Duloxetine Interactions: What Not To Eat, Take, or Drink
Alcohol is one of the most common and underestimated risks for people taking duloxetine.
Both substances affect the CNS, but in different directions. Duloxetine stabilizes neurotransmitter signaling, while alcohol disrupts it. When combined, the result can feel unpredictable — sometimes numbing, sometimes overwhelming.

If you’re taking duloxetine, you’re likely doing so because life already feels heavy. Depression may have drained motivation, anxiety may have made everyday decisions exhausting, or chronic pain may have reshaped how your body feels each morning.
When a medication becomes part of that picture, one of the first questions people quietly ask is: “What could make this worse?” That concern is valid.
What Is Duloxetine?
Duloxetine is a prescription medication classified as a serotonin-norepinephrine reuptake inhibitor (SNRI). SNRIs work by increasing the availability of two neurotransmitters — serotonin and norepinephrine — which help regulate mood, emotional processing, and pain signaling.
It is commonly prescribed for:
-
Major depressive disorder
-
Chronic musculoskeletal pain
-
Diabetic nerve pain
-
Fibromyalgia
Unlike short-acting medications that primarily sedate, duloxetine works gradually by influencing brain signaling pathways involved in emotional regulation and pain perception. Because of this broad effect, it interacts with more systems than people often expect.
People around may notice that when duloxetine works well, emotional responses become steadier, pain flares become less overwhelming, and daily functioning improves. When interactions occur, those same gains can erode quickly.
How Duloxetine Affects the Central Nervous System?
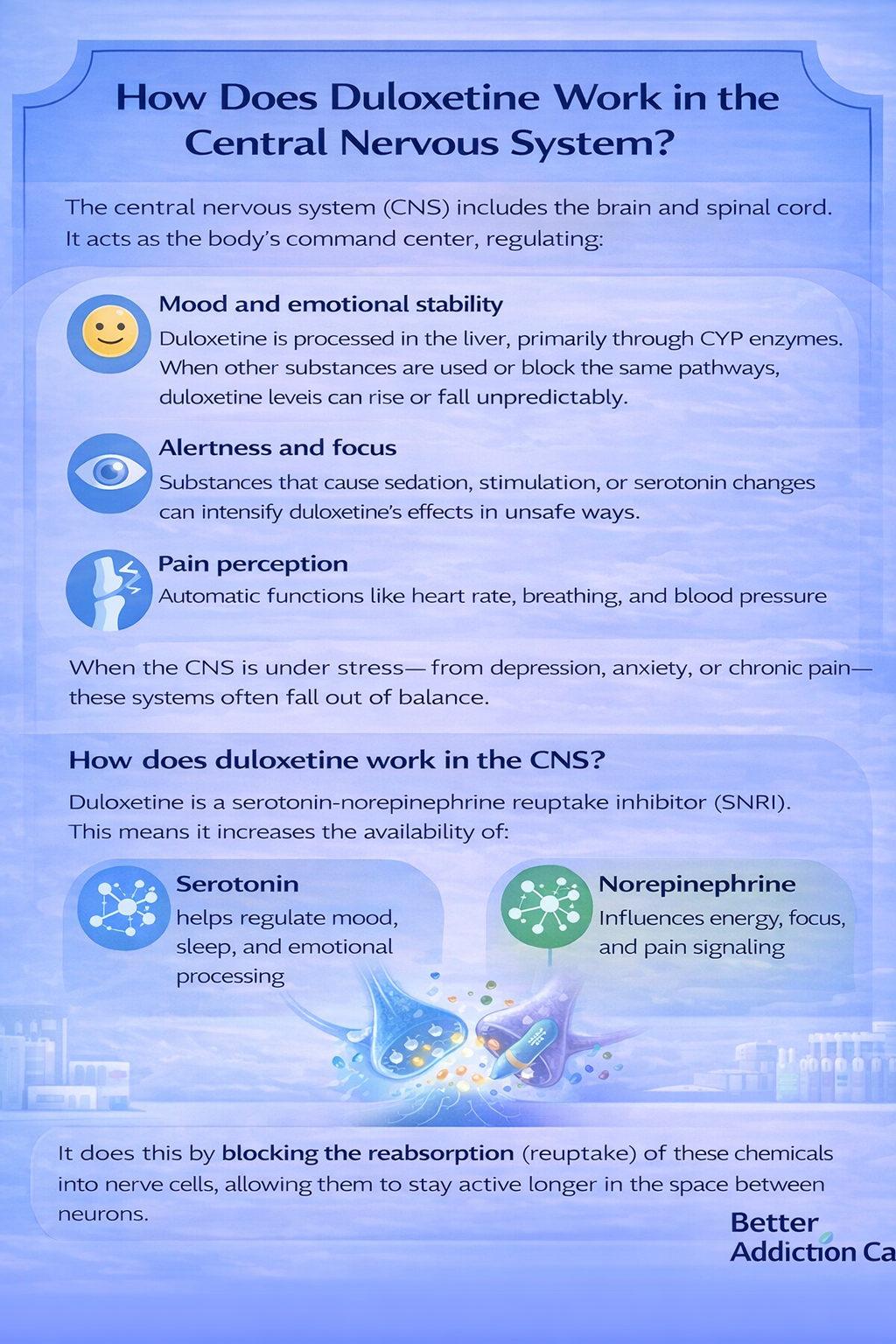
The central nervous system (CNS) includes the brain and spinal cord. It acts as the body’s command center, regulating:
-
Mood and emotional stability
-
Alertness and focus
-
Pain perception
-
Automatic functions like heart rate, breathing, and blood pressure
When the CNS is under stress — from depression, anxiety, or chronic pain — these systems often fall out of balance.
How does duloxetine work in the CNS?
Duloxetine is a serotonin-norepinephrine reuptake inhibitor (SNRI). This means it increases the availability of:
-
Serotonin, which helps regulate mood, sleep, and emotional processing
-
Norepinephrine, which influences energy, focus, and pain signaling
It does this by blocking the reabsorption (reuptake) of these chemicals into nerve cells, allowing them to stay active longer in the space between neurons.
A helpful analogy: it’s like stabilizing the volume on a radio station that used to fade in and out unpredictably.
Why does this makes interactions more likely?
Because duloxetine directly changes neurotransmitter balance, the CNS becomes more sensitive to other substances that:
-
Increase or decrease serotonin
-
Stimulate or depress nervous system activity
-
Affect alertness, coordination, or breathing
When multiple substances act on the same systems, effects don’t simply stack — they can amplify each other. This is why interactions may lead to:
-
Sudden drowsiness or agitation
-
Confusion or slowed reaction time
-
Emotional blunting or heightened anxiety
Why Drug and Alcohol Interactions Occur?
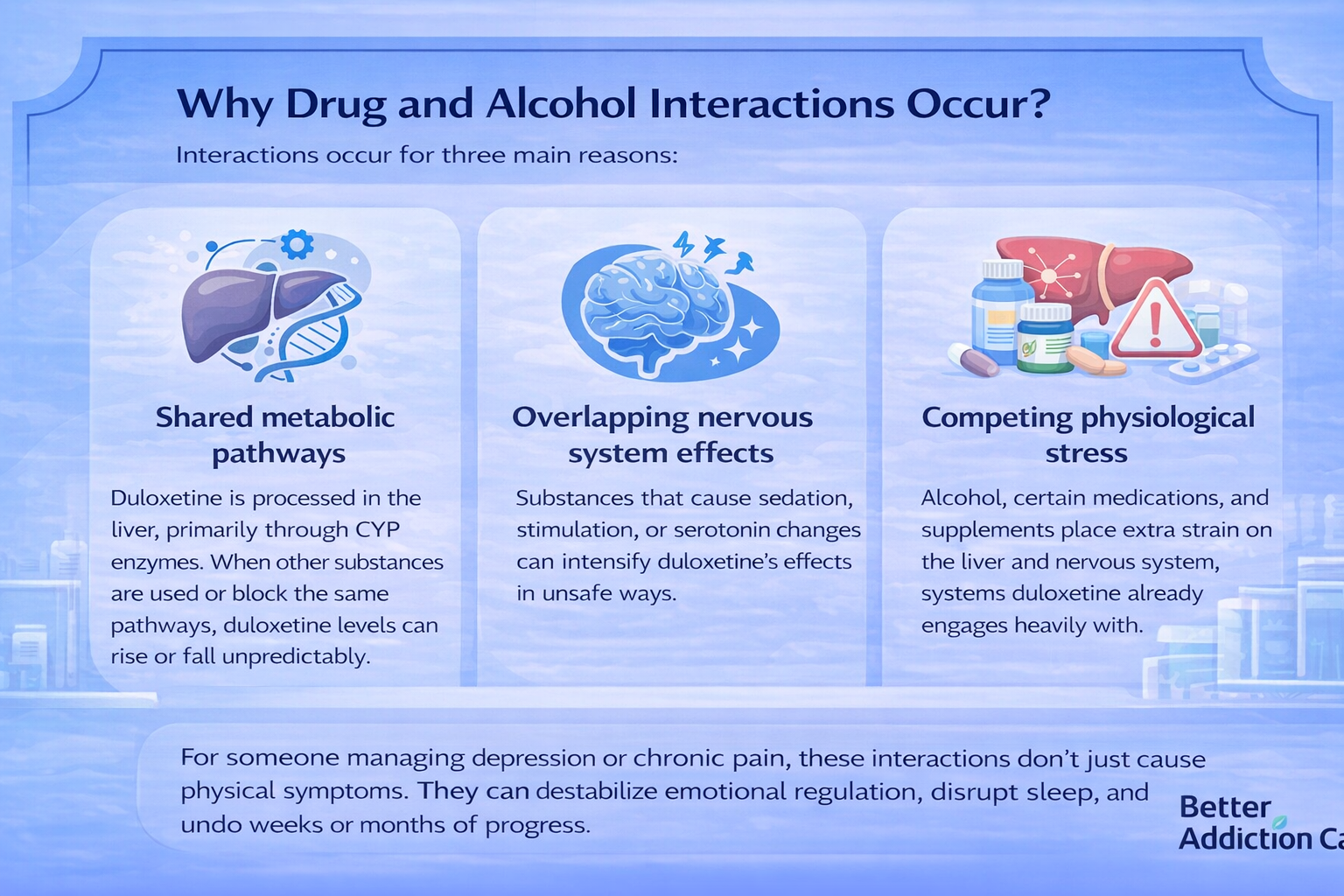
Interactions occur for three main reasons:
-
Shared metabolic pathways
Duloxetine is processed in the liver, primarily through CYP enzymes. When other substances are used or block the same pathways, duloxetine levels can rise or fall unpredictably. -
Overlapping nervous system effects
Substances that cause sedation, stimulation, or serotonin changes can intensify duloxetine’s effects in unsafe ways. -
Competing physiological stress
Alcohol, certain medications, and supplements place extra strain on the liver and nervous system, systems duloxetine already engages heavily with.
For someone managing depression or chronic pain, these interactions don’t just cause physical symptoms. They can destabilize emotional regulation, disrupt sleep, and undo weeks or months of progress.
Duloxetine and Alcohol Interactions
Alcohol is one of the most common and underestimated risks for people taking duloxetine.
Both substances affect the CNS, but in different directions.
Duloxetine stabilizes neurotransmitter signaling, while alcohol disrupts it. When combined, the result can feel unpredictable — sometimes numbing, sometimes overwhelming.
Factors that increase risk
Interaction risks rise when any of the following are present:
-
Regular alcohol use, especially more than 2–3 times per week
-
Higher duloxetine doses, which place a greater demand on liver metabolism
-
Existing liver stress, fatigue, or other medical conditions
Even people who previously tolerated alcohol well may notice stronger effects once duloxetine is added.
Possible effects of combining alcohol with duloxetine
This combination may lead to:
-
Increased dizziness and poor coordination (raising fall or accident risk)
-
Emotional blunting, irritability, or mood swings
-
Worsening depression or anxiety symptoms rather than relief
-
Elevated liver enzyme levels, indicating increased liver strain
What families often notice first?
From a family perspective, interaction effects may show up as:
-
Sudden fatigue after small amounts of alcohol
-
Withdrawal from conversation or social activities
-
Noticeable mood changes that feel “out of character.”
These changes are not personal failings or lack of effort — they are neurochemical responses to competing substances.
Clinical guidance
Most clinical guidance recommends avoiding alcohol entirely while taking duloxetine, especially during the first 6–8 weeks of treatment when the brain and nervous system are still adapting to the medication[1].
Avoidance helps protect early progress and reduces the risk of destabilizing side effects.
Prescription Drug Interactions With Duloxetine
Certain prescription medications carry higher interaction risks due to how they affect serotonin, blood pressure, or sedation.
Medications That Increase Serotonin
Combining duloxetine with other serotonin-increasing drugs can lead to serotonin syndrome, a potentially dangerous condition caused by excessive serotonin activity.
This may include:
-
Other antidepressants
-
Certain migraine medications
-
Some pain medications
Symptoms can range from agitation and sweating to confusion and muscle rigidity.
Sedatives and Nervous System Depressants
Medications that slow the CNS can intensify duloxetine-related side effects, such as:
-
Drowsiness
-
Slowed reaction time
-
Impaired judgment
This overlap raises accident and fall risk, especially in adults over 50.
Blood Pressure and Heart-Related Medications
Duloxetine can slightly raise blood pressure in some individuals.
When combined with medications that also influence cardiovascular function, monitoring becomes essential.
Families often notice this as headaches, restlessness, or increased fatigue — signs that should prompt a medication review rather than self-adjustment.
Over-the-Counter Medication Interactions
Over-the-counter medications are often viewed as “safe” because they don’t require a prescription. That assumption makes interaction risks easy to overlook — especially for people taking duloxetine, where even common products can interfere with nervous system balance.
Cold and Flu Products
Many cold and flu remedies contain ingredients that:
-
Influence serotonin activity
-
Stimulate the nervous system
-
Raise heart rate or blood pressure
When combined with duloxetine, these products may increase:
-
Restlessness or jitteriness
-
Heart-rate changes or palpitations
-
Sleep disruption or nighttime anxiety
These effects are more likely when multiple cold products are taken together or used for several days in a row.
Antihistamines and Sleep Aids
Antihistamines and non-prescription sleep aids often cause sedation on their own. When paired with duloxetine, they can intensify nervous system slowing, leading to:
-
Brain fog and difficulty concentrating
-
Delayed reaction times, affecting driving or work tasks
-
Increased fall risk, especially at night or in older adults
For someone already managing depression, anxiety, or chronic pain, this added cognitive fog can feel discouraging.
Many people describe it as feeling like they’ve “slid backward,” even though the issue is not the medication failing — it’s an interaction altering how the CNS functions.
Duloxetine and Recreational or Non-Prescribed Substances
Recreational or non-prescribed substances interact with duloxetine in ways that are often unpredictable and harder to reverse than prescription interactions. Because these substances are not taken under medical supervision, changes in dose, timing, or potency can quickly destabilize the nervous system.
Cannabis
Some people use cannabis to cope with pain, sleep problems, or anxiety. However, when combined with duloxetine, cannabis may:
-
Increase dissociation (feeling detached from thoughts or surroundings)
-
Trigger anxiety spikes or panic-like symptoms
-
Worsen attention and concentration problems
Because cannabis can dull awareness of internal warning signals, the combination may mask early signs that duloxetine is no longer feeling stable or well-tolerated.
Illicit or Non-Prescribed Substances
Substances that strongly affect serotonin, dopamine, or overall CNS activity pose a much higher risk when combined with duloxetine. Potential consequences include:
-
Sudden mood destabilization
-
Agitation or emotional volatility
-
Cardiovascular stress, such as heart-rate or blood-pressure changes[2]
These reactions can escalate quickly and may require medical intervention. For individuals with a history of substance misuse, these combinations are particularly risky — not because of moral failure, but because neurochemical systems are already more sensitive.
Who Is at Higher Risk From Interactions?
Certain groups face an elevated risk of duloxetine interactions:
-
Adults over 60 – Age-related changes in metabolism can make the body slower to clear medications, increasing side effect likelihood.
-
People taking multiple medications – Combining duloxetine with other prescriptions or supplements raises the chance of harmful drug–drug interactions.
-
Individuals with liver conditions – Since duloxetine is metabolized in the liver, pre-existing liver issues can lead to higher drug levels and toxicity.
-
Those with a history of substance misuse – Prior substance use can make the nervous system more sensitive, increasing the risk of adverse reactions or misuse.
-
People in the early weeks of duloxetine treatment – The body is adjusting to the medication, making interactions and side effects more noticeable during this period.
People often spot warning signs first, such as confusion, unsteadiness, unusual fatigue, or emotional flattening, even before the person taking the medication recognizes a link to interactions. Early observation can help prevent complications by alerting healthcare providers promptly.
Common Side Effects That May Worsen With Interactions
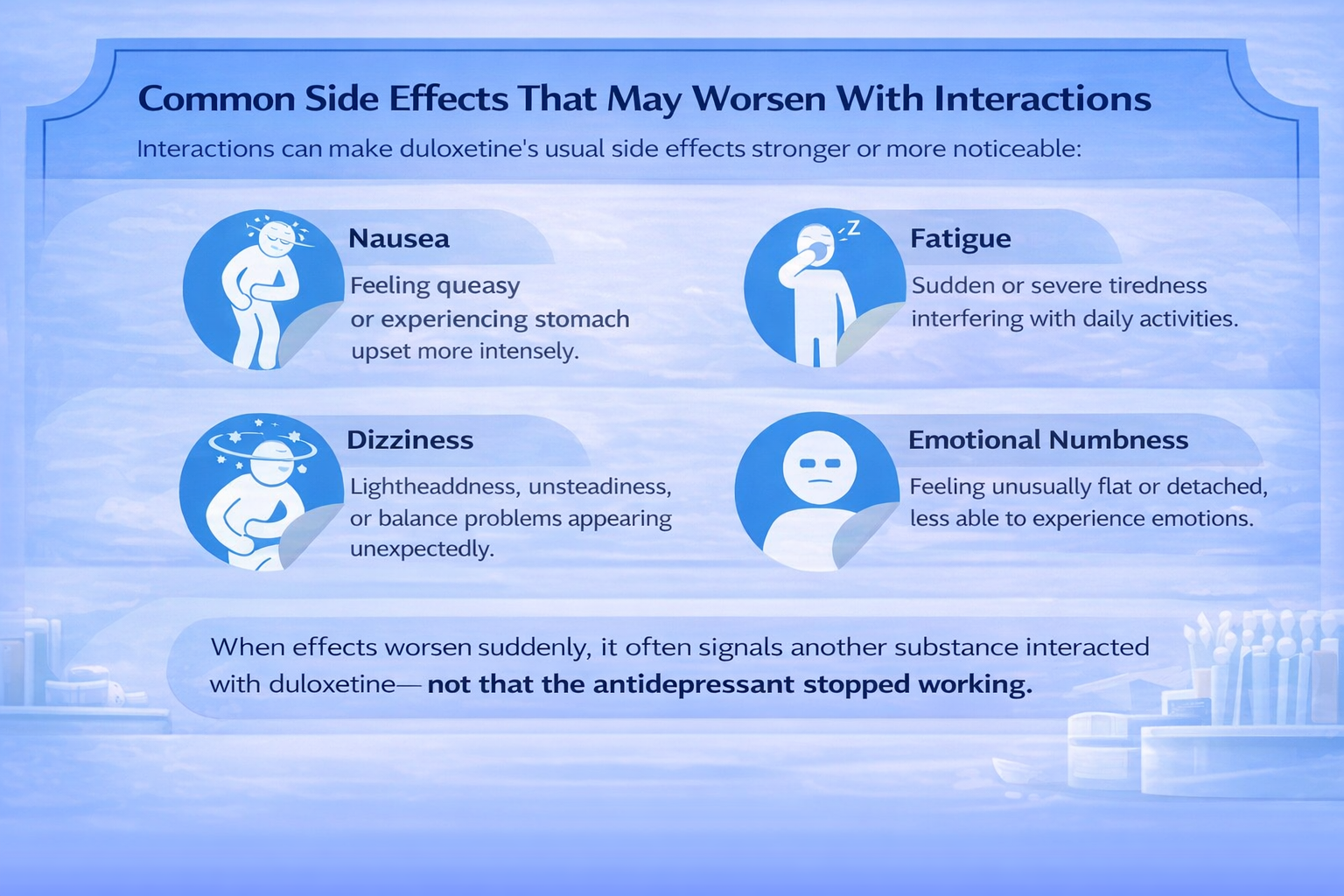
Interactions can make duloxetine’s usual side effects stronger or more noticeable:
-
Nausea – Feeling queasy or experiencing stomach upset more intensely than usual.
-
Fatigue – Sudden or severe tiredness that interferes with daily activities.
-
Dizziness – Lightheadedness, unsteadiness, or balance problems that appear unexpectedly.
-
Emotional numbness – Feeling unusually flat, detached, or less able to experience emotions.
When these effects worsen suddenly, it often indicates that another substance, food, or medication is interacting with duloxetine — not that the antidepressant has “stopped working.”
Recognizing these signs early allows for adjusting treatment safely before more serious complications develop.
Warning Signs of a Dangerous Interaction
Seek urgent medical attention if any of these appear:
-
Severe confusion or agitation – Sudden disorientation, restlessness, or unusual behavior changes.
-
Rapid heart rate – Palpitations or heartbeat that feels unusually fast or irregular.
-
High fever or heavy sweating – Body temperature spikes or drenching sweat without an obvious cause.
-
Muscle rigidity or tremors – Stiff muscles, shaking, or involuntary movements that appear quickly.
-
Fainting or loss of coordination – Dizziness leading to falls or inability to move safely.
These are escalation signals, not minor inconveniences. Prompt action can prevent serious complications and protect the nervous system.
Safe Use and Risk-Reduction Guidelines
Practical steps to reduce interaction risk and maintain stability:
-
Keep a complete medication list – Include prescription drugs, over-the-counter meds, and supplements.
-
Avoid alcohol – Especially during the first weeks of duloxetine treatment, as it can amplify side effects.
-
Introduce new medications one at a time – Allows the body and healthcare providers to monitor for reactions.
-
Report mood or physical changes promptly – Early reporting of nausea, dizziness, or emotional changes can prevent serious issues.
Families can support safety by tracking changes, encouraging open communication, and noting patterns, rather than assuming side effects are “normal” or temporary.
Duloxetine and Dependency or Misuse Considerations
Duloxetine is not considered addictive in the way opioids or benzodiazepines are. However, abrupt stopping, skipping doses, or misusing the medication can trigger withdrawal-like symptoms, including:
-
Dizziness or lightheadedness – Feeling unsteady or off-balance unexpectedly.
-
Irritability or mood swings – Sudden frustration, agitation, or emotional sensitivity.
-
“Brain zaps” – Brief, electric-shock sensations in the head, often occurring when doses are missed or stopped abruptly.
For individuals in addiction recovery, the primary concern isn’t craving duloxetine itself — it’s the destabilization of mental health or mood, which can increase relapse risk if not monitored.
Risk reduction strategies include:
-
Gradually tapering doses under medical supervision rather than stopping suddenly.
-
Maintaining consistent dosing schedules.
-
Regular check-ins with healthcare providers to track mood, sleep, and physical side effects.
-
Families observing changes in behavior or mood and reporting them promptly.
With careful monitoring and professional guidance, the risks of misuse or destabilization are significantly minimized, making duloxetine a safe tool for treating depression, anxiety, or neuropathic pain in most adults[3].
When to Speak With a Doctor or Specialist?
Professional input is essential if:
-
You’re prescribed a new medication
-
Alcohol use feels difficult to stop
-
Side effects escalate suddenly
-
Emotional stability declines
Asking for help is not a setback — it’s a protective decision.
Final Takeaway
Duloxetine can be highly effective for managing depression, anxiety, and chronic pain, but its benefits are best preserved when interactions are recognized and avoided.
Being informed about what not to eat, drink, or combine with the medication — and tracking changes in mood, energy, or physical symptoms — empowers both individuals and families to maintain stability.
Proactive risk management, open communication with healthcare providers, and careful monitoring help prevent complications, protect progress, and ensure duloxetine remains a safe, reliable part of recovery and daily life.
Stability is built through informed choices, not perfection.
FAQs
No. Alcohol increases the risk of liver strain, dizziness, emotional instability, and worsening depression when combined with duloxetine. These risks are higher during the first 6–8 weeks of treatment and with regular alcohol use. Even small amounts can interfere with how stable the medication feels day to day.
There are no specific foods that must be avoided. However, large amounts of caffeine or energy drinks may worsen anxiety, sleep disruption, or jitteriness in some people taking duloxetine. Paying attention to how your body responds is more helpful than following rigid food rules.
Yes. Many cold, flu, and allergy products contain ingredients that affect the nervous system or blood pressure. When combined with duloxetine, they may increase dizziness, restlessness, or heart-rate changes. Always check labels or ask a pharmacist before using OTC products.
Not always. Some supplements influence serotonin levels or liver metabolism, which can increase side-effect risk when combined with duloxetine. Supplements should be treated like medications — discuss them with a healthcare professional before starting.
Seek urgent medical care for symptoms such as severe confusion, agitation, rapid heart rate, heavy sweating, muscle stiffness, or fainting. These may indicate a serious reaction and should not be ignored.
Do not panic or stop duloxetine abruptly. Contact your prescribing provider or a medical professional as soon as possible, especially if symptoms are worsening. Many interaction effects improve once the other substance clears, but guidance helps prevent complications.
Yes, many people use duloxetine safely for months or years under medical supervision. Avoiding high-risk interactions and monitoring changes early helps maintain emotional and physical stability over time.







