and cravings without producing an intense euphoric high, making it a safe option during detox and maintenance. Taken daily as a sublingual tablet or film, buprenorphine also has a ceiling effect that reduces the risk of misuse and overdose, establishing it as a key element of MAT protocols.
-
Methadone: Methadone is a full opioid agonist that occupies the same receptors as heroin and prescription opioids, helping to prevent withdrawal symptoms and cravings while producing minimal euphoria when used appropriately. Administered in doses ranging from 10 mg to 120 mg per day, methadone must be dispensed through federally certified opioid treatment programs. It remains a cornerstone for long-term maintenance therapy due to its proven effectiveness in stabilizing patients.
-
Naltrexone: Naltrexone is a non-opioid opioid antagonist that completely blocks opioid receptors, preventing users from experiencing any euphoric effects if they relapse. Available as a daily oral tablet (50 mg) or a monthly injectable formulation (380 mg Vivitrol), naltrexone is initiated after full detoxification. Unlike methadone or buprenorphine, naltrexone carries no risk of misuse or physical dependence, offering an important alternative for individuals seeking non-opioid-based recovery solutions.
-
Clonidine: Clonidine is an alpha-2 adrenergic agonist used off-label to alleviate opioid withdrawal symptoms such as anxiety, agitation, sweating, and high blood pressure. Although not an opioid itself, clonidine reduces sympathetic nervous system overactivity during detoxification. While slightly less effective than buprenorphine in controlling all withdrawal symptoms, clonidine remains a valuable option to ease acute withdrawal and support initial stabilization.
-
Suboxone: Suboxone is a combination medication containing buprenorphine and naloxone. Buprenorphine suppresses withdrawal symptoms and cravings, while naloxone acts as an abuse-deterrent by precipitating withdrawal if the medication is injected instead of taken orally. Suboxone is administered sublingually, in daily doses ranging from 4 mg to 24 mg. As a central component of modern MAT programs, Suboxone offers both safety and effectiveness, though access remains limited in specific demographics, such as adolescent treatment centers.
What Medications Are Used for Alcohol Addiction?

The medications used for alcohol addiction include disulfiram, acamprosate, naltrexone, gabapentin, and topiramate. These FDA-approved or evidence-supported treatments are paramount for reducing cravings, supporting abstinence, and preventing relapse after detox. Each medication works through different mechanisms to stabilize brain chemistry disrupted by chronic alcohol use, helping patients with alcohol addiction maintain long-term sobriety alongside therapy and behavioral interventions.
The medications used for alcohol addiction are as follows:
-
Disulfiram: Disulfiram, commonly known by its brand name Antabuse, works by causing unpleasant physical reactions such as nausea, flushing, and palpitations if alcohol is consumed. This aversive effect creates a strong deterrent against drinking. Disulfiram is prescribed after the detoxification phase when the patient has already stopped drinking. Patients using disulfiram had higher abstinence rates compared to controls, as studied by Skinner MD, Lahmek P, Pham H, Aubin HJ. et al. 2014, titled "Disulfiram efficacy in the treatment of alcohol dependence: a meta-analysis."
-
Acamprosate: Acamprosate (Campral) helps stabilize neurotransmitter activity in the brain, particularly balancing glutamate and GABA systems disrupted by long-term alcohol exposure. It is used to reduce post-acute withdrawal symptoms like insomnia, anxiety, and cravings. Taken as two 333 mg tablets three times daily, acamprosate significantly improves the chances of maintaining abstinence, with a study by Witkiewitz K, Saville K, Hamreus K. et al. 2012, titled "Acamprosate for treatment of alcohol dependence: mechanisms, efficacy, and clinical utility," showing an 86% reduction in relapse risk among treated patients.
-
Naltrexone: Naltrexone blocks opioid receptors involved in the brain's reward system, reducing the pleasurable effects associated with alcohol consumption and thereby diminishing the urge to drink. Available both as a daily oral tablet (50 mg) and a once-monthly injectable formulation (Vivitrol 380 mg), naltrexone has demonstrated strong outcomes in helping individuals achieve and maintain sobriety. Unlike disulfiram, it does not require abstinence before initiation and is started while the individual is still drinking to help cut down consumption.
-
Gabapentin: Gabapentin, although developed initially for seizures and nerve pain, is increasingly used off-label to manage symptoms associated with alcohol withdrawal and early recovery. It alleviates insomnia, anxiety, and cravings by modulating GABA activity, providing a smoother stabilization after detox. Anton RF, Latham P, Voronin K, et al. 2020, titled "Efficacy of Gabapentin for the Treatment of Alcohol Use Disorder in Patients With Alcohol Withdrawal Symptoms: A Randomized Clinical Trial," report that approximately 75% of trials using gabapentin for alcohol dependence showed positive treatment outcomes, making it a valuable adjunct medication.
-
Topiramate: Topiramate, an anticonvulsant, has shown effectiveness in reducing alcohol cravings and promoting abstinence by influencing GABA and glutamate neurotransmission. Although not formally FDA-approved for alcohol use disorder, it is prescribed off-label when first-line treatments are ineffective or poorly tolerated. Research suggests that topiramate reduces heavy drinking days and improves overall abstinence rates, although careful dose titration is necessary to manage side effects like cognitive slowing or paresthesia.
What Are the Side Effects of Drug Withdrawal Medications?
The side effects of drug withdrawal medications include nausea, dizziness, drowsiness, dry mouth, constipation, mood swings, and sleep disturbances. These effects vary depending on the substance being treated and the specific medication used. While they are generally manageable, understanding these side effects is important to ensure safe withdrawal management and minimize additional health risks.
The side effects of drug withdrawal medications are as follows:
Opioid Withdrawal Medications
Opioid withdrawal medications, such as buprenorphine and methadone, commonly cause nausea, dizziness, constipation, sweating, and headache. Nausea and dizziness result from the medications' effects on the central nervous system and gastrointestinal tract, while constipation occurs due to slowed intestinal motility, an opioid-related typical impact. Sweating and headaches are linked to the body's adjustment to the medication's partial agonist or antagonist actions.
Alcohol Withdrawal Medications
Alcohol withdrawal medications, including benzodiazepines and acamprosate, lead to drowsiness, dry mouth, fatigue, and low blood pressure. Drowsiness and fatigue occur as these medications depress the central nervous system to stabilize withdrawal symptoms. Dry mouth results from reduced saliva production, and low blood pressure (hypotension) occurs due to the sedative properties of the medications, requiring careful monitoring during detox.
Benzodiazepine Withdrawal Medications
Medications used for benzodiazepine withdrawal, such as diazepam and flumazenil, cause drowsiness, confusion, blurred vision, and muscle weakness. Drowsiness and confusion happen because these drugs alter GABA neurotransmission, which impacts cognitive and motor functions, as studied by Mind in "Side effects of Benzodiazepines." Blurred vision and muscle weakness are less common but occur due to central nervous system suppression and muscle relaxation effects.
Stimulant Withdrawal Medications
Stimulant withdrawal medications cause insomnia, anxiety, headache, and upset stomach. Insomnia and anxiety arise as the brain adjusts to decreased dopamine stimulation, commonly disrupted during stimulant use, according to MedLink Neurology, in "Stimulant-dependent sleep disorder." Headaches and gastrointestinal discomfort result from the nervous system's response to withdrawal and medication effects on the vascular and digestive systems.
Nicotine Withdrawal Medications
Nicotine withdrawal medications, including nicotine replacement therapies and bupropion, lead to dry mouth, nausea, dizziness, and vivid dreams. Dry mouth and nausea occur as side effects of altered neurotransmitter activity, while dizziness reflects changes in cardiovascular function, as Drugs.com studied in "Bupropion Side Effects: Common, Severe, Long Term.” Vivid dreams are linked to the way medications like bupropion influence REM sleep cycles during withdrawal.
Cannabis Withdrawal Medications
Cannabis withdrawal medications are associated with mood swings, fatigue, difficulty concentrating, and sleep problems. Mood swings and concentration difficulties arise as the endocannabinoid system recalibrates after long-term cannabis exposure. Fatigue and sleep disturbances, including insomnia and vivid dreams, reflect the brain's adaptation to the absence of THC and related psychoactive effects.
How Do Drug Withdrawal Medications Work?
Drug withdrawal medications work by stabilizing brain chemistry, easing withdrawal symptoms, and reducing the risk of dangerous complications. For opioid withdrawal, medications like buprenorphine and methadone bind to opioid receptors to partially or fully activate them, preventing severe cravings and withdrawal pain without producing a high. Alcohol withdrawal medications such as benzodiazepines enhance GABA receptor activity, calming the nervous system to prevent seizures and delirium.
For benzodiazepine withdrawal, long-acting agents like diazepam are used in tapering schedules to gradually reduce GABA receptor stimulation, allowing the brain to adjust safely over time. Across all substances, the mechanisms focus on receptor binding, slow tapering, and symptom relief to support safe recovery.
What Is the Timeline for Using Withdrawal Medications?
The timeline for using withdrawal medication depends on the severity of the addiction, the substance involved, and individual patient needs. In the short term, medications are used during the acute withdrawal phase, which lasts a few days to a few weeks, depending on the drug (for example, opioid detox lasts 7 to 10 days). During this phase, withdrawal medications stabilize symptoms and prevent health crises.
In the long term, especially in cases like opioid or alcohol addiction, medications continue for months or even years as part of medication-assisted treatment (MAT) to support recovery and prevent relapse. Tapering schedules are customized based on detox duration and the management of post-acute withdrawal symptoms.
Where to Get Drug Withdrawal Medication?
Drug withdrawal medications are obtained from licensed healthcare providers who assess, prescribe, and monitor treatment. They are available through primary care doctors, addiction specialists, and detox or rehab centers that offer medication-assisted treatment (MAT) programs. Inpatient and outpatient rehab facilities integrate medication into their broader recovery services.
Once prescribed, many withdrawal medications are filled at pharmacies. Specialized MAT clinics and federally certified opioid treatment programs (OTPs) also distribute medications like methadone and buprenorphine under supervision to ensure safe use and minimize the risk of dependence or misuse.
What Are the Benefits of Using Drug Withdrawal Medications?
The benefits of using withdrawal medications are symptom relief, reduced cravings, and increased treatment success. These medications help ease the most difficult parts of withdrawal, making it easier for individuals to safely detox and stay engaged in recovery programs without overwhelming discomfort or relapse.
The benefits of using withdrawal medications are as follows:
-
Symptom relief: Withdrawal medications significantly reduce acute symptoms like anxiety, nausea, sweating, and cravings, helping individuals manage the physical and psychological distress of detox more comfortably. This relief supports safer, more tolerable detox experiences.
-
Reduced cravings: By interacting with brain receptors, medications like buprenorphine or naltrexone lower intense drug cravings, reducing the urge to relapse during early recovery stages. This allows patients to focus more on therapy and long-term recovery planning.
-
Increased treatment success: With proper medical management, withdrawal medications improve retention in treatment programs and support sustained recovery. They provide the necessary support needed to stabilize individuals during detox and early recovery, which is when relapse risk is highest.
What Are the Risks of Using Withdrawal Medications?
The risks of using withdrawal medications are dependency, side effects, and the potential for. While these medications offer major benefits during detox and recovery, they must be carefully prescribed and monitored to minimize new health complications or addiction risks.
The risks of using withdrawal medications are as follows:
-
Dependency: Some withdrawal medications, especially opioid-based ones like methadone, carry a risk of creating new physical dependencies if not carefully tapered or monitored.
-
Side effects: Withdrawal medications cause side effects such as dizziness, nausea, drowsiness, or low blood pressure. Managing these side effects is important for patient safety and comfort and requires individualized dosing and medication selection adjustments.
-
Misuse potential: Certain withdrawal medications have a risk of being misused, particularly if taken outside of prescribed guidelines. Drugs like Suboxone and methadone must be dispensed in controlled settings to prevent diversion, abuse, or unsupervised dose escalation.
What Is the Difference Between Detox and Taking Withdrawal Medications?
The difference between detox medications and withdrawal medications is that detox medications are primarily used for immediate, short-term relief during the acute phase of withdrawal. At the same time, withdrawal medications also support long-term management and relapse prevention. During medical detox, medications are administered to stabilize patients and alleviate severe symptoms like seizures, hallucinations, or extreme cravings.
In contrast, withdrawal medications, especially those used in medication-assisted treatment (MAT), continued for weeks, months, or longer to maintain symptom control, reduce cravings, and prevent relapse after the acute withdrawal phase ends. Both approaches aim for symptom relief but differ in duration and overall treatment goals.
What Are the Drug Withdrawal Symptoms Treated by Medications?
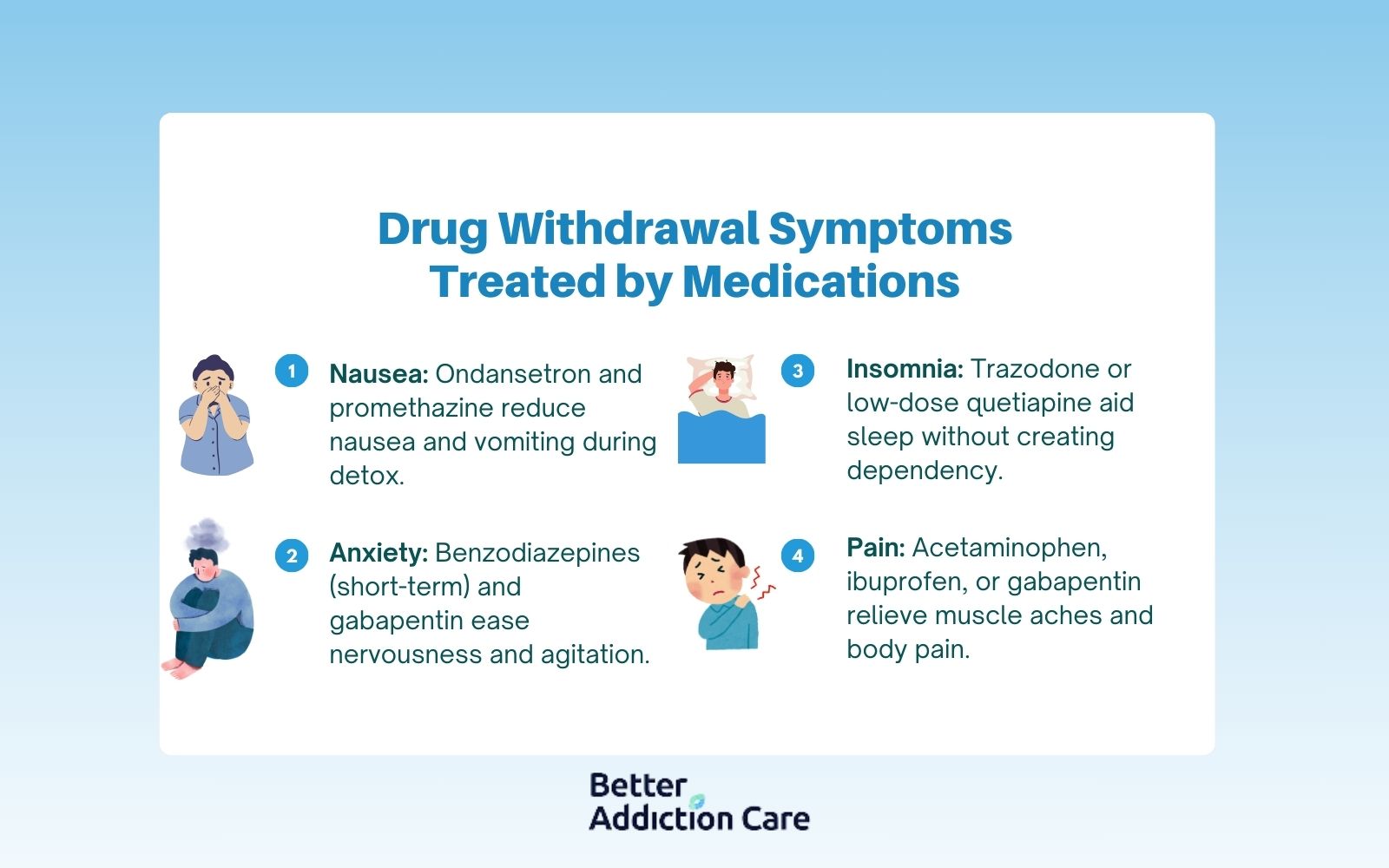
The drug withdrawal symptoms treated by medications are primarily those that cause significant discomfort or risk during detox, such as nausea, insomnia, anxiety, and physical pain. Effective symptom management through MAT (medication-assisted treatment) and detox medications helps ensure safer withdrawal and supports long-term recovery.
The drug withdrawal symptoms treated by medications are as follows:
-
Nausea: Medications like ondansetron or promethazine ease nausea and vomiting during detox, providing relief and preventing dehydration.
-
Insomnia: Sleep disturbances are common in withdrawal; medications like trazodone or low-dose quetiapine are prescribed to help restore restful sleep without promoting new dependencies.
-
Anxiety: Anti-anxiety medications such as benzodiazepines (for short-term detox) or non-addictive options like gabapentin are used to calm excessive nervousness and emotional distress.
-
Pain: Non-opioid pain relievers like acetaminophen, ibuprofen, or gabapentin help manage muscle aches, cramps, and overall body pain that accompany withdrawal.
How Quickly Do Drug Withdrawal Medications Work?
The speed at which drug withdrawal medications work depends on whether they are treating acute withdrawal symptoms or post-acute withdrawal syndrome (PAWS). In acute withdrawal, medications like buprenorphine for opioids or benzodiazepines for alcohol withdrawal start working within a few hours, providing noticeable relief during the first 24 to 72 hours of detox.
For post-acute withdrawal symptoms, such as anxiety, sleep disturbances, and cravings, medications like acamprosate or naltrexone take several days to weeks to achieve full therapeutic effects. The detox timeline varies by substance, but most acute symptoms are managed within 7 to 14 days, while treatment for PAWS continues for several months to stabilize long-term recovery.
What Happens if I Relapse While Taking Drug Withdrawal Medications?
If you relapse while taking drug withdrawal medications, the outcome depends on the specific medication you are prescribed. For instance, relapsing while on naltrexone offers immediate protection because it blocks the euphoric effects of opioids or alcohol, reducing reinforcement and helping prevent a full return to substance use.
However, relapsing while on buprenorphine or methadone is still risky; although these medications reduce cravings and withdrawal, using opioids on top of them overrides their protective effects, leading to overdose due to lowered tolerance.
Studies, including one by the National Institute on Drug Abuse (NIDA), show that individuals who stay on MAT after relapse are more likely to regain sobriety than those who discontinue treatment. Continuing medication management, adjusting doses, and reinforcing behavioral therapies are critical steps after a relapse to support recovery without restarting detox entirely.
How Can Individuals Find Local Drug Rehab Facilities That Offer Medication-assisted Withdrawal Programs?
Individuals find local drug rehab facilities that offer medication-assisted withdrawal programs by searching specialized online directories, consulting healthcare providers, and contacting addiction treatment centers directly. These facilities provide medically supervised detox combined with FDA-approved medications tailored to reduce withdrawal symptoms and support recovery. Verifying insurance coverage and reviewing program details ensures the chosen facility meets individual needs.
Better Addiction Care provides comprehensive resources and assistance in locating appropriate treatment options in your area. Call (888) 766-0149 or use our online tool find local drug rehab facilities that specialize in medication-assisted treatment programs and personalized recovery plans.
Related Articles
Treatment Centers in Oregon









