Anabolic Steroid Addiction and Abuse Signs, Risks, and Treatment
For many people, anabolic steroids begin as a way to “get ahead”—a little extra muscle, faster recovery from workouts, pressure to look more defined, or to keep up with peers who seem to be transforming their bodies quickly. But slowly, something shifts.
A person who once felt proud of their discipline now feels terrified of losing the progress they've made. People around you also start noticing mood swings, secrecy, irritability, and an overwhelming focus on the gym.
Your loved one may insist they’re “fine,” that they’re “just cycling,” and that they can stop at any time. Yet when they try, the depression, fatigue, and cravings hit so hard they run straight back to the drugs.

Key Takeaways
-
Steroid addiction develops from a combination of hormonal suppression, reward pathway reinforcement, body-image concerns, and social pressures—making dependence powerful and multilayered.
-
Withdrawal can be physically and emotionally severe, including depression, fatigue, hormonal instability, and suicidal thoughts—requiring medical oversight and structured support to prevent relapse.
-
Recovery is possible through medical hormone restoration, psychotherapy, family involvement, and structured treatment, helping individuals rebuild identity, confidence, and emotional balance without steroids.
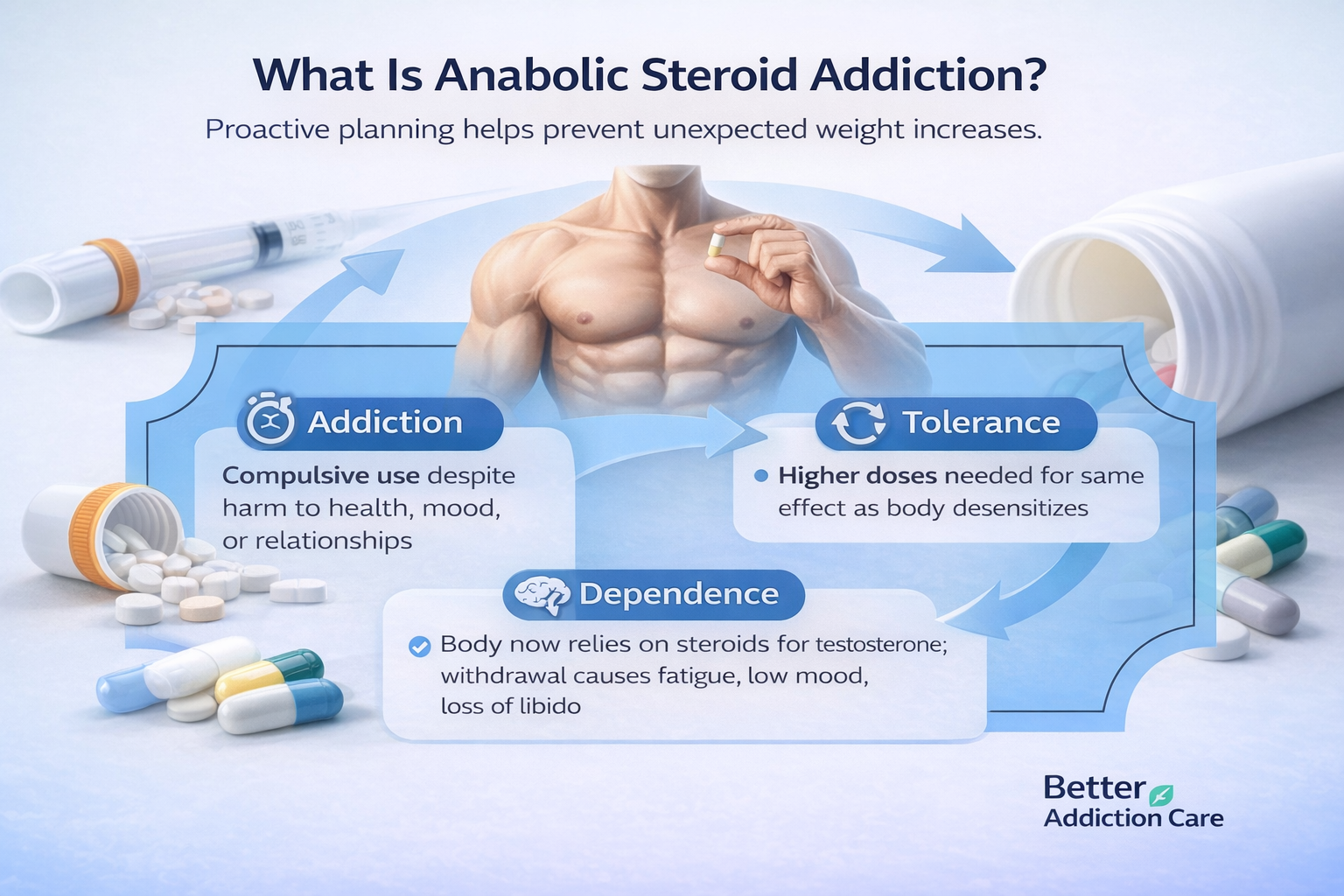
What Is Anabolic Steroid Addiction?
Anabolic-androgenic steroids (AAS) are synthetic versions of testosterone—the primary male sex hormone responsible for muscle growth, energy, libido, and mood regulation. When taken in doses far beyond medical levels, they artificially elevate testosterone and trigger rapid muscle gain and performance changes.
Here’s where the addiction pathway begins:
Tolerance
Over time, the body becomes desensitized. Someone who once took a “mild” dose now needs significantly higher amounts for the same effect.
Dependence
Steroid use suppresses the hypothalamic-pituitary-gonadal (HPG) axis—the hormonal system that regulates testosterone. When steroids stop, the body struggles to produce its own hormones. This leads to withdrawal symptoms: severe fatigue, low mood, anxiety, insomnia, and loss of libido.
Addiction
Compulsive use continues despite damage to health, relationships, employment, and emotional well-being. Many individuals with steroid addiction report feeling “small,” depressed, or worthless when they’re off-cycle—a distortion of body image known as muscle dysmorphia (a psychiatric condition characterized by the obsessive belief that one is too small, even when objectively muscular).
Families often don’t recognize this as addiction because it doesn’t resemble substance “abuse” in the traditional sense. But the pattern—compulsion, reinforcement, withdrawal, and continued use despite harm—matches the clinical criteria.
Why Steroid Addiction Feels Different (and More Confusing) to Families?
Steroid addiction is often hidden behind the appearance of discipline. A person may still attend work, eat clean, follow strict routines, and spend hours training. But underneath, their identity becomes fragile—entirely dependent on size, strength, and the validation of others.
Key reasons families feel confused:
-
They don’t see intoxication. Steroids don’t create a “high.” Instead, they subtly shift mood, confidence, aggression, and judgment, making changes less obvious than with other drugs.
-
The culture normalizes it. Fitness communities, gyms, and online influencers often encourage or downplay steroid use, masking risks.
-
Emotional and behavioral changes seem unrelated. Irritability, rage, secrecy, or obsessive focus on diet and physique can look like personality changes rather than drug effects.
-
Withdrawals resemble a mental health crisis. Post-cycle low testosterone may trigger severe depression, anxiety, or even suicidal thoughts—often misinterpreted as unrelated emotional struggles.
The truth? Steroid addiction alters both body and identity, creating confusion for loved ones—but with proper medical care, therapy, and family support, recovery is achievable.
Signs & Symptoms of Steroid Addiction
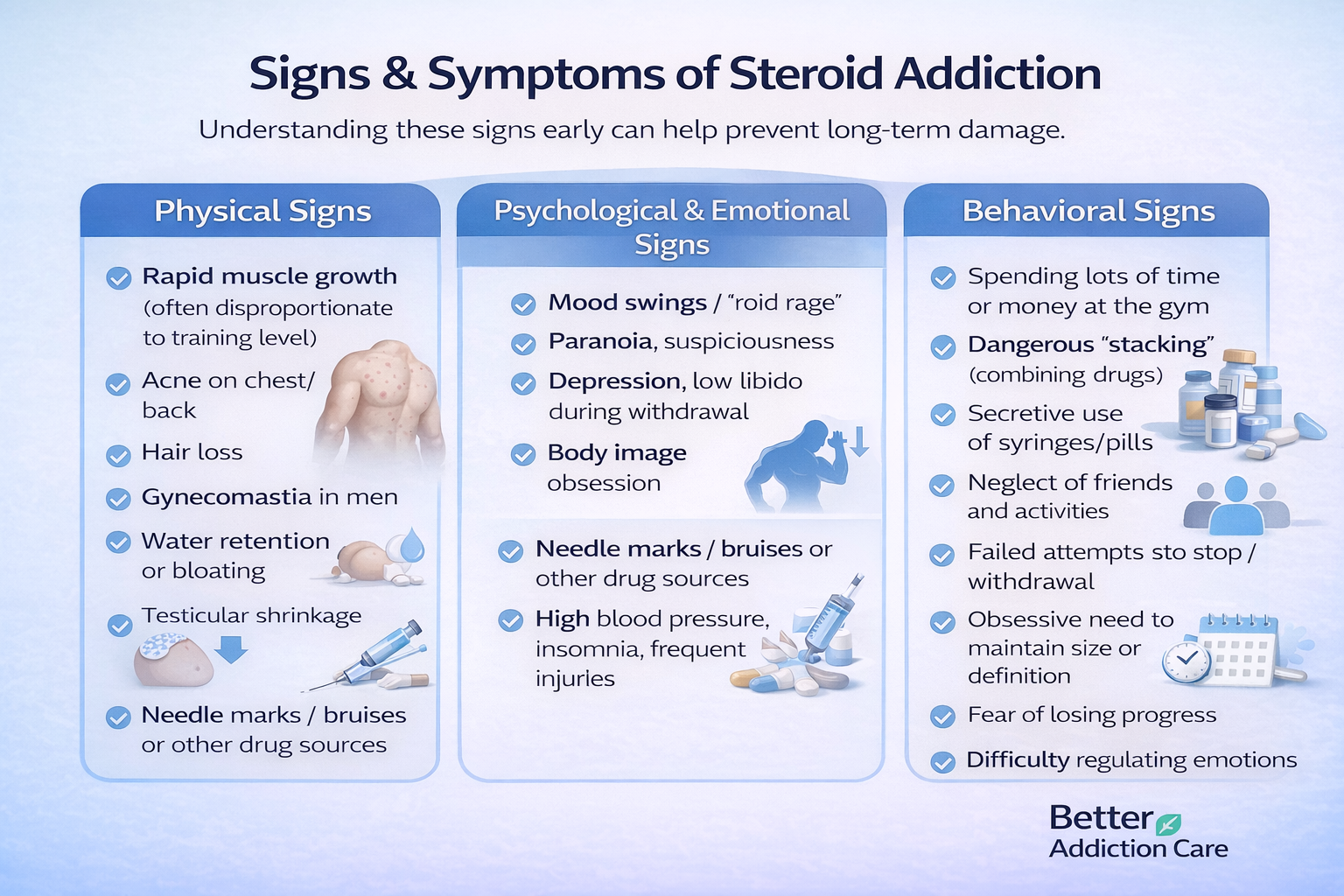
Understanding the signs early helps families intervene before long-term damage occurs.
Physical Signs
These symptoms stem from hormonal imbalance, testosterone suppression, and direct organ strain:
-
Rapid muscle growth (often disproportionate to training level)
-
Acne on chest/back
-
Hair loss
-
Gynecomastia (breast tissue growth in men due to estrogen conversion)
-
Water retention or bloating
-
High blood pressure
-
Testicular shrinkage
-
Low sperm count or infertility
-
Unusually frequent injuries due to rapid muscle–tendon imbalance
-
Injection marks on thighs, shoulders, or glutes
-
Insomnia or disrupted sleep
Psychological & Emotional Signs
These mental and emotional changes are heavily tied to steroid-related hormone fluctuations.
-
Mood swings—rapid shifts between irritability, aggression, and euphoria
-
Increased anxiety or paranoia
-
Aggressive outbursts (“roid rage”)
-
Depression, especially during the “off-cycle.”
-
Body dissatisfaction, even when extremely muscular
-
Obsessive need to maintain size or definition
-
Fear of losing progress
-
Difficulty regulating emotions
-
Cravings to resume use after stopping
Researchers have found that AAS use is strongly associated with increased aggression and mood instability due to the way high-dose testosterone interacts with the prefrontal cortex—the brain area responsible for impulse control and emotional regulation[1].
Behavioral Signs
Behavioral patterns are often the clearest indicators:
-
Strict “cycle” schedules (on/off periods)
-
Using multiple steroids at once (“stacking”)
-
Spending excessive money on drugs, syringes, or supplements
-
Hiding vials, needles, or pills
-
Lying about injections or prescriptions
-
Excessive time spent at the gym (2–3 hours/day or more)
-
Avoiding social events to prevent missing workouts or meals
-
Extreme diet rigidity; panic if routine changes
-
Repeated failed attempts to stop
-
Continuing despite health scares
One of the most painful patterns for families is emotional distancing—your loved one may shut down, avoid conversations, or become defensive when steroids are mentioned.
How Common Is Steroid Addiction?
Anabolic steroid misuse is far more widespread than most families realize. National survey data indicate that an estimated 1 million individuals in the United States have used anabolic steroids, particularly young men seeking physical enhancement[2].
Use is especially common among:
-
Gym-goers and bodybuilders
-
Competitive athletes
-
Individuals with muscle dysmorphia
-
First responders, military personnel, and physically demanding occupations
-
Teens and young adults influenced by social media fitness culture
While not everyone who experiments becomes addicted, research shows that about 30% of long-term AAS users develop dependence, with withdrawal being a major driver of continued use [3].
Families often underestimate risk because steroid use is framed as “fitness,” “self-improvement,” or “discipline.” In reality, the emotional and hormonal consequences can be severe.
Why Steroid Addiction Happens? Causes and Progression
Steroid addiction does not start with a desire to “get high.” It begins with the desire to feel strong, look better, or perform at a higher level.
That longing for improvement may seem harmless, even admirable, but the biological, psychological, and social reinforcements surrounding anabolic steroids make the pathway to addiction far more powerful than many expect.
1. Neurobiology: How Steroids Change the Body and Brain
Anabolic steroids fundamentally alter how the body regulates hormones, motivation, and emotional stability. These internal changes create a physiological environment where quitting becomes extremely difficult.
Hormonal Suppression: The HPG Axis Shutdown
When someone takes anabolic steroids, the brain senses extremely high testosterone levels.
In response, the hypothalamic–pituitary–gonadal (HPG) axis drastically reduces or shuts down natural testosterone production. This “shutdown” is what causes:
-
Testicular shrinkage
-
Loss of sperm count
-
Drop in libido
-
Depression and fatigue when off-cycle
Because the body no longer produces its own hormones, users often feel incapable of functioning normally without steroids. This hormonal imbalance becomes the driving force behind dependence.
Reward Pathway Reinforcement
High-dose testosterone increases dopamine activity in the mesolimbic reward system, reinforcing behaviors that feel rewarding or validating. During steroid cycles, people often describe:
-
Elevated motivation
-
Increased confidence
-
Stronger sense of power or capability
-
Faster recovery that makes training more enjoyable
This shift in reward circuitry creates powerful psychological reinforcement, making the person want to repeat the experience.
Impaired Impulse Control and Aggression
Elevated testosterone affects the prefrontal cortex—the brain region responsible for decision-making, empathy, and emotional regulation. This is why families witness:
-
Sudden emotional outbursts
-
Impulsive behavior
-
Aggression
-
Lowered frustration tolerance
A US-based study found long-term AAS users often show heightened aggression and significant mood instability driven by these neurobiological changes[1].
This isn’t “bad behavior”—it’s the outcome of a dominating hormonal influence on brain circuits.
2. Psychological Triggers: Why the Mind Gravitates Toward Steroid Use
Muscle Dysmorphia (The “Never Big Enough” Trap)
Muscle dysmorphia is a subtype of body dysmorphic disorder where individuals believe they look too small or weak, even when objectively muscular. Steroids can temporarily silence this internal criticism—making them psychologically addictive.
Identity and Self-Worth Become Physique-Dependent
For many, the gym becomes a sanctuary—a place where structure, control, and achievement feel attainable. Steroids amplify that sense of mastery. When off-cycle, losing muscle or strength can feel like losing identity, causing intense emotional distress.
Relief From Emotional or Social Pain
Steroids may begin as a solution to:
-
Low confidence
-
Past bullying
-
Trauma
-
Insecurity around masculinity
-
Pressure to perform in competitive environments
Over time, steroids become a coping strategy—an emotional crutch to avoid vulnerability.
3. Environmental and Social Drivers
Gym Culture and Peer Influence
In many fitness communities, steroid use is normalized and even celebrated. People may hear:
-
“Everyone’s doing it.”
-
“You won’t get to the next level without gear.”
-
“One cycle won’t hurt.”
This social reinforcement lowers perceived risk and increases willingness to experiment.
Online Access and Influencer Pressure
The internet has made steroids extremely accessible. Underground labs ship steroids internationally with minimal regulation. Influencers normalize massive physiques, creating unrealistic expectations for young men who don't understand that many of these physiques are chemically assisted.
Silence, Stigma, and Lack of Education
Because steroid addiction is not widely discussed, many users don’t know the risks until withdrawal symptoms strike. Shame then prevents them from asking for help.
4. The Cycle-to-Dependence Pathway: How It Actually Progresses
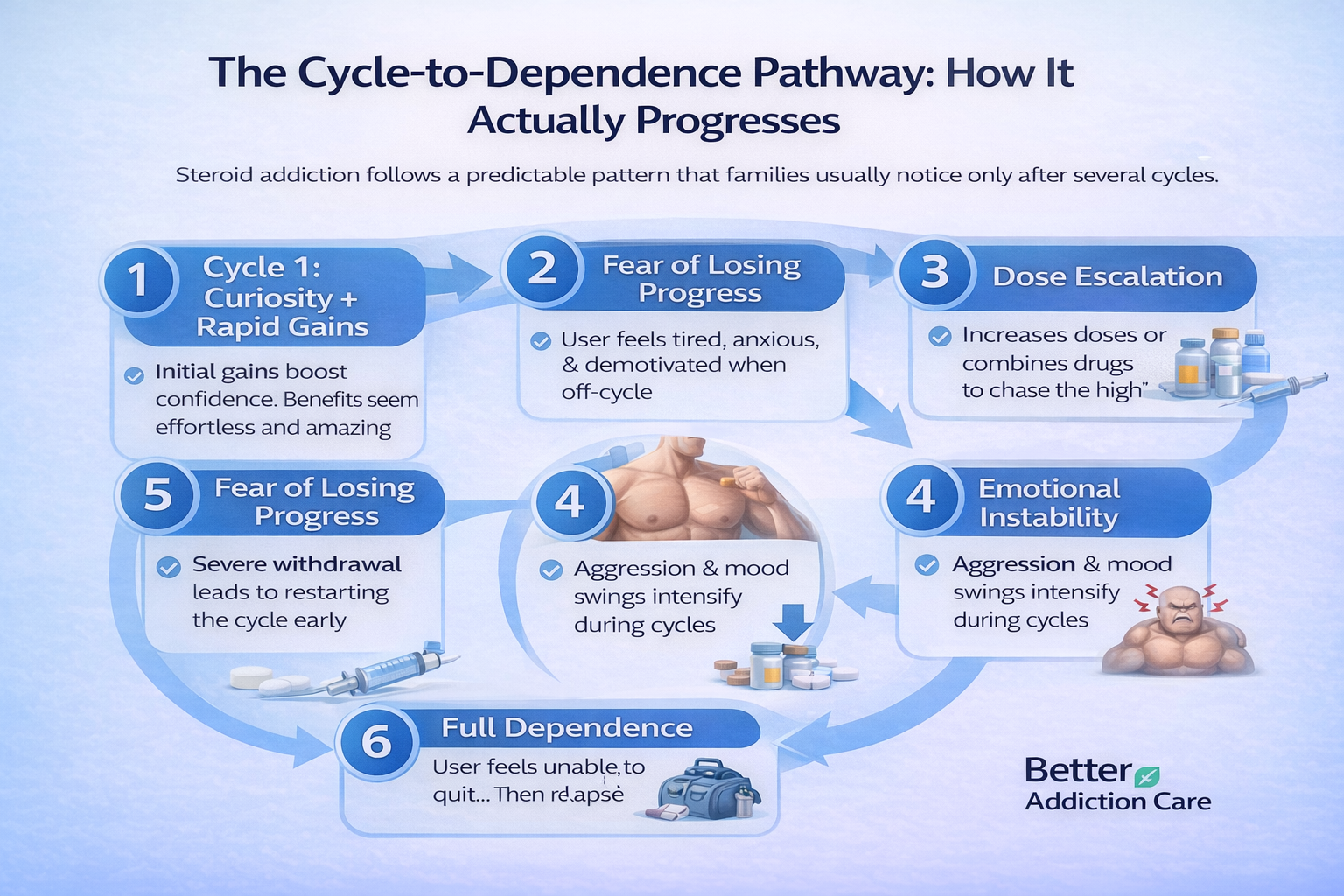
Steroid addiction follows a predictable pattern that families usually notice only after several cycles.
Cycle 1: Curiosity + Rapid Gains
The journey often begins with fascination—friends, social media, or athletic pressure can spark curiosity. The person experiences rapid improvements in strength, muscle size, and recovery time—results far beyond what natural training alone achieves. These early gains reinforce use and create a sense of invincibility.
Cycle 2: Fear of Losing Progress
When the cycle ends and natural testosterone drops, the individual may feel fatigued, demotivated, anxious, or depressed. Physique changes can reverse, triggering body-image concerns. Families may notice unusual withdrawal from social activities or sudden irritability.
Cycle 3: Dose Escalation
To counter declining results, the person often increases doses or combines multiple compounds—a practice called “stacking.” This escalation may temporarily restore performance but also magnifies health risks, including cardiovascular strain, liver damage, and hormonal imbalances.
Cycle 4: Emotional Instability
Persistent hormonal fluctuations contribute to mood swings, aggression, and conflict with loved ones. Anxiety, depression, and impulsive behaviors intensify. Families often report feeling as if they are “walking on eggshells” around the user.
Cycle 5: Attempts to Quit… Then Relapse
Stopping steroids triggers withdrawal symptoms such as fatigue, insomnia, joint pain, and emotional lows. The discomfort can be so severe that restarting the cycle seems like the only relief. Each relapse reinforces the psychological and physical dependence, making it harder to quit next time.
Cycle 6: Full Dependence
At this stage, steroid use is no longer about enhancing appearance or performance. It becomes a necessity to maintain normal functioning and avoid collapse—physically, emotionally, and socially. The person may isolate, hide usage, and exhibit compulsive patterns that severely impact health, relationships, and daily life.
Short-Term & Long-Term Side Effects
Short-Term Side Effects (During Active Cycles)
Steroids elevate testosterone far above normal biological limits, resulting in:
-
Intense acne or oily skin due to increased sebaceous gland activity
-
Water retention leading to bloating
-
Insomnia from overstimulation
-
Increased heart rate and blood pressure
-
Headaches
-
Irritability and agitation
-
Changes in libido (either increased or decreased)
Many users misinterpret these as just “part of the cycle,” not realizing they indicate significant hormonal disruption.
Long-Term Side Effects (Months to Years)
Cardiovascular Risks
Steroids can reduce HDL (“good”) cholesterol and increase LDL (“bad”) cholesterol, accelerating plaque formation in arteries. This dramatically increases the long-term risk of:
-
Heart attack
-
Stroke
-
Hypertension
Liver and Kidney Stress
Oral steroids (especially 17-alpha-alkylated compounds) can cause liver inflammation and enzyme elevation.
Endocrine Damage
Chronic suppression of the HPG axis can result in:
-
Hypogonadism (chronically low testosterone)
-
Infertility
-
Erectile dysfunction
-
Hormonal imbalance
Some individuals require lifelong medical hormone therapy after prolonged steroid use.
Psychiatric Instability
Steroid-induced hormone shifts can contribute to:
-
Major depressive episodes
-
Emotional volatility
-
Paranoia
Social and Lifestyle Impacts
-
Strained relationships
-
Financial stress due to drug and supplement costs
-
Missed life events due to rigid routines
-
Decline in academic or work performance
-
Social isolation
Families often describe their loved one as “living in a bubble” centered solely around physique and training.
What Steroid Withdrawal Really Feels Like?
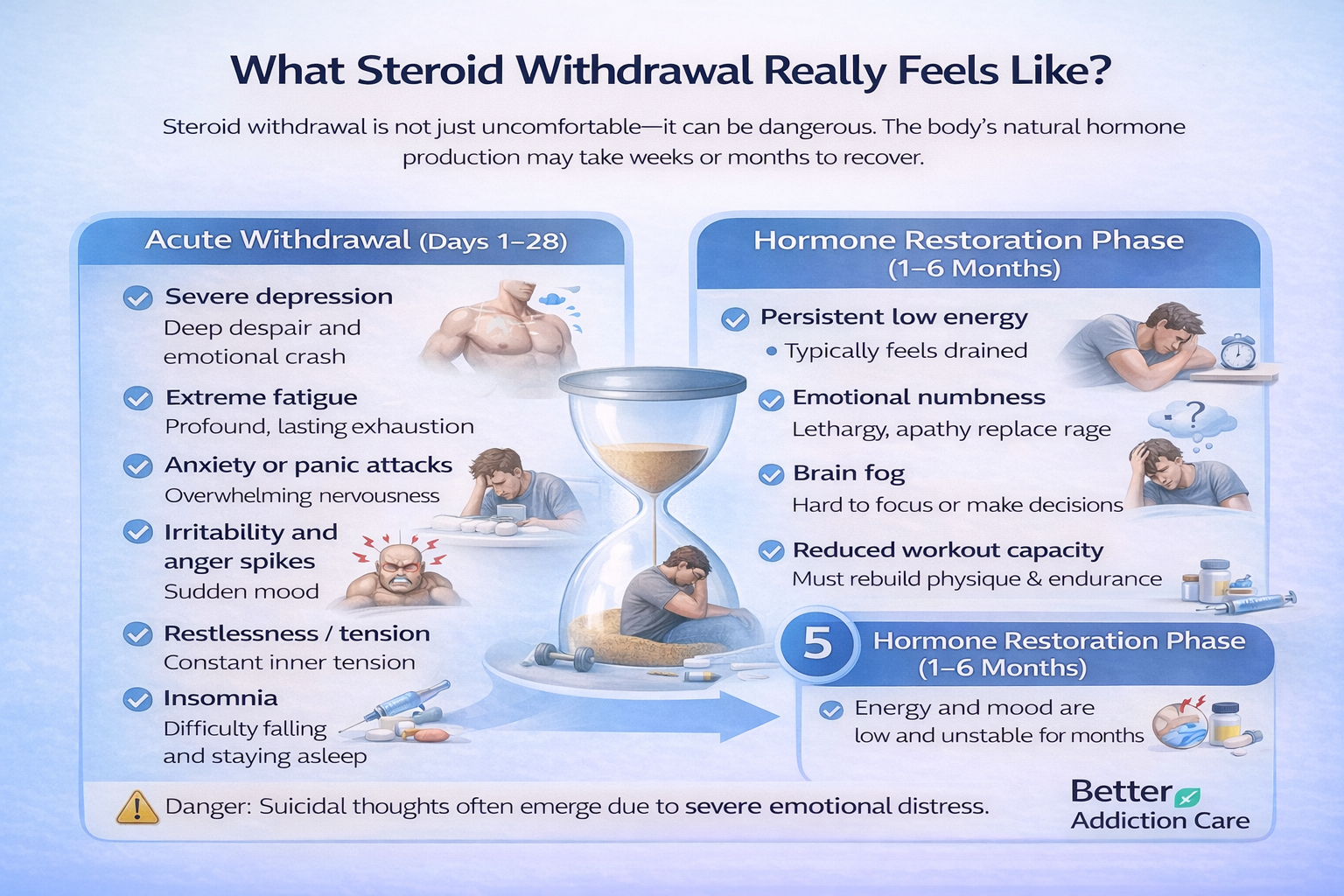
Steroid withdrawal is not just uncomfortable—it can be dangerous. The body’s natural hormone production may take weeks or months to recover.
Acute Withdrawal (Days 1–28)
Symptoms in this stage are intense and often overwhelming:
-
Severe depression — a deep emotional crash triggered by sudden hormonal collapse
-
Extreme fatigue — even simple tasks feel exhausting or impossible
-
Anxiety or panic attacks — the nervous system becomes hypersensitive
-
Irritability and anger spikes — small frustrations feel explosive
-
Restlessness and inability to relax — constant inner tension
-
Insomnia despite exhaustion — sleep feels broken or unreachable
-
Loss of libido and drive — both physical and emotional motivation drop sharply
-
Strong cravings to use again — driven by the desire to stop emotional and physical discomfort
This is the period where suicidal thoughts are most likely due to drastic mood instability.
Hormone Restoration Phase (1–6 Months)
As the body slowly tries to restart natural testosterone, people may experience:
-
Persistent low energy — feeling “drained” even with rest
-
Emotional flatness or numbness — a sense of not caring about anything
-
Brain fog — difficulty focusing, planning, or making decisions
-
Cravings to feel normal — not for muscle gains, but to feel stable again
-
Reduced performance and physique changes — strength, muscle fullness, and workout capacity decline
Without proper medical and emotional support, this long, uncomfortable stretch often leads to relapse because daily functioning feels nearly impossible.
Treatment Options for Steroid Addiction
Recovery requires a holistic, evidence-based plan that treats the biological hormone disruption, the psychological drivers, and the lifestyle patterns that keep your loved one trapped in the steroid cycle.
1. Medical Evaluation & Hormonal Assessment
A medical provider begins with a full hormonal and physical assessment to understand the degree of suppression and organ stress, helping create a safe, individualized treatment plan.
They will typically measure:
-
Testosterone levels – to determine how severely the HPG axis is suppressed.
-
LH/FSH (pituitary hormones) – low levels signal disrupted hormone signaling from the brain.
-
Liver enzymes – especially important for oral steroids that strain the liver.
-
Kidney function – prolonged use can impact filtration and hydration balance.
-
Blood lipids – high LDL and low HDL increase cardiovascular risks.
-
Blood pressure – steroids commonly elevate it and require monitoring.
From there, treatment may include:
Hormone Restoration Therapy
Short-term medications may be used to stimulate natural testosterone production, reduce withdrawal symptoms, and support endocrine recovery while the body stabilizes.
Medication for Depression/Anxiety
Some individuals develop severe mood crashes during withdrawal; temporary antidepressants or anti-anxiety medications can reduce suffering and support emotional safety.
Nutritional and Lifestyle Guidance
A structured plan for sleep, diet, hydration, and training helps rebuild energy, stabilize mood, and support the body’s natural hormone restoration.
2. Withdrawal Management (Medical Detox)
Steroid detox should always happen under medical supervision because hormonal crashes can trigger serious emotional and physical symptoms that are unsafe to manage alone.
Medical detox is especially important if:
-
Depression is intense and affecting daily functioning.
-
There is suicidal risk during hormonal collapse.
-
Multiple substances are involved, such as stimulants or opioids.
-
Aggression or mood instability is severe, putting the person or others at risk.
Medical detox provides safety, monitoring, and stabilization, helping your loved one navigate the hardest early weeks without relapsing simply to escape withdrawal.
3. Psychotherapy and Behavioral Support
Therapy addresses the emotional and identity-based components of steroid addiction—areas that medical treatment alone cannot fix.
Cognitive Behavioral Therapy (CBT)
Helps individuals challenge distorted beliefs about size, strength, and self-worth while developing healthier, more flexible patterns of thinking.
Motivational Interviewing (MI)
Supports individuals who feel conflicted, ambivalent, or defensive about change, helping them build internal motivation step by step.
Body Image–Focused Therapy
Essential for those with muscle dysmorphia, offering tools to rebuild confidence and identity without relying on steroids.
Family Therapy
Improves communication, reduces blame, and strengthens the family’s ability to support recovery without enabling harmful patterns.
4. Levels of Care
Treatment intensity should match the severity of symptoms, mental health needs, and withdrawal risks.
Inpatient/Residential Treatment
Provides 24/7 support for individuals with severe withdrawal, co-occurring disorders, or unsafe home environments.
Intensive Outpatient Programs (IOP)
Offer several weekly therapy sessions and medical monitoring while the person continues living at home.
Standard Outpatient Treatment
Best for those with stable functioning who still need ongoing therapy, psychiatric support, and medical follow-up.
5. Peer Support & Recovery Capital
Support groups and community-based recovery networks help reduce shame, rebuild connection, and create accountability—especially valuable for people who feel isolated in fitness-focused or competitive environments.
6. Adjunct Supports
Daily habits play a large role in mood stability, hormone recovery, and the prevention of relapse.
Helpful adjunct supports include:
-
A balanced, nutrient-dense diet to support energy, mood, and metabolic health.
-
Moderate strength training that avoids the overtraining cycles associated with steroid use.
-
Consistent sleep hygiene to stabilize hormones and emotional regulation.
-
Stress management tools, such as mindfulness or breathing practices, to reduce triggers and improve resilience.
Recovery from steroid addiction isn’t only about stopping the drugs—it is about rebuilding identity, restoring emotional balance, and helping the body return to its natural rhythm with structured support and compassion.
When This Becomes an Emergency?
Steroid withdrawal and long-term high-dose use can trigger sudden medical and psychiatric crises. Families should trust their instincts—if something feels dangerously “off,” it is safer to act immediately rather than wait and see.
Emergency care is critical when symptoms suggest hormonal collapse, cardiac strain, or severe mood instability that could put your loved one or others at risk.
Seek immediate emergency help if your loved one shows:
-
Suicidal thinking or self-harm behaviors – a known risk during sharp testosterone drops.
-
Severe or worsening depression – especially if they appear hopeless, withdrawn, or unable to function.
-
Chest pain, shortness of breath, or heart palpitations – steroids significantly strain the cardiovascular system and can trigger life-threatening events.
-
Signs of liver or kidney failure, such as yellowing skin, dark urine, abdominal swelling, or sudden vomiting.
-
Violent behavior, extreme agitation, or uncontrollable rage – hormonal instability can impair judgment and increase impulsivity.
-
Confusion, dizziness, or fainting – possible signs of severe blood pressure changes.
In these moments, calling emergency services can prevent fatal complications and ensure your loved one receives rapid, appropriate medical stabilization.
Conclusion:
Steroid addiction is often hidden behind discipline and performance.
But beneath that exterior is a person in pain—someone who once wanted to feel stronger and now feels trapped by cycles they can’t escape alone. Recovery is absolutely possible with the right combination of medical support, therapy, family involvement, and time.
Healing takes patience, understanding, and evidence-based interventions, and setbacks are a normal part of the process. The very fact that you are reading this and seeking knowledge is a sign of courage and the first step toward reclaiming control. Support, treatment, and time can restore both health and hope.
FAQs
Yes. Even planned cycles or “moderate” doses can suppress natural testosterone, leading to hormonal withdrawal and emotional crashes when the cycle ends. This withdrawal-driven pattern is one of the main reasons people develop dependence, even if they started with disciplined or “controlled” use.
Cardiovascular strain is the most dangerous risk—high-dose steroids can raise blood pressure, worsen cholesterol levels, and increase the likelihood of a heart attack or stroke. Psychiatric instability, liver damage, infertility, and severe mood crashes during withdrawal also pose significant long-term dangers.
Relapse is common because withdrawal causes profound fatigue, depression, and loss of motivation. Relapse doesn’t mean failure; it signals that medical and psychological support may need adjustment. When hormone stabilization and therapy are combined, relapse risk decreases, and recovery becomes more sustainable.
No. Stopping abruptly without medical supervision can trigger severe depression, suicidal thoughts, and cardiovascular instability. A supervised withdrawal plan and hormone restoration support make detox significantly safer and more effective.
Stay calm, nonjudgmental, and focused on understanding the hormonal and emotional factors involved. Encourage medical evaluation, join therapy sessions if recommended, and help your loved one maintain structure—sleep, meals, and follow-up appointments. Support is most effective when it is consistent and compassionate.
Steroid withdrawal is usually not physically life-threatening, but the psychological risks can be serious. The sharp drop in testosterone increases the likelihood of severe depression, hopelessness, and suicidal thinking, which is why medical supervision and emotional monitoring are essential for safety.
Resources
Related Articles
Treatment Centers in Virginia









