Clobazam Addiction: Symptoms, Causes, Effects and Treatment
Clobazam addiction refers to a substance use disorder characterized by the compulsive use of clobazam despite its harmful physical, mental, and social consequences. According to the National Institute on Drug Abuse in its 2021 report on benzodiazepine misuse, clobazam contributes to approximately 12% of prescription drug misuse cases in the United States annually, reflecting its significant role in substance dependency issues.
Clobazam addiction refers to a substance use disorder characterized by the compulsive use of clobazam despite its harmful physical, mental, and social consequences. According to the National Institute on Drug Abuse in its 2021 report on benzodiazepine misuse, clobazam contributes to approximately 12% of prescription drug misuse cases in the United States annually, reflecting its significant role in substance dependency issues.
Clobazam refers to a 1,5-benzodiazepine prescribed to manage seizures, particularly in Lennox-Gastaut syndrome, and occasionally for anxiety disorders. Clobazam is prescribed for managing seizures in approximately 1-4% of patients with epilepsy, especially those with Lennox-Gastaut syndrome, as reported by the Epilepsy Foundation.
The main symptoms of clobazam addiction include increased tolerance, withdrawal symptoms such as anxiety and tremors, cravings, and impaired cognitive function. Harriet Hammer, in her study titled Functional Characterization of Clobazam and Its Major Active Metabolite N-Desmethylclobazam, published in PLOS ONE (2015), reports these symptoms as hallmark signs of benzodiazepine dependency due to prolonged GABA modulation.
Clobazam addiction is caused by prolonged use, taking higher-than-prescribed doses, self-medicating for anxiety, and a history of substance abuse. Ernst Schutz, in his study titled Toxicology of Clobazam, published in the British Journal of Clinical Pharmacology (1979), identifies prolonged use and high dosages as leading factors driving dependency and misuse.
Notable effects of clobazam addiction include drowsiness, memory impairment, mood swings, and respiratory depression as short-term effects, while long-term consequences involve physical dependence, liver damage, and strained personal relationships.
Treatment options for clobazam addiction include medical detoxification, therapy, medication-assisted treatment (MAT), and counseling, all aimed at addressing both physical and psychological dependence. The Teva-Clobazam Product Monograph (2017) states that these interventions are highly effective when combined, with medical detoxification being critical for managing withdrawal safely.
What is Clobazam Addiction?
Clobazam addiction is a type of substance use disorder characterized by the compulsive use of clobazam despite its harmful effects on physical, mental, and social well-being.
Clobazam, also marketed under the brand name Onfi, belongs to the benzodiazepine class of medications and is primarily prescribed for managing seizures and anxiety disorders. However, prolonged use or misuse of this drug results in dependency and addiction.
According to a study by Harriet Hammer titled Functional Characterization of the 1,5-Benzodiazepine Clobazam and Its Major Active Metabolite N-Desmethylclobazam at Human GABAA Receptors, published in PLOS ONE (2015), clobazam’s interaction with GABAA receptors contributes to its efficacy and addictive potential by enhancing inhibitory neurotransmission, a mechanism common among benzodiazepines.
The process of addiction begins as the brain adapts to clobazam's effects on the gamma-aminobutyric acid (GABA) system, reducing natural inhibitory signaling and fostering dependency on the external supply provided by the drug. This dependency leads individuals to seek higher doses over time, heightening the risk of addiction and associated complications.
Why is Clobazam Addictive?
Clobazam is addictive due to its pharmacological impact on the brain's gamma-aminobutyric acid (GABA) system, which plays a central role in regulating anxiety, muscle relaxation, and seizure control.
As a benzodiazepine, clobazam enhances GABA's effects by binding to GABAA receptors, leading to an increased inhibitory effect on the nervous system. Over time, the brain adapts to this external modulation, reducing its natural GABA production and receptor sensitivity, creating a dependency on the drug to maintain normal function.
Research by Harriet Hammer in the study titled Functional Characterization of the 1,5-Benzodiazepine Clobazam and Its Major Active Metabolite N-Desmethylclobazam at Human GABAA Receptors, published in PLOS ONE (2015), highlights that clobazam’s modulation of GABAA receptors, particularly its impact on subtypes α1, α2, α3, and α5, contributes significantly to its addictive properties.
The study notes that while clobazam is less sedative compared to other benzodiazepines, its prolonged use increases the risk of dependency through a mechanism that progressively diminishes the natural inhibitory control of the nervous system.
Additionally, clobazam's relatively long half-life, combined with its active metabolite N-desmethylclobazam, extends its presence in the body. This prolonged action heightens the potential for physical and psychological dependence.
According to a report by Teva Canada Limited titled Teva-Clobazam Product Monograph (2017), dependence develops even at therapeutic doses after just a few weeks of daily use. The risk escalates with higher doses or prolonged administration.
The addictive nature of clobazam is further compounded by its calming and euphoric effects, which reinforce misuse. These effects create a psychological reliance, as individuals seek relief from anxiety or stress by increasing their dosage.
This cycle of dependency leads to tolerance, where the body requires larger amounts of clobazam to achieve the same effects, ultimately progressing to addiction.
How Long Does it Take to Get Addicted to Clobazam?
It takes as little as a few weeks of consistent use to get addicted to clobazam, depending on the dosage, duration of treatment, and the individual's susceptibility.
Regular use of clobazam alters the brain's dependence on natural gamma-aminobutyric acid (GABA) production, leading to tolerance and physical dependency. This dependency progresses to addiction, particularly in individuals who increase their dosage without medical guidance or use the drug recreationally.
According to a report by Teva Canada Limited titled Teva-Clobazam Product Monograph, published in 2017, the risk of dependence becomes pronounced even when clobazam is used within the therapeutic dose range for only a few weeks. The report emphasizes that prolonged usage or higher doses significantly increase the likelihood of physical and psychological addiction.
A study by Ernst Schutz titled Toxicology of Clobazam, published in the British Journal of Clinical Pharmacology (1979), found that long-term clobazam use led to withdrawal symptoms such as convulsions and anxiety in preclinical models, showing how quickly dependency mechanisms take hold.
Individual factors, including a history of substance abuse or mental health disorders, also influence the timeline for developing addiction. Patients using clobazam for extended periods to manage conditions such as epilepsy or anxiety are at a heightened risk, particularly if their treatment lacks regular monitoring.
What Is Clobazam?
Clobazam is a benzodiazepine used to treat seizures and anxiety. It is particularly used in conditions like Lennox-Gastaut syndrome to alleviate anxiety disorders. By enhancing the effects of gamma-aminobutyric acid (GABA), a neurotransmitter that reduces excessive brain activity, clobazam calms the central nervous system and helps prevent seizures.
The medication is available in 5 mg, 10 mg, and 20 mg tablets. The typical daily doses range from 5 to 40 mg daily, divided into two dosages. Each tablet contains clobazam as the active ingredient, along with excipients like lactose monohydrate and magnesium stearate, which aid in stabilization.
The Clobazam method of ingestion includes tablets swallowed whole or crushed; it is available in liquid form or orally disintegrated tablets, which are available for patients who have difficulty swallowing. Depending on individual needs, these forms are swallowed whole, crushed, or dissolved.
According to a report by the U.S. Department of Health and Human Services titled Analysis of Benzodiazepine Prescriptions in the United States, published in 2021, benzodiazepines, including clobazam, accounted for approximately 92 million prescriptions, reflecting their significant use in treating neurological conditions and anxiety.
What are The Signs and Symptoms of Clobazam?
The signs and symptoms of Clobazam are explained below:
-
Increased Tolerance: Increased tolerance occurs when the body requires higher doses of clobazam to achieve the same therapeutic or calming effect. This happens as the brain's GABA receptors adapt to the drug's presence, diminishing its efficacy over time.
According to a study by Ernst Schutz titled Toxicology of Clobazam, published in the British Journal of Clinical Pharmacology (1979), tolerance to clobazam develops with prolonged use, particularly at higher doses, as the body compensates by downregulating receptor sensitivity. This adaptation compels users to increase their intake, which accelerates the progression to addiction and creates dependency. -
Dependence: Dependence refers to the body's reliance on clobazam to maintain normal physiological functions, leading to withdrawal symptoms when the drug is reduced or stopped. Dependence manifests because clobazam alters GABA activity, and the brain compensates by producing less of its natural inhibitory signals. A report by Teva Canada Limited titled Teva-Clobazam Product Monograph (2017) highlights that even therapeutic doses of clobazam taken for just a few weeks cause physical dependence. Withdrawal symptoms, including anxiety, seizures, and muscle pain, are indicators of dependence.
-
Cravings: Cravings are the intense desire to consume clobazam, driven by psychological dependency. They occur because the brain associates clobazam use with relief from anxiety or stress, reinforcing the behavior. The reinforcing effects of clobazam are tied to its ability to modulate GABA pathways. Over time, these effects create a compulsive urge to use the drug, even when it is no longer medically necessary. Cravings are a hallmark of substance use disorders and drive risky behavior, such as self-medication or overdose.
-
Drowsiness: Drowsiness is a common symptom associated with clobazam use and withdrawal. The drug’s sedative properties are due to its enhancement of GABA’s inhibitory effects, which slow down brain activity and induce sleep-like states.
A study by Schliessbach et al., titled Analgesic Effect of Clobazam in Chronic Low-Back Pain but Not in Experimentally Induced Pain, published in the European Journal of Pain (2017), identifies drowsiness as a primary side effect of clobazam, particularly at higher doses. During withdrawal, the absence of clobazam leads to rebound insomnia or fatigue, exacerbating dependency symptoms. -
Cognitive Impairment: Cognitive impairment refers to difficulties in memory, attention, and decision-making, commonly experienced by those misusing clobazam. The drug’s impact on GABA receptors disrupts normal brain function, impairing cognitive processing.
Chronic clobazam use is associated with slowed mental activity and poor decision-making, which are exacerbated during withdrawal. Prolonged benzodiazepine use leads to persistent deficits in cognitive performance, which contribute to social and occupational dysfunction. -
Mood Changes: Mood changes, including irritability, anxiety, or depression, are common with clobazam use and withdrawal. These occur as the brain struggles to regulate emotions without the drug’s calming effect. Research by Harriet Hammer in Functional Characterization of Clobazam and Its Major Active Metabolite N-Desmethylclobazam, published in PLOS ONE (2015), highlights that abrupt cessation or reduction in clobazam use results in emotional dysregulation due to the disrupted GABAergic balance. Such mood swings further reinforce the cycle of addiction.
-
Social Withdrawal: Social withdrawal involves avoiding friends, family, and responsibilities due to preoccupation with clobazam use. This behavior stems from feelings of shame, dependence, or fear of judgment. Social withdrawal exacerbates addiction by isolating individuals from support systems. It is both a symptom of psychological dependency and a contributor to its progression, as isolation reduces the likelihood of seeking help or intervention.
-
Doctor Shopping: Doctor shopping refers to visiting multiple healthcare providers to obtain clobazam prescriptions illicitly. This behavior is driven by dependency and the need to secure more of the drug. Doctor shopping is a red flag for addiction, as it indicates that individuals are taking steps to circumvent medical guidance. Regulatory bodies identify this behavior as a primary indicator of substance misuse, often prompting intervention.
-
Physical Symptoms (e.g., Dizziness, Weakness): Clobazam’s effects on the central nervous system cause physical symptoms such as dizziness and weakness. These are common side effects of the drug and also emerge during withdrawal. During withdrawal, the absence of clobazam causes rebound hyperactivity in the nervous system, resulting in symptoms like dizziness, muscle weakness, and tremors. These symptoms show the physical dependency that characterizes addiction.
-
Risky Behavior: Individuals misusing clobazam often engage in risky behavior, such as driving under the influence or engaging in unsafe activities. This occurs because the drug impairs judgment and increases impulsivity. A study by Biehl et al., Studies of Clobazam and Car-Driving, published in the British Journal of Clinical Pharmacology (1979), found that clobazam users exhibited delayed reaction times and impaired concentration, leading to higher incidences of risky actions.
What are The Causes of Clobazam Addiction?
The causes of clobazam addiction include prolonged use, using higher doses than prescribed, self-medicating, genetic predisposition, co-occurring disorders, a history of substance abuse, and lack of medical supervision.
Prolonged use and escalating doses lead to physical dependence, while self-medication and inadequate medical oversight increase the risk of misuse and addiction, particularly in individuals with underlying mental health conditions or genetic vulnerabilities.
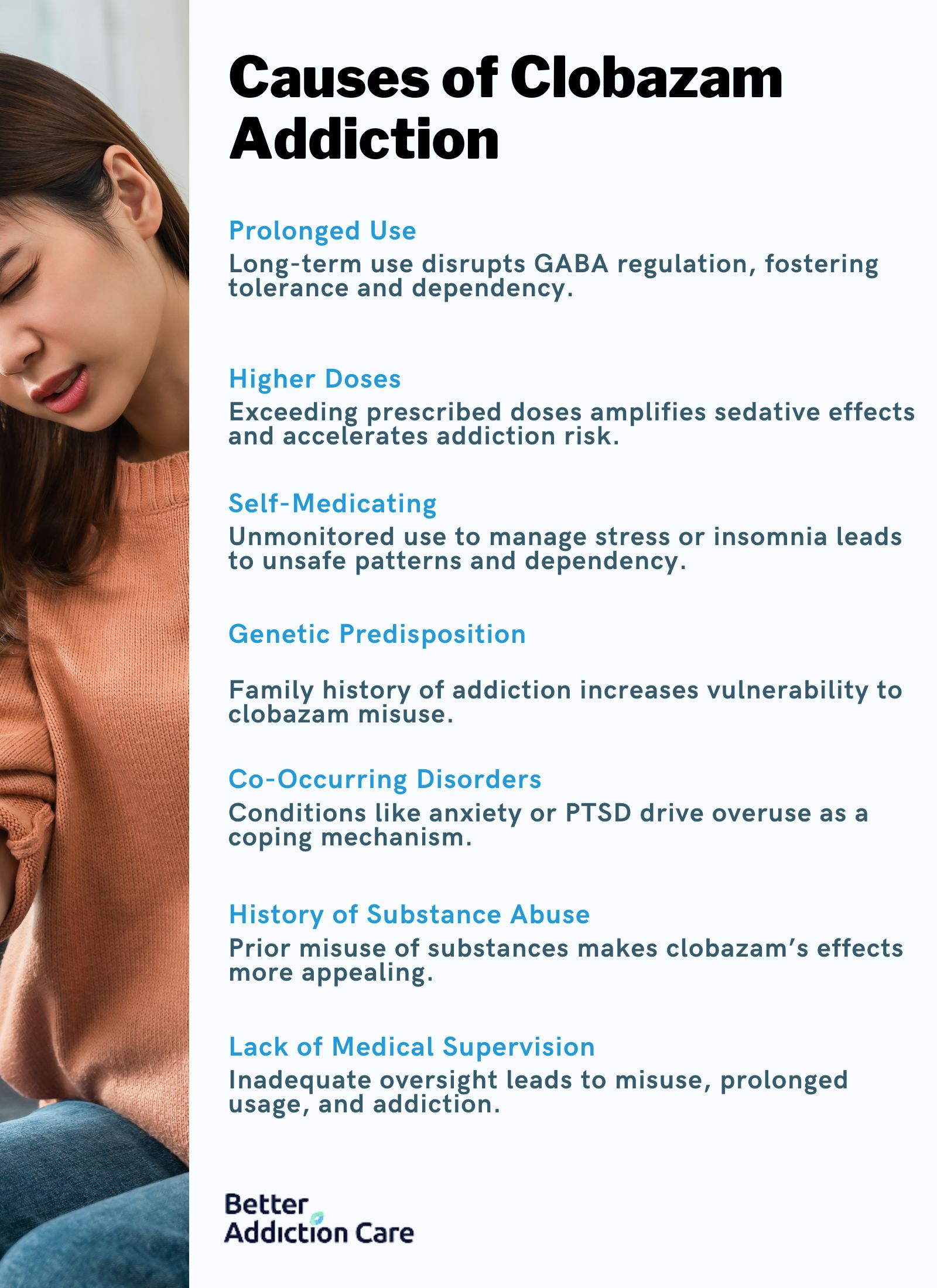
The causes of clobazam addiction are explained below:
-
Prolonged use of clobazam: Extended use of clobazam alters the brain’s natural regulation of gamma-aminobutyric acid (GABA), creating a dependency on the external supply provided by the medication. Over time, the body’s own GABA production decreases, leading to tolerance and the need for higher doses to achieve the same effects. Prolonged exposure also reinforces the brain's reward mechanisms, increasing the likelihood of addiction. According to a report by Teva Canada Limited titled Teva-Clobazam Product Monograph (2017), even therapeutic doses taken over several weeks lead to dependency and withdrawal symptoms upon cessation.
-
Using higher doses than prescribed: Exceeding prescribed doses accelerates the brain’s adaptation to clobazam, which diminishes its therapeutic effects and fosters tolerance. This behavior stems from a desire to amplify the drug’s calming or euphoric effects. Higher doses not only enhance the risk of dependency but also increase the likelihood of experiencing withdrawal symptoms such as anxiety and insomnia. The study by Ernst Schutz titled Toxicology of Clobazam, published in the British Journal of Clinical Pharmacology (1979), emphasizes that escalating doses intensify the sedative effects, making addiction more probable.
-
Self-medicating: Self-medicating with clobazam to manage stress, anxiety, or insomnia bypasses critical safety protocols, leading to unregulated and unsafe usage patterns. Individuals take doses higher than medically advised or use the drug for unintended purposes, compounding the risk of addiction. This behavior is particularly problematic because it prevents proper monitoring of side effects or dependency development. Morrison et al.'s study, A Phase 1 Open-Label Pharmacokinetic Trial to Investigate Possible Drug-Drug Interactions with Clobazam and Cannabidiol, published in Clinical Pharmacology in Drug Development (2019), notes that unmonitored use is a significant factor in clobazam misuse and subsequent addiction.
-
Genetic predisposition: A family history of addiction predisposes individuals to dependency on substances like clobazam. Genetic factors influence the brain’s reward system, making it more responsive to the pleasurable effects of the drug and harder to regulate its use. This inherent vulnerability increases the likelihood of developing addiction even when clobazam is taken as prescribed.
-
Co-occurring disorders: Mental health conditions such as anxiety, depression, or post-traumatic stress disorder (PTSD) drive individuals to overuse clobazam for its sedative properties. These co-occurring disorders increase reliance on the drug as a coping mechanism, heightening the risk of addiction. Without appropriate treatment for the underlying mental health issues, patients are more likely to misuse clobazam in an attempt to self-manage their symptoms.
-
History of substance abuse: Individuals with a prior history of substance abuse are at heightened risk of clobazam addiction due to established patterns of seeking and using psychoactive substances. Clobazam’s calming and euphoric effects make it particularly attractive to those who have previously misused drugs or alcohol, as it provides a similar sense of relief or escape.
-
Lack of medical supervision: Insufficient oversight during treatment with clobazam leaves patients vulnerable to mismanagement of the medication. Without regular monitoring by healthcare professionals, individuals take the drug longer than necessary, increase their dosage unsupervised, or misuse it. This lack of regulation allows dependency and addiction to develop unchecked.
What are The Effects of Clobazam Addiction?
The effects of clobazam addiction affect individuals both physically and psychologically, with short and long-term consequences. Short-term effects primarily involve the drug’s impact on the central nervous system, while long-term effects result from chronic misuse and dependency.
Many of these effects, especially withdrawal symptoms, occur when the drug is reduced or stopped suddenly, showing the addictive nature of clobazam.
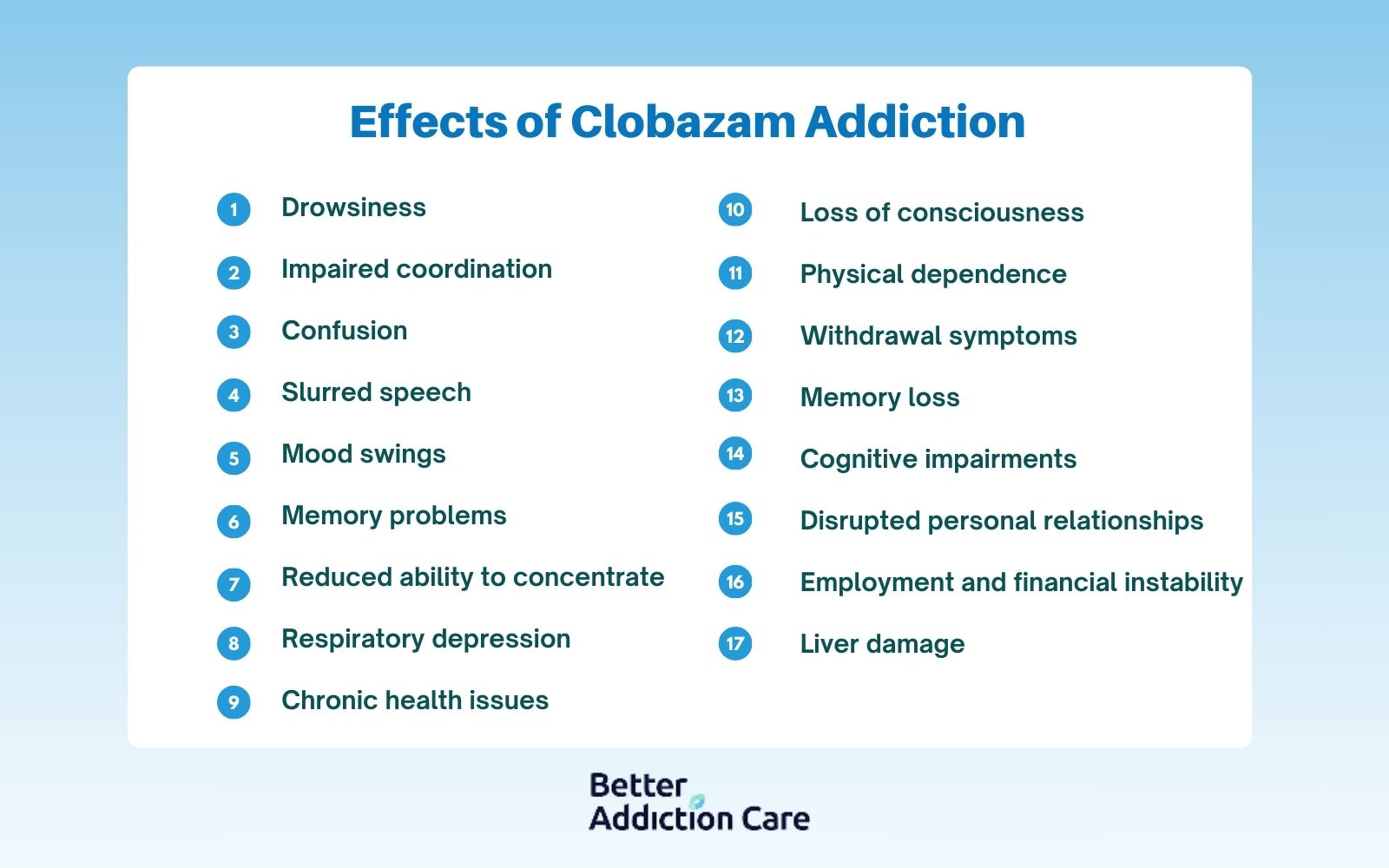
The effects of Clobazam addiction are detailed below:
-
Drowsiness: Drowsiness is a short-term physical effect caused by clobazam’s sedative properties, which slow down central nervous system activity. This symptom impairs daily functioning and increases the risk of accidents. According to a study by Schliessbach et al., "Analgesic Effect of Clobazam in Chronic Low-Back Pain but Not in Experimentally Induced Pain," published in the European Journal of Pain (2017), drowsiness is a frequent side effect of clobazam use.
-
Impaired coordination: Clobazam affects motor control, leading to impaired coordination and a short-term physical effect. This symptom poses risks during activities requiring precise movements, such as driving or operating machinery. The Teva-Clobazam Product Monograph (2017) notes that impaired coordination is a common concern among clobazam users, especially at higher doses.
-
Confusion: Confusion is a short-term psychological effect caused by clobazam’s depressant action on brain activity, disrupting cognitive clarity. This symptom is associated with higher doses or withdrawal periods. Ernst Schutz, in the study Toxicology of Clobazam, published in the British Journal of Clinical Pharmacology (1979), highlights confusion as a primary indicator of clobazam misuse.
-
Slurred speech: Slurred speech is a short-term physical effect caused by clobazam’s suppression of motor control in the brain's speech centers. This symptom is a direct result of the drug’s impact on central nervous system activity and worsens with higher doses.
-
Mood swings: Mood swings are a psychological effect that is both short- and long-term, depending on the stage of addiction or withdrawal. Clobazam disrupts emotional regulation by altering GABAergic signaling, leading to episodes of irritability, anxiety, or euphoria. Harriet Hammer’s study, Functional Characterization of Clobazam and Its Major Active Metabolite N-Desmethylclobazam, published in PLOS ONE (2015), identifies mood instability as a withdrawal symptom due to the brain’s inability to stabilize emotions without the drug.
-
Memory problems: Memory problems are a short-term psychological effect linked to clobazam’s suppression of cognitive processes. Prolonged misuse exacerbates this issue, leading to long-term memory deficits. The Teva-Clobazam Product Monograph (2017) explains that benzodiazepines like clobazam impair memory formation, particularly short-term recall, during both use and withdrawal.
-
Reduced ability to concentrate: Clobazam diminishes the ability to focus, a short-term psychological effect resulting from its sedative action. This symptom affects productivity and cognitive performance, particularly during periods of active use or early withdrawal.
-
Respiratory depression: Respiratory depression is a severe short-term physical effect where breathing slows significantly, posing a life-threatening risk, especially at higher doses. This symptom arises from clobazam’s depressant impact on the respiratory centers of the brain.
-
Loss of consciousness: Loss of consciousness is a critical short-term physical effect that occurs when clobazam is taken in excessive doses. This symptom necessitates immediate medical attention. Research by Biehl et al., titled Studies of Clobazam and Car-Driving, emphasizes the danger of high-dose clobazam use leading to sudden unconsciousness.
-
Physical dependence: Physical dependence is a long-term effect that develops as the body adapts to the presence of clobazam. Dependence manifests through withdrawal symptoms like seizures, muscle pain, and anxiety when the drug is discontinued. The Teva-Clobazam Product Monograph explains that dependence develops even with therapeutic use over several weeks.
-
Withdrawal symptoms (e.g., seizures, tremors, severe anxiety): Withdrawal symptoms are a combination of physical and psychological effects experienced when clobazam is reduced or stopped. These symptoms, including seizures and severe anxiety, are hallmark signs of long-term dependence.
-
Memory loss: Chronic clobazam use leads to memory loss, a long-term psychological effect caused by the drug’s disruption of neural pathways involved in memory formation and recall. This symptom is particularly evident in individuals with long-term dependency, affecting their quality of life.
-
Cognitive impairments: Cognitive impairments, including reduced problem-solving ability and slower mental processing, are long-term psychological effects. These deficits are irreversible after prolonged misuse, emphasizing the drug’s impact on brain health.
-
Disrupted personal relationships: Addiction-induced mood swings, social withdrawal, and erratic behavior lead to disrupted relationships, a long-term social effect. These issues strain family and professional interactions, often leaving individuals isolated.
-
Employment and financial instability: Addiction’s impact on concentration, productivity, and decision-making often leads to job loss and financial difficulties, making this a significant long-term social consequence.
-
Liver damage: Chronic use of clobazam places stress on the liver, leading to long-term physical effects such as liver toxicity and potential organ failure. This condition shows the cumulative damage caused by prolonged drug metabolism.
-
Chronic health issues: Chronic misuse contributes to gastrointestinal, cardiovascular, and immune system dysfunction, making it a long-term physical effect. These conditions worsen over time, complicating recovery.
What is The Withdrawal Timeline for Clobazam?
The withdrawal timeline for clobazam addiction ranges from a few days to several months, with some symptoms potentially persisting for over a year in severe cases. This process is divided into phases, each with distinct symptoms that reflect the body's gradual adaptation to the absence of clobazam.
The withdrawal timeline for clobazam is explained below:
-
Initial Phase (6-24 Hours): This phase begins shortly after the last dose, especially for those taking lower doses. Symptoms include mild anxiety, restlessness, and irritability as the body starts to recognize the absence of clobazam’s calming effects. Physical symptoms such as mild tremors or sweating also occur during this phase.
-
Acute Phase (2-5 Days): The acute phase represents the peak of withdrawal intensity and is characterized by more severe physical and psychological symptoms. Common symptoms include heightened anxiety, muscle tremors, insomnia, and gastrointestinal distress. In individuals with significant dependence, seizures also occur during this phase, necessitating medical supervision.
-
Subacute Phase (6-14 Days): Symptoms during the subacute phase begin to taper off but remain disruptive. Anxiety and mood instability persist, accompanied by fatigue, mild tremors, and difficulty concentrating. Sleep disturbances continue, although their severity decreases. Harriet Hammer, in Functional Characterization of Clobazam and Its Major Active Metabolite N-Desmethylclobazam, published in PLOS ONE (2015), notes that emotional dysregulation and cognitive impairments are common during this stage.
-
Post-Acute Phase (2-4 Weeks): During this phase, symptoms become less severe but may still include intermittent anxiety, low energy, and occasional mood swings. Cognitive function and sleep patterns gradually improve. However, cravings for clobazam may persist, requiring psychological support to prevent relapse.
-
Prolonged Phase (1-3 Months): In individuals with long-term or high-dose use, some withdrawal symptoms may persist for several months. These symptoms, referred to as post-acute withdrawal syndrome (PAWS), include episodic anxiety, depression, and difficulty concentrating. According to Ernst Schutz in Toxicology of Clobazam, published in the British Journal of Clinical Pharmacology (1979), these prolonged symptoms reflect the long-term adaptations of the brain to benzodiazepine use.
How to Treat Clobazam Addiction?
To treat clobazam addiction, a combination of medical detoxification, therapy, medication-assisted treatment (MAT), counseling, and support groups is essential. These interventions target both the physical dependency and the psychological aspects of addiction, ensuring a comprehensive recovery plan adapted to the unique challenges posed by clobazam.

The ways to treat clobazam addiction are explained below:
1. Medical Detoxification: Medical detoxification is the first step in treating clobazam addiction and involves safely managing withdrawal symptoms under medical supervision. A gradual tapering schedule is implemented to minimize severe withdrawal effects such as seizures or anxiety.
This process is highly effective for clobazam due to its long half-life, allowing physicians to control symptom progression more predictably. According to the Teva-Clobazam Product Monograph (2017), medically supervised detox reduces the risk of life-threatening withdrawal complications and provides a structured path to discontinuation.
2. Therapy: Therapy, particularly cognitive-behavioral therapy (CBT), plays a vital role in addressing the psychological dependency on clobazam. CBT helps patients identify triggers, develop coping strategies, and restructure thought patterns that contribute to substance use.
Specific to clobazam, therapy focuses on reducing reliance on the drug for managing anxiety or stress. Harriet Hammer’s study, published in PLOS ONE (2015), states that addressing psychological triggers is critical for reducing relapse risks in benzodiazepine addiction.
3. Treatment (Inpatient vs. Outpatient): Inpatient treatment provides a controlled environment for individuals with severe clobazam addiction, offering 24-hour medical care and access to therapeutic interventions. This approach is particularly effective for those at risk of severe withdrawal symptoms, such as seizures or suicidal ideation.
Outpatient treatment, while less intensive, allows patients to stay at home and maintain daily responsibilities while attending regular therapy sessions. For clobazam addiction, inpatient care is recommended during detoxification, transitioning to outpatient care for long-term recovery.
4. Medication-Assisted Treatment (MAT): MAT involves using medications such as antidepressants or anticonvulsants to manage withdrawal symptoms and stabilize mood. For clobazam addiction, medications like gabapentin are prescribed to address anxiety and prevent seizures during withdrawal.
Ernst Schutz’s study, published in the British Journal of Clinical Pharmacology (1979), highlights the effectiveness of using adjunct medications to reduce withdrawal severity and support recovery. MAT is particularly useful in maintaining physiological stability during the early stages of treatment.
5. Counseling: Individual and group counseling helps patients explore the emotional and behavioral roots of their clobazam addiction. This approach allows individuals to address co-occurring mental health disorders, such as anxiety or depression, which drive benzodiazepine misuse. Counseling adapted to clobazam users focuses on managing anxiety without reliance on medication, fostering sustainable coping mechanisms.
6. Support Groups: Support groups such as Narcotics Anonymous (NA) or specialized benzodiazepine recovery programs provide peer support and accountability throughout recovery. These groups are particularly beneficial for clobazam addiction as they address the unique challenges of benzodiazepine withdrawal and dependency. Peer interactions foster a sense of community and resilience, which are necessary for preventing relapse.
How is Clobazam Regulated in The US?
Clobazam is regulated in the US through the Controlled Substances Act (CSA), which classifies it as a Schedule IV controlled substance due to its potential for abuse and dependency.
The regulation of clobazam is overseen by the Drug Enforcement Administration (DEA) and the Food and Drug Administration (FDA), ensuring its medical use is carefully monitored while minimizing the risk of misuse.
As a Schedule IV substance, clobazam is recognized to have a lower abuse potential compared to Schedule II or III drugs. Still, it poses a risk of physical and psychological dependence.
According to the DEA's Controlled Substances Act guidelines, Schedule IV substances, including clobazam, are available by prescription only, and their distribution is tightly controlled to prevent diversion or illegal use.
The FDA also mandates that prescribing information highlights the risks of addiction and dependence associated with clobazam, ensuring that healthcare providers and patients are informed of its proper usage.
What is Clobazam Half-Life?
The average half-life of clobazam ranges from 36 to 42 hours, during which time the drug's concentration in the bloodstream reduces by half. Depending on individual factors, it takes approximately 10 days for clobazam to fully clear from the body.
Age, liver function, metabolic rate, and the use of other medications influence how quickly or slowly clobazam is metabolized and excreted. For instance, individuals with impaired liver function or those taking medications that inhibit liver enzymes experience a prolonged clearance time.
Clobazam’s long half-life significantly impacts withdrawal and dependency. The slower onset of withdrawal symptoms delays recognition of dependency, while its prolonged presence in the body increases the duration of the withdrawal process.
This extended timeline contributes to a heightened risk of dependency, as the drug’s calming effects last longer, making individuals more likely to continue using it to avoid withdrawal discomfort.
According to the Teva-Clobazam Product Monograph (2017), the active metabolite N-desmethylclobazam also prolongs the drug's overall effects, further complicating withdrawal and dependency management.
What is Clobazam Used for?
Clobazam is used for the treatment of seizures, particularly epilepsy, management of Lennox-Gastaut syndrome, anxiety disorders, muscle spasms, sedation prior to medical procedures, and as adjunctive therapy for drug-resistant epilepsy.
Its primary action is to enhance the effects of gamma-aminobutyric acid (GABA). This neurotransmitter helps calm overactive nerve signals, making it effective for a range of neurological and psychiatric conditions.

Conditions clobazam is used for are explained below:
-
Treatment of seizures (epilepsy): Clobazam is a key medication in controlling seizures, particularly in patients with epilepsy who have not responded well to other treatments. According to the Centers for Disease Control and Prevention (CDC), approximately 3.4 million Americans, including 470,000 children, have active epilepsy. Clobazam is prescribed to reduce the frequency and severity of seizures, providing critical support for these individuals in managing their condition.
-
Management of Lennox-Gastaut syndrome: Lennox-Gastaut syndrome is a rare and severe form of childhood epilepsy characterized by multiple seizure types and cognitive impairment. Clobazam is specifically FDA-approved for managing seizures in this condition, as it has been shown to reduce seizure frequency significantly. The Epilepsy Foundation reports that Lennox-Gastaut syndrome accounts for 1-4% of all childhood epilepsy cases in the U.S., affecting approximately 14,500 to 40,000 children.
-
Anxiety disorders: Clobazam’s anxiolytic properties make it a secondary treatment for anxiety disorders, helping to alleviate severe symptoms of nervousness and panic. According to the National Institute of Mental Health (NIMH), over 40 million adults in the U.S. suffer from anxiety disorders annually, representing nearly 19% of the population. While not a first-line treatment, clobazam is prescribed in cases where other therapies are insufficient.
-
Muscle spasms: Clobazam is effective in relieving muscle spasms because it relaxes muscles by reducing excessive neuronal activity. Muscle spasms are a common symptom of various neurological conditions, including multiple sclerosis and spinal cord injuries, and affect millions of Americans. Clobazam helps improve mobility and reduce pain in affected individuals.
-
Sedation pre-procedure: Clobazam is a pre-procedural sedative used to calm patients and ensure their comfort during medical or dental treatments. This use is particularly beneficial for individuals with severe anxiety about procedures, enabling smoother and more effective interventions.
-
Adjunctive therapy for resistant epilepsy: For patients with drug-resistant epilepsy, clobazam is often added to existing treatment regimens to improve seizure control. This is particularly important given that about 30% of epilepsy patients do not achieve seizure freedom with standard medications, according to the CDC. Clobazam’s role as an adjunctive therapy has been widely recognized for enhancing outcomes in such challenging cases.
What is The Chemical Composition of Clobazam?
The chemical composition of clobazam is 1H-1,5-benzodiazepine-2,4-dione, 7-chloro-1-methyl-5-phenyl. Its molecular formula is C16H13ClN2O2, with a molecular weight of 300.74 g/mol.
The chemical structure of clobazam features a fused 1,5-diazepine ring system, distinct from the more common 1,4-diazepines, which alters its pharmacokinetic and pharmacodynamic properties. A chlorine atom on the aromatic ring enhances its potency, while the ketone group at the 2-position contributes to its sedative and anticonvulsant effects.
This structural arrangement differentiates Clobazam from other benzodiazepines. It makes it less sedative while retaining strong anticonvulsant properties, which are necessary for managing conditions like Lennox-Gastaut syndrome and refractory epilepsy.
The unique 1,5-diazepine configuration is central to its pharmacological profile, optimizing its efficacy while minimizing some common benzodiazepine side effects.
Can You Overdose on Clobazam?
Yes, it is possible to overdose on clobazam if the recommended dosage is exceeded. The typical therapeutic dose of clobazam ranges from 5 mg to 40 mg per day, divided into two doses.
Overdoses occur when individuals consume significantly higher amounts, such as exceeding 50 mg to 100 mg or more in a single administration, either intentionally or accidentally. The risk is compounded when clobazam is taken with alcohol or other central nervous system depressants, which can amplify its sedative effects and increase toxicity.
Clobazam overdoses are not uncommon. According to the National Poison Data System (NPDS) annual report, benzodiazepines, including clobazam, accounted for approximately 35,000 emergency department visits in the U.S. in 2020 due to overdose cases. The report highlights that polydrug use, where clobazam is combined with opioids or alcohol, significantly increases the likelihood of fatal outcomes.
Symptoms of a clobazam overdose include extreme drowsiness, confusion, respiratory depression, and, in severe cases, loss of consciousness or death. Prompt medical attention is essential to manage overdose cases, requiring the administration of flumazenil, a benzodiazepine antagonist, to reverse the effects.
Is Clobazam a Controlled Substance?
Yes, clobazam is a controlled substance in the United States because of its potential for abuse, dependency, and overdose. It is classified as a Schedule IV drug under the Controlled Substances Act (CSA), indicating a lower risk of abuse compared to higher schedules but still requiring regulation to prevent misuse.
Individuals consuming clobazam in doses exceeding 100 mg, especially in combination with alcohol, present with life-threatening respiratory issues requiring emergency intervention. According to the National Institute on Drug Abuse (NIDA), benzodiazepine-related overdoses accounted for over 16% of all drug overdose deaths in 2021, with polydrug interactions being a leading factor.
What is The Typical Dosage for Clobazam?
The typical dosage of clobazam ranges from 5 mg to 40 mg per day, divided into two doses, depending on the patient’s age, condition, and response to treatment.
For adults managing seizures or Lennox-Gastaut syndrome, the initial dose is generally 5 mg to 10 mg per day, divided into two doses, with gradual titration up to a maximum of 40 mg daily. Pediatric doses are calculated based on weight, usually starting at 0.5 mg/kg/day.
Clobazam’s long half-life allows for flexible dosing schedules, but adherence to prescribed limits is critical to minimize the risk of dependency or overdose.
Current research indicates no significant differences in dosage recommendations between male and female adults. However, physiological factors such as body weight, metabolic rate, and liver function influence the drug's efficacy and tolerance in individuals.
According to the FDA-approved Clobazam Prescribing Information, careful monitoring is essential for all patients, particularly during dose escalation or long-term therapy, to ensure safety and therapeutic effectiveness.
Should You Take Clobazam When You're Pregnant?
No, you should not take clobazam when pregnant due to its potential risks to the fetus. Clobazam, like other benzodiazepines, has been associated with an increased risk of congenital malformations, particularly during the first trimester.
According to the FDA, benzodiazepines carry a Pregnancy Category D designation, indicating positive evidence of human fetal risk based on adverse reaction data.
Prolonged use of clobazam during pregnancy leads to neonatal withdrawal syndrome, characterized by irritability, respiratory distress, and feeding difficulties in newborns. The National Institute on Drug Abuse states this risk as a significant concern for infants exposed to benzodiazepines in utero.
Furthermore, prenatal exposure to benzodiazepines impairs fetal brain development, affecting cognitive and motor functions later in life. Research published in The American Journal of Obstetrics and Gynecology advises caution in prescribing these drugs to pregnant individuals due to these long-term risks.
Does Clobazam Make You High?
Yes, clobazam can make individuals feel high, particularly when taken in higher doses than prescribed or used recreationally.
Clobazam is a benzodiazepine that enhances the effects of gamma-aminobutyric acid (GABA), a neurotransmitter that calms the central nervous system. This action produces feelings of relaxation and euphoria in some individuals, which is perceived as high.
The misuse of clobazam also leads to sedation and a sense of detachment from reality effects that recreational users seek. Finally, its slow onset and long half-life prolong these calming sensations, increasing the potential for misuse and dependency.
The National Institute on Drug Abuse reports that benzodiazepines, including clobazam, are among the most misused prescription drugs due to their sedative and euphoric properties.
Is Clobazam a Benzodiazipine?
Yes, clobazam is a benzodiazepine because it belongs to the class of drugs that act on gamma-aminobutyric acid (GABA) receptors in the brain to produce calming effects.
Unlike the more common 1,4-benzodiazepines, clobazam is a 1,5-benzodiazepine characterized by its unique chemical structure. This structure contributes to its anticonvulsant properties with comparatively less sedation. This distinction makes it particularly effective for managing seizures while maintaining its classification as a benzodiazepine.
How Does Clobazam Make You Feel?
Clobazam makes you feel calm and relaxed by enhancing the activity of gamma-aminobutyric acid (GABA), a neurotransmitter that reduces overactive brain signals. This calming effect helps alleviate symptoms of anxiety, stress, and seizures, making it an effective treatment for various neurological and psychiatric conditions.
At therapeutic doses, clobazam primarily reduces excessive nerve activity without causing intense sedation, allowing patients to maintain normal functioning.
However, higher doses or misuse of clobazam produce a sense of euphoria, sedation, and even detachment from reality. These effects are due to its depressant action on the central nervous system, which leads to drowsiness, impaired coordination, and a slowed perception of the environment.
Over time, regular use alters the brain’s natural calming mechanisms, contributing to dependency and reinforcing its misuse. This blend of therapeutic benefits and potential side effects shows the importance of using clobazam strictly under medical supervision.
How Does Clobazam Interact with Other Drugs?
Clobazam interacts with other drugs, such as opioids, other benzodiazepines, antidepressants, and alcohol, by amplifying their sedative and depressant effects.
These interactions are dangerous, increasing the risk of respiratory depression, excessive sedation, and overdose. The combination of clobazam with these substances is a significant concern, particularly in polydrug use, which accounts for a large proportion of drug-related fatalities.
Opioids combined with clobazam significantly increase the risk of respiratory depression, as both substances suppress the central nervous system. According to the National Institute on Drug Abuse (NIDA), opioids were involved in 80,411 overdose deaths in the United States in 2021, and benzodiazepines like clobazam are implicated as contributing substances.
When used with other benzodiazepines, clobazam amplifies the sedative effects, leading to profound drowsiness and loss of coordination. The Centers for Disease Control and Prevention (CDC) notes that benzodiazepines are frequently involved in emergency department visits due to drug interactions, particularly when taken with similar medications.
Antidepressants, especially those with sedative properties like tricyclic antidepressants or selective serotonin reuptake inhibitors (SSRIs), compound clobazam’s effects, leading to increased sedation and cognitive impairment.
Alcohol is one of the most dangerous substances to combine with clobazam. Both act as central nervous system depressants, significantly increasing the likelihood of respiratory failure and death. The National Institute on Alcohol Abuse and Alcoholism (NIAAA) reports that 95,000 deaths annually in the U.S. are alcohol-related, and polydrug use with benzodiazepines exacerbates these risks.
How Long Does Clobazam Stay in Your System?
Clobazam stays in your system for approximately 10 days after the last dose, with its average half-life ranging from 36 to 42 hours. This timeline varies depending on several factors, including the individual’s age, liver function, metabolic rate, dosage, and duration of use.
For instance, older adults or individuals with impaired liver function process the drug more slowly, prolonging its presence in the body. Conversely, younger individuals with faster metabolisms tend to clear clobazam more quickly.
The drug’s long half-life is further extended by its active metabolite, N-desmethylclobazam, which persists in the system for even longer, contributing to its sustained effects. Additionally, interactions with other medications, such as enzyme inhibitors or inducers, alter how quickly clobazam is metabolized.
This prolonged presence makes clobazam effective for managing chronic conditions like epilepsy but also complicates withdrawal and increases the risk of dependency with prolonged use.
What is The Difference Between Clobazam and Xanax?
The difference between clobazam and Xanax are in their uses, strength, and addiction potential. Clobazam is primarily prescribed for seizures, while Xanax treats anxiety and panic disorders.
Xanax addiction is common because the drug is more potent due to its rapid onset and intense sedative effects, making it effective for acute anxiety but more prone to misuse. Clobazam’s slower onset and longer half-life make it less addictive, though prolonged use still carries risks.
According to the National Institute on Drug Abuse, Xanax is one of the most commonly misused benzodiazepines, with over 16 million prescriptions issued annually in the U.S., reflecting its widespread use and potential for abuse.
What is The Difference Between Clobazam and Ativan?
The difference between clobazam and Ativan lies in their applications, strength, and duration of action. Clobazam is used primarily for seizures, while Ativan is prescribed for anxiety disorders and acute seizure management.
Ativan has a faster onset but a shorter half-life, making it suitable for immediate relief but requiring more frequent dosing. This shorter half-life contributes to the widespread Ativan addiction. Clobazam’s longer half-life offers sustained effects, particularly for epilepsy.
According to the National Institute on Drug Abuse, Ativan and similar benzodiazepines contribute to approximately 12% of all benzodiazepine misuse cases in the U.S., highlighting its addiction potential.
Does Clozabam Make You Sleepy?
Yes, clobazam makes you sleepy because it acts as a central nervous system depressant by enhancing the effects of gamma-aminobutyric acid (GABA), which slows brain activity. This sedative effect reduces overactive neural signaling, leading to drowsiness.
Another reason is its long half-life, which sustains its calming properties over an extended period. This makes sleepiness a common side effect, especially in individuals taking higher doses. Clobazam’s interaction with other medications or substances, such as alcohol, also amplifies its sedative effects, further contributing to drowsiness.
Is Clobazam a Controlled Drug?
Yes, clobazam is a controlled drug classified as a Schedule IV substance under the Controlled Substances Act (CSA) in the United States. This classification is due to its potential for abuse and dependency.
According to the Drug Enforcement Administration (DEA), Schedule IV drugs like clobazam have a lower risk of abuse compared to higher schedules but still require regulation to prevent misuse.
Who is At Risk for Clobazam Addiction?
People at risk for clobazam addiction include those with a history of substance abuse, mental health conditions, prolonged or high-dose use, and a lack of medical supervision.
Individuals with a history of substance abuse are at higher risk because they already have patterns of behavior that reinforce dependency on psychoactive substances. Mental health conditions, such as anxiety or depression, lead to over-reliance on clobazam for emotional relief, increasing the likelihood of misuse.
Prolonged or high-dose use causes the brain to adapt to clobazam’s effects, making physical and psychological dependency more likely. A lack of medical supervision exacerbates these risks by allowing misuse, unmonitored dose escalation, or prolonged therapy beyond therapeutic needs.
The National Institute on Drug Abuse emphasizes that these risk factors are prevalent among individuals misusing benzodiazepines like clobazam, requiring careful oversight to prevent addiction.
What Are The Complications of Abruptly Stopping Clobazam Use?
The complications of abruptly stopping clobazam use are seizures, severe anxiety, tremors, and rebound insomnia. These complications occur because the body becomes physically dependent on clobazam to regulate gamma-aminobutyric acid (GABA) activity, which calms the nervous system.
When clobazam is abruptly discontinued, its effects disappear, causing hyperactivity in the brain and neurological and psychological symptoms.
Seizures are one of the most severe complications, as the brain’s reduced GABA activity triggers uncontrolled neural firing. Severe anxiety and tremors result from the nervous system's heightened excitability, while rebound insomnia occurs as the body struggles to restore normal sleep regulation without the sedative effects of clobazam.
According to the Teva-Clobazam Product Monograph (2017), withdrawal symptoms like these begin within hours to days of cessation, emphasizing the need for gradual tapering to minimize risks.
Is Clobazam a High-Risk Medication?
Yes, clobazam is considered a high-risk medication due to its potential for dependency, withdrawal complications, and interactions with other substances. As a benzodiazepine, clobazam alters gamma-aminobutyric acid (GABA) activity, making prolonged use likely to result in physical and psychological dependency.
Abrupt discontinuation can lead to severe withdrawal symptoms, including seizures and anxiety, which pose significant health risks. Additionally, clobazam’s sedative effects are amplified when combined with alcohol or opioids, increasing the likelihood of respiratory depression and overdose.
According to the FDA, benzodiazepines like clobazam require careful prescription and monitoring due to these risks.
Does Clobazam Addiciton Impact Mental Health?
Yes, clobazam addiction impacts mental health by exacerbating anxiety, depression, and emotional instability. Dependency on clobazam alters the brain’s natural regulation of gamma-aminobutyric acid (GABA), creating a reliance on the drug to manage stress and anxiety.
Over time, this dependency worsens baseline anxiety and leads to depressive symptoms when the drug is unavailable or during withdrawal. Additionally, prolonged misuse affects cognitive function, memory, and emotional regulation, making it difficult for individuals to cope without medication.
According to the National Institute on Drug Abuse, benzodiazepine misuse is strongly associated with co-occurring mental health disorders, further complicating treatment and recovery.
What Alternative Medications Are Used Instead of Clobazam?
The alternative medications used instead of clobazam are lamotrigine, valproic acid, levetiracetam, and topiramate. These medications are commonly prescribed for managing seizures and epilepsy and are preferred when benzodiazepines are unsuitable due to dependency risks or side effects.
Lamotrigine is widely used as an antiepileptic drug, particularly for generalized and partial seizures. It stabilizes neuronal activity by inhibiting sodium channels, making it an effective long-term option.
Valproic acid, another popular choice, works by increasing gamma-aminobutyric acid (GABA) levels in the brain, offering seizure control without the sedative properties of clobazam.
Levetiracetam, known for its fewer side effects and lower risk of dependency, has also gained popularity in treating epilepsy, especially in pediatric patients.
According to the Epilepsy Foundation, levetiracetam accounts for a significant portion of antiepileptic prescriptions due to its high tolerability and effectiveness in over 70% of patients with focal seizures.







