Amitriptyline Withdrawal: Symptoms, Timeline, and Care
Stopping amitriptyline abruptly can trigger withdrawal because the brain loses a source of chemical support too quickly. The nervous system, which has been relying on the medicine’s steady influence, suddenly has to recalibrate.

Key Takeaways
-
Is withdrawal real? Yes. Amitriptyline withdrawal happens because your brain is adjusting to chemical changes. The symptoms are temporary and manageable with proper support.
-
How should I stop safely? A gradual, medically supervised taper is the safest method. It prevents unnecessary discomfort and protects your mental health.
-
What helps recovery? Healthy routines, therapy, stress-reduction tools, social support, and ongoing medical guidance make the transition smoother.
What Amitriptyline Does in the Body?
Amitriptyline is a tricyclic antidepressant (TCA) commonly prescribed for depression, anxiety, chronic pain, migraines, and sleep disturbances. It works by increasing the availability of serotonin and norepinephrine, two key neurotransmitters that help regulate emotional stability, sleep quality, nerve pain, and overall stress response. [1]
Over weeks and months, your brain and body slowly adapt to these enhanced chemical levels. They become your system’s “new normal.” When the medication is reduced or stopped, the nervous system must adjust again—this time in the opposite direction.
Why Withdrawal Happens?
Stopping amitriptyline abruptly can trigger withdrawal because the brain loses a source of chemical support too quickly. The nervous system, which has been relying on the medicine’s steady influence, suddenly has to recalibrate.
This readjustment creates temporary discomfort—what we call withdrawal symptoms. It’s not a sign of harm from the medication; it’s simply the body working to regain balance.
Common reasons this happens include:
-
A sudden drop in serotonin and norepinephrine activity
-
Increased sensitivity of nerve pathways
-
Temporary dysregulation of sleep, mood, or pain signals
These changes are reversible. They typically improve as your body re-stabilizes.
Withdrawal vs. Relapse: How to Tell the Difference?
Understanding the difference helps people avoid unnecessary fear.
Withdrawal
-
Starts quickly — often within 1–4 days of reducing or stopping the dose
-
Symptoms may come and go, rise and fall throughout the day
-
Includes more physical discomforts (nausea, dizziness, sleep changes, flu-like feelings, anxiety spikes)
-
Usually improves within days to weeks
Relapse
-
Returns gradually, often over weeks
-
Symptoms become persistent rather than fluctuating
-
Reflects a return of the original condition (depression, anxiety, or pain)
-
Responds better to long-term treatment adjustments
Knowing this difference often reduces panic and helps families understand what’s happening.
Withdrawal ≠ Addiction
Amitriptyline does not cause addiction.
There are:
-
No cravings
-
No compulsive drug-seeking behavior
-
No psychological reinforcement cycle
Withdrawal simply means the body is adjusting to the absence of a medicine it has grown used to. It is a physiological process, not an addictive one.
This distinction is important because many people feel unnecessary shame or fear when they experience withdrawal symptoms. In reality, it’s a normal and temporary neurological response.
What Are the Common Symptoms of Amitriptyline Withdrawal?
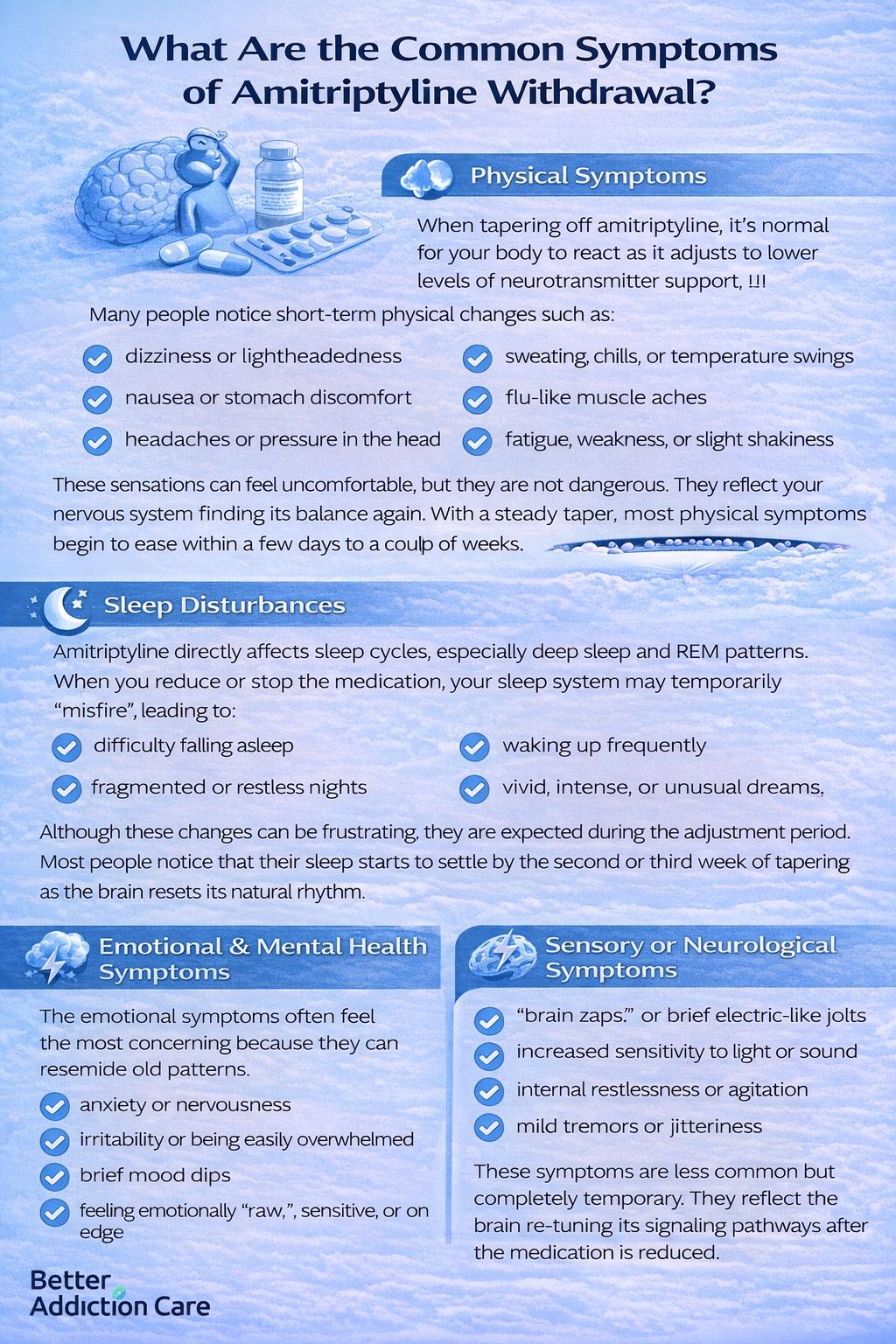
Physical Symptoms
When tapering off amitriptyline, it’s normal for your body to react as it adjusts to lower levels of neurotransmitter support.[1] Many people notice short-term physical changes such as:
-
dizziness or lightheadedness
-
nausea or stomach discomfort
-
headaches or pressure in the head
-
sweating, chills, or temperature swings
-
flu-like muscle aches
-
fatigue, weakness, or slight shakiness
These sensations can feel uncomfortable, but they are not dangerous. They reflect your nervous system finding its balance again. With a steady taper, most physical symptoms begin to ease within a few days to a couple of weeks.
Sleep Disturbances
Amitriptyline directly affects sleep cycles, especially deep sleep and REM patterns. When you reduce or stop the medication, your sleep system may temporarily “misfire,” leading to:
-
difficulty falling asleep
-
waking up frequently
-
fragmented or restless nights
-
vivid, intense, or unusual dreams
Although these changes can be frustrating, they are expected during the adjustment period.
Most people notice that their sleep starts to settle by the second or third week of tapering as the brain resets its natural rhythm.
Emotional & Mental Health Symptoms
The emotional symptoms often feel the most concerning because they can resemble old patterns. It’s common to experience:
-
anxiety or nervousness
-
irritability or being easily overwhelmed
-
brief mood dips
-
feeling emotionally “raw,” sensitive, or on edge
These reactions can mimic a relapse, but in withdrawal they tend to come in waves and improve as the dosage stabilizes. They are signs of chemical recalibration—not signs that you are “slipping back” or losing progress. With reassurance, support, and proper tapering, these emotional shifts gradually settle. [2]
Sensory or Neurological Symptoms
As the nervous system adjusts, some people experience unusual sensory sensations, such as:
-
“brain zaps” or brief electric-like jolts
-
increased sensitivity to light or sound
-
internal restlessness or agitation
-
mild tremors or jitteriness
These symptoms are less common but completely temporary.
They reflect the brain re-tuning its signaling pathways after the medication is reduced. With time and a slow taper, they usually lessen and disappear.
What Is the Typical Amitriptyline Withdrawal Timeline?
Factors That Affect the Timeline
-
how long you’ve been taking amitriptyline
-
your dose
-
taper speed
-
your personal sensitivity
-
co-existing mental health needs
Everyone’s journey is slightly different.
Why Should Amitriptyline Be Tapered Slowly?
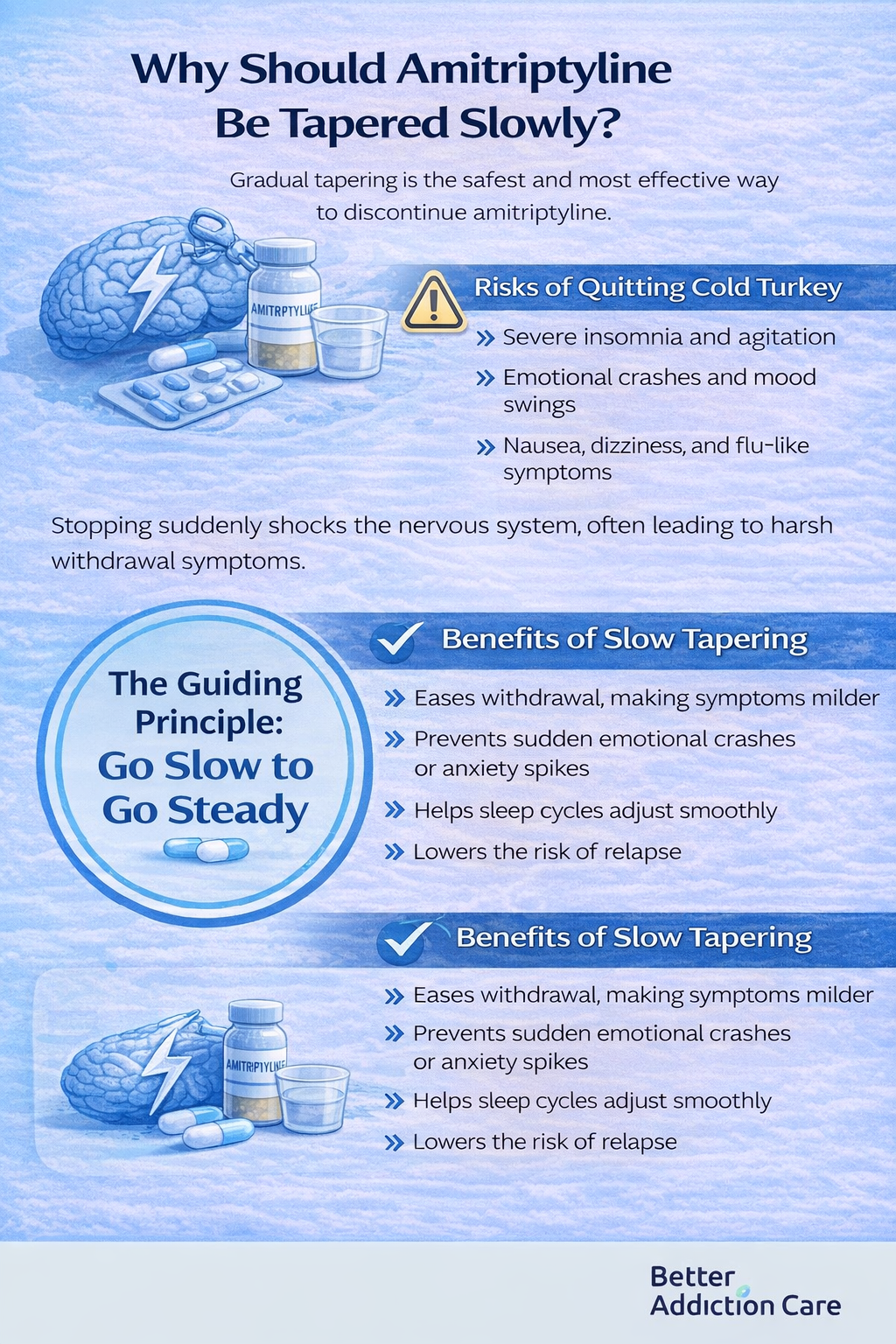
Tapering off amitriptyline slowly is one of the safest and most effective ways to prevent unnecessary discomfort. Because the medication affects serotonin, norepinephrine, sleep rhythms, and nerve sensitivity, your brain needs time to adjust when the dose decreases. [3] A gradual approach protects both physical and emotional well-being.
Risks of Quitting Cold Turkey
Stopping amitriptyline without a taper can shock the nervous system. Because the medication has been supporting serotonin and norepinephrine pathways, removing it suddenly creates an abrupt chemical gap.
The brain tries to compensate quickly, and that rapid readjustment leads to intensified withdrawal.
People who quit cold turkey often report:
-
severe insomnia that makes it difficult to fall asleep or stay asleep
-
emotional crashes where mood drops suddenly or overwhelmingly
-
sharp mood swings, moving from calm to agitated within minutes
-
heightened anxiety or irritability, sometimes out of proportion to the situation
-
a re-emergence of old symptoms like chronic pain, depression, or panic attacks
-
physical discomfort, such as nausea, dizziness, sweating, chills, or body aches
These reactions are not signs of personal weakness—they are physiological responses to a sudden chemical shift. When the brain is forced to rebalance too quickly, symptoms become more intense, unpredictable, and emotionally taxing.
Cold turkey also increases the risk of thinking the medication “needs to be restarted,” even when the issue is purely withdrawal, not relapse.
Benefits of Slow Tapering
A slow taper gives your brain space to adapt gradually. Each small dose reduction teaches the nervous system how to function with slightly less medication, keeping the transition stable and manageable.
A well-planned taper:
-
reduces the severity of withdrawal, making symptoms milder and easier to handle
-
supports emotional steadiness, preventing sudden crashes or anxiety spikes
-
protects sleep, helping your natural sleep rhythm return without disruption
-
lowers the risk of relapse, because symptoms don’t overwhelm you
-
creates a smoother long-term outcome, allowing you to discontinue safely and confidently
Slow tapering is not about being cautious for its own sake—it is about being kind to your brain. It honors the biology of recovery and respects the emotional experience of the person going through it.
The Guiding Principle: Go Slow to Go Steady
This approach is used by clinicians worldwide because it aligns with how the nervous system heals. Going slowly:
-
prevents distressing withdrawal waves
-
allows you to notice early signs of discomfort
-
gives your doctor time to adjust your taper plan
-
empowers you to stay in control of the process
-
strengthens long-term success by avoiding overwhelm
Let your symptoms—not the calendar—set your pace.
Withdrawal is not a race. A personalized, flexible taper—guided by a healthcare professional—helps your body adjust at a pace that feels safe, stable, and sustainable.
What Helps Manage Amitriptyline Withdrawal Symptoms?
Managing withdrawal isn’t something you have to navigate alone. Healthcare providers play a crucial role in keeping the process safe, steady, and emotionally manageable. Their guidance helps reduce discomfort, prevent setbacks, and ensure that any symptoms you experience are part of a normal adjustment—not a warning sign.
1. Monitoring Symptoms and Adjusting the Taper
A key part of withdrawal management is regular check-ins. [4] Your provider tracks how your body responds at each dose reduction, watching for changes such as:
-
dizziness
-
sleep disruption
-
anxiety
-
mood shifts
-
headaches or nausea
If symptoms become too intense, the tapering schedule can be slowed, paused, or slightly adjusted. This flexible approach keeps your nervous system supported and prevents unnecessary distress.
2. Distinguishing Withdrawal from Relapse
Withdrawal and relapse can feel similar, but they follow different timelines. A clinician helps you understand:
-
withdrawal: fast onset, fluctuating, often physical
-
relapse: slower return, persistent, tied to the original condition
Knowing the difference helps reduce fear and prevents people from assuming their condition is “coming back.” This clarity alone can provide enormous relief.
3. Providing Reassurance and Short-Term Support
Your provider may offer temporary treatments to make the process smoother, such as:
-
short-term sleep aids
-
anti-nausea medications
-
anxiety-reducing strategies
-
pain relief for headaches or body aches
These aren’t long-term prescriptions—they’re short-term tools that support comfort while your brain recalibrates. Reassurance and education are just as important; knowing that what you’re feeling is expected makes withdrawal far less overwhelming.
4. Tracking Overall Mental Health
The emotional aspect of withdrawal can be the most confusing. Healthcare providers help by:
-
monitoring mood changes
-
assessing stress levels
-
preventing old symptoms from resurfacing
-
offering coping strategies and therapy support if needed
This holistic approach protects your mental well-being during a period of biological change. With proper monitoring, early warning signs are caught quickly, allowing the taper to stay safe and steady.
Coping Strategies That Help During Withdrawal
1. How Can I Improve My Sleep?
-
Keep a predictable sleep schedule.
-
Reduce screen exposure before bed.
-
Use grounding techniques and slow breathing.
-
Avoid long naps that disrupt nighttime rest.
2. What Should I Eat and Drink?
-
Stay hydrated.
-
Choose balanced meals with proteins, whole grains, and fruits.
-
Avoid excess caffeine and sugary snacks—they worsen symptoms.
3. Should I Exercise?
-
Gentle activity supports mood regulation and sleep.
-
Walking, stretching, and light workouts are ideal.
-
Avoid heavy exercise if you feel dizzy or fatigued.
4. How Can I Reduce Stress and Anxiety?
-
Breathing exercises
-
Journaling
-
Mindfulness or grounding methods
-
Therapy or counseling
Small, steady practices make big differences.
5. How Can I Stay Connected and Supported?
Do not isolate yourself during withdrawal.
Share your plan with trusted loved ones.
Support groups—online or in person—help reduce fear and shame.
6. Does Routine Matter?
Yes. Predictability keeps symptoms stable.
Simple rituals—morning sunlight, regular meals, bedtime routines—anchor the nervous system.
When Should I Seek Medical Help During Withdrawal?
Seek help urgently if you notice:
-
severe depression or suicidal thoughts
-
hallucinations
-
heart-related symptoms (chest pain, palpitations)
-
inability to function in daily life
-
symptoms not improving with taper adjustments
These signs mean you need extra support—not that you've done anything wrong.
What Comes After Withdrawal?
Rebuilding Emotional and Physical Balance
As withdrawal symptoms fade, your body gradually reclaims its natural rhythm. You may notice:
-
Sleep becomes more restorative without artificial adjustment
-
Mood stabilizes and emotional swings are less intense
-
Energy levels improve, making daily tasks easier
This phase is about reconnecting with your body and mind. Simple routines—morning sunlight, gentle exercise, regular meals—support the nervous system as it fully recalibrates.
Recognize that recovery may feel uneven at first; some days will be better than others, and that’s completely normal.
Staying Connected to Professional Support
Even after tapering ends, ongoing guidance is crucial. Healthcare providers can help you:
-
Schedule follow-ups to track mood, sleep, and overall health
-
Adjust long-term medication plans if symptoms of depression, anxiety, or pain persist
-
Provide reassurance and tools to manage stress or minor setbacks
Continuing mental health care—through therapy, counseling, or check-ins—ensures that your recovery remains stable and prevents old symptoms from returning.
Long-Term Habits That Protect Recovery
Recovery isn’t just about stopping medication—it’s about building resilience. Integrating healthy habits into your daily life strengthens emotional and physical well-being:
-
Regular exercise: boosts mood, improves sleep, and reduces stress
-
Nutritious meals: stabilize energy levels and support brain chemistry
-
Consistent sleep patterns: reinforce natural circadian rhythms
-
Stress-reduction tools: mindfulness, breathing exercises, or journaling
-
Family and social support: encourages accountability and emotional reassurance
-
Therapy or emotional support: helps process lingering feelings and maintain coping strategies
These practices make your nervous system more adaptable and reduce the likelihood of future disruptions.
Recovery Is Ongoing
It’s important to remember that finishing withdrawal is not the finish line. Instead, it marks the start of a more grounded, self-aware chapter in life. Emotional growth, physical resilience, and mental clarity continue to develop over months.
Recovery is a journey of small, consistent steps. Every positive habit, healthy interaction, and mindful choice strengthens your long-term well-being. [5]
With patience, support, and realistic expectations, life after withdrawal can feel more balanced, energized, and emotionally secure than before starting medication.
Conclusion
Amitriptyline withdrawal is uncomfortable, but it is temporary and manageable.
With slow tapering, compassionate support, and healthy daily habits, your symptoms will improve and your body will regain balance. This process requires patience—not perfection. Stay connected, stay steady, and never attempt to stop abruptly.
You’re not alone. Healing is possible, and every step you take is progress.
FAQs
It’s strongly discouraged. Cold turkey increases the risk of intense withdrawal and emotional instability, making the process unnecessarily difficult.
Most people improve within 3–4 weeks, though some need longer depending on dose and duration. Recovery speed varies by individual.
Not necessarily. Withdrawal can mimic old symptoms, but they often fade with time and proper support, rather than indicating a relapse.
Hydration, sleep hygiene, gentle movement, grounding exercises, and stable routines all support the nervous system during withdrawal.
By listening without judgment, helping with routines, and staying present during tougher days, they provide emotional and practical stability.
Contact a healthcare provider immediately. Taper adjustments, short-term medications, or supportive interventions can relieve severe discomfort safely.







