Cymbalta Withdrawal: Symptoms, Timeline, and Tips for Quitting
Stopping Cymbalta (duloxetine) can be overwhelming for the person taking it and for their family. Many people are told it’s “Easy to stop,” only to feel unprepared when symptoms appear.
This page is designed to explain what happens, why it happens, and how Cymbalta can be stopped safely, gradually, and with realistic hope, using evidence-based guidance.
Key Takeaways
-
Is Cymbalta withdrawal real?
Yes. Cymbalta withdrawal, clinically called antidepressant discontinuation syndrome, is well-documented and temporary, though symptoms can feel intense without proper tapering and support[1]. -
What is the safest way to stop Cymbalta?
Gradual dose reduction under medical supervision is consistently associated with fewer and milder withdrawal symptoms compared to stopping abruptly [2]. -
What helps recovery most?
A combination of slow tapering, symptom monitoring, lifestyle stabilization, and family support helps the nervous system rebalance and reduces fear-driven setbacks.
What Happens When You Stop Taking Cymbalta?
Cymbalta (duloxetine) is a serotonin–norepinephrine reuptake inhibitor (SNRI), a medication that increases the availability of serotonin and norepinephrine, chemicals involved in mood regulation, pain perception, and stress response.
When someone takes Cymbalta daily, the brain adapts to this altered chemical environment. Specifically, areas such as the prefrontal cortex (the brain’s planning and emotional regulation center) adjust how receptors respond to these neurotransmitters.
When Cymbalta is reduced too quickly or stopped suddenly, the brain does not immediately return to its pre-medication state. Instead, it enters a temporary imbalance, leading to withdrawal symptoms.
It’s important for families to understand:
-
Withdrawal is not relapse. Withdrawal symptoms often appear quickly after dose changes and improve with time.
-
Withdrawal is not addiction. There are no drug cravings or compulsive drug-seeking behaviors, only physiological readjustment.
-
Your loved one is not “going backwards.” Their nervous system is recalibrating, much like a thermostat being reset gradually rather than abruptly.
What Are the Common Symptoms of Cymbalta Withdrawal?

Withdrawal symptoms vary depending on dose, duration of use, taper speed, and individual sensitivity. Organizing symptoms by category helps families recognize what is happening and respond with reassurance rather than alarm.
Physical Symptoms
Common physical symptoms may include:
-
Dizziness or lightheadedness – often worsens with sudden standing or movement, typically short-lived but can feel alarming.
-
Nausea or gastrointestinal discomfort – mild to moderate stomach upset, sometimes including diarrhea or loss of appetite.
-
Headaches or pressure sensations – tension-type or sinus-like headaches can appear during dose reductions.
-
Fatigue or flu-like feelings – low energy, muscle aches, or general malaise are common as the body adjusts.
-
Sweating or chills – temperature regulation may fluctuate temporarily, causing intermittent sweating or shivering.
These symptoms are common, time-limited, and manageable for most people when Cymbalta is tapered gradually. For families, recognizing these as withdrawal-related—not signs of illness—can reduce panic and unnecessary emergency visits.
Sleep Disturbances
Sleep-related symptoms may include:
-
Difficulty falling or staying asleep – insomnia or frequent awakenings can appear in the first 1–2 weeks of tapering.
-
Vivid or intense dreams – unusually detailed or emotional dreams are common as the nervous system recalibrates.
-
Restless or non-restorative sleep – waking feeling unrefreshed despite adequate hours of sleep
Sleep disruptions often begin within the first 1-2 weeks of dose reduction and gradually improve over 3-6 weeks as serotonin and norepinephrine signaling stabilizes. Supporting consistent sleep routines can significantly ease this phase.
Emotional and Mental Health Symptoms
Emotional symptoms can be especially distressing and may include:
-
Heightened anxiety – sudden or intense feelings of worry that may not match the situation.
-
Irritability or emotional sensitivity – minor frustrations can feel overwhelming or trigger tears.
-
Low mood or tearfulness – temporary sadness or mood dips are common, not necessarily relapse.
-
Mood swings – rapid shifts between emotional highs and lows can occur as serotonin and norepinephrine levels fluctuate.
These symptoms can mimic depression or anxiety relapse, which is why reassurance and careful monitoring are critical. Research shows that withdrawal-related mood changes often improve as tapering stabilizes, whereas relapse tends to persist or worsen over time[2].
Sensory or Neurological Symptoms
Less common but widely reported symptoms include:
-
“Brain zaps” – brief, electric-shock-like sensations in the head or body; unsettling but harmless.
-
Sensitivity to light or sound – the nervous system may overreact temporarily to environmental stimuli.
-
Tremors or internal restlessness – mild shaking, jitteriness, or a sense of internal agitation.
These symptoms indicate temporary hypersensitivity of the nervous system. While unsettling, they are not dangerous and usually fade as the brain recalibrates serotonin signaling pathways.
What Is the Typical Cymbalta Withdrawal Timeline?
Withdrawal unfolds in phases, not all at once. Understanding this progression helps families anticipate challenges rather than fear them.
Important note: Timelines vary depending on dose, length of use, and taper speed. Slower tapers often reduce peak intensity and shorten overall recovery.
Why Should Cymbalta Be Tapered Slowly?
Stopping Cymbalta abruptly—sometimes called “cold turkey”—can overwhelm the nervous system, triggering intense reactions that may be mistaken for relapse rather than withdrawal. Risks include:
-
Severe withdrawal symptoms
Dizziness, nausea, flu-like sensations, and electric-shock sensations (“brain zaps”) can appear suddenly.
-
Sleep collapse
Insomnia or fragmented sleep can intensify mood instability.
-
Emotional dysregulation
Heightened anxiety, irritability, or sudden low moods can be overwhelming.
-
Cognitive confusion
Difficulty concentrating and memory lapses may make it hard to distinguish withdrawal from returning depression or anxiety.
Why gradual tapering works?
-
Stepwise receptor adjustment
The brain’s serotonin and norepinephrine receptors slowly recalibrate, minimizing shock to the system.
-
Lowered stress on body and mind
Physical symptoms and emotional turbulence are less severe when dose reductions follow the nervous system’s pace.
-
Better long-term outcomes
Research consistently shows that patients who taper slowly experience less discontinuation distress and are less likely to restart the medication due to overwhelming withdrawal[3].
Key principle: Go slow to go steady. Tapering schedules should be guided by how the body responds—not by rigid calendar deadlines. Flexibility reduces both physical discomfort and emotional uncertainty.
What Helps Manage Cymbalta Withdrawal Symptoms?
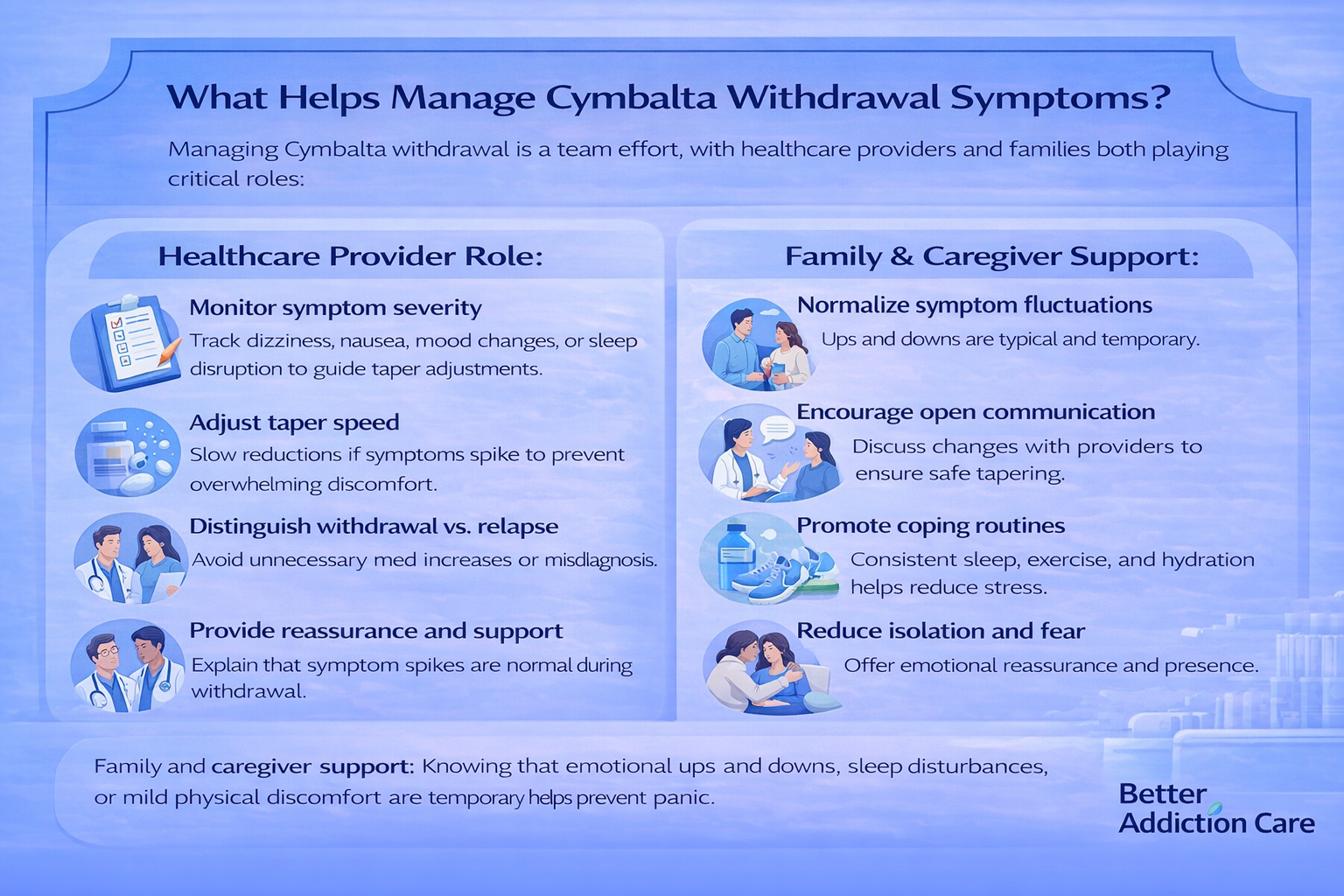
Managing Cymbalta withdrawal is a team effort, with healthcare providers and families both playing critical roles:
Healthcare providers are supported by:
-
Monitoring symptom severity – regular check-ins help track dizziness, nausea, mood changes, or sleep disruption and guide adjustments to the taper.
-
Adjusting taper speed – slowing reductions if symptoms spike can prevent overwhelming discomfort.
-
Distinguishing withdrawal from relapse – helps avoid unnecessary medication increases or misdiagnoses.
-
Providing reassurance – explaining that sudden symptoms are normal during withdrawal can reduce anxiety and fear-driven decisions.
-
Supporting overall mental health – offering coping strategies, therapy referrals, or short-term symptom relief as needed.
Family and caregiver support:
-
Normalize symptom fluctuations – knowing that emotional ups and downs, sleep disturbances, or mild physical discomfort are temporary helps prevent panic.
-
Encourage open communication – tracking symptoms and discussing changes with providers ensures safe tapering.
-
Promote coping routines – consistent sleep schedules, gentle exercise, hydration, and relaxation techniques can reduce stress on the nervous system.
-
Reduce isolation – emotional reassurance and presence make withdrawal feel more manageable and less frightening.
What Coping Strategies Help Manage Withdrawal Symptoms?
1. How Can I Improve My Sleep?
-
Keep consistent sleep and wake times – even small variations can disrupt the body’s internal clock.
-
Limit screen exposure before bed – blue light can interfere with melatonin production.
-
Create a calm evening routine – gentle stretching, reading, or warm showers signal the nervous system that it’s time to rest.
-
Optimize your sleep environment – cool, dark, quiet rooms with minimal distractions can improve sleep quality.
Benefit: Better sleep strengthens emotional resilience and reduces the intensity of withdrawal symptoms.
2. What Should I Eat and Drink During Withdrawal?
-
Eat balanced meals – include protein, complex carbs, and healthy fats to support stable energy and neurotransmitter function.
-
Stay hydrated – water helps reduce headaches, dizziness, and overall fatigue.
-
Limit caffeine and alcohol – both can increase anxiety, disrupt sleep, and amplify withdrawal effects.
-
Small, frequent meals – can help prevent energy crashes and nausea that often accompany tapering.
3. Should I Exercise?
-
Gentle activity – walking, yoga, or light stretching 20–30 minutes, 3–4 times per week, supports mood without overtaxing the nervous system.
-
Avoid high-intensity workouts during early tapering – intense exercise can temporarily spike anxiety or fatigue.
Benefit: Moderate movement helps regulate serotonin and norepinephrine naturally, complementing the taper.
4. How Can I Reduce Stress and Anxiety?
-
Breathing exercises – diaphragmatic breathing or box breathing calms the autonomic nervous system.
-
Mindfulness and meditation – short, daily practices can reduce rumination and anxiety spikes.
-
Predictable daily routines – scheduled meals, sleep, and relaxation periods signal safety to the brain.
Benefit: Lowered stress helps the prefrontal cortex better regulate emotions during chemical readjustment.
5. How Can I Stay Connected and Supported?
-
Maintain communication – talk openly with family, friends, or trusted peers about what you’re experiencing.
-
Support groups – connecting with others going through withdrawal can normalize experiences and reduce fear.
-
Check-ins with healthcare providers – sharing symptom progress helps adjust taper plans safely.
Benefit: Emotional support reduces feelings of isolation, which can intensify withdrawal symptoms.
6. Does Routine Matter?
-
Yes. Predictable patterns signal safety to the nervous system.
-
Daily structure – consistent sleep, meals, movement, and relaxation periods stabilize mood and energy levels.
-
Small rituals – morning stretches, evening tea, or journaling can anchor the day and reduce anxiety.
Benefit: Routine helps the body and mind adapt gradually to chemical changes, improving tolerance to withdrawal stress.
When Should I Seek Medical Help During Withdrawal?
Seek professional support if your loved one experiences:
-
Suicidal thoughts or behaviors
-
Severe or worsening depression
-
Inability to function daily for several weeks
-
Confusion, disorientation, or extreme agitation
These signs require timely evaluation and adjustment of the tapering plan.
What Comes After Withdrawal? (Long-Term Recovery)
Life after Cymbalta withdrawal often involves rediscovering your natural emotional rhythm.
Many people notice clearer thinking, more stable moods, and renewed energy once the nervous system readjusts. Recovery is a gradual process, and ongoing support is key.
Long-term recovery is supported by:
-
Regular medical check-ins – monitoring mental health ensures any returning symptoms are addressed early and safely.
-
Therapy or counseling – cognitive-behavioral therapy (CBT), mindfulness-based therapy, or supportive counseling can strengthen coping skills and emotional regulation.
-
Exercise and nutrition – consistent physical activity and balanced meals continue to support neurotransmitter health and overall brain function.
-
Ongoing family involvement – open communication, encouragement, and shared coping strategies reinforce a safe, supportive environment.
-
Self-monitoring and journaling – tracking moods, triggers, and sleep can highlight patterns and help prevent setbacks.
-
Mind-body practices – meditation, yoga, or breathing exercises reinforce nervous system stability and reduce lingering anxiety.
Recovery doesn’t end when withdrawal symptoms fade. Emotional resilience, coping strategies, and healthy routines take time to rebuild.
With steady support, most people find that life after Cymbalta can feel more balanced, manageable, and emotionally fulfilling.
Conclusion
Cymbalta withdrawal is real, temporary, and manageable. It is not a failure, weakness, or sign that recovery isn’t possible.
With gradual tapering, medical supervision, and consistent support, most people regain stability and confidence over time. Patience, compassion, and evidence-based care make a meaningful difference—for individuals and the families who walk beside them.
FAQs
Stopping Cymbalta abruptly can overwhelm the nervous system, causing dizziness, nausea, “brain zaps,” and mood swings. These withdrawal symptoms can be severe and frightening. Medical professionals strongly recommend a gradual taper, allowing the brain to adjust slowly, reducing discomfort and lowering the risk of misinterpreting withdrawal for relapse.
Cymbalta withdrawal symptoms typically improve within 4–8 weeks, though some individuals may experience milder effects for longer. Duration depends on dose, taper speed, and individual brain chemistry. Following a slow taper, practicing self-care, and maintaining medical support usually help the nervous system recalibrate more smoothly and reduce the overall intensity of symptoms.
Withdrawal can mimic relapse, with mood swings, irritability, or anxiety spikes. Proper tapering, symptom tracking, and emotional support help distinguish temporary withdrawal effects from a true recurrence of depression or anxiety. Most people find that once the nervous system stabilizes, underlying mental health symptoms are manageable with therapy, lifestyle routines, and follow-up care.
Supporting the nervous system through structured routines, adequate sleep, gentle exercise, and balanced nutrition can reduce withdrawal intensity. Mindfulness, breathing exercises, and emotional support from loved ones also help manage stress and anxiety. These strategies work alongside tapering to strengthen resilience and improve both physical comfort and emotional stability during withdrawal.
Family and friends can provide crucial support by listening without judgment, validating symptoms, and encouraging adherence to the taper plan. Offering reassurance during symptom spikes, helping maintain routines, and gently motivating healthy habits like sleep, meals, and light activity can reduce stress, prevent isolation, and promote a smoother, safer withdrawal experience.
If withdrawal symptoms become overwhelming, it’s important to contact your healthcare provider. They can slow the taper, suggest temporary relief strategies, and monitor for complications. Supportive interventions may include short-term symptom management, therapy check-ins, or adjustments in routines, helping you regain control and safely navigate the most difficult stages of withdrawal.
Resources
Related Articles
Treatment Centers in Virginia










