Hydrocodone Addiction Definition, Symptoms, Causes, Side Effects, and Treatment
Hydrocodone is prescribed to ease pain, but for many, it brings a very different kind of suffering, dependence that reshapes health, relationships, and daily life.
What begins as relief after an injury or surgery can quietly progress into cravings, withdrawal symptoms, and cycles that feel impossible to break.
For care providers, families, and people around, this shift is heartbreaking to watch; for individuals, it’s overwhelming to live through.
Given the challenges, a critical question arises: What exactly is hydrocodone addiction, how does it affect people, and what can be done to treat it?
Hydrocodone addiction develops when repeated use rewires the brain’s reward system, leading to tolerance, dependence, and withdrawal if use stops.

Symptoms can emerge within weeks of misuse, but with treatment, many people see withdrawal symptoms peak in the first 3–5 days and cravings gradually ease over 2–3 months. This isn’t just medical information — it’s a path forward.
Understanding these stages helps in:
-
Recognize warning signs early instead of missing them,
-
Know when to seek urgent professional help, and
-
Support their loved one with realistic expectations of recovery timelines.
Key Takeaways
-
Hydrocodone addiction develops gradually — what starts as prescribed pain relief can turn into dependence and addiction marked by cravings, withdrawal, and loss of control. Recognizing early warning signs such as drowsiness, mood swings, and secrecy can help families step in before the problem deepens.
-
Addiction is driven by multiple factors, not weakness. Genetics, mental health challenges, and environmental pressures all contribute. Understanding this removes stigma and reinforces that recovery requires medical support, not blame.
-
Treatment works, and recovery is possible. Evidence-based options like medication-assisted treatment, counseling, and structured programs significantly improve outcomes. While withdrawal is tough, symptoms peak in the first week and gradually ease with proper care. With the right treatment plan and strong support, many people go on to rebuild healthier, more stable lives.
What Is Hydrocodone Addiction?
Hydrocodone is an opioid painkiller—safe and helpful when used as directed. But when it’s taken too often or in higher doses, the body starts to rely on it. That’s when addiction takes hold.
The drug activates your brain’s “feel-good” circuits. Over time, your brain stops responding the same way. Now you need more just to feel “normal.” That’s tolerance. Stop taking it, and withdrawal symptoms like anxiety or nausea can hit—this is physical dependence.
Hydrocone Dependence vs Hydrocodone Addiction: It’s important to note the distinction between physical dependence and addiction. Dependence happens when the body adapts to the drug, and withdrawal occurs if it’s stopped.
Addiction goes a step further: it’s marked by compulsive use, loss of control, and continued misuse despite negative consequences. Both can exist together, but addiction represents a deeper and more disruptive problem.
Addiction isn’t just about the drug—it’s about loss of control.
Even if someone wants to quit, cravings and discomfort can be overwhelming. Early recognition opens the door to treatment—not guilt, not shame, just help.
Signs & Symptoms of Hydrocodone Addiction
Physical Symptoms
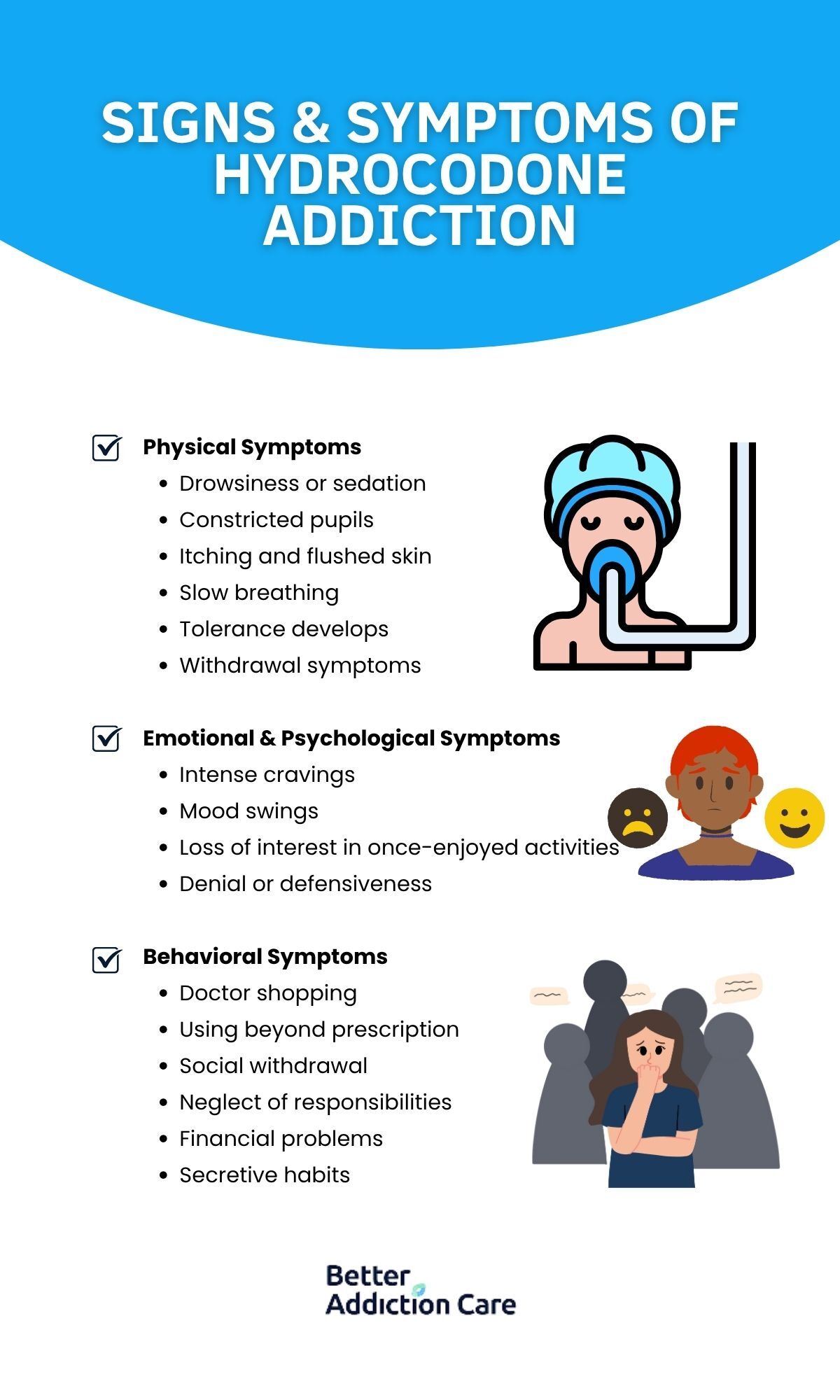
Hydrocodone directly affects the central nervous system, which is why the first warning signs often appear in the body.
-
Drowsiness or sedation is common, with individuals frequently “nodding off” or struggling to stay awake during normal activities.
-
Constricted pupils may be noticeable, even in low-light environments, signaling the body’s opioid response.
-
Nausea or vomiting often occurs, particularly as the effects of the drug wear off.
-
Itching and flushed skin can develop because hydrocodone triggers histamine release in the body.
-
Slow breathing is another critical sign, since opioids suppress respiratory function and can sometimes slow it to dangerous levels.
-
Tolerance develops when someone needs increasingly higher doses of hydrocodone to achieve the same pain relief or sense of calm.
-
Withdrawal symptoms such as muscle aches, sweating, restlessness, or insomnia may appear when hydrocodone use is reduced or stopped.
Emotional & Psychological Symptoms
Addiction also reshapes how a person feels and reacts emotionally, often just as disruptively as the physical changes.
-
Intense cravings create a constant mental pull toward taking more hydrocodone, even when it’s harmful.
-
Mood swings may appear, with periods of irritability, anxiety, or depression alternating with brief moments of euphoria.
-
Loss of interest in once-enjoyed activities—whether hobbies, work, or family time—is another common indicator.
-
Denial or defensiveness often surfaces when loved ones raise concerns, leading to secrecy and strained communication.
Behavioral Symptoms
Families frequently notice changes in behavior before they recognize the physical or emotional signs. These patterns can disrupt work, school, and relationships.
-
Doctor shopping occurs when someone visits multiple healthcare providers in an effort to secure extra prescriptions.
-
Using beyond prescription is another red flag, as the person begins taking more than the doctor ordered or using the medication without a valid medical need.
-
Social withdrawal becomes common, with individuals avoiding gatherings, friends, or conversations to conceal their use.
-
Neglect of responsibilities often shows up in missed deadlines, skipped classes, or difficulty managing childcare or work duties.
-
Financial problems may arise, marked by unexplained spending, borrowing, or money disappearing from shared accounts.
-
Secretive habits develop as individuals hide pills, lie about their usage, or disappear for extended periods without explanation.
How Common Are These Symptoms?
Hydrocodone addiction is far more widespread than many realize. One large international review of over 4.3 million patients prescribed opioids—including hydrocodone—found that one in three showed signs of dependence, while one in ten developed full dependence[1].
In the U.S., national survey data show that among adults who used prescription opioids in the past year, 12.1% misused them and 7% met criteria for a prescription opioid use disorder[2].
In clinical settings, prevalence is even higher. Among chronic pain outpatients on long-term opioid therapy, nearly 35% met criteria for opioid use disorder, with 21.7% classified as moderate and 13.2% as severe[3].
Withdrawal symptoms—a hallmark of physical dependence—are also common. In one study of people who inject opioids, 85% reported withdrawal in the past six months, with 29% experiencing it monthly and 35% experiencing it weekly[4].
Causes of Hydrocodone Addiction
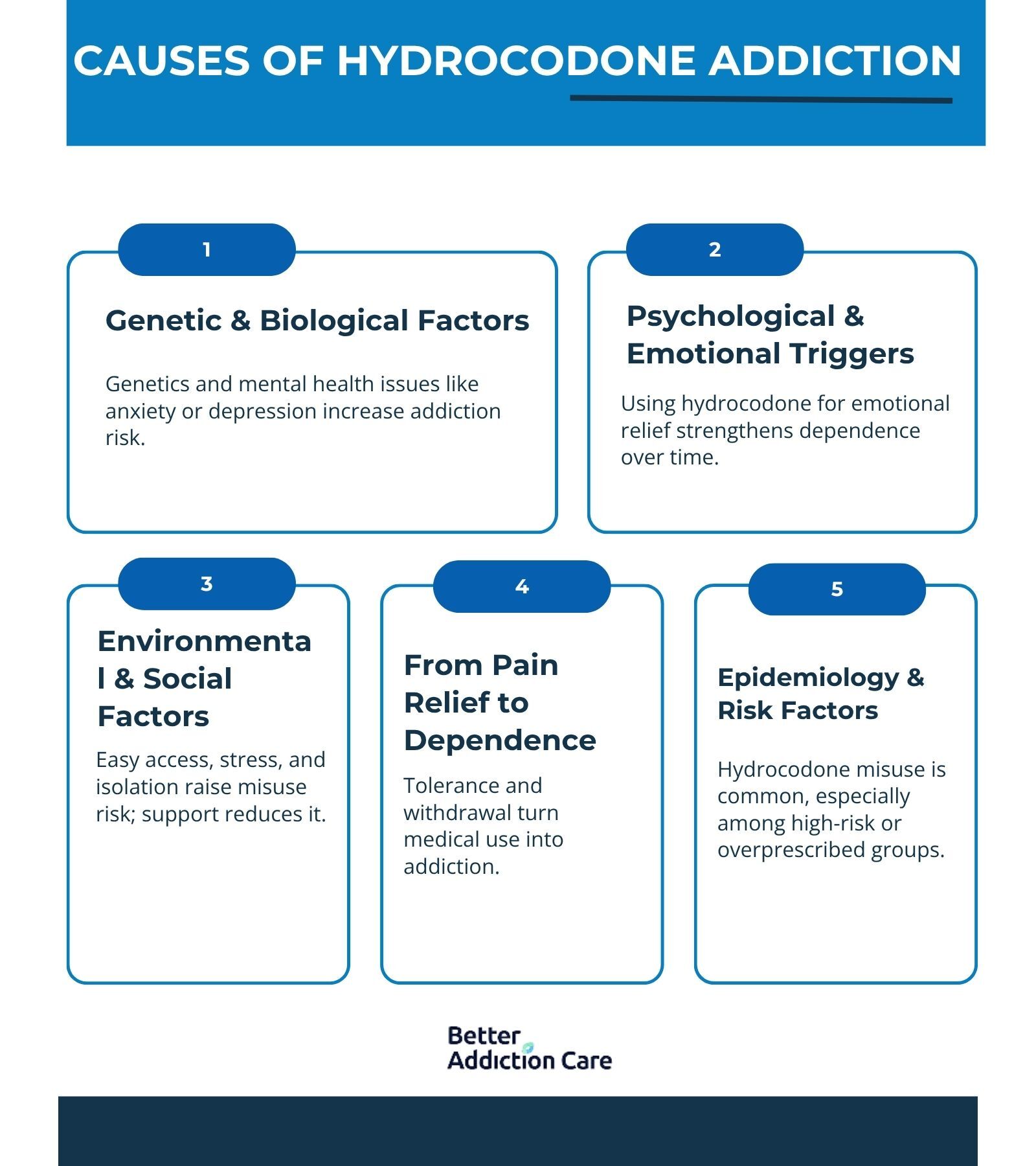
Addiction doesn’t come down to a single choice—it’s the result of overlapping medical, psychological, and social factors.
For many, hydrocodone starts as a legitimate prescription for pain relief. But over time, the brain, body, and environment can work together in ways that make stopping incredibly difficult.
How Hydrocodone Affects the Brain?
Hydrocodone binds to opioid receptors in the brain, particularly in the prefrontal cortex and the brain’s reward pathway. This action dulls pain but also releases dopamine, the neurotransmitter responsible for feelings of pleasure and reward.
Over time, the brain adapts: natural dopamine production decreases, while cravings for hydrocodone increase. This creates a cycle where the drug becomes less about pain relief and more about avoiding discomfort, withdrawal, or emotional distress.
Research shows that repeated opioid exposure increases the likelihood of dependence, and one in ten patients prescribed opioids long-term will develop an addiction[1].
Genetic & Biological Factors
Not everyone who takes hydrocodone becomes addicted. Family history plays a role—genetics can account for 40–60% of an individual’s vulnerability to addiction, according to the National Institute on Drug Abuse[5].
People with certain gene variations may metabolize opioids differently, making them more prone to dependence. Additionally, individuals with existing mental health conditions like depression, anxiety, or PTSD are more likely to misuse prescription opioids, using them not just for pain but as a form of self-medication.
Psychological & Emotional Triggers
Addiction often takes root when hydrocodone becomes tied to emotional relief. Someone recovering from surgery might notice the drug also numbs stress, eases loneliness, or calms anxiety.
Over time, the brain begins to associate hydrocodone with escape—not just from pain, but from life’s difficulties. This makes the cycle of dependence stronger. Studies suggest that opioid misuse is significantly more common in individuals reporting high levels of untreated psychological distress[2].
Environmental & Social Factors
Circumstances matter. Easy access to prescriptions, limited medical oversight, or living in a community with high rates of opioid prescribing can all raise the risk.
Social isolation makes things worse, while supportive environments can sometimes delay or reduce dependence. Financial stress, family conflict, or lack of access to healthier coping outlets also fuel the path to misuse.
In fact, research indicates that doctor shopping and over-prescription remain strong predictors of misuse and eventual addiction[3].
From Pain Relief to Dependence
For most people, addiction doesn’t start with the intention to misuse. It begins with legitimate pain management—an injury, surgery, or chronic condition. The problem arises when tolerance builds, requiring higher doses for the same effect, and withdrawal symptoms surface when trying to cut back.
According to one large study, 85% of opioid users reported withdrawal symptoms within six months, making stopping without support extremely difficult[4].
Epidemiology & Risk Factors
Recent surveys estimate that millions of Americans misuse prescription pain relievers each year, with hydrocodone being among the most frequently involved opioids[2].
While anyone prescribed the medication can develop dependence, some groups are at higher risk: individuals with chronic pain conditions, those with untreated mental health disorders, and people with a family history of substance use disorders[3].
Overprescription has also played a role—at one point, hydrocodone combination products were the most prescribed medications in the country[2]. The shift to stricter regulation in 2014 (moving hydrocodone products to Schedule II) reduced some availability, but misuse remains significant.
Recognizing these broader risk factors helps families understand that addiction isn’t a sign of weakness; it’s a predictable outcome when biology, mental health, and environment collide.
Short-Term and Long-Term Side Effects of Hydrocodone Addiction
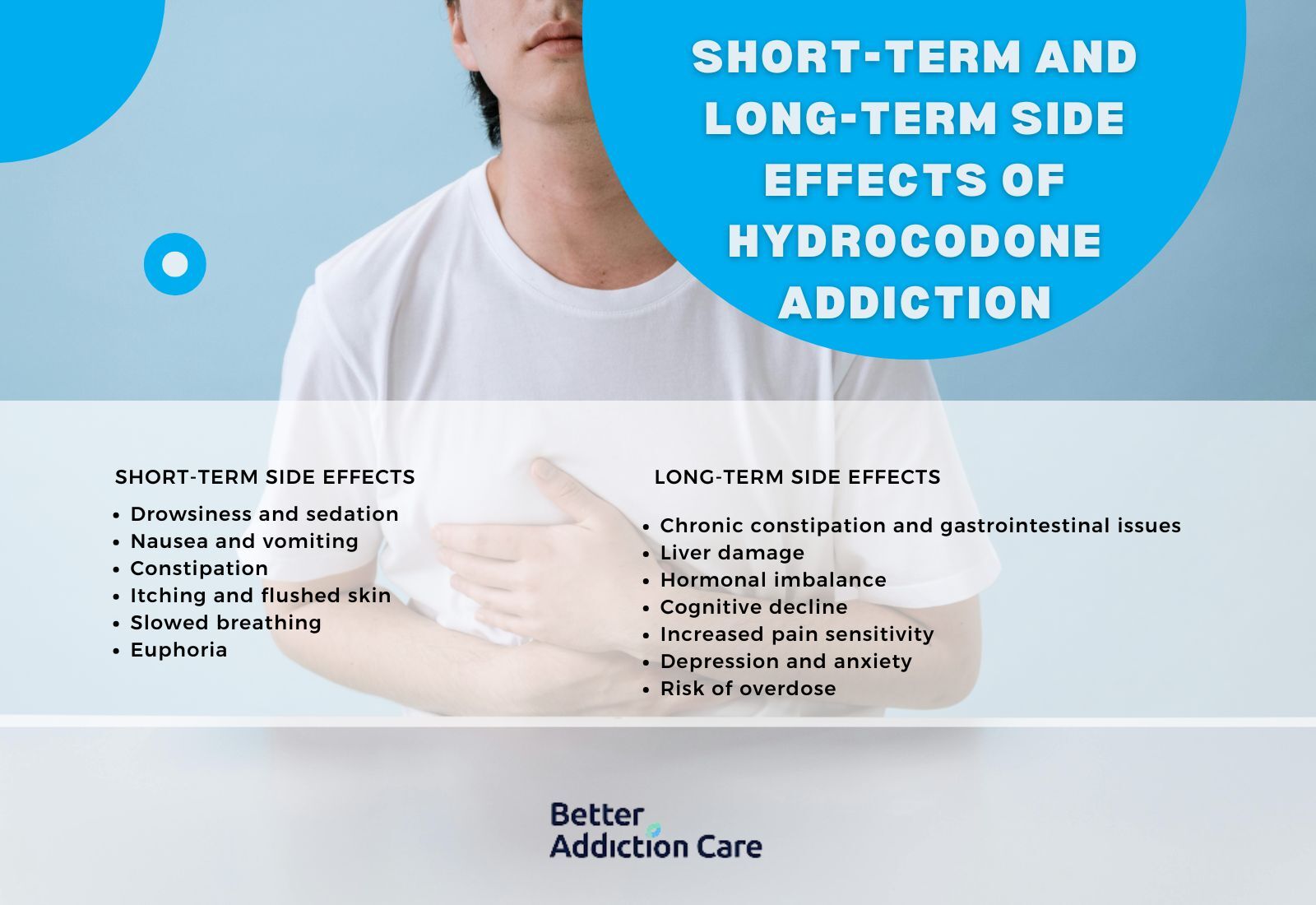
Hydrocodone may begin as a pain reliever, but its effects ripple far beyond pain control. These side effects show up both in the short term—within weeks or months of use—and in the long term, when use continues for years.
Recognizing these risks helps people understand that hydrocodone addiction is not just about dependence, but also about the toll it takes on health, relationships, and overall life quality.
Short-Term Side Effects
In the early stages, side effects may look like inconveniences, but they are warning signs that the body is already under strain.
-
Drowsiness and sedation. Hydrocodone slows the central nervous system, leading to frequent nodding off, difficulty concentrating, and impaired driving or work performance.
-
Nausea and vomiting. Gastrointestinal discomfort is one of the earliest signs of misuse.
-
Constipation. A nearly universal side effect of opioids which can become chronic even with short-term use.
-
Itching and flushed skin. Caused by histamine release, this can be mistaken for allergies but is opioid-related.
-
Slowed breathing. Respiratory suppression is dangerous—it increases the risk of accidental overdose even at therapeutic doses[1].
-
Euphoria. The “high” that makes hydrocodone prone to misuse, reinforcing the brain’s craving cycle[2].
Long-Term Side Effects
When hydrocodone use stretches into months or years, the consequences grow more severe—affecting both body and mind.
-
Chronic constipation and gastrointestinal issues. Long-term opioid users often experience painful, ongoing digestive problems.
-
Liver damage. Many hydrocodone formulations are combined with acetaminophen, which in high doses can cause liver toxicity.
-
Hormonal imbalance. Long-term opioid use can disrupt testosterone, estrogen, and cortisol, leading to fatigue, infertility, or osteoporosis.
-
Cognitive decline. Prolonged use impairs memory, focus, and decision-making—sometimes persisting even after stopping.
-
Increased pain sensitivity. Known as opioid-induced hyperalgesia, where the body becomes more sensitive to pain rather than less[5].
-
Depression and anxiety. Emotional health often worsens over time, reinforcing the cycle of dependence.
-
Risk of overdose. Tolerance builds, driving individuals to take dangerously high doses, sometimes mixing with alcohol or other depressants, which significantly increases overdose risk[1].
Impact on Relationships and Daily Life
The side effects are not only medical—they reshape how someone lives day to day. Missed work, declining school performance, strained relationships, and financial instability often stem directly from hydrocodone misuse.
People may feel helpless as their loved one withdraws, becomes irritable, or struggles with responsibilities.
-
Side effects are more than a list of symptoms—they are signals of progression.
What may start as mild nausea or fatigue can escalate into life-threatening respiratory depression or organ damage if addiction continues unchecked.
For caregivers and relatives, recognizing both the short-term and long-term effects can help distinguish between “just side effects” and red flags that require immediate medical help.
Treatment Options for Hydrocodone Addiction
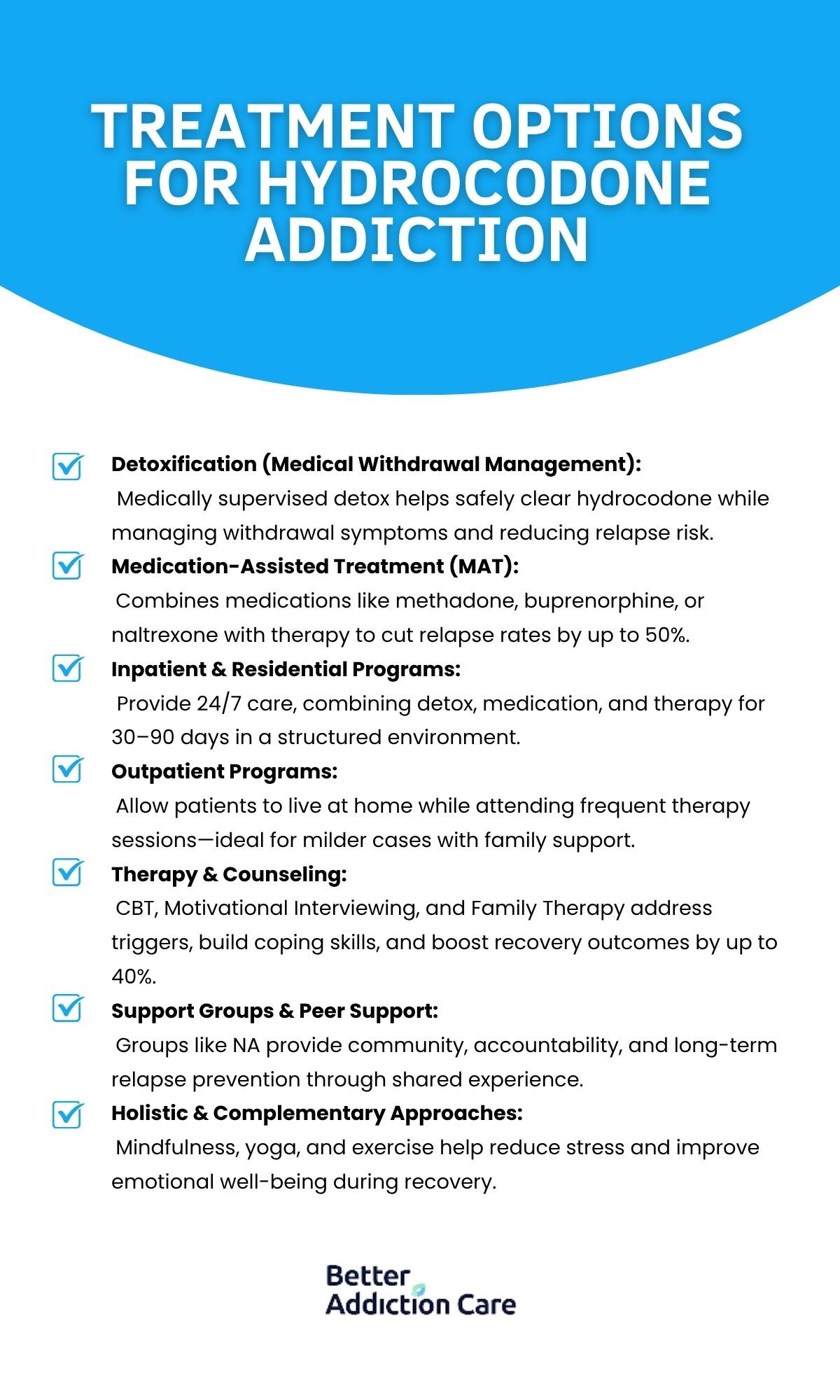
Hydrocodone addiction recovery is possible with the right support and medical guidance. Treatment is not “one-size-fits-all.” The most effective care combines medical, psychological, and social approaches, tailored to the individual’s needs and stage of recovery.
Detoxification (Medical Withdrawal Management)
The first step for many is detox—the process of clearing hydrocodone from the body under medical supervision. Attempting to quit “cold turkey” at home can be dangerous, as withdrawal symptoms are not only painful but may trigger relapse.
In a supervised setting, doctors may use tapering strategies or prescribe medications such as clonidine (to ease anxiety and sweating) or buprenorphine (to reduce cravings and withdrawal symptoms).
According to research, 85% of opioid users report withdrawal within six months, showing just how critical safe management is during this phase[4].
Medication-Assisted Treatment (MAT)
MAT is one of the most evidence-backed approaches for opioid addiction. It combines FDA-approved medications with counselling and Behavioral therapies.
-
Methadone. A long-acting opioid agonist that stabilizes brain chemistry and reduces cravings.
-
Buprenorphine. A partial agonist that eases withdrawal and lowers the risk of misuse.
-
Naltrexone. An opioid antagonist that blocks the euphoric effects of opioids, helping to prevent relapse.
Studies consistently show that MAT can cut relapse rates in half compared to non-medicated approaches[5].
Inpatient & Residential Programs
For individuals with severe addiction or unsafe home environments, inpatient treatment offers 24/7 support. These programs combine detox, therapy, medication, and skill-building in a structured environment.
Stays can range from 30 to 90 days, depending on the program and patient needs.
Outpatient Programs
Outpatient care allows individuals to live at home while attending therapy and medical appointments several times a week. This option is often best for those with strong family support and less severe addiction patterns.
Intensive outpatient programs (IOPs) can provide 9–20 hours per week of structured treatment.
Therapy & Counseling
Addiction is not just physical—it rewires thought patterns and coping strategies. Evidence-based therapies include:
-
Cognitive Behavioral Therapy (CBT): Helps patients recognize triggers and reframe harmful thought patterns.
-
Motivational Interviewing (MI): Encourages personal motivation for change rather than relying on external pressure.
-
Family Therapy: Involves loved ones in recovery, addressing communication breakdowns, and rebuilding trust.
Therapies like these have been shown to improve long-term recovery rates by 25–40% when combined with MAT[5].
Support Groups & Peer Support
Programs like Narcotics Anonymous (NA) or non-12-step alternatives provide ongoing peer support, which can be vital in reducing relapse risk. Having a community of people who understand the challenges creates accountability and belonging.
Holistic & Complementary Approaches
While not a replacement for medical treatment, holistic therapies—such as mindfulness meditation, yoga, and exercise—help address the stress, anxiety, and depression that often accompany recovery. For some, these practices significantly improve quality of life and resilience.
Withdrawal Timeline Detail
One of the hardest parts of recovery is withdrawal—the period when the body and brain struggle to adjust without hydrocodone.
Withdrawal unfolds in two phases:
-
Acute withdrawal (first 3–7 days): Physical symptoms dominate. People may experience muscle aches, nausea, sweating, chills, and severe insomnia[4]. While painful, these symptoms are usually not life-threatening with proper medical support.
-
Protracted withdrawal (weeks to months): Once the physical pain subsides, emotional and psychological challenges often remain. Anxiety, mood swings, fatigue, and intense cravings can linger, sometimes for months[4].
This timeline helps to set realistic expectations: the first week is often the toughest physically, but the longer-lasting psychological symptoms are what make ongoing treatment and support groups so important.
When to Seek Immediate Help?
Certain signs require urgent medical attention, such as:
-
Severe withdrawal symptoms (intense vomiting, dehydration, hallucinations).
-
Suicidal thoughts or self-harm Behaviors.
-
Signs of overdose: slowed breathing, blue lips/fingertips, unresponsiveness.
In these cases, emergency services should be contacted right away.
Hydrocodone addiction is treatable. While relapse may occur—as it does with other chronic illnesses like diabetes or hypertension—each attempt at recovery builds resilience.
Caregivers and individuals should know that progress is often measured in steady improvements, not perfection.
While treatment focuses on breaking free from misuse, it’s equally important to understand how hydrocodone should be used safely in medical settings—and the dangers of overdose when safety steps are ignored.
Dosing & Safety / Overdose Risks
Hydrocodone is typically prescribed in tablet or extended-release formulations, with doses ranging from 10 to 20 mg every 12–24 hours, depending on the severity of pain and patient tolerance[5]. When taken exactly as directed under medical supervision, it can be effective and relatively safe.
The risks rise sharply when pills are taken in higher amounts, combined with alcohol or sedatives, or used without a prescription. An overdose occurs when breathing slows to the point that oxygen can’t reach the brain, a medical emergency that can be fatal without rapid intervention[1].
Families should also know about naloxone, a life-saving medication that can reverse an opioid overdose when administered quickly[5].
Safe practices—such as storing medications securely, never sharing prescriptions, and properly disposing of unused pills—are just as critical in preventing misuse as formal treatment programs.
Conclusion
Hydrocodone addiction is not a sudden fall—it’s a gradual shift that reshapes the body, mind, and daily life.
The journey can feel isolating, but knowing the signs, understanding the causes, and recognizing the risks gives families and individuals the power to step in early.
The truth is clear: addiction is treatable. Millions of people have faced the same fears, taken the first step, and rebuilt their lives. While recovery is rarely a straight path, with the right mix of medical treatment, therapy, and support, lasting healing is possible.
Common questions Related To Hydrocodone Addiction
Yes. Even patients who follow medical instructions may develop tolerance and physical dependence over time. That’s why doctors closely monitor long-term opioid prescriptions and often taper patients off gradually.
The biggest dangers include respiratory depression, overdose, and death. Long-term use can also cause liver damage (especially when combined with acetaminophen), severe constipation, hormonal imbalances, and mental health decline.
Relapse rates for opioid use disorders range from 40–60%, similar to chronic conditions like diabetes or asthma[5]. Relapse doesn’t mean treatment has failed—it signals that the plan may need adjustment, often with stronger support or different medications.
Some people attempt to quit hydrocodone on their own, but the success rate is much lower, and the risk of relapse or overdose is higher. Evidence shows that treatment combining medication, counseling, and social support is far more effective than self-detox.
The most impactful steps families can take include:
- Educating themselves about addiction as a medical condition.
- Encouraging treatment without blame or judgment.
- Offering emotional support and consistency.
- Joining family therapy or support groups to learn coping strategies.
Hydrocodone withdrawal is usually not directly life-threatening, but it can be extremely uncomfortable, causing dehydration, severe anxiety, or suicidal thoughts. Medical supervision is strongly recommended to manage symptoms safely.
Resources
Related Articles
Treatment Centers in New Jersey










