Hydroxyzine Addiction: Uses, Side Effects & Misuse Risks
Hydroxyzine (commonly sold as Atarax or Vistaril depending on formulation) is a first-generation antihistamine with strong sedative and anxiolytic properties.
It blocks histamine H1 receptors and also has anticholinergic and antiadrenergic effects; these central nervous system actions explain its calming and antihistamine effects. Clinically, hydroxyzine is prescribed for:
- Symptomatic relief of anxiety and tension associated with psychoneurosis or organic disease states.
-
Short-term treatment of insomnia when anxiety is a contributory factor.
-
Treatment of pruritus (severe itching) and as an adjunct for allergic conditions.
-
Adjunctive use for nausea and premedication for anesthesia in some settings.
Hydroxyzine exists as hydroxyzine hydrochloride and hydroxyzine pamoate; dosing and formulations differ, but both cross the blood–brain barrier and can cause central sedation. Product monographs and prescribing information note both therapeutic uses and important safety warnings (including QT prolongation risk in overdose). [1]
Key Takeaways
-
Hydroxyzine misuse and psychological dependence can develop when people rely on its sedating or anxiolytic effects. It is not a classic addictive drug, but problematic use and withdrawal-like symptoms are documented.
-
Misuse often begins as self-medication for insomnia or anxiety; social, biological, and prescription-access factors influence risk.
-
Safe discontinuation, clinician-guided tapering, and addressing underlying sleep or anxiety disorders reduce harm and support recovery. Immediate medical evaluation is needed for overdose or dangerous combinations.
Tolerance, Dependence, and Addiction — What’s the Difference?
-
Tolerance — needing higher doses to achieve the same sedating or anxiolytic effect. While tolerance to sedation can occur with repeated hydroxyzine use, it differs from the robust pharmacologic tolerance seen with classic addictive substances.
-
Dependence — physiologic adaptation that leads to symptoms if the medication is stopped abruptly. Withdrawal-like symptoms (e.g., rebound anxiety, insomnia, tremor) have been reported after prolonged hydroxyzine use or abrupt cessation.
-
Addiction — compulsive drug-seeking behavior driven by reward-circuit changes and cravings. Hydroxyzine does not reliably produce euphoria or strong dopamine-mediated reward, so it is not classically addictive in the same way as opioids or stimulants. However, psychological reliance, dose escalation, diversion, and misuse are clinically significant and documented.
Signs & Symptoms of Hydroxyzine Misuse
Physical Signs of Misuse or Overuse

-
Excessive Sedation or Daytime Sleepiness: Taking extra doses or stacking doses for sleep can lead to prolonged daytime drowsiness, impaired attention, and fall risk—especially in older adults.
-
Dizziness, Faintness, or Falls: Anticholinergic and antihistaminic effects (plus orthostatic changes) can cause lightheadedness and falls. Elderly patients are especially vulnerable.
-
Slowed Thinking and Poor Coordination: Overuse can impair reaction time and coordination, increasing accident risk (e.g., while driving).
-
Cardiac Effects (QT Prolongation): In overdose or when combined with other QT-prolonging drugs, hydroxyzine can prolong the QT interval and — rarely — precipitate torsades de pointes. ECG monitoring is advised in suspected overdose.
-
Anticholinergic Symptoms: Dry mouth, constipation, blurred vision, urinary retention — especially at higher doses or in polypharmacy contexts.
Emotional & Psychological Signs
-
Using Hydroxyzine for Self-Medication: People frequently turn to hydroxyzine to calm anxiety, fall asleep, or blunt emotional distress—sometimes without a clear medical indication. This pattern signals misuse when it becomes habitual or is increased without clinician guidance.
-
Preoccupation With the Medication: Worrying about running out, seeking additional supplies, or relying on it nightly despite negative effects indicates problematic use.
-
Irritability or Restlessness When a Dose Is Missed: Abruptly stopping hydroxyzine can produce rebound anxiety, insomnia, or restlessness; patients sometimes interpret these as cravings, which can reinforce continued use.
Behavioral Signs
-
Taking Higher or Altered Doses Without Medical Guidance: Increasing nightly doses, using someone else’s prescription, or taking the medication in ways not prescribed are red flags.
-
Mixing Hydroxyzine With Alcohol or Other Sedatives: Combining with benzodiazepines, opioids, or alcohol greatly increases sedation, respiratory depression risk, and overdose potential. This is a common and dangerous misuse pattern.
-
Doctor Shopping or Pharmacy Irregularities: While less commonly reported than with controlled substances, multiple prescribers, lost prescription reports, or frequent early refills suggest diversion or misuse.[2]
How Common Is Hydroxyzine Misuse?
General Prevalence
Because hydroxyzine is not a controlled substance and is widely prescribed, misuse detection relies on case reports, poison center data, and surveys rather than centralized prescription monitoring.
Several studies and reviews show that nonmedical use of first-generation antihistaminergic anxiolytics (including hydroxyzine) occurs in some populations—frequently as self-medication or as part of polydrug use with opioids or CNS depressants.
In the United States in 2023, hydroxyzine was one of the most commonly prescribed medications, ranking #39 overall with over 15 million estimated prescriptions and an estimated ~4.1 million patients receiving it that year. [3]
Clinical Settings
In hospital and perioperative settings, hydroxyzine is used commonly; errors in dosing or interactions may be underrecognized. In research among people with opioid dependence, hydroxyzine was reported as ever used by 62 % of the sample, with 12 % reporting non-medical use at some point (combined with promethazine and related antihistamines). [2]
Withdrawal Frequency
Hydroxyzine is not classified as a controlled substance and is generally considered to have low potential for classical physical addiction, so standard epidemiological surveys rarely report specific withdrawal prevalence.
Some clinical and anecdotal sources describe mild withdrawal-like symptoms (e.g., anxiety, insomnia, irritability) in a subset of people after long-term or high-dose use, but precise population rates are not established in large surveys.
Controlled clinical trial data in anxiety treatment have shown that hydroxyzine does not consistently produce rebound anxiety or typical withdrawal syndromes when stopped after short-term use, though individual variation exists and long-term use has not been systematically studied. [4]
Causes: Why Does Hydroxyzine Get Misused?
How Hydroxyzine Affects the Brain?
Hydroxyzine blocks central H1 histamine receptors and has anticholinergic and antiadrenergic properties; these actions produce sedation and anxiolysis rather than strong dopaminergic reward. Its calming effect can be emotionally reinforcing for people under acute stress or with insomnia—leading to repeated use.
How Hydroxyzine Interacts With Brain Pathways?
-
Does not reliably stimulate the dopamine reward system → lower risk of classic euphoria-driven addiction.
-
Produces sedation and autonomic modulation → the calming feeling can become behaviorally reinforcing.
-
Anticholinergic and antihistaminic effects can blunt arousal and anxiety quickly → perceived “fast relief” encourages repeated use.
Genetic & Biological Factors
-
Metabolic differences (CYP interactions) can slow hydroxyzine breakdown, causing the drug to stay in the body longer. This increases sedation, next-day drowsiness, and overall sensitivity—especially in people taking other CYP-metabolized medications or those with liver impairment.
-
Coexisting anxiety or insomnia can lead people to rely on hydroxyzine for fast relief. Because it works quickly, it may be used more often during stressful moments or sleepless nights, increasing sensitivity to side effects and withdrawal.
-
Older age or polypharmacy raises the risk of stronger sedation and drug interactions. Aging slows metabolism, and taking multiple medications can amplify drowsiness, confusion, or falls, even at standard doses.
Psychological & Emotional Triggers
Use often begins with a strong desire to regain control—usually over racing thoughts, sleeplessness, or overwhelming anxiety. When hydroxyzine provides quick, almost immediate relief, it can unintentionally condition the brain to rely on it during moments of distress.
This creates a habit loop that’s easy to reinforce:
stress or panic → take hydroxyzine → feel calm → repeat the behavior the next time symptoms appear.
Over weeks or months, this pattern can evolve into a form of psychological dependence, where the medication becomes the default coping strategy. Instead of building emotional resilience or using a variety of calming skills, the person may start to believe that they cannot sleep, relax, or manage stress without it.
For individuals dealing with chronic anxiety, trauma, or intense life stressors, the drive to repeat this cycle is even stronger. Hydroxyzine becomes not just a medication, but a symbol of safety and control, making it harder to reduce or discontinue use even when side effects appear. [5]
Environmental & Social Factors
-
Easy access through active prescriptions or leftover tablets can normalize frequent use. When hydroxyzine is readily available in a medicine cabinet, it becomes a quick, low-effort solution during stressful moments.
-
Borrowing medication from friends or family often starts as a short-term fix for acute insomnia or sudden anxiety. Over time, this informal sharing can reinforce the idea that hydroxyzine is a harmless, convenient option—blurring the line between appropriate use and dependency-driven behavior.
-
Limited access to psychotherapy, CBT-I, or supportive mental-health resources means many people rely solely on medication to manage chronic anxiety or sleep issues. When therapeutic alternatives are unavailable or unaffordable, hydroxyzine naturally becomes the default coping tool.
-
Vague or open-ended instructions such as “take as needed” can lead to unintentional nightly use, higher doses, or taking the medication at the first sign of stress. Without clear boundaries on frequency or duration, people may escalate their use without realizing it, increasing the risk of dependence-like patterns.
From Medical Use to Misuse (Progression)
A typical pattern:
-
Hydroxyzine is prescribed (or used) for anxiety, itching, or occasional insomnia.
-
The user notices rapid calming and easier sleep.
-
On stressful nights, they take an extra tablet “just once.”
-
Over weeks to months, extra dosing becomes routine to guarantee sleep or calm.
-
Missing a dose produces rebound symptoms (insomnia, anxiety) that prompt more frequent use.
This creates an emotional/behavioral reliance loop—stress → hydroxyzine → temporary relief → higher dosing—driven largely by the medication’s sedative utility rather than a drug-induced euphoric high.
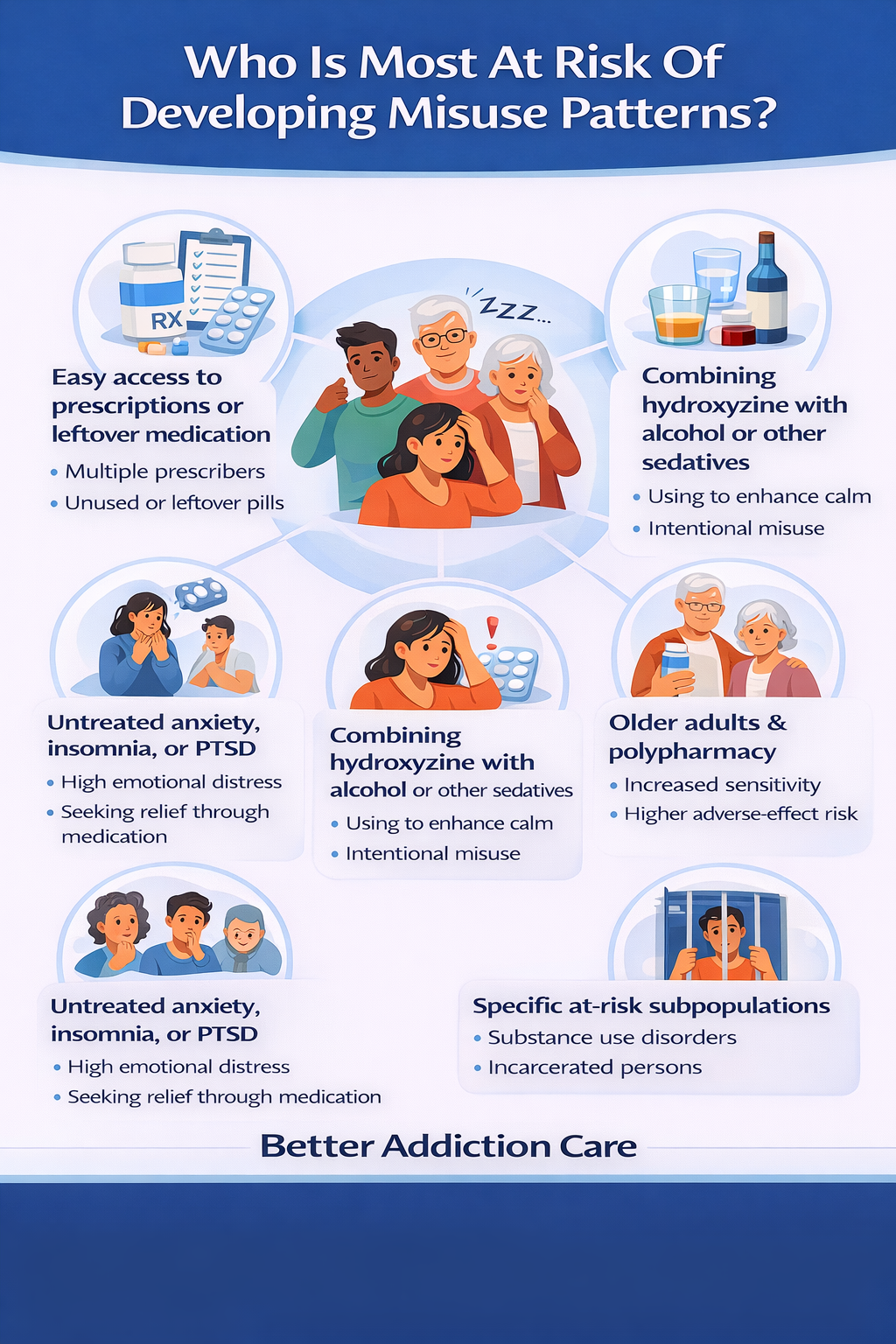
Who Is Most At Risk Of Developing Misuse Patterns?
-
Individuals with untreated or undertreated anxiety, panic disorder, PTSD, or chronic insomnia.
-
People with easy access to prescriptions, leftover medication, or multiple prescribers.
-
Patients who combine hydroxyzine with alcohol or other sedatives intentionally to enhance calm.
-
Older adults and those with polypharmacy (increased sensitivity and adverse-effect risk).
-
Specific subpopulations—such as incarcerated persons or those with substance use disorders—have been reported to use sedating antihistamines nonmedically.
Side Effects of Hydroxyzine
Short-Term Side Effects
-
Sedation and somnolence — These are the most common effects and are strongly dose-related. Many people experience noticeable drowsiness within 30–60 minutes of taking the medication.
-
Dizziness and orthostasis — Lightheadedness, unsteadiness, or a drop in blood pressure may occur, especially when starting treatment or increasing the dose. Standing up too quickly can intensify these symptoms.
-
Anticholinergic effects — Dry mouth, constipation, urinary hesitancy, and blurred vision can appear shortly after dosing. While usually mild, they may be more bothersome in sensitive individuals.
-
Impaired coordination and slowed reaction times — These motor effects mean people should be cautious about driving, operating machinery, or performing tasks requiring alertness, particularly during the first few days of use.
Long-Term Side Effects
-
Cognitive slowing and daytime impairment — Consistent nightly use or higher-than-recommended doses can lead to memory issues, reduced focus, or feeling mentally “foggy” during the day. This is especially noticeable in individuals using hydroxyzine as a sleep aid.
-
Cardiac effects — Hydroxyzine can prolong the QT interval, increasing the risk of arrhythmias such as torsade de pointes in cases of high doses, overdose, or when combined with other QT-prolonging drugs. Product monographs explicitly warn about this risk, particularly in people with underlying cardiac conditions or electrolyte abnormalities.
-
Anticholinergic burden over time — Although hydroxyzine is not the most potent anticholinergic agent, chronic use contributes to cumulative exposure. In older adults, long-term anticholinergic load is associated with cognitive decline and increased dementia risk in observational studies. The relevance depends on dose, frequency, and total duration of use.
-
Polypharmacy-related harms — Combining hydroxyzine with other sedatives—such as opioids, benzodiazepines, alcohol, muscle relaxants, or other antihistamines—can lead to additive sedation, slowed breathing, and increased risk of accidental overdose. This is particularly concerning in individuals with chronic pain, anxiety disorders, or insomnia who may already be on multiple CNS-depressant medications.
Impact on Daily Life
-
Daytime sleepiness and reduced alertness can interfere with nearly every aspect of functioning — from concentration at work or school to safe driving. Even modest nighttime doses may cause next-day grogginess, slowed reaction times, and decreased productivity.
-
Reliance on medication for sleep can unintentionally block progress with healthier, more sustainable sleep strategies. When someone depends on hydroxyzine to fall asleep, they may not engage in behavioral approaches like CBT-I, stimulus control, sleep scheduling, or relaxation training — all of which lead to long-term improvement without medication.
-
Chronic use can complicate management of existing health conditions, especially in older adults. Anticholinergic effects such as urinary retention, constipation, dry mouth, and blurred vision can worsen baseline issues (e.g., prostate enlargement, chronic constipation, glaucoma). Over time, these side effects may trigger new medical appointments, additional medications, or reduced quality of life. [6]
Treatment Considerations When Misuse Or Problematic Patterns Appear
Because hydroxyzine misuse is different from classical substance addictions, treatment emphasizes safe medication management, addressing underlying anxiety/insomnia, and reducing dangerous polydrug use.
Detox / Withdrawal Management
Hydroxyzine “withdrawal” is typically less severe than benzodiazepine or alcohol withdrawal but can be uncomfortable. Symptoms may include rebound anxiety, insomnia, tremor, sweating, headache, or nausea. Clinicians decide on outpatient vs inpatient care based on psychiatric stability and overdose risk. Abrupt cessation can worsen insomnia and anxiety—structured tapering reduces these problems.
Supports:
-
Structured tapering: Gradual dose reduction to limit rebound.
-
Adjunct medications: Non-addictive sleep aids or short-term alternatives may be used to manage acute insomnia under medical supervision.
-
Monitoring: Regular check-ins to assess sleep, anxiety, and risk of relapse into sedative combinations.
-
Stabilization planning: Identify triggers and create behavioral alternatives.
Medication-Assisted Strategies (Not Traditional MAT)
Hydroxyzine is not an opioid, so traditional MAT does not apply. Clinicians may use:
-
SSRIs/SNRIs or buspirone for underlying anxiety disorders.
-
Melatonin or nonbenzodiazepine hypnotics (short-term) when indicated.
-
Sleep-focused CBT (CBT-I) as a nonpharmacologic mainstay. [1]
Levels of Care
-
Inpatient/Residential — for severe psych instability, dangerous polydrug use, or high overdose risk.
-
Intensive Outpatient Programs (IOP) — structured therapy, psychiatric checks, and relapse prevention.
-
Standard Outpatient Care — weekly or biweekly therapy plus medication management for long-term support.
Therapies
Behavioral therapies help break reliance on sedating medications.
-
CBT (Cognitive Behavioral Therapy) for anxiety and insomnia — reduces need for medication by building sleep and coping skills.
-
Motivational Interviewing (MI) — helps with ambivalence and building motivation for change.
-
Family Therapy — supports household communication, safe medication storage, and monitoring for diversion.
Therapy focuses on coping skills, relapse prevention, and reducing dependence on sedation for emotional comfort.
Peer Support & Recovery Capital
Peer groups and community supports reduce isolation and strengthen recovery. Options include:
-
SMART Recovery and peer-led mental health groups.
-
Local anxiety or sleep disorder support groups.
-
Community wellness resources that promote routine, exercise, and social connection.
These resources reinforce behavioral strategies and offer accountability.
Holistic Supports (Adjunct Care)
-
Mindfulness and meditation to reduce stress without sedatives.
-
Exercise routines to improve sleep quality and mood.
-
Sleep hygiene practices to prevent nighttime anxiety and reduce medication reliance.
-
Balanced nutrition and hydration to maintain energy and support physical health.
-
Breathing techniques and relaxation exercises for acute anxiety management.
Stabilization & Immediate Safety
Assess for acute toxicity or dangerous combinations (e.g., heavy alcohol or opioid co-ingestion). Emergency management focuses on airway, breathing, circulation, and supportive care. Hydroxyzine overdose may require ECG monitoring for arrhythmia; there is no specific antidote.
Tapering And Discontinuation Management
Slow, clinician-guided tapering is recommended to minimize rebound anxiety and insomnia. There is no universal taper schedule—clinicians individualize depending on dose and duration. Proactive planning, sleep supports, and alternative anxiolytic strategies reduce discontinuation symptoms and relapse risk.
Withdrawal / Discontinuation Timeline — What To Expect?
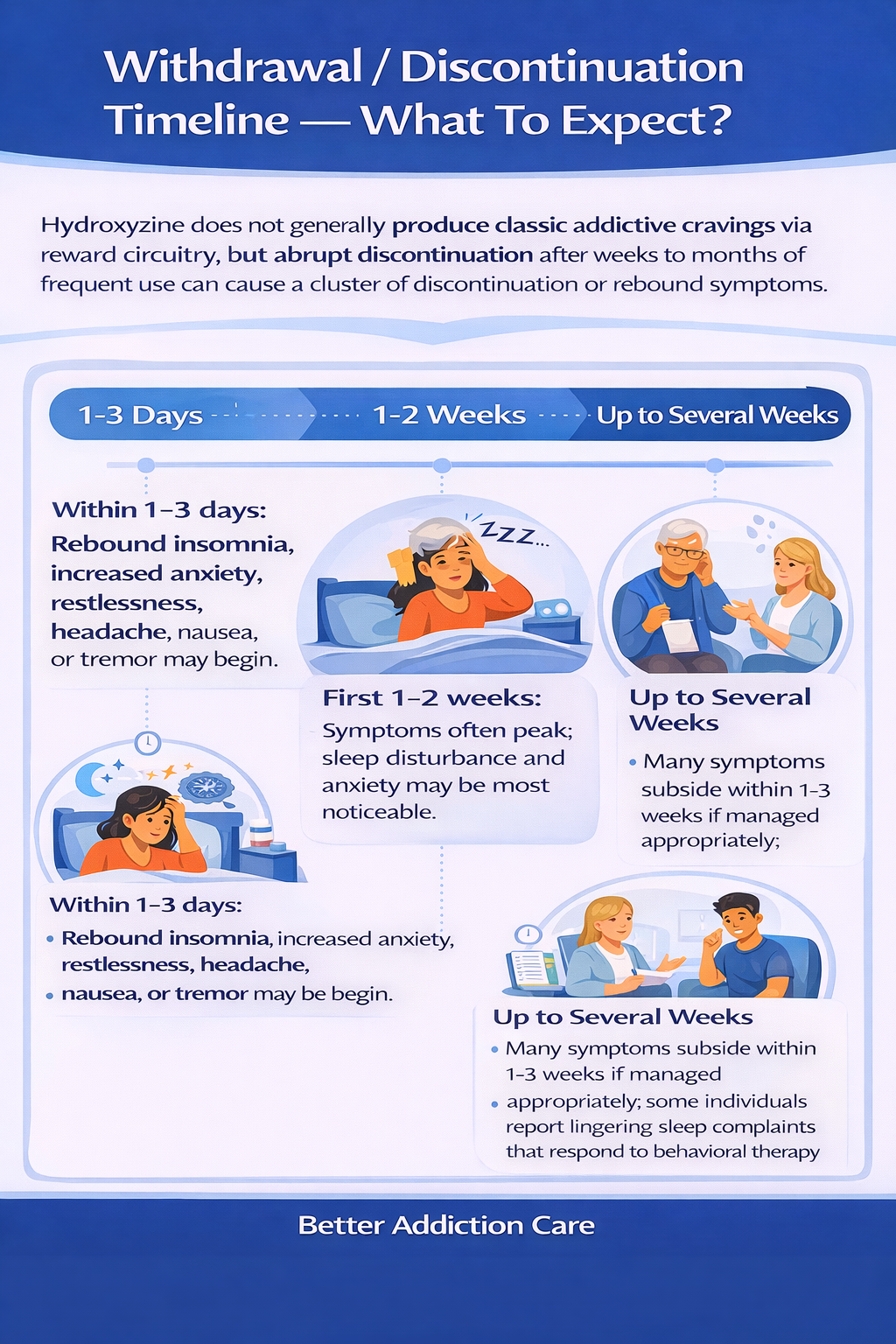
Hydroxyzine does not generally produce classic addictive cravings via reward circuitry, but abrupt discontinuation after weeks to months of frequent use can cause a cluster of discontinuation or rebound symptoms.
Typical pattern seen:
-
Within 1–3 days: rebound insomnia, increased anxiety, restlessness, headache, nausea, or tremor may begin.
-
First 1–2 weeks: symptoms often peak; sleep disturbance and anxiety may be most noticeable.
-
Up to several weeks: many symptoms subside within 1–3 weeks if managed appropriately; some individuals report lingering sleep complaints that respond to behavioral therapy and sleep hygiene. Rare severe cardiac events are generally related to overdose or drug interactions rather than discontinuation.
When To Seek Immediate Help?
Seek urgent care or emergency services if:
-
Severe difficulty breathing, loss of consciousness, or severe hypotension occurs (possible in overdose or dangerous combinations).
-
Severe chest pain, fainting, or neurologic changes (evaluate for cardiac or neurologic emergencies).
-
Severe agitation, suicidal ideation, or psychotic symptoms — urgent psychiatric evaluation is needed.
-
Signs of arrhythmia (palpitations, syncope) — seek emergency care and ECG monitoring.
Dosing & Safety / Overdose Risks
Typical Therapeutic Ranges & Formulations
Hydroxyzine dosing varies by indication: lower single doses for pruritus or mild anxiety, divided dosing for more severe symptoms, and larger IM doses used acutely in some medical settings. Clinicians individualize dosing by age, comorbidity, and drug interactions. Product monographs and prescribing information should be consulted.
High-Risk Combinations
Alcohol, benzodiazepines, opioids, and other CNS depressants amplify hydroxyzine’s sedating effects and can increase the risk of respiratory depression, coma, or death. QT-prolonging drugs (certain antipsychotics, some antidepressants, antiarrhythmics) increase arrhythmia risk when combined with hydroxyzine.
Overdose Mechanism
Overdose can cause extreme drowsiness, confusion, anticholinergic toxicity (dry mouth, hyperthermia, urinary retention), hypotension, and cardiac arrhythmias including torsade de pointes. ECG monitoring and supportive care are essential; hemodialysis is unlikely to be helpful.
Safe Use Practices
-
Store medication securely to prevent access by children, teens, or individuals with substance misuse risk.
-
Do not share tablets or take more than prescribed.
-
Avoid alcohol and other sedatives while using hydroxyzine.
-
Inform prescribers about all medications, supplements, and cardiac history before starting hydroxyzine.
-
Dispose of unused medication through take-back programs when available.
Conclusion
Hydroxyzine is an effective medication for allergies, itching, anxiety, and as an adjunct in medical settings when used appropriately. Although it is not highly addictive in the classic sense, psychological dependence, dose escalation, and withdrawal-like symptoms can occur.
Safe use means taking hydroxyzine only as prescribed, avoiding routine nightly use for insomnia without further assessment, monitoring for cardiac or anticholinergic side effects, and tapering gradually under medical guidance if discontinuing.
If you or someone you care about is using hydroxyzine irregularly, taking extra doses, or is worried about stopping:
-
Talk to your prescriber openly about how you use the medication and any other substances.
-
Do not stop suddenly; follow a taper plan with a clinician.
-
Use non-drug strategies for sleep and anxiety (CBT-I, sleep hygiene, therapy).
-
Seek medical evaluation for concerning side effects (excessive sedation, falls, palpitations, signs of metabolic or anticholinergic problems).
FAQs
Hydroxyzine is not classically addictive (it does not reliably cause euphoria or strong dopamine-mediated reinforcement) and is not a controlled substance. However, psychological dependence and problematic patterns of use have been reported, and abrupt discontinuation can cause rebound symptoms. So “not addictive” does not mean “risk-free.”
The most serious dangers occur when hydroxyzine is combined with alcohol, opioids, or benzodiazepines (increased sedation and respiratory depression) or with drugs that prolong QT interval (risk of torsade de pointes). Overdose can lead to severe sedation, cardiac arrhythmias, and anticholinergic toxicity.
“Relapse” into problematic sedative use often reflects return of underlying anxiety, sleep problems, or environmental stressors. It indicates a need to re-evaluate the treatment plan rather than personal failure. Behavioral strategies, monitored tapering, and psychotherapy reduce relapse risk.
Stopping abruptly can cause rebound insomnia and anxiety. While hydroxyzine withdrawal is usually less medically dangerous than alcohol or benzodiazepine withdrawal, stopping suddenly may be uncomfortable and destabilizing. A clinician-guided taper is safer.
Families can help by learning the signs of misuse, offering nonjudgmental support, encouraging therapist or prescriber contact, helping secure medications, and assisting with behavioral sleep strategies. Observing warning signs early can prevent escalation.
Hydroxyzine withdrawal is rarely life-threatening by itself. Overdose or severe interactions (e.g., with opioids) can be life-threatening. Supervised tapering and monitoring to minimize risk.
Resources
Related Articles
Treatment Centers in New York










