Amitriptyline HCl: Uses, Side Effects, and Misuse Risks
Amitriptyline hydrochloride (HCl) is a prescription medication classified as a tricyclic antidepressant (TCA). TCAs were among the first antidepressants developed and are still widely used today—not only for depression, but for chronic pain, migraine prevention, insomnia, and certain anxiety-related conditions.

Key Takeaways
-
Amitriptyline HCl is a tricyclic antidepressant (TCA) primarily prescribed for depression, nerve pain, migraines, and sleep-related conditions.
-
It changes how serotonin and norepinephrine function in the brain, which can improve mood and pain perception but also increases side effect risk.
-
Misuse often begins unintentionally through dose escalation, long-term unsupervised use, or using it for sleep relief.
Withdrawal, overdose, and cardiac risks make medical supervision essential, especially if stopping or combining with other substances. Evidence-based treatment options exist for both safe tapering and misuse recovery.
Although newer antidepressants exist, amitriptyline remains prescribed because:
-
It is effective at low doses for pain and sleep
-
It has broad neurological effects
-
It is cost-effective and widely available
However, those same properties also explain why amitriptyline carries higher side effects and misuse risks compared to newer medications.
Amitriptyline is not a controlled substance, but that does not mean it is risk-free.
Why People Search for Amitriptyline Information?
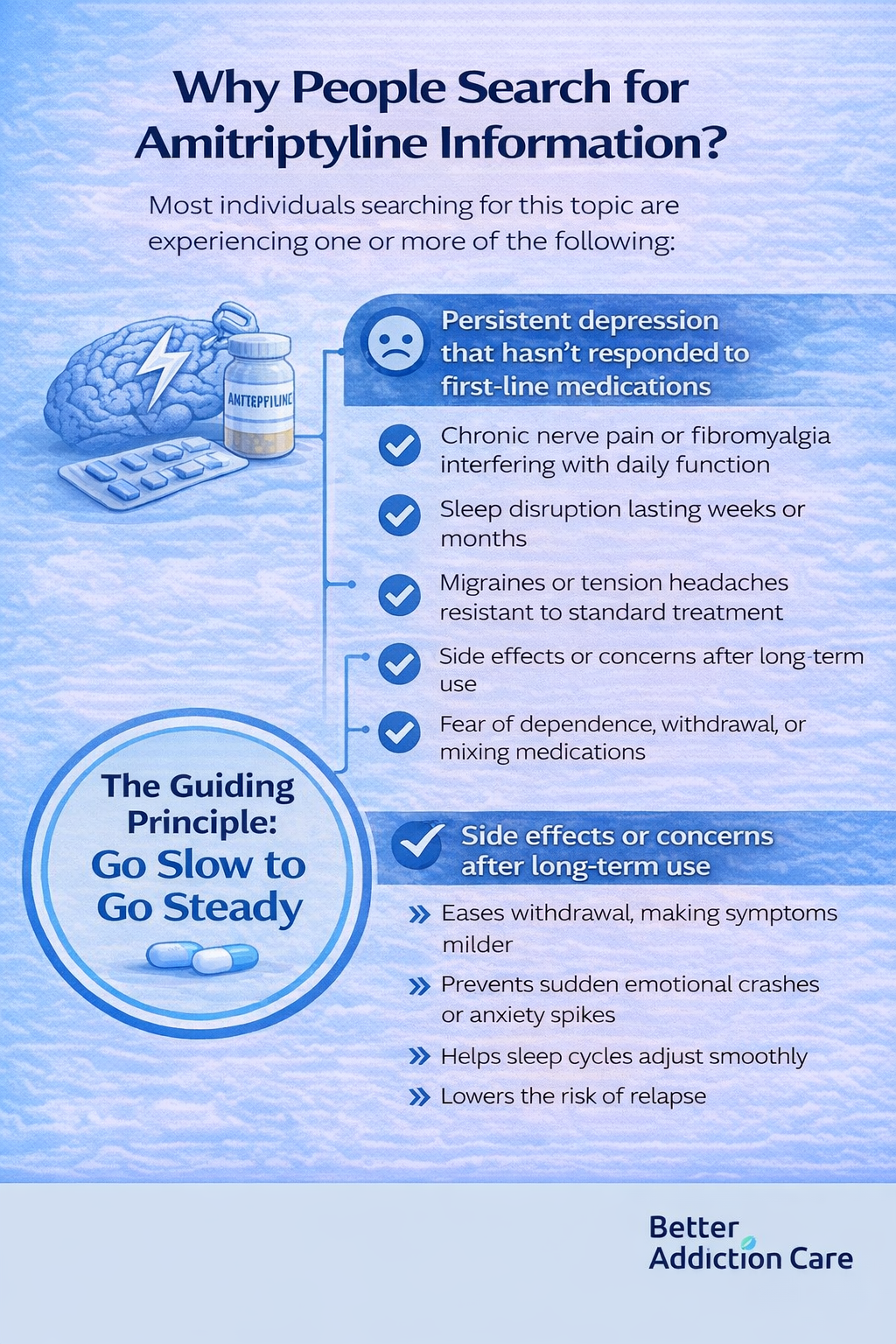
Most individuals searching for this topic are experiencing one or more of the following:
-
Persistent depression that hasn’t responded to first-line medications
-
Chronic nerve pain or fibromyalgia interfering with daily function
-
Sleep disruption lasting weeks or months
-
Migraines or tension headaches resistant to standard treatment
-
Side effects or concerns after long-term use
-
Fear of dependence, withdrawal, or mixing medications
How Amitriptyline Works in the Brain?
Amitriptyline primarily affects two key neurotransmitters:
-
Serotonin – involved in regulating mood, emotional processing, sleep cycles, and appetite.
-
Norepinephrine – plays a role in alertness, attention, pain modulation, and the body’s stress response.
Mechanism of Action
Amitriptyline works by blocking the reuptake of serotonin and norepinephrine in the brain.
Reuptake is the process by which the brain normally clears these neurotransmitters from the synaptic gap to recycle them.
By slowing this process, amitriptyline allows more neurotransmitters to remain active between neurons, enhancing their communication.
Example: Think of neurotransmitters like emails in an inbox.
Normally, they’re quickly deleted after being read. Amitriptyline keeps them in the inbox longer, so more “messages” get delivered, amplifying their effect.
This action explains both the therapeutic effects and some of the side effects:
-
Therapeutic effects: improved mood, reduced anxiety, better sleep, and decreased pain sensitivity.
-
Side effects: drowsiness, dry mouth, constipation, blurred vision, and potential changes in heart rhythm.
By modulating these neurotransmitters, amitriptyline influences multiple brain systems, which is why it can treat depression, chronic pain, and sleep disturbances—but also why careful dosing and monitoring are essential.
Approved and Off-Label Uses of Amitriptyline
1. Major Depressive Disorder
Amitriptyline was originally developed for depression and remains effective, especially in:
-
Severe or treatment-resistant cases
-
Depression with prominent sleep disturbance or physical pain
Clinical response typically appears in 4–6 weeks, not immediately.
2. Chronic Neuropathic Pain
Amitriptyline is commonly prescribed for: [3]
-
Diabetic neuropathy
-
Postherpetic neuralgia
-
Fibromyalgia
Pain relief often occurs at lower doses (10–50 mg) than those used for depression.
3. Migraine Prevention
Unlike acute migraine medications, amitriptyline is used preventively: [3]
-
Taken daily
-
Reduces migraine frequency over 6–8 weeks
-
Especially useful when migraines co-occur with sleep issues
4. Insomnia (Off-Label)
Amitriptyline’s sedating effect makes it frequently prescribed for sleep, even though it is not FDA-approved for insomnia. [2]
This is one of the most common pathways to misuse, particularly when:
-
Doses are increased without guidance
-
Used nightly for months or years
-
Combined with alcohol or sedatives
Typical Dosage Ranges
Higher doses do not necessarily equate to better outcomes.
Side effects increase non-linearly, especially beyond 75 mg/day.
Short-Term Side Effects (First Days to Weeks)

Many people experience side effects during the early phase of amitriptyline treatment, particularly within the first 7 to 14 days. For many individuals, these effects gradually improve within 2–4 weeks as the body adjusts.
However, some symptoms may persist or require dose adjustments.
Common Short-Term Effects
-
Drowsiness or heavy sedation, especially during the day or after dose increases
-
Dry mouth and throat, sometimes leading to increased thirst
-
Constipation, due to slowed intestinal movement
-
Blurred vision, particularly when focusing on close objects
-
Dizziness when standing, known as orthostatic hypotension, caused by temporary drops in blood pressure
These effects are dose-dependent and tend to be more noticeable at higher starting doses or when doses are increased too quickly.
Anticholinergic Effects
Amitriptyline blocks acetylcholine, a neurotransmitter that helps regulate many automatic body functions, including:
-
Saliva production, which keeps the mouth and throat moist
-
Gut movement, which supports normal digestion and bowel function
-
Eye focus, especially for near vision
This mechanism is known as an anticholinergic effect. While it contributes to some of amitriptyline’s therapeutic benefits, it also explains many of the early physical side effects people experience when starting the medication.
Long-Term Side Effects (Weeks to Months)
With ongoing use, amitriptyline may cause additional side effects that develop gradually over weeks or months.
These effects are more likely with higher doses, long-term treatment, or limited medication review, making regular monitoring important.
Cognitive Effects
-
Slowed thinking or mental processing
-
Memory difficulties, particularly short-term recall
-
Reduced concentration, which may affect work or daily tasks
These symptoms are sometimes mistaken for aging, depression, or stress rather than medication effects.
Metabolic & Physical Effects
-
Gradual weight gain, often related to appetite changes
-
Increased appetite, particularly for carbohydrates
-
Heat intolerance, due to impaired temperature regulation
Cardiovascular Risks
Amitriptyline can affect cardiac conduction, meaning it alters how electrical signals travel through the heart.
In some individuals, this may increase the risk of irregular heart rhythms.
Risk is higher with:
-
Higher or rapidly increased doses
-
Pre-existing heart conditions
-
Electrolyte imbalances (such as low potassium or magnesium)
-
Overdose or medication interactions
Because these risks may not cause obvious early symptoms, periodic medical evaluation is essential during long-term use.
When Side Effects Become a Warning Sign?
Seek medical evaluation if you experience:
-
Persistent confusion or disorientation
-
Heart palpitations or fainting
-
Severe constipation lasting days
-
Unusual agitation or mood changes
-
Worsening depression or suicidal thoughts
These are not adjustment effects and should not be ignored.
Amitriptyline and Misuse: How It Actually Begins?
Most amitriptyline misuse does not start intentionally or recreationally. In many cases, it develops gradually as people try to manage persistent symptoms such as poor sleep, emotional distress, or ongoing pain.
Common Misuse Patterns Include:
-
Increasing the dose for better sleep when the original dose no longer feels effective
-
Using daytime doses for emotional numbing, stress relief, or calming effects
-
Taking extra pills during periods of high stress or anxiety
-
Combining amitriptyline with alcohol to intensify sedation or relaxation
Over time, the brain adjusts to repeated exposure. This adaptation means higher doses are needed to achieve the same effect, a process known as tolerance. As tolerance increases, the risk of side effects, dependence, and overdose also rises.
Is Amitriptyline a Drug addiction?
Amitriptyline does not cause classic drug addiction in the way substances like opioids, stimulants, or benzodiazepines do. It does not typically produce cravings or compulsive drug-seeking behavior.
However, amitriptyline can cause physical dependence, meaning:
-
The body adapts to the medication over time
-
Stopping suddenly can trigger withdrawal symptoms, even when used as prescribed
This distinction is clinically important. Dependence is a predictable physiological response, not a personal failing, and it can be managed safely with gradual tapering and medical support.
Amitriptyline Withdrawal (Discontinuation Syndrome)
Stopping amitriptyline suddenly or too quickly can lead to a group of symptoms known as discontinuation syndrome. These symptoms often begin within 24–72 hours after the last dose, especially in individuals who have used the medication for several weeks or longer. [1][2]
Common Withdrawal Symptoms
-
Nausea and gastrointestinal upset, including stomach pain or diarrhea
-
Flu-like body aches, fatigue, and general discomfort
-
Rebound insomnia, often worse than baseline sleep problems
-
Anxiety, irritability, or restlessness
-
Sensory disturbances, sometimes described as “electric shock” sensations or tingling
These symptoms are typically temporary, but they can be distressing without proper preparation.
What Influences Withdrawal Severity?
The intensity and duration of withdrawal symptoms commonly correlate with:
-
Length of time the medication was used
-
Daily dose at the time of discontinuation
-
How quickly the dose is reduced
A gradual, supervised taper over several weeks significantly lowers the risk and severity of withdrawal symptoms.
Safe Discontinuation: What Evidence-Based Tapering Looks Like?
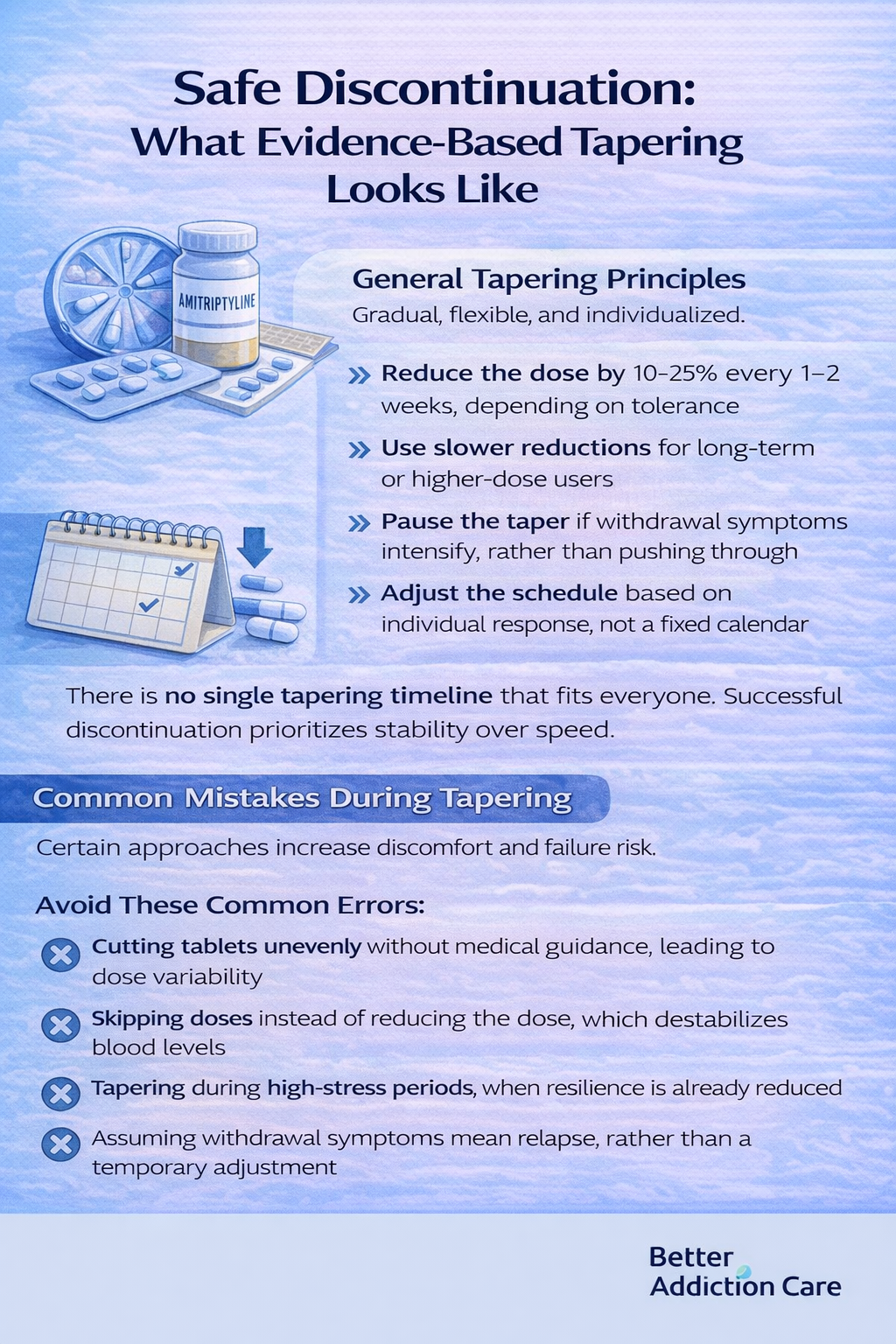
Abrupt discontinuation is one of the most common and avoidable causes of amitriptyline-related distress. Evidence-based tapering focuses on allowing the nervous system time to adjust.
General Tapering Principles
-
Reduce the dose by 10–25% every 1–2 weeks, depending on tolerance
-
Use slower reductions for long-term or higher-dose users
-
Pause the taper if withdrawal symptoms intensify, rather than pushing through
-
Adjust the schedule based on individual response, not a fixed calendar
There is no single tapering timeline that fits everyone. Successful discontinuation prioritizes stability over speed.
Common Mistakes During Tapering
Certain approaches increase discomfort and failure risk.
Avoid These Common Errors:
-
Cutting tablets unevenly without medical guidance, leading to dose variability
-
Skipping doses instead of reducing the dose, which destabilizes blood levels
-
Tapering during high-stress periods, when resilience is already reduced
-
Assuming withdrawal symptoms mean relapse, rather than a temporary adjustment
Withdrawal symptoms resolve with time and proper support. Relapse reflects a return of the underlying condition and requires a different clinical response.
Overdose Risk: Why Amitriptyline Is Clinically Serious?
Amitriptyline overdose is considered a medical emergency. Even doses only 2–3 times higher than prescribed can be life-threatening, particularly in individuals with pre-existing heart conditions, electrolyte imbalances, or when combined with alcohol or other sedating medications.
Overdose Effects
An amitriptyline overdose can impact multiple body systems, including:
-
Neurological: Severe confusion, delirium, agitation, or even coma.
-
Seizures: Overstimulation of the nervous system can trigger convulsions.
-
Cardiovascular: Dangerous heart rhythm disturbances, such as tachycardia, arrhythmias, or conduction blocks, which can be fatal if untreated.
-
Respiratory: Slowed or depressed breathing, which can lead to insufficient oxygen levels.
Because of these risks, tricyclic antidepressants (TCAs) like amitriptyline are prescribed cautiously.
Special care is taken with patients who have suicidal ideation, history of overdose, or concurrent use of interacting medications.
Medical monitoring and clear instructions on safe dosing are essential to prevent accidental toxicity [2].
Dangerous Drug Interactions
Amitriptyline affects the central nervous system and heart, which means combining it with certain substances can significantly increase the risk of serious side effects.
Some interactions can become dangerous even at standard prescription doses.
Avoid Combining Amitriptyline With:
-
Alcohol, which intensifies sedation and impairs breathing
-
Benzodiazepines (such as diazepam or alprazolam), which further depress the nervous system
-
Opioids increase the risk of slowed or stopped breathing
-
Other antidepressants without medical supervision, due to heightened serotonin or cardiac effects
-
Certain heart medications, which may worsen rhythm disturbances
Why These Combinations Are Risky?
When taken together, these substances can significantly increase:
-
Excessive sedation, leading to impaired alertness or loss of consciousness
-
Respiratory suppression, where breathing becomes dangerously slow or shallow
-
Cardiac risk, including irregular heart rhythms and blood pressure instability
Because these interactions may not cause immediate warning signs, medical guidance is essential before combining amitriptyline with any other medication or substance.
When Amitriptyline Use Becomes Concerning?
Amitriptyline use may become concerning when reliance increases or control feels reduced, even if the medication was originally taken exactly as prescribed.
These patterns often develop gradually and can be easy to overlook without regular review.
Consider a Professional Review If
-
You feel unable to sleep or function without amitriptyline
-
Your dose has increased beyond what was originally prescribed
-
You experience anxiety, discomfort, or irritability when a dose is missed
-
You’re using the medication for reasons other than its original purpose, such as emotional numbing or stress relief
-
Stopping or reducing the dose feels physically or emotionally overwhelming
These signs are early indicators of physiological adaptation or dependence, not personal failure. Identifying them early makes safer adjustments more achievable.
Evidence-Based Help Options
The most effective support depends on how amitriptyline is being used and for how long. Treatment plans are individualized and focused on safety and stability.
If You’re Prescribed Amitriptyline
-
Medication review and dose optimization to ensure ongoing benefit
-
A gradual, supervised tapering plan if reduction is appropriate
-
Alternative treatments for pain or sleep, including non-pharmacological options
If Misuse Has Developed
-
Structured outpatient treatment, tailored to medication-related dependence
-
Medication-assisted tapering to reduce withdrawal symptoms
-
Cognitive behavioral therapy (CBT) to address sleep, stress, or emotional reliance
-
Monitoring for relapse triggers, especially during high-stress periods
Professional support significantly reduces withdrawal severity, medical risks, and long-term complications, while improving overall outcomes.
Amitriptyline vs Newer Antidepressants
Many people prescribed amitriptyline wonder why an older antidepressant is still used when newer options exist. The answer lies in the mechanism strength versus the safety margin.
Amitriptyline (TCA)
-
Strong effects on serotonin and norepinephrine
-
Broad impact across multiple brain systems
-
Higher anticholinergic and cardiac risk
-
Narrower therapeutic window (smaller gap between effective and dangerous doses)
SSRIs (Selective Serotonin Reuptake Inhibitors)
-
Target serotonin more selectively
-
Fewer cardiac risks
-
Lower overdose toxicity
-
Often first-line for depression and anxiety
SNRIs (Serotonin–Norepinephrine Reuptake Inhibitors)
-
Affect both serotonin and norepinephrine, but more selectively than TCAs
-
Commonly used for pain and depression
-
Better tolerated long-term for many individuals
Why is Amitriptyline still prescribed?
Despite the availability of newer antidepressants, amitriptyline remains in use because it can be highly effective when other treatments fall short.
Clinicians may consider it when symptoms are complex or resistant to first-line options.
Amitriptyline is often prescribed because:
-
It works well for pain-dominant symptoms, including neuropathic pain and fibromyalgia [3]
-
It can improve sleep disruption associated with depression or chronic pain
-
It may benefit individuals with treatment-resistant depression, where other medications have failed
However, this effectiveness comes with a greater physiological burden on the body. Its broad effects on the brain, nervous system, and heart mean that regular monitoring and dose reassessment are essential, particularly with long-term use.
Amitriptyline and Emotional Regulation
While amitriptyline can reduce depressive symptoms and emotional distress, it may also dampen emotional responsiveness in some individuals, especially at higher doses or with prolonged use.
This can include:
-
Reduced ability to feel pleasure or emotional reward
-
Flattened emotional reactions, both positive and negative
-
Decreased motivation or emotional engagement
These effects are not universal and do not occur in everyone. However, when they do appear, they should prompt a medication review, not silent endurance or dose escalation.
Amitriptyline for Sleep: Why This Use Is Often Misunderstood?
Sleep-related prescribing is one of the most commonly misunderstood aspects of amitriptyline use. While it is frequently used for insomnia, it is not a sleep medication by design.
Why It’s Commonly Used for Sleep?
-
Sedation occurs quickly, often within days
-
Low doses are initially effective for sleep onset
-
It is not a controlled substance, leading to a perception of lower risk
Why Problems Develop Over Time?
-
Sedation does not equal restorative sleep
-
Tolerance can develop within weeks, reducing effectiveness
-
Dose escalation becomes tempting as sleep benefits fade
-
Underlying insomnia remains untreated, especially when behavioral factors are ignored
Amitriptyline can help you fall asleep, but it does not correct sleep architecture or address the root causes of chronic insomnia over the long term. For many individuals, this mismatch contributes to dependence and long-term sleep difficulties.
Psychological Reliance: The Overlooked Risk
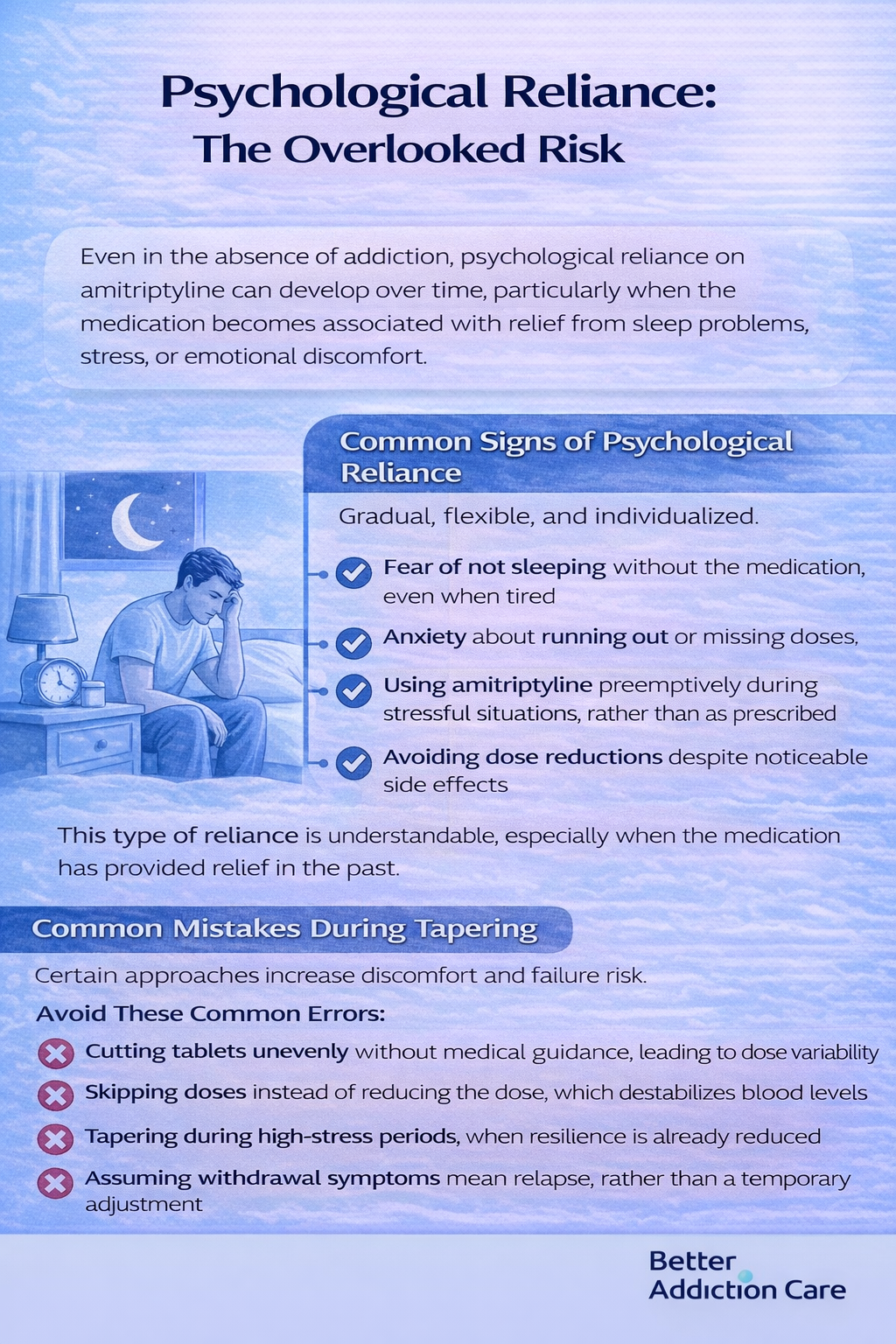
Even in the absence of addiction, psychological reliance on amitriptyline can develop over time, particularly when the medication becomes associated with relief from sleep problems, stress, or emotional discomfort.
Common Signs of Psychological Reliance
-
Fear of not sleeping without the medication, even when tired
-
Anxiety about running out or missing doses
-
Using amitriptyline preemptively during stressful situations, rather than as prescribed
-
Avoiding dose reductions despite noticeable side effects
This type of reliance is understandable, especially when the medication has provided relief in the past. Importantly, it is treatable through structured tapering, supportive therapy, and alternative symptom-management strategies.
What Safe Amitriptyline Use Actually Looks Like?
Safe amitriptyline use is not defined by the absence of side effects or challenges, but by ongoing evaluation and adjustment over time. Safety depends on how intentionally the medication is used and monitored.
Evidence-Based Safety Practices
-
Regular medication reviews every 3–6 months to reassess benefit and risk
-
Clear treatment goals, focusing on one primary target (sleep, pain, or mood—not all simultaneously)
-
Use of the lowest effective dose rather than automatic escalation
-
Routine monitoring for cognitive changes and cardiac side effects
-
Defined tapering plans before committing to long-term continuation
When these practices are missing, the likelihood of side effects, dependence, and misuse increases over time.
If You’re Considering Stopping Amitriptyline
Stopping amitriptyline is possible—even after years of use—but how the medication is discontinued matters more than the decision itself.
-
Never stop abruptly, unless medically necessary
-
Expect temporary discomfort during the tapering process
-
Symptoms during taper are not the same as relapse
-
Slower dose reductions improve success and tolerability
-
Professional support significantly improves outcomes
Discontinuation should be viewed as a gradual process, not a single event. With the right plan, most people can reduce or stop amitriptyline safely and successfully.
What Recovery and Stability Look Like?
Recovery and stability do not mean never needing medication again or avoiding treatment altogether. Instead, stability is defined by informed, intentional use and a clear sense of control over treatment decisions.
Stability typically includes:
-
Using medication intentionally, with a clear purpose and regular reassessment
-
Understanding risks and benefits clearly, rather than relying on assumptions
-
Having alternative strategies in place for sleep, pain, or emotional regulation
-
Feeling in control of medication use, rather than dependent on it to function
With proper medical guidance, many people can transition to safer medication regimens, reduce their dose, or discontinue amitriptyline entirely when appropriate. Progress may be gradual, but it is achievable with the right support and monitoring.
Final Perspective: Using Amitriptyline Safely and Responsibly
Amitriptyline HCl is a powerful and versatile medication that can provide meaningful relief from depression, chronic pain, migraines, and sleep disturbances.
Its effectiveness stems from its broad impact on multiple neurotransmitter systems, which allows it to address both mood and physical symptoms.
If you’re using amitriptyline, safe and responsible use involves:
-
Regular medical review: Periodic check-ins with a healthcare provider help ensure the dose is still appropriate, benefits continue to outweigh risks, and side effects are managed promptly.
-
Avoiding silent dose escalation: Increasing the dose without guidance can lead to dependence, overdose, or worsening side effects. Any adjustments should always be supervised.
-
Understanding and managing dependence: Physical dependence can develop with long-term use, but it is predictable and manageable with structured tapering plans and support.
-
Seeking support when needed: Professional guidance—including medication review, tapering strategies, and behavioral therapies—significantly improves safety, comfort, and long-term outcomes.
Help exists, and safer paths forward are possible with the right guidance.
FAQs
Amitriptyline can be used long-term for certain conditions, but only with regular medical reassessment. Extended use increases the risk of cognitive slowing, weight gain, and cardiac effects, especially at higher doses. Periodic dose review helps ensure benefits continue to outweigh risks.
Yes. Abruptly stopping amitriptyline can trigger discontinuation symptoms such as nausea, anxiety, sleep disturbance, and flu-like discomfort. These symptoms are usually temporary but can be distressing. Gradual dose reduction over weeks, guided by a clinician, significantly lowers withdrawal severity.
Amitriptyline does not cause classic drug addiction involving cravings or compulsive use. However, it can lead to physical dependence and psychological reliance, particularly with long-term or off-label use for sleep. This distinction is important because dependence can be managed safely with structured tapering.
Stopping amitriptyline without medical guidance increases the risk of withdrawal symptoms and symptom rebound. A supervised tapering plan allows the nervous system to adjust gradually and helps distinguish temporary withdrawal effects from relapse, improving safety and long-term outcomes.
Amitriptyline has a relatively long half-life and can remain in the body for several days after the last dose. Detectable effects may persist longer in people taking higher doses or using it long term, which is why gradual tapering is preferred over sudden discontinuation.
Amitriptyline is sometimes prescribed off-label for sleep because it causes sedation, but it is not a sleep medication by design. Long-term use for insomnia may lead to tolerance and dependence. Ongoing review and alternative sleep treatments are often safer and more effective.







