Cymbalta for Pain, Anxiety & Other Uses: Is It Abusable?
Many people turn to Cymbalta when pain, anxiety, or depression start interfering with daily life. When the medication finally brings relief, it’s natural to want that stability to last. But over time, some people take extra doses on difficult days, adjust timing on their own, or feel uneasy about missing a pill.

Key Takeaways
-
Cymbalta helps with depression, anxiety, and chronic pain by balancing brain chemicals.
-
It isn’t considered addictive, but emotional reliance and misuse can still develop for some people.
-
Stopping suddenly may trigger withdrawal symptoms, so a slow, supervised taper is safest.
-
With medical guidance, therapy, and supportive habits, people can recover from misuse or dependence-like patterns.
Families are often surprised when someone feels sick, irritable, or anxious during missed doses or a taper. Cymbalta isn’t an opioid or benzodiazepine, so these reactions can be confusing. But because it affects mood, pain, and stress pathways, stopping too quickly can trigger real discomfort.
This article explains what Cymbalta does, why some people struggle with withdrawal or misuse patterns, and how safe tapering and supportive care can help. The goal is to give individuals and families clarity—and reassure them that these challenges are manageable with the right guidance.
What Is Cymbalta Misuse?
Cymbalta (duloxetine) is an SNRI antidepressant used for:
-
Major depressive disorder
-
Neuropathic pain
-
Fibromyalgia
-
Chronic musculoskeletal pain
-
Pelvic pain
-
Diabetic neuropathy
Its mechanism targets serotonin and norepinephrine pathways—chemicals that regulate mood, energy, and how the brain interprets pain.
Tolerance: Some people find that Cymbalta stops working as well after months or years. They may want higher doses or take more on difficult days.
Dependence: Stopping Cymbalta abruptly can trigger withdrawal symptoms (sometimes called Cymbalta discontinuation syndrome), which may include dizziness, brain zaps, nausea, panic spikes, or flu-like symptoms. [1]
Misuse: Cymbalta misuse is different from addiction. It means using the medication in ways not prescribed:
-
Taking extra doses for emotional numbing
-
Using it for energy or calm
-
Continuing despite side effects
-
Hoarding pills for fear of running out
-
Feeling unable to miss a dose
While Cymbalta is not considered chemically addictive like opioids or benzodiazepines, these patterns can still cause harm and require support.
Signs & Symptoms of Cymbalta Misuse
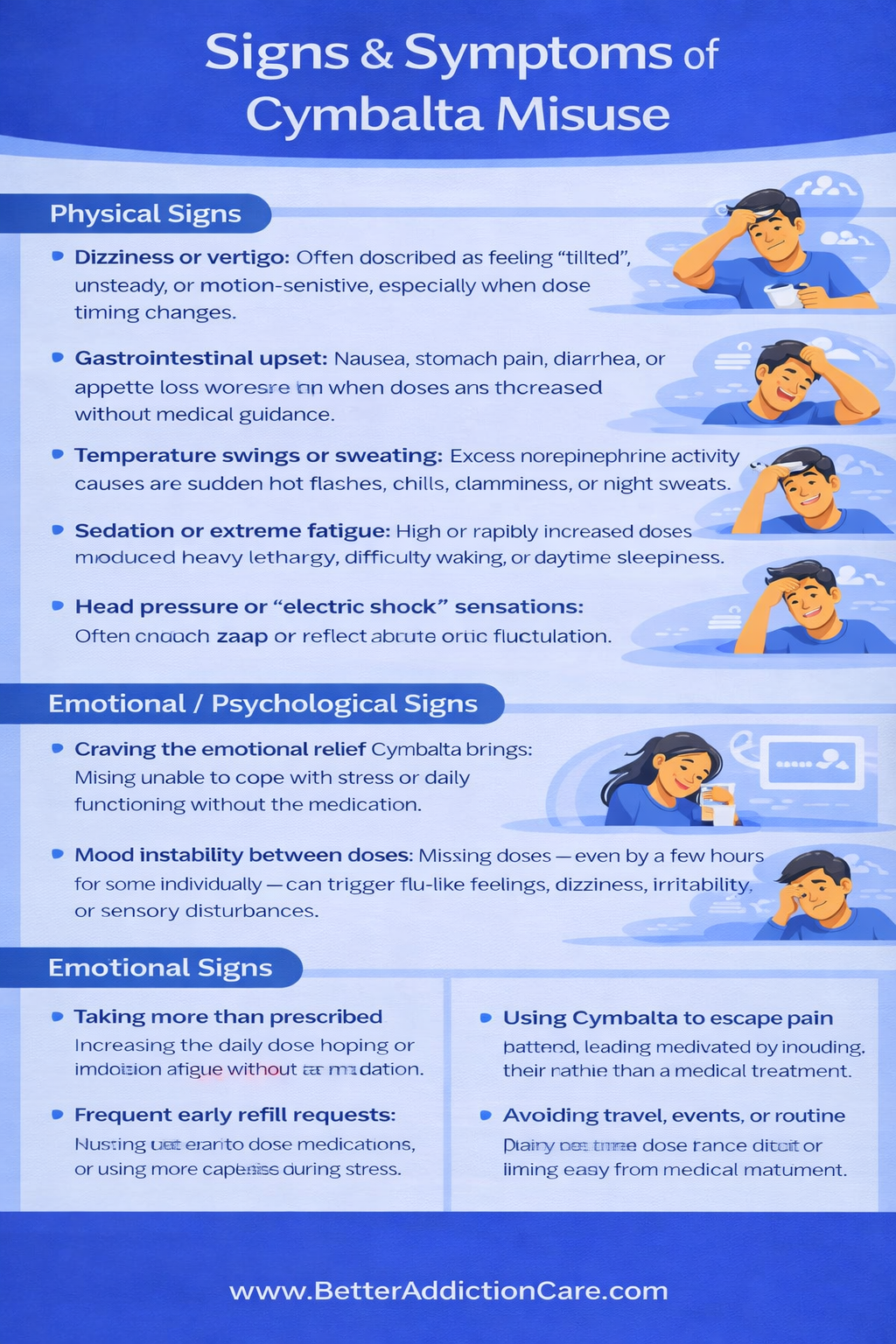
Physical Signs
-
Dizziness or vertigo: Often described as feeling “tilted,” unsteady, or motion-sensitive, especially when dose timing changes.
-
Gastrointestinal upset: Nausea, stomach pain, diarrhea, or appetite loss can worsen when doses are increased without medical guidance.
-
Temperature swings or sweating: Excess norepinephrine activity can cause sudden hot flashes, chills, clamminess, or night sweats.
-
Sedation or extreme fatigue: High or rapidly increased doses may produce heavy lethargy, difficulty waking, or daytime sleepiness.
-
Head pressure or “electric shock” sensations: Often called “brain zaps,” these sensations reflect abrupt serotonin fluctuations and are more common during erratic dosing.
-
Sleep disruptions: Insomnia, vivid dreams, or oversleeping may signal that the medication is being taken inconsistently.
-
Withdrawal-like rebound symptoms: Missing doses—even by a few hours for some individuals—can trigger flu-like feelings, dizziness, irritability, or sensory disturbances.
Emotional / Psychological Sign
-
Craving the emotional relief Cymbalta brings: Feeling unable to cope with stress or daily functioning without the medication.
-
Mood instability between doses: Irritability, sadness, or emotional volatility when a dose is late or missed.
-
Anxiety spikes: Heightened worry or panic related to timing, access to medication, or the possibility of running out.
-
Fear of tapering: A strong reluctance or panic at the idea of reducing the dosage, even under medical supervision.
-
Emotional blunting: Feeling disconnected, numb, or “flattened,” leading some individuals to increase their dose without approval.
-
Return of depression when adjusting doses: Rapid emotional decline during self-directed tapering attempts.
Behavioral Signs
-
Taking more than prescribed: Increasing the daily dose, hoping for faster emotional relief or stronger effects.
-
Frequent early refill requests: Running out early due to dose adjustments or using more capsules during stress.
-
Using Cymbalta to escape emotional pain: Relying on the medication as a coping tool rather than a medical treatment.
-
Avoiding travel, events, or routine activities: Fear of missing doses or being away from the medication.
-
Social withdrawal: Isolation or reduced engagement due to fatigue, emotional detachment, or sedation.
-
Declining daily functioning: Missing work, school, or home responsibilities because of Cymbalta-related side effects or sedation.
How Common Is It?
General Prevalence
Cymbalta is one of the more frequently prescribed antidepressants. In 2023, it ranked among the top 40 most-prescribed medications in the United States, with over 18 million prescriptions filled that year. [2]
Because of its wide use, a large number of people are exposed, which increases the absolute number of individuals who might experience withdrawal or discontinuation problems. But importantly, the fact that many people use it does not mean misuse or addiction is common.
Clinical Settings / Higher-Risk Populations
There’s no strong evidence that duloxetine is a drug of abuse in clinical settings. Pre-marketing data showed no signs of dependence or drug-seeking behavior. Post-marketing reports do show cases of withdrawal symptoms, and one analysis noted duloxetine among the antidepressants most often linked to “withdrawal syndrome.” [3]
Still, these reflect difficulties with tapering—not misuse or addiction. Most patients experiencing problems aren’t seeking Cymbalta recreationally; they’re dealing with discontinuation effects.
Withdrawal / Discontinuation Frequency
A recent (2025) meta-analysis of antidepressant discontinuation in randomized trials found that withdrawal or discontinuation symptoms after stopping antidepressants are often below the threshold for clinically significant withdrawal syndrome[4]. These symptoms — including dizziness, nausea, headache, or irritability — are classified as physiologic discontinuation effects, not true addictive withdrawal. Careful tapering can usually prevent or minimize these symptoms.
Causes: Why Does Cymbalta Misuse Happen?
Cymbalta (duloxetine) is not considered a classic addictive drug, but misuse can still develop. This usually happens when the emotional stability, pain relief, or anxiety reduction it provides becomes a psychological coping mechanism.
Neurobiology: How Cymbalta Affects the Brain?
Cymbalta acts as an SNRI (serotonin–norepinephrine reuptake inhibitor). It increases the availability of these neurotransmitters, helping the brain regulate:
-
emotional distress
-
physical pain signals
-
stress reactivity
-
energy and focus
-
mood stability
When used as prescribed, this leads to steadier emotional and physical functioning. But when doses shift unpredictably—or when a person depends heavily on Cymbalta for emotional grounding—the brain adapts to the medication’s constant presence.
Over time, the nervous system becomes accustomed to the artificial stability Cymbalta provides. If doses are taken late, increased without guidance, or stopped abruptly, the system may temporarily destabilize, leading to:
-
spikes of panic or anxiety
-
irritability or agitation
-
dizziness or vertigo
-
sensory disturbances (brain zaps, head pressure)
-
amplified pain symptoms
-
emotional flooding or tearfulness
These reactions are not “addiction.” They are signs of neurochemical readjustment—essentially the brain recalibrating after losing the medication it has come to rely on for balance.
For some individuals who are especially sensitive to serotonin or norepinephrine changes, this instability can make them fear missing doses and encourage misuse, such as taking extra medication for “just-in-case” emotional control.
Genetic & Biological Factors
Cymbalta misuse risk is influenced by biological vulnerability, not personal weakness. Factors that can increase susceptibility include:
-
family history of depression, anxiety, or substance-use disorders
-
variations in CYP1A2 or CYP2D6 metabolism (slower or faster breakdown can intensify effects) [5]
-
heightened sensitivity to serotonin/norepinephrine shifts
-
co-occurring conditions such as PTSD, panic disorder, generalized anxiety, chronic depression, or chronic pain
People with these vulnerabilities may find Cymbalta’s emotional or physical relief especially reinforcing. Over time, they may start relying on the medication more heavily during stress, leading to dose escalation or psychological dependence.
Psychological & Emotional Triggers
Much like with Buspar, Cymbalta misuse often begins as self-soothing, not recreational use. Individuals may start taking extra doses during moments of emotional overload, hoping for faster relief.
Common emotional triggers include:
-
using Cymbalta to escape intense stress
-
increasing dosage during emotional crises or panic episodes
-
leaning on Cymbalta to maintain day-to-day functioning
-
feeling unable to cope without the chemical stability it provides
This pattern often starts subtly:
Stress → extra Cymbalta dose → temporary relief → brain links medication with emotional safety.
Once relief becomes tied to the medication rather than to coping skills, emotional reliance can build—even if the individual follows most of their prescription rules.
Environmental & Social Factors
External pressures can quietly push someone toward Cymbalta misuse, especially when life becomes unmanageable.
Contributing factors include:
-
chronic workplace or caregiver stress
-
limited access to therapy or mental-health support
-
long-term physical pain leading to emotional exhaustion
-
financial strain or instability
-
isolation, relationship stress, or lack of social support
-
Inconsistent follow-up with healthcare providers
Many individuals also misunderstand Cymbalta as “totally safe” simply because it’s not an opioid or benzodiazepine. This misconception may lead to self-directed dose increases or keeping extra capsules on hand “just in case.”
From Pain or Anxiety Relief to Dependence (Progression)
For many people, misuse develops gradually and often unintentionally. It begins with genuine relief—less pain, calmer emotions, a sense of finally feeling normal.
Then life becomes stressful again:
-
The dose stops feeling as effective
-
emotional pressure rises
-
physical symptoms flare
-
Sleep quality worsens
-
everyday challenges accumulate
A person may take an extra capsule “just this once” to get through a difficult day. Then again, during a stressful week. Then it becomes a routine fallback.
Soon, missing a dose feels frightening—not because Cymbalta is addictive, but because the brain is now dependent on its chemical regulation.
This is not classic addiction. It is relief-seeking under pressure, amplified by neurochemical sensitivity and emotional strain.
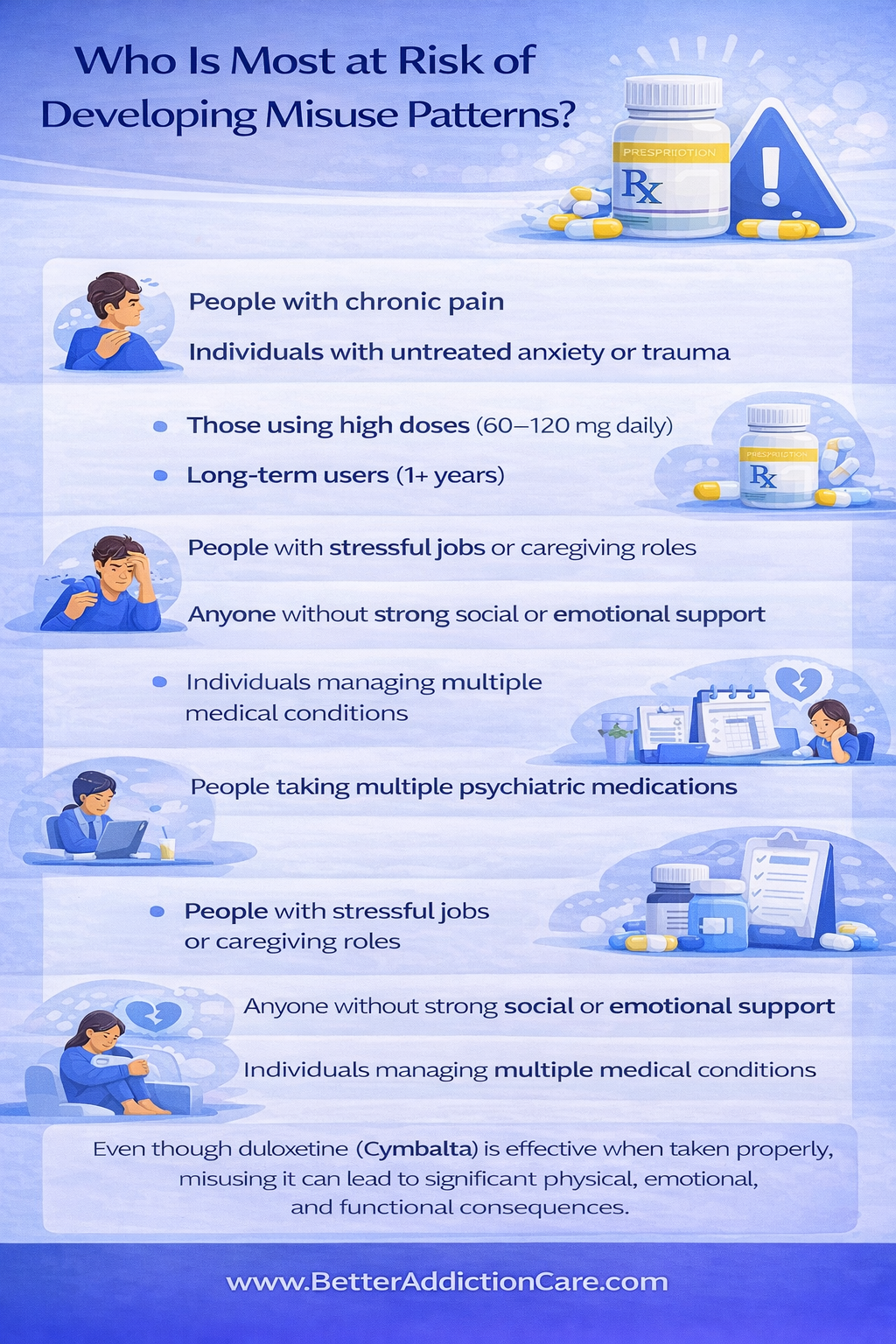
Who Is Most at Risk of Developing Misuse Patterns?
-
People with chronic pain
-
Individuals with untreated anxiety or trauma
-
Those using high doses (60–120 mg daily)
-
Long-term users (1+ years)
-
People with stressful jobs or caregiving roles
-
Anyone without strong social or emotional support
-
Individuals managing multiple medical conditions
-
People taking multiple psychiatric medications
Even though duloxetine (Cymbalta) is effective when taken properly, misusing it can lead to significant physical, emotional, and functional consequences.
Side Effects of Cymbalta Misuse
Short-Term Effects
-
Sedation, fatigue, or drowsiness: Especially when higher-than-prescribed doses are taken or mixed with other depressants.
-
Nausea, digestive upset, or stomach pain: Cymbalta’s gastrointestinal side effects intensify with misuse.
-
Agitation, restlessness, or shakiness: Some people experience jitteriness or a “wired” feeling.
-
Headaches and dizziness: These can impair judgment, coordination, and reaction time.
-
Appetite changes: Either increased hunger or loss of appetite.
-
Increased sweating or flushing: Due to overstimulation of the nervous system.
Long-Term Effects
-
Worsening depression or anxiety: Erratic, non-medical dosing can destabilize mood and worsen symptoms.
-
Persistent sexual dysfunction: Low libido, difficulty achieving orgasm, or erectile dysfunction may become long-lasting.
-
Elevated blood pressure: Especially concerning in those with cardiovascular risk.
-
Weight fluctuations: Due to appetite disruption and metabolic changes.
-
Liver strain or damage: Risk is significantly higher when combined with alcohol.
-
Emotional blunting: Feeling detached, numb, or unable to fully experience emotions.
-
Tapering difficulties: Misuse increases the likelihood of severe withdrawal symptoms.
-
Dependence-like patterns: Psychological reliance on the medication’s effects.
Impact on Daily Life
-
Decline in work or school performance due to fatigue, poor concentration, or emotional instability.
-
Missed deadlines and reduced productivity from inconsistent functioning.
-
Memory or attention problems that interfere with tasks and decision-making.
-
Avoidance of social activities because of mood changes or side effects.
-
Relationship tension caused by irritability, withdrawal, or emotional flatness.
-
Feeling disconnected or “not yourself” due to emotional numbness.
-
Financial strain from repeated medical consultations or unnecessary dose adjustments.
-
Lower physical activity levels because of dizziness, fatigue, or body aches.
Treatment Options for Cymbalta Misuse
Recovery from Cymbalta misuse looks different for every person. Factors such as duration of use, current dose, past antidepressant trials, co-occurring anxiety or chronic pain, trauma history, and overall emotional resilience all influence the tapering strategy.
A good treatment plan is collaborative—not prescriptive—so the individual feels heard, supported, and never rushed or dismissed. Tailoring the approach improves comfort, safety, and long-term stability.
Detox / Withdrawal Management
Setting Options
-
Outpatient Care: Most people taper duloxetine safely at home with consistent medical supervision.
-
Inpatient or Residential Care: Recommended when withdrawal symptoms are severe, when there is polydrug use, or when someone has co-occurring mental health conditions that make home management difficult.
Supports During Detox
-
Gradual tapering schedules (4–12+ weeks): Slow dose reductions significantly reduce “brain zaps,” dizziness, anxiety spikes, or GI symptoms.
-
Cross-tapering to fluoxetine (“Prozac bridge”): Helps buffer withdrawal because it has a long half-life and smoother discontinuation profile.
-
Adjunct medications:
-
Anti-nausea meds for GI distress
-
Hydroxyzine or buspirone for anxiety
-
Beta-blockers for severe agitation or palpitations
-
Sleep supports (melatonin, trazodone, or non-habit-forming aids)
-
Monitoring: Regular checks of blood pressure, sleep patterns, mood fluctuations, and return of pain symptoms.
Avoiding cold-turkey discontinuation is crucial—most severe Cymbalta withdrawal cases result from sudden stopping. [1]
Medication-Assisted Approaches (Supportive, Not Substitutive)
Cymbalta is not addictive in the classic sense, so typical addiction MAT (methadone, buprenorphine, naltrexone) is not used for duloxetine misuse.
However, physicians may support stabilization using:
-
Fluoxetine bridging to smooth withdrawals.
-
Short-term, non-benzodiazepine anxiolytics to manage taper-related anxiety.
-
Pain management medications to address flare-ups in fibromyalgia or neuropathic pain during dose reductions.
-
Switching to an alternative antidepressant if depression or anxiety resurges.
These strategies help reduce discomfort and maintain emotional stability during and after tapering.
Levels of Care
-
Inpatient/Residential Treatment (30–90 days): Offers 24/7 monitoring, structured routines, daily therapy, and safe medication management.
-
Partial Hospitalization Program (PHP): Full-day treatment with skills groups, medical oversight, and intensive therapy while allowing the individual to sleep at home.
-
Intensive Outpatient Program (IOP): Multiple therapy sessions per week, combining group therapy, individual counseling, and medication management.
-
Standard Outpatient Care: Regular appointments with a psychiatrist, therapist, or both—ideal for mild to moderate withdrawal and long-term recovery.
Therapies (Core Supports for Stability)
-
Cognitive Behavioral Therapy (CBT): Helps build coping skills and reduce reliance on medication for mood regulation.
-
Acceptance & Commitment Therapy (ACT): Especially helpful for chronic pain or generalized anxiety.
-
Motivational Interviewing (MI): Strengthens confidence and reduces fear around tapering.
-
Trauma-Focused Therapies: EMDR or trauma-informed CBT when PTSD or unresolved trauma contributes to misuse.
-
Family Therapy: Improves communication, reduces conflict, and brings loved ones into the recovery plan.
-
Pain-Focused Therapy: Teaches strategies for managing flare-ups without returning to higher Cymbalta doses.
Peer Support & Recovery Capital
-
SMART Recovery, Refuge Recovery, or anxiety-focused groups for people who prefer non-12-step options.
-
Peer mentors who offer shared lived experience and practical support.
-
Faith-based or community-based groups that provide a sense of belonging.
-
Recovery-friendly workplaces with flexible policies.
-
Family education so loved ones understand withdrawal and provide healthy support.
Recovery capital means strengthening both internal resources (resilience, coping skills, motivation) and external supports (family, community, stability) so long-term recovery is sustainable.
Holistic Supports (Adjunct Tools to Strengthen Recovery)
-
Gentle exercise, such as walking, yoga, or pilates, to regulate mood and reduce tension.
-
Anti-inflammatory or balanced nutrition to support brain and gut health.
-
Mindfulness, grounding, or meditation practices to calm the nervous system.
-
Sleep hygiene optimization: consistent sleep schedule, reduced screen time, supportive nighttime routine.
-
Physical therapy, stretching, or heat therapy for those tapering off Cymbalta due to chronic pain issues.
-
Routine-building to restore predictability during emotional ups and downs.
-
Journaling or reflective writing for emotional processing.
-
Breathwork and relaxation exercises to manage anxiety surges.
These holistic tools don’t replace medical care—but they significantly improve resilience and make recovery smoother and more comfortable.
Withdrawal Timeline — What to Expect When Stopping Cymbalta?
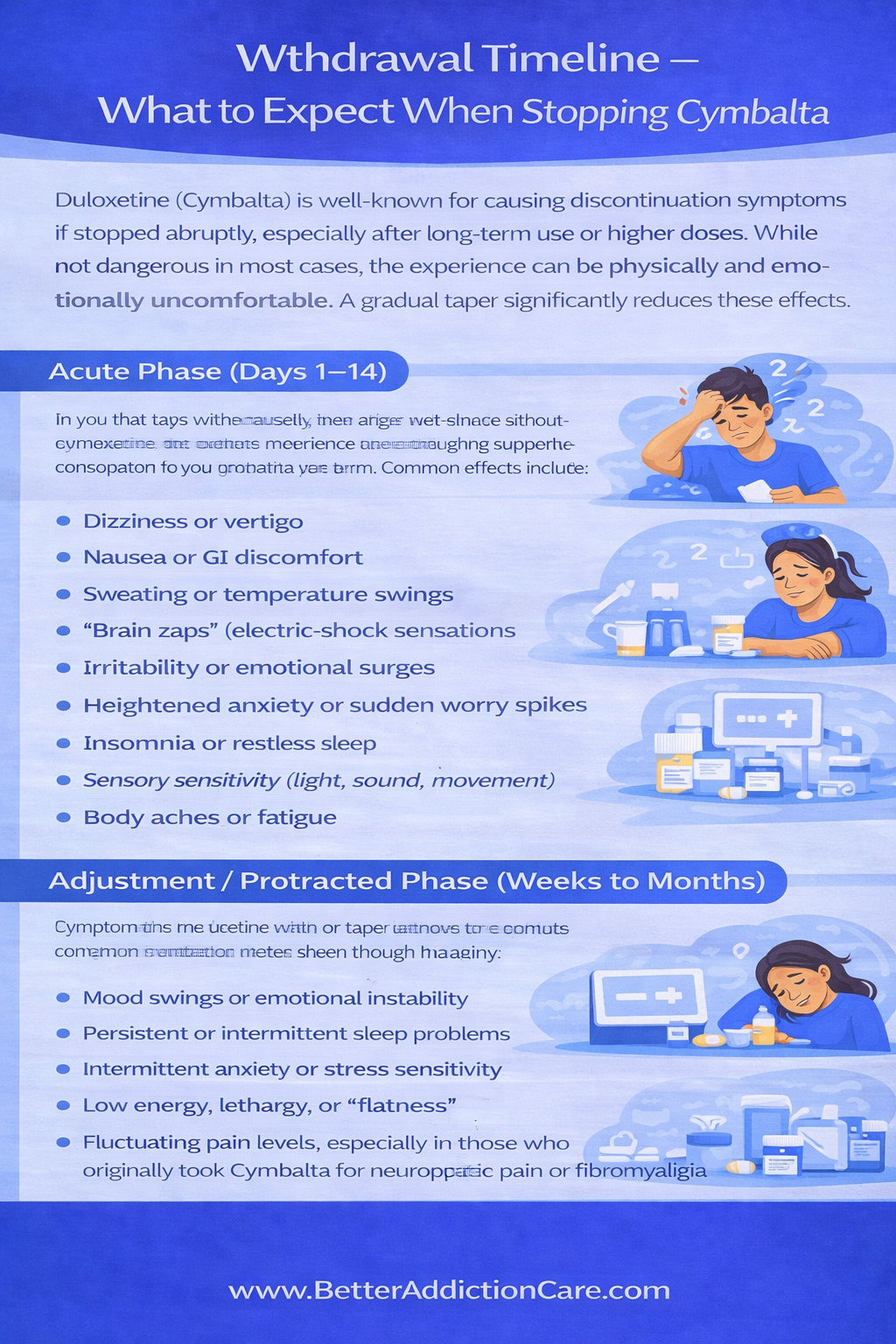
Duloxetine (Cymbalta) is well-known for causing discontinuation symptoms if stopped abruptly, especially after long-term use or higher doses. While not dangerous in most cases, the experience can be physically and emotionally uncomfortable. A gradual taper significantly reduces these effects.
Acute Phase (Days 1–14)
In the first days to two weeks after dose reduction or abrupt cessation, many people experience a cluster of neurological and physical symptoms as serotonin-norepinephrine levels shift. Common effects include:
-
Dizziness or vertigo
-
Nausea or GI discomfort
-
Sweating or temperature swings
-
“Brain zaps” (electric-shock sensations)
-
Irritability or emotional surges
-
Heightened anxiety or sudden worry spikes
-
Insomnia or restless sleep
-
Sensory sensitivity (light, sound, movement)
-
Body aches or fatigue
These symptoms are typically reversible and tend to peak within the first week. Supportive care, slow tapering, and short-term symptomatic medications often help significantly.
Adjustment / Protracted Phase (Weeks to Months)
A smaller subset of people experience lingering discontinuation effects as the nervous system rebalances. These may include:
-
Mood swings or emotional instability
-
Persistent or intermittent sleep problems
-
Intermittent anxiety or stress sensitivity
-
Low energy, lethargy, or “flatness.”
-
Fluctuating pain levels, especially in those who originally took Cymbalta for neuropathic pain or fibromyalgia
These symptoms do not indicate permanent damage. They reflect the brain’s gradual recalibration of serotonin and norepinephrine pathways.
Stabilization Phase (1–3+ Months)
Most patients return to baseline over the following months with the help of:
-
a slow, personalized tapering plan,
-
psychotherapy,
-
routine-building, and
-
adjunct medications for sleep, anxiety, or nausea.
Cravings or compulsive urges for Cymbalta are uncommon, since it is not habit-forming in a classical sense. Emotional stability typically improves as the individual adopts alternative coping strategies and the brain’s chemical balance normalizes.
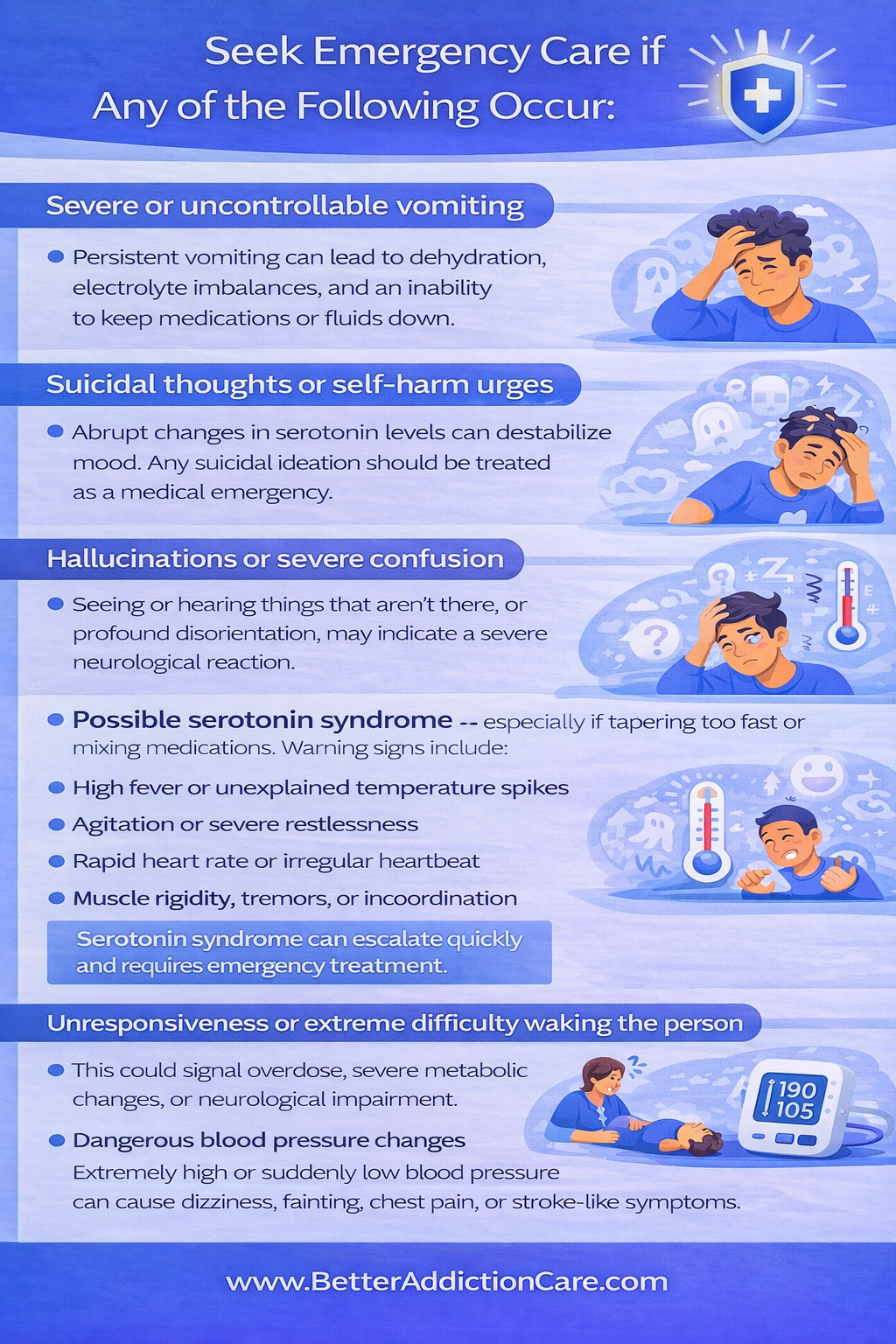
When to Seek Immediate Help?
While most Cymbalta withdrawal symptoms are uncomfortable rather than dangerous, certain red flags require urgent medical attention. These signs may indicate a severe reaction, a medical complication, or an emerging mental-health crisis.
Seek emergency care if any of the following occur:
-
Severe or uncontrollable vomiting: Persistent vomiting can lead to dehydration, electrolyte imbalances, and an inability to keep medications or fluids down.
-
Suicidal thoughts or self-harm urges: Abrupt changes in serotonin levels can destabilize mood. Any suicidal ideation should be treated as a medical emergency.
-
Hallucinations or severe confusion: Seeing or hearing things that aren’t there, or profound disorientation, may indicate a severe neurological reaction.
-
Possible serotonin syndrome — especially if tapering too fast or mixing medications. Warning signs include:
-
High fever or unexplained temperature spikes
-
Agitation or severe restlessness
-
Rapid heart rate or irregular heartbeat
-
Muscle rigidity, tremors, or incoordination
-
Confusion, delirium, or dramatic mental status changes
Serotonin syndrome can escalate quickly and requires emergency treatment.
-
Unresponsiveness or extreme difficulty waking the person: This could signal overdose, severe metabolic changes, or neurological impairment.
-
Dangerous blood pressure changes: Extremely high or suddenly low blood pressure can cause dizziness, fainting, chest pain, or stroke-like symptoms.
Emergency Steps
If any of the above symptoms appear:
-
Contact local emergency services immediately (ambulance, ER, or your country’s emergency hotline).
-
Bring a full medication history, including:
-
Current Cymbalta dose
-
Taper schedule (if applicable)
-
All other medications, supplements, or substances
-
Recent dose changes or missed doses
-
Do not attempt to self-manage severe reactions at home. Rapid medical evaluation is critical.
Dosing & Safety / Overdose Risks
Typical Prescribing Ranges
-
30 mg daily (starting dose)
-
60 mg daily (therapeutic dose)
-
Up to 120 mg daily in select cases
High-Risk Combinations
-
Benzodiazepines
-
Opioids
-
Other serotonergic medications
-
Illicit substances
-
Stimulants
These combinations increase sedation, blood pressure changes, or serotonin syndrome risk.
Overdose Mechanism
Cymbalta overdose primarily affects:
-
cardiovascular system
-
central nervous system
-
serotonin levels
Symptoms may include agitation, confusion, nausea, rapid heart rate, or high blood pressure.
Safe Use Practices
-
Do not adjust the dose without medical guidance
-
Store medication securely
-
Never share prescriptions
-
Follow taper plans carefully
-
Track mood, pain, and sleep changes
-
Attend regular follow-ups
Conclusion
Cymbalta helps thousands of people reclaim their lives from pain and anxiety. But when relief becomes dependence-like patterns or withdrawal begins interfering with daily functioning, it’s important to recognize the signs early and seek support.
Misuse or difficulty stopping Cymbalta does not mean someone is “addicted,” broken, or weak. It means their nervous system has adapted to a medication that deeply affects mood, pain perception, and energy regulation.
The good news is that stabilization is absolutely achievable. With supervised tapering, therapeutic support, medical guidance, and steady lifestyle reinforcement, individuals feel like themselves again. Families regain clarity. Stress eases. Life becomes manageable.
If you or someone you care about is struggling, the next step is simple: schedule a professional assessment. A personalized plan—detox, tapering, therapy, and support—can make the process smoother and safer.
Relief is possible. Healing is possible. And no one has to go through it alone.
FAQs
Not in the traditional sense. Cymbalta isn’t considered chemically addictive like opioids or benzodiazepines. However, some people may develop emotional reliance, experience withdrawal discomfort, or feel the need to increase the dose, which can resemble dependence.
Serious risks may include:
- Severe withdrawal symptoms
- Elevated blood pressure
- Serotonin syndrome (rare but dangerous)
- Emotional or mood destabilization
Yes. It’s common for anxiety, depression, or pain to return during tapering. This does not mean treatment failed — it often indicates that the taper is too fast and needs a slower, more gradual approach.
Usually not. Cymbalta is known for difficult, sometimes severe withdrawal. Most people do best with a slow, medically supervised taper to minimize symptoms.
Families can help by:
- Listening without judgment
- Educating themselves about discontinuation
- Encouraging medical guidance
- Helping maintain structure and routine
- Offering emotional support and safety
Withdrawal is rarely life-threatening, but symptoms can be intense, disorienting, and emotionally destabilizing. Severe mental health symptoms — such as suicidal thoughts, hallucinations, or extreme agitation — require immediate medical help.
Resources
Related Articles
Treatment Centers in New Jersey










