What Is GHB? Effects, Risks, and Legal Status
Gamma-hydroxybutyrate (GHB) is a substance most people encounter during moments of concern—not curiosity. People often search for information after unexplained blackouts, emergency room visits, or sudden personality changes.

Key Takeaways
-
GHB carries a high medical risk due to its narrow safety margin. Small changes in dose or timing can quickly shift effects from relaxation to overdose, leading to loss of consciousness, slowed breathing, or medical emergencies without clear warning signs.
-
Dependence and withdrawal can develop rapidly and unpredictably. Physical dependence may form within weeks, and withdrawal can become life-threatening without medical supervision, making professional detox an essential safety measure.
-
Families often recognize warning signs before a crisis occurs. Blackouts, memory gaps, frequent dosing, anxiety between doses, or mixing GHB with alcohol are signals that medical risk is increasing and intervention may be needed.
-
Early, medically informed treatment improves outcomes for both individuals and families. When care is matched to the level of risk, recovery becomes safer, more stable, and more sustainable over time.
Individuals may search because they are experiencing loss of control, intense anxiety between doses, or withdrawal symptoms they do not understand.
Disclaimer: This content is for educational purposes only and does not substitute medical or legal advice. Substance laws and clinical recommendations change, and professional evaluation is essential in any situation involving drug use or withdrawal.
What Is GHB?
Gamma-hydroxybutyrate (GHB) is a central nervous system depressant, meaning it slows brain activity. [1] In small amounts, GHB exists naturally in the human brain. When taken as a drug, however, it overwhelms the brain’s regulatory systems.
In the United States, a pharmaceutical form of GHB—sodium oxybate—is FDA-approved under strict controls for treating narcolepsy, a neurological sleep disorder. Outside of this medical use, GHB is illegal and dangerous.
Common Street Names
-
G
-
Liquid Ecstasy (misleading; GHB is not a stimulant)
-
Scoop
-
Goop
-
Fantasy
GHB is most commonly found as a colorless, odorless liquid, but may also appear as a powder or capsule. Because it dissolves easily in drinks and has little taste, accidental overdose is high.
How GHB Is Consumed and Typical Dosages?
GHB is most commonly found as a colorless, odorless liquid, but it can also appear as a powder or capsule. Its form affects how quickly it works and how dangerous it can be.
-
Liquid: Often added to drinks, making accidental overdose easy. Effects appear within 10–20 minutes.
-
Powder or Capsule: May be mixed into food or beverages; onset is slightly slower but still rapid.
-
Typical Street Doses: Vary widely; there is no standardized “safe” amount. Even experienced users may misjudge potency.
Because GHB is absorbed quickly and its effects peak fast, small measurement errors can lead to sudden unconsciousness or overdose.
How GHB Affects the Brain and Body?
GHB primarily affects GABA receptors—chemical messengers that regulate calmness and inhibition in the brain. GABA (gamma-aminobutyric acid) acts like the brain’s braking system.
What Happens in the Brain?
Once GHB enters the bloodstream, it reaches the brain quickly and overstimulates GABA receptors. This affects several key areas:
-
Prefrontal cortex: Decision-making and impulse control weaken, leading to risky or uncharacteristic behavior.
-
Hippocampus: Memory formation is suppressed, causing blackouts where your loved one appears awake but remembers nothing later.
-
Brainstem: Breathing and heart rate may slow at higher doses, increasing overdose risk.
Because these systems regulate survival, even small dose changes can have serious consequences.
One of the most dangerous features of GHB is the narrow gap between effects. The difference between relaxation and unconsciousness is small and inconsistent.
This happens because:
-
GHB is absorbed rapidly and peaks quickly.
-
Tolerance can change from day to day.
-
The body does not process GHB at a steady rate.
A dose that seemed manageable before can suddenly cause a medical emergency.
How GHB Affects the Body?
GHB impacts multiple body systems at the same time:
-
Breathing: Slows respiration, raising the risk of oxygen deprivation.
-
Heart function: Can lower heart rate and blood pressure.
-
Muscle control: Causes poor coordination, weakness, or sudden collapse.
-
Stomach and airway: Increases vomiting risk, which is dangerous if consciousness is reduced.
Snoring, shallow breathing, or long pauses between breaths are warning signs—not normal sleep.
How Repeated Use Changes Brain Chemistry?
With repeated use, the brain reduces its own calming chemicals in response to constant GHB exposure. Over time, the nervous system depends on the drug to stay balanced.
This leads to:
-
Anxiety and agitation between doses.
-
Inability to sleep without GHB.
-
Severe symptoms when use stops suddenly.
These changes are biological, not behavioral. They explain why stopping without medical support can be dangerous.
Short-Term Effects of GHB Use
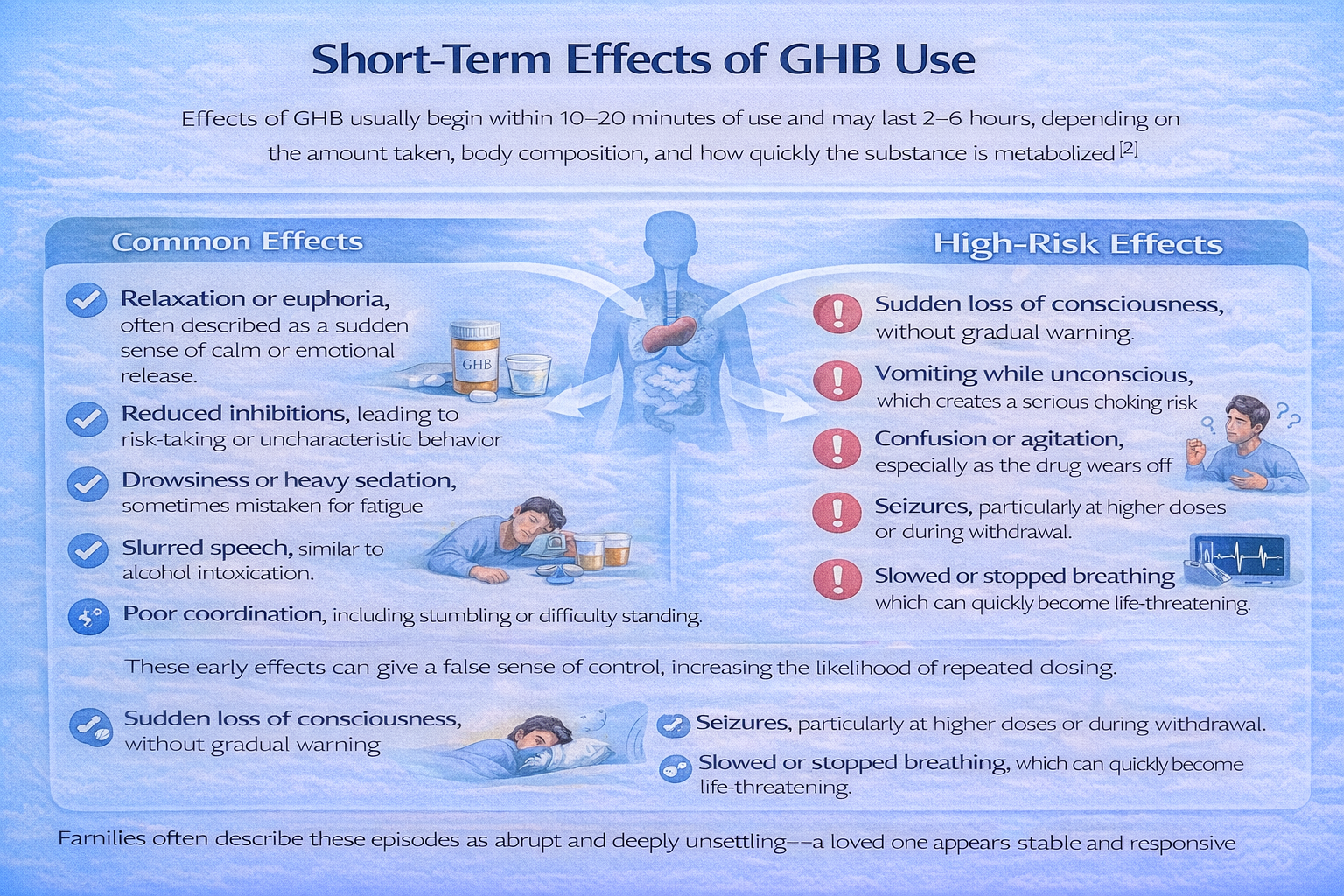
Effects of GHB usually begin within 10–20 minutes of use and may last 2–6 hours, depending on the amount taken, body composition, and how quickly the substance is metabolized[2]. What makes GHB especially dangerous is how fast these effects can intensify, often without clear warning signs.
Common Effects
At lower or initial doses, the sufferer or loved ones may notice effects that appear mild or even misleadingly manageable:
-
Relaxation or euphoria, often described as a sudden sense of calm or emotional release
-
Reduced inhibitions, leading to risk-taking or uncharacteristic behavior
-
Drowsiness or heavy sedation, sometimes mistaken for fatigue
-
Slurred speech, similar to alcohol intoxication
-
Poor coordination, including stumbling or difficulty standing
These early effects can give a false sense of control, increasing the likelihood of repeated dosing.
High-Risk Effects
With slightly higher amounts—or when doses overlap—effects can escalate rapidly:
-
Sudden loss of consciousness, without gradual warning
-
Vomiting while unconscious, which creates a serious choking risk
-
Confusion or agitation, especially as the drug wears off
-
Seizures, particularly at higher doses or during withdrawal
-
Slowed or stopped breathing, which can quickly become life-threatening
Families often describe these episodes as abrupt and deeply unsettling—a loved one appears stable and responsive one moment, then becomes dangerously impaired or unresponsive the next.
This unpredictability is a defining risk of GHB use and a key reason medical intervention is often required.
Long-Term Effects of GHB Use
Repeated GHB use can have lasting impacts on both the brain and body. People often notice gradual changes in behavior or health that signal chronic risk.
Cognitive Effects
-
Memory problems: Difficulty forming or recalling new memories, similar to repeated blackouts, can become persistent.
-
Trouble concentrating: Tasks that require focus or multi-step thinking may feel overwhelming.
-
Slowed decision-making: Impulse control and judgment weaken, increasing risky behaviors even outside intoxication periods.
Emotional Effects
-
Persistent anxiety: The brain’s natural calming mechanisms are disrupted, causing ongoing nervousness or restlessness.
-
Depression and mood swings: Emotional regulation may become unstable, leading to frequent irritability, sadness, or sudden emotional outbursts.
-
Increased sensitivity to stress: Even minor challenges can feel overwhelming, heightening frustration or fear.
Physical Effects
-
Sleep disruption: Chronic users often struggle with insomnia or fragmented sleep, even when not using GHB.
-
Low energy and fatigue: The body’s nervous system may feel constantly depleted, making daily activities exhausting.
-
Cardiovascular irregularities: Occasional changes in heart rate or blood pressure can occur, increasing long-term risk.
Social and Lifestyle Effects
-
Strained relationships: Friends and family may feel confused, frustrated, or mistrustful due to unpredictable behavior or blackouts.
-
Loss of stability: Work, school, or daily routines often suffer as cognitive and emotional impairments accumulate.
-
Isolation: Individuals may withdraw socially or rely heavily on GHB to manage emotional stress, worsening dependency.
Understanding these long-term effects helps families recognize that addiction is a medical issue, not a character flaw.
GHB and Memory Loss: Why Blackouts Are Common?
One of the most alarming effects of GHB is memory loss, often described as a blackout. This occurs because GHB suppresses activity in the hippocampus, the part of the brain responsible for forming and storing new memories.
When the hippocampus is disrupted, experiences may occur in real time but are never properly recorded.
As a result:
-
A person may appear awake, responsive, and able to talk, yet later have no memory of events.
-
Awareness and consent are severely impaired because the brain cannot fully process or retain information.
-
Medical emergencies become confusing afterward, making it difficult for individuals to explain what happened or recognize the seriousness of the situation.
These memory gaps are not the same as falling asleep or resting. They reflect suppressed brain function, where essential systems involved in awareness and recall are temporarily shut down.
For individuals, repeated blackouts are a critical warning sign that the brain is being placed under dangerous strain and that professional evaluation is needed.
Signs and Red Flags for Families
Families often see warning signs before a medical emergency occurs. Early recognition can save lives and prevent crises.
-
Frequent blackouts or memory gaps
-
Sudden personality changes or unusual risk-taking
-
Repeated use in short intervals, indicating tolerance or dependence
-
Agitation, anxiety, or insomnia between doses
-
Mixing GHB with alcohol or other sedatives
If these behaviors appear, professional evaluation should be sought immediately.
Overdose Risk: Why GHB Is Especially Dangerous?
GHB carries a higher overdose risk than many other substances because the line between a “manageable” dose and a life-threatening one is extremely thin. Consumers are often shocked by how quickly a situation escalates, even when use seems unchanged.
Several factors increase this risk:
-
No standardized street dose, meaning potency varies widely from one source to another
-
Rapid absorption, with effects appearing quickly after use
-
Short duration, which encourages repeated dosing to maintain effects
Together, these factors make GHB unpredictable, even for individuals who believe they understand their limits.
Dose Timing Matters?
Because GHB wears off relatively quickly, many people re-dose every 2–4 hours. The danger lies in timing. If a new dose is taken before the previous one has fully cleared, the effects stack rather than reset.
Breathing, heart rate, and consciousness can drop suddenly, leading to overdose without gradual warning signs.
This risk exists even in experienced users and increases sharply when GHB is combined with other depressants.
Co-Use Risks: GHB with Other Substances
Combining GHB with other depressants dramatically increases overdose risk. One should be aware of how interactions affect the body.
-
Alcohol: Slows breathing and reduces consciousness, compounding GHB’s effects
-
Benzodiazepines: Can trigger severe sedation, memory loss, or respiratory failure
-
Opioids: Significantly increase the risk of fatal overdose
Even small amounts of these combinations can be life-threatening.
Signs of GHB Overdose
-
Unresponsiveness or inability to wake
-
Shallow, irregular, or stopped breathing
-
Bluish lips or fingertips, indicating low oxygen levels
-
Seizures or uncontrolled muscle movements
Any of these signs indicates a medical emergency. Immediate professional care is critical, as timely intervention can be life-saving.
GHB Dependence and Addiction
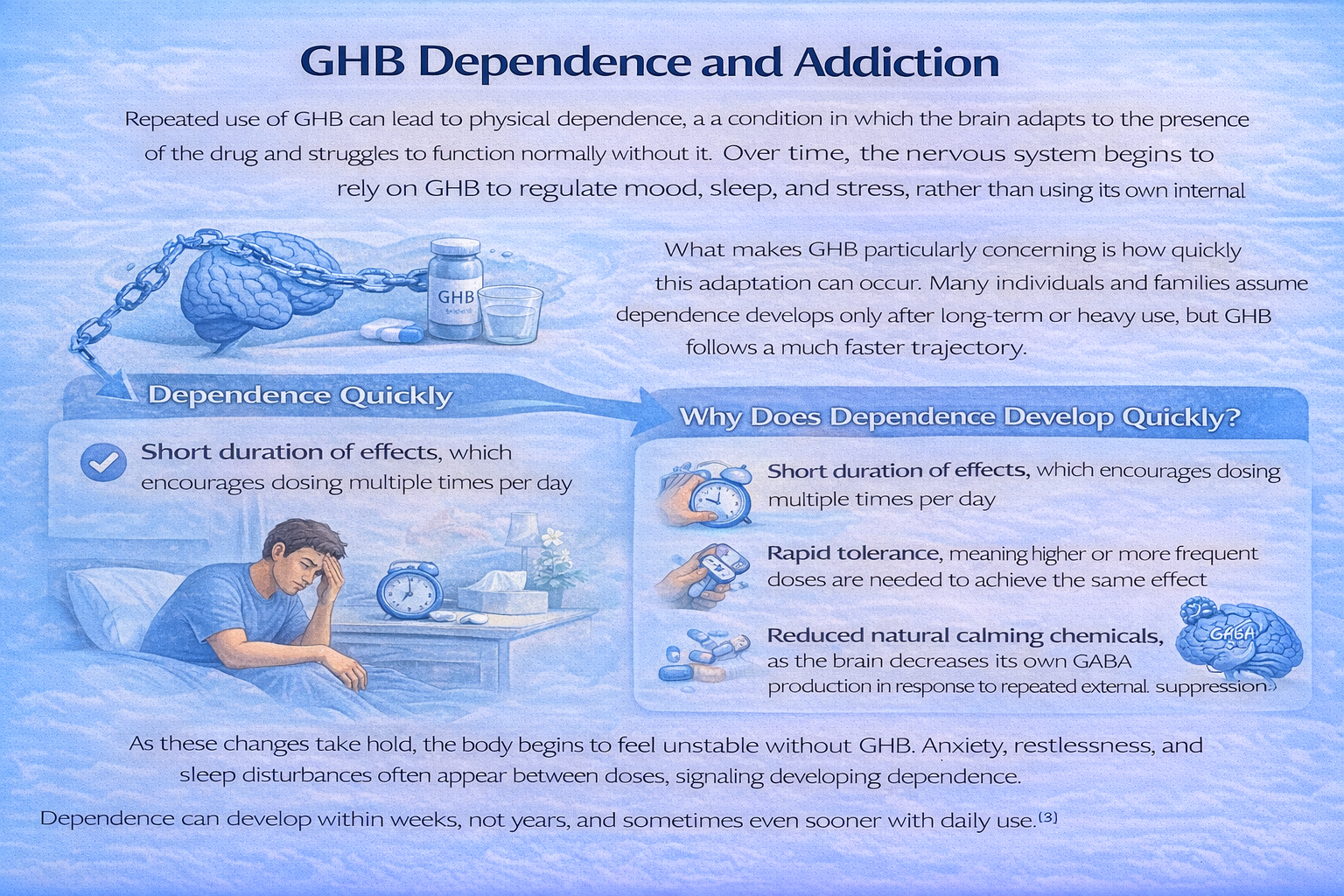
Repeated use of GHB can lead to physical dependence, a condition in which the brain adapts to the presence of the drug and struggles to function normally without it.
Over time, the nervous system begins to rely on GHB to regulate mood, sleep, and stress, rather than using its own internal mechanisms.
What makes GHB particularly concerning is how quickly this adaptation can occur. Many individuals and families assume dependence develops only after long-term or heavy use, but GHB follows a much faster trajectory.
Why Does Dependence Develop Quickly?
Several factors accelerate the process:
-
Short duration of effects, which encourages dosing multiple times per day
-
Rapid tolerance, meaning higher or more frequent doses are needed to achieve the same effect
-
Reduced natural calming chemicals, as the brain decreases its own GABA production in response to repeated external suppression
As these changes take hold, the body begins to feel unstable without GHB. Anxiety, restlessness, and sleep disturbances often appear between doses, signaling developing dependence.
Dependence can develop within weeks, not years, and sometimes even sooner with daily use. [3]
This rapid progression often surprises both individuals and families, delaying recognition of the problem until withdrawal symptoms or medical crises occur.
GHB Withdrawal: A Medical Emergency
GHB withdrawal is considered one of the most dangerous withdrawal syndromes, particularly because of how quickly symptoms can appear and intensify.
Unlike some substances where discomfort builds gradually, GHB withdrawal can escalate within hours and become unpredictable without warning.
Symptoms may begin as soon as 1–6 hours after the last dose, especially in individuals who use GHB frequently or daily. As the brain struggles to function without the drug’s suppressive effects, the nervous system can enter a state of extreme overactivation.
Common Withdrawal Symptoms
-
Severe anxiety and panic, often sudden and overwhelming
-
Tremors or shaking, especially in the hands and arms
-
Insomnia lasting several days, which further worsens mental and physical stress
-
Hallucinations, including visual or auditory disturbances
-
Delirium, marked by confusion, agitation, and disorientation
-
Elevated heart rate and blood pressure, increasing the risk of cardiac complications
Without medical supervision, these symptoms can progress to seizures, dangerous cardiovascular strain, or medical collapse. For this reason, home detox is strongly discouraged, and medically supervised withdrawal management is essential for safety.
Impact on Families and Relationships
GHB use and withdrawal do not affect the individual alone. Families and close relationships often carry a significant emotional and psychological burden.
Common experiences include:
-
Constant fear of overdose, especially during sleep or periods of unresponsiveness
-
Emotional exhaustion, caused by repeated crises and unpredictability
-
Confusion and distress due to memory gaps, which can disrupt communication and trust
-
Loss of stability, as routines, responsibilities, and relationships become strained
Families need to understand that dependence reflects changes in brain chemistry, not a lack of effort or character.
Recovery is possible, but it typically requires medical support, structured treatment, and family-informed care to restore safety and stability over time.
When Professional Help Is Necessary?
Recognizing when to seek professional help can prevent medical emergencies and long-term harm. Because GHB affects critical brain and nervous system functions, delays in care can quickly increase risk.
Seek Immediate Professional Evaluation If:
-
GHB is used daily or multiple times per day, indicating developing dependence
-
Withdrawal symptoms appear between doses, such as anxiety, shaking, or insomnia
-
There have been blackouts, collapses, or emergency room visits, even if the person recovered quickly
-
GHB is combined with alcohol or sedatives, which sharply increases overdose risk
Early professional involvement:
-
Reduces the risk of overdose and severe withdrawal
-
Allows for safer, medically supervised detox if needed
-
Improves long-term recovery outcomes by addressing issues before the crisis escalates
If you are unsure whether the situation is serious enough, that uncertainty itself is a reason to seek professional guidance. Early evaluation is about safety—not judgment—and can make a meaningful difference in recovery.
Treatment Options for GHB Use Disorder (U.S.)
Effective treatment for GHB use disorder requires a care plan matched to medical risk, not willpower alone. Because GHB affects critical brain and nervous system functions, professional treatment is often necessary to ensure safety during both stabilization and recovery.
Medically Supervised Detox
Medically supervised detox is often the first and most critical step, especially for individuals who use GHB daily or experience symptoms between doses.
Key components include:
-
Continuous medical monitoring to respond quickly to changes in heart rate, blood pressure, or breathing
-
Stabilization of vital signs, reducing the risk of medical complications
-
Prevention and management of seizures and delirium, which can occur during withdrawal
Detox provides a safe environment where the brain and body can begin to rebalance under professional care.
Inpatient or Residential Treatment
Following detox, many individuals benefit from inpatient or residential treatment, where recovery can continue in a structured, supportive setting.
This level of care offers:
-
A stable, substance-free environment that reduces immediate relapse risk
-
Behavioral therapy to address triggers, coping skills, and underlying stressors
-
Ongoing medical oversight, particularly during early stabilization
This phase helps individuals rebuild routines and regain physical and emotional stability.
Ongoing Recovery Support
Long-term recovery often requires continued support beyond inpatient care.
Common components include:
-
Individual therapy to strengthen emotional regulation and decision-making
-
Relapse prevention planning, focusing on high-risk situations and early warning signs
-
Family education and involvement, helping loved ones understand recovery and provide healthy support
Recovery is achievable, especially when treatment intensity is matched to the level of medical and psychological risk. With appropriate care, many individuals regain stability, health, and long-term functioning.
Recovery Timeline and Expectations
Recovery from GHB use disorder is possible but requires structured, medically informed care. Families often ask how long stabilization and ongoing recovery take.
-
Detox: Usually lasts several days under medical supervision; intensity depends on usage history
-
Early Recovery (Weeks 1–12): Physical stabilization, withdrawal management, and initial therapy
-
Ongoing Recovery (Months 3–12): Cognitive and emotional rebuilding, relapse prevention, and family involvement
-
Long-Term: Many individuals regain stable sleep, emotional regulation, and improved relationships over 6–12 months
Recovery is gradual, and setbacks are part of the process, but consistent professional care dramatically improves outcomes.
Legal Status of GHB in the United States
GHB’s legal status in the U.S. is often confusing, especially for families encountering the substance for the first time. Understanding the distinction between illegal GHB and its tightly regulated medical form helps clarify why enforcement is strict while medical care remains protected.
Federal Classification (U.S.) [3]
Under federal law, GHB is classified differently depending on how it is used:
-
Schedule I:
-
Applies to non-medical GHB
-
Indicates a high potential for abuse
-
Possession, manufacture, or distribution is illegal
-
Schedule III:
-
Applies to FDA-approved sodium oxybate (used to treat narcolepsy)
-
Available only through a restricted medical program
-
Requires strict physician oversight and monitoring
This dual classification exists because the substance has legitimate medical use but carries serious risks outside controlled settings.
Why Are GHB Laws Strict?
Federal restrictions are designed to reduce harm, not punish medical emergencies. Laws remain strict due to:
-
High overdose risk, even with small dosing errors
-
A documented history of misuse, particularly in social settings
-
Severe and potentially life-threatening withdrawal, which requires medical care
What does this mean during a Medical Emergency?
In emergencies, health and safety come first. Medical professionals prioritize stabilizing the individual, not legal consequences.
Delaying care due to fear of legal trouble can increase the risk of serious injury or death.
If GHB use is suspected, seeking immediate medical help is always the safest and most responsible step.
Conclusion
GHB is a powerful and unpredictable substance that affects the brain and body in ways that can quickly become dangerous. Its ability to cause rapid dependence, severe withdrawal, and overdose makes early recognition and professional intervention essential.
Families play a critical role in noticing warning signs such as blackouts, frequent dosing, or agitation between doses. Understanding that these behaviors reflect changes in brain chemistry, not lack of willpower, is key to responding with safety and support.
Recovery is possible with medically supervised detox, structured treatment, and ongoing support, including family involvement and relapse prevention planning. Early action not only protects your loved one from immediate harm but also lays the foundation for long-term health, stability, and hope.
FAQs
In the U.S., GHB is misused for its sedative and euphoric effects. Some individuals use it to relax or induce sleep. A regulated form is prescribed for narcolepsy. Non-medical use carries a high overdose and dependence risk due to unpredictable dosing.
GHB is metabolized quickly, often within 4–6 hours. This short detection window means drug tests may miss it unless conducted soon after use. Rapid clearance increases overdose risk because users may re-dose before previous doses fully wear off.
Yes. GHB can cause physical dependence within weeks if used repeatedly. The brain adapts quickly, especially when GHB is used to manage anxiety or sleep problems. What begins as occasional use can escalate rapidly.
Yes, with rapid medical intervention. Emergency care focuses on airway protection and monitoring. Because GHB leaves the system quickly, supportive care is often effective when provided early.
Both depress the central nervous system, but GHB acts faster, has a narrower safety margin, and causes more severe withdrawal. Alcohol effects are easier to dose and recognize, while GHB overdose occurs more unpredictably.
Yes. With medically supervised detox and structured treatment, many people regain stable sleep, emotional regulation, and cognitive clarity. Ongoing support is especially important during the first 6–12 months.
Resources
Related Articles
Treatment Centers in Oregon










