is ibogaine Addictive? Causes and Side Effects
Ibogaine is a psychoactive alkaloid derived from the Tabernanthe iboga plant, traditionally used in ceremonial contexts in Central and West Africa. In modern contexts, it is used—usually outside the United States—in unregulated clinics for opioid withdrawal and other substance-related concerns.

In the U.S., ibogaine is a Schedule I controlled substance, meaning it is illegal to possess, manufacture, or use it for medical treatment[1].
Ibogaine does not cause chemical addiction:
-
It does not stimulate dopamine reward pathways
-
It does not create cravings
-
It does not produce tolerance
-
It does not cause physical dependence
-
It does not produce withdrawal symptoms
Key Takeaways
- Ibogaine is not chemically addictive but risky. Misuse stems from psychological reliance, emotional vulnerability, or repeated attempts to “reset” substance use rather than true physiological dependence.
- Serious medical and legal risks exist. Cardiovascular complications, neurological effects, and psychological strain are common, especially in unregulated settings. Ibogaine is Schedule I in the U.S., making possession or use illegal.
- Safer, evidence-based recovery options are available. Medication-assisted treatment (MAT), behavioral therapies, structured care, and peer support provide medically supervised, effective, and sustainable pathways to long-term recovery.
However, people may still use ibogaine in unsafe, repeated, or compulsive patterns, driven by:
-
desperation to stop opioid withdrawal
-
belief in online claims of rapid detox
-
psychological attraction to psychedelic experiences
-
fear of traditional treatment
-
repeated relapse cycles
For this reason, “ibogaine addiction” is best understood as a pattern of risky misuse, rather than true chemical dependency. Ibogaine cannot create physiological addiction, but unsafe behavioral patterns can still develop.
Signs & Symptoms of Ibogaine Misuse
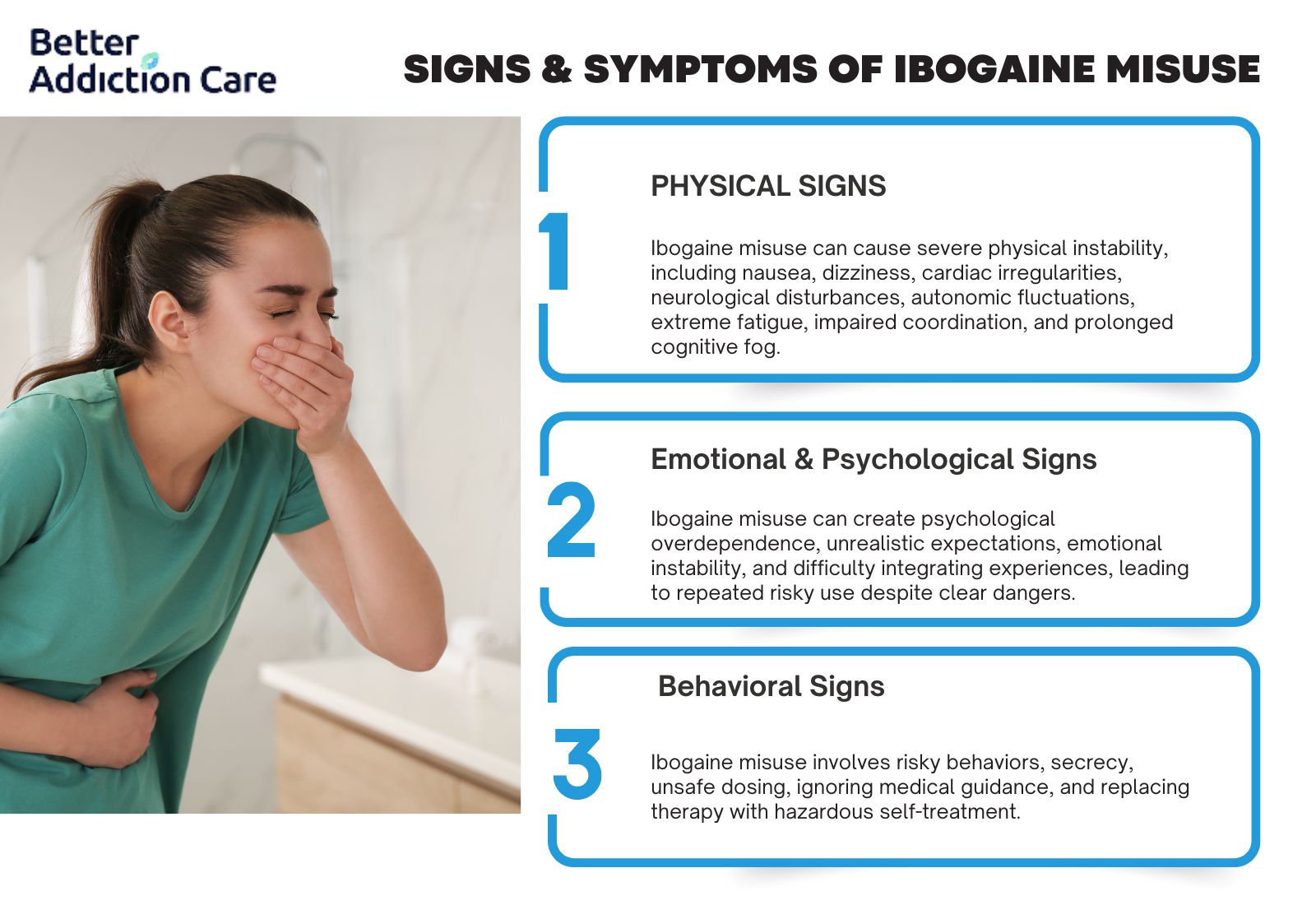
Ibogaine produces intense psychoactive effects and significant medical risks. Misuse does not look like substance addiction; instead, it presents as unsafe behavior, psychological overreliance, or medical complications.
Physical Signs
-
Nausea and vomiting during or after use
-
Severe dizziness or inability to stand without support
-
Rapid or irregular heartbeat, sometimes described as “fluttering”
-
Chest pain or tightness, often related to arrhythmias
-
Blood pressure instability (sudden drops or spikes)
-
Severe fatigue lasting 12–48 hours post-session
-
Tremors or muscle stiffness
-
Visual disturbances, flashbacks, or perceptual distortions
-
Poor coordination during and after use
-
Fainting or near-fainting episodes
-
Sweating, chills, and temperature swings
-
Extended sleep episodes, sometimes lasting 12–24 hours
-
Lingering cognitive fog for days or weeks
These symptoms are not signs of addiction—they indicate toxicity, cardiac strain, or neurological disruption.
Emotional & Psychological Signs
-
Overreliance on the “reset” experience
-
Belief that ibogaine is the only thing that can stop withdrawal
-
Repeating treatments despite medical risks
-
Dissociation, emotional detachment, or blunted affect
-
Heightened anxiety after treatment, especially if relief fades
-
Unrealistic expectations, e.g., expecting a “permanent cure”
-
Panic when withdrawal returns, prompting unsafe dosing choices
-
Increased irritability or mood swings
-
Confusion or difficulty integrating hallucinations
-
Emotional crashes following intense psychedelic episodes
These psychological symptoms may lead people to seek repeated sessions despite significant risk.
Behavioral Signs
-
Traveling repeatedly to unregulated clinics
-
Scheduling multiple ibogaine treatments in short intervals
-
Using ibogaine without medical screening
-
Hiding ibogaine use from healthcare providers or family
-
Attempting to import or self-source ibogaine illegally
-
Abandoning safer evidence-based treatments
-
Mixing ibogaine with other substances, especially opioids
-
Ignoring contraindications such as heart disease or use of SSRIs
-
Self-medicating trauma with psychedelics rather than therapy
-
Relying on online groups promoting ibogaine as a “cure”
These patterns reflect risk-taking behavior, not addiction.
How Common Is It?
General prevalence: Ibogaine use is rare in the U.S.
Because ibogaine is illegal and carries life-threatening risks, usage rates are extremely low. Most individuals who pursue ibogaine travel to countries where clinics operate without FDA standards. Studies suggest a small but growing number of Americans travel abroad each year seeking ibogaine-assisted detox [2].
Ibogaine is not tracked by U.S. prescribing or surveillance systems because:
-
It is Schedule I
-
It has no medical use
-
No legal prescribing pathway exists
-
No addiction monitoring system lists it
Clinical Settings: Who Typically Seeks Ibogaine Treatment?
Patients who pursue ibogaine often share:
-
histories of failed opioid detox attempts
-
strong fear of withdrawal
-
dissatisfaction with MAT
-
reluctance to use methadone or buprenorphine
-
exposure to online ibogaine testimonials
-
interest in psychedelic-assisted “reset” experiences
-
high relapse frequency
-
limited access to therapy or structured care
Common characteristics:
-
Age 25–55
-
History of opioid dependence
-
Multiple previous treatment episodes
-
Financial strain due to relapse cycles
-
Past trauma or emotional distress
-
Unstable access to primary care
Why is this population vulnerable?
Ibogaine’s marketing as a “one-time detox” appeals to individuals already experiencing:
-
exhaustion
-
hopelessness
-
frustration with long-term recovery models
-
fear of withdrawal
-
difficulty accessing stable care
This makes them more prone to seek rapid, unregulated solutions.
Withdrawal frequency: Ibogaine withdrawal = 0%
Ibogaine:
-
does not cause withdrawal
-
does not create dependence
-
does not produce cravings
But withdrawal from the original substance—usually opioids—resurfaces quickly.
Research shows ibogaine’s effects on opioid withdrawal are temporary. Many individuals experience:
-
return of withdrawal in 24–72 hours
-
emotional instability
-
cravings returning
-
physical rebound
-
confusion when the “reset” feeling fades
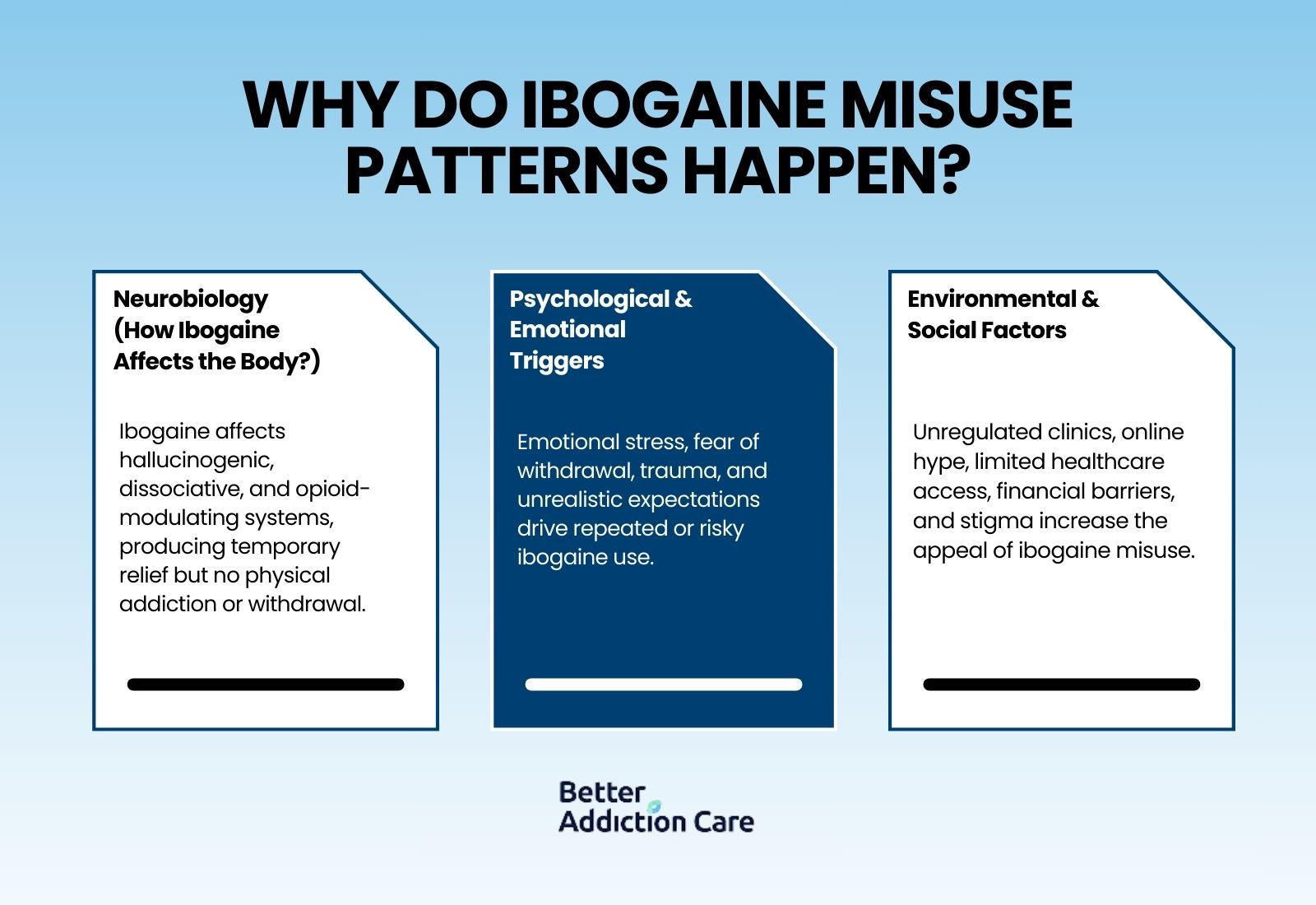
Causes: Why do ibogaine misuse patterns happen?
Ibogaine misuse does not emerge from chemical dependence. Instead, it develops from psychological reinforcement, emotional vulnerability, and environmental pressures—often experienced by individuals who feel stuck, desperate, or unsupported in their recovery.
Neurobiology (How Ibogaine Affects the Body?)
Ibogaine produces a unique combination of hallucinogenic, dissociative, and opioid-modulating effects. These sensations can create a sense of emotional relief or “psychological reset,” which some individuals seek repeatedly even though ibogaine itself is not addictive.
Ibogaine affects several biological systems:
-
NMDA receptors → powerful dream-like hallucinations, dissociation, and memory distortion, which some interpret as “insightful” or therapeutic.
-
Serotonin transporters → shifts in mood, perception, and emotional processing that temporarily reduce distress or craving-like feelings.
-
Kappa-opioid receptors → short-term relief from opioid withdrawal symptoms, which can motivate repeated attempts to self-treat.
-
Cardiac ion channels → QT-interval prolongation and arrhythmia risk, making repeated use medically dangerous.
Key distinctions that prevent addiction from forming:
-
No tolerance buildup — the body does not require escalating doses to achieve the same effects.
-
No compulsive dopamine-driven reinforcement — ibogaine does not stimulate the reward pathway that underlies addiction[2].
-
No withdrawal syndrome — stopping ibogaine does not produce physical dependence symptoms.
-
No habit-forming reinforcement loop — people do not develop cravings or compulsive use.
However, psychological reinforcement can occur when individuals become attached to the idea that ibogaine provides answers, clarity, or a fast reset.
Psychological & Emotional Triggers
Most ibogaine misuse starts with emotional drivers rather than chemical ones. People often turn to ibogaine during periods of fear, overwhelm, or desperation.
Misuse is more likely when individuals:
-
Fear opioid withdrawal intensely and seek anything that promises relief without long-term medication.
-
Feel hopeless after multiple relapses and see ibogaine as a final option.
-
Desire a rapid solution that bypasses the time required for structured treatment.
-
Want to avoid long-term medications such as buprenorphine or methadone due to stigma or misunderstanding.
-
Crave emotional clarity or insight after trauma, grief, or major life changes.
-
Perceive ibogaine as a guaranteed “cure” based on testimonials and anecdotal claims.
-
Spend significant time in online recovery forums where dramatic stories create unrealistic expectations.
-
Have untreated trauma that drives impulsive or experimental decisions.
-
Are influenced by psychedelic communities that frame ibogaine as a spiritual or transformative tool.
These psychological patterns can lead to repeated or risky use, even without physiological addiction.
Environmental & Social Factors
Outside pressures also play a major role in shaping ibogaine misuse patterns. Many people pursue ibogaine because they feel limited or unsupported by traditional healthcare systems.
Common environmental and social drivers include:
-
Unregulated clinics promoting ibogaine as a cure, often with limited medical screening and no emergency resources.
-
Viral online content portraying dramatic transformations that obscure risks.
-
Peer influence in harm-reduction circles, where ibogaine is sometimes viewed as an alternative pathway for detox.
-
Long waitlists for inpatient treatment, causing people to seek immediate options outside the medical system.
-
Financial barriers that make long-term, evidence-based treatment feel inaccessible.
-
A strong cultural preference for “natural” or plant-based therapies, increasing willingness to try undocumented treatments.
-
Limited access to primary-care providers, leaving people to self-treat with information from online sources.
-
Social stigma around MAT, driving individuals toward ibogaine as a way to avoid being seen as “on medication.”
These factors often combine to make ibogaine appear more appealing than medically approved treatments, despite its well-documented risks.
From Initial Use to Risky Patterns (Progression)
Ibogaine does not create chemical dependence, but people can still develop risky usage patterns driven by psychological reinforcement, withdrawal fear, or repeated attempts to “reset” their substance use. Progression happens through behavior and emotion—not biology.
Typical Pattern of Escalation:
-
Curiosity or Desperation: Individuals research ibogaine after struggling with relapse, withdrawal distress, or failed conventional treatment.
-
Seeking a “Safe Reset”: Books treatment abroad or online, believing ibogaine is a safer alternative to opioids or other addictive substances.
-
Short-Term Relief: Experiences a temporary reduction in withdrawal symptoms, creating a sense of hope and reward.
-
Perceived Emotional Clarity: Hallucinogenic or introspective effects are interpreted as psychological insight or a breakthrough.
-
Return of Withdrawal Symptoms: Within days to weeks, opioid or substance withdrawal symptoms resume.
-
“Need Another Session” Belief: Person develops the idea that repeated ibogaine sessions are required to maintain relief or prevent relapse.
-
Planning Repeat Use: Begins scheduling or seeking multiple treatments, increasing exposure risk.
-
Cumulative Health Risks: Repeated sessions elevate the risk of cardiac complications, arrhythmias, or interactions with other medications.
-
Behavioral Entrapment: Cycle is reinforced by psychological expectations and perceived benefits, not by tolerance or chemical dependence.
Who Is Most at Risk of Developing Ibogaine Misuse Patterns?
Certain individuals are more vulnerable to risky or repeated ibogaine use, especially when support, guidance, or medical supervision is limited. Risk factors are behavioral, psychological, and situational rather than biological dependence.
Populations at Higher Risk:
-
Severe or Untreated Opioid Withdrawal: Those experiencing intense withdrawal symptoms may pursue ibogaine as a desperate alternative.
-
Frequent Relapse Histories: Individuals who repeatedly relapse may see ibogaine as a “quick fix” rather than engaging in long-term recovery planning.
-
Co-Occurring PTSD or Trauma: Adults managing unresolved trauma may interpret hallucinogenic experiences as emotional breakthroughs, increasing the likelihood of repeat sessions.
-
Fear of Medication-Assisted Treatment (MAT): Those hesitant to use methadone, buprenorphine, or other MAT options may self-direct toward ibogaine.
-
Non-Responsive to Traditional Detox: Individuals who have not succeeded with inpatient or outpatient detox programs may escalate risk by seeking alternative treatments.
-
Influenced by Online Testimonials: Exposure to anecdotal success stories or social media hype can create unrealistic expectations and reinforce repeated use.
-
Pre-Existing Cardiac Conditions: Adults with heart disease or arrhythmias face higher medical risks, making unsupervised sessions particularly dangerous.
-
Lack of Structured Recovery Support: Those without counseling, peer support, or follow-up care are more likely to repeat sessions impulsively.
-
Limited Medical Access or Insurance: Individuals without reliable healthcare oversight may attempt high-risk treatments to self-manage withdrawal or cravings.
Side Effects of Ibogaine
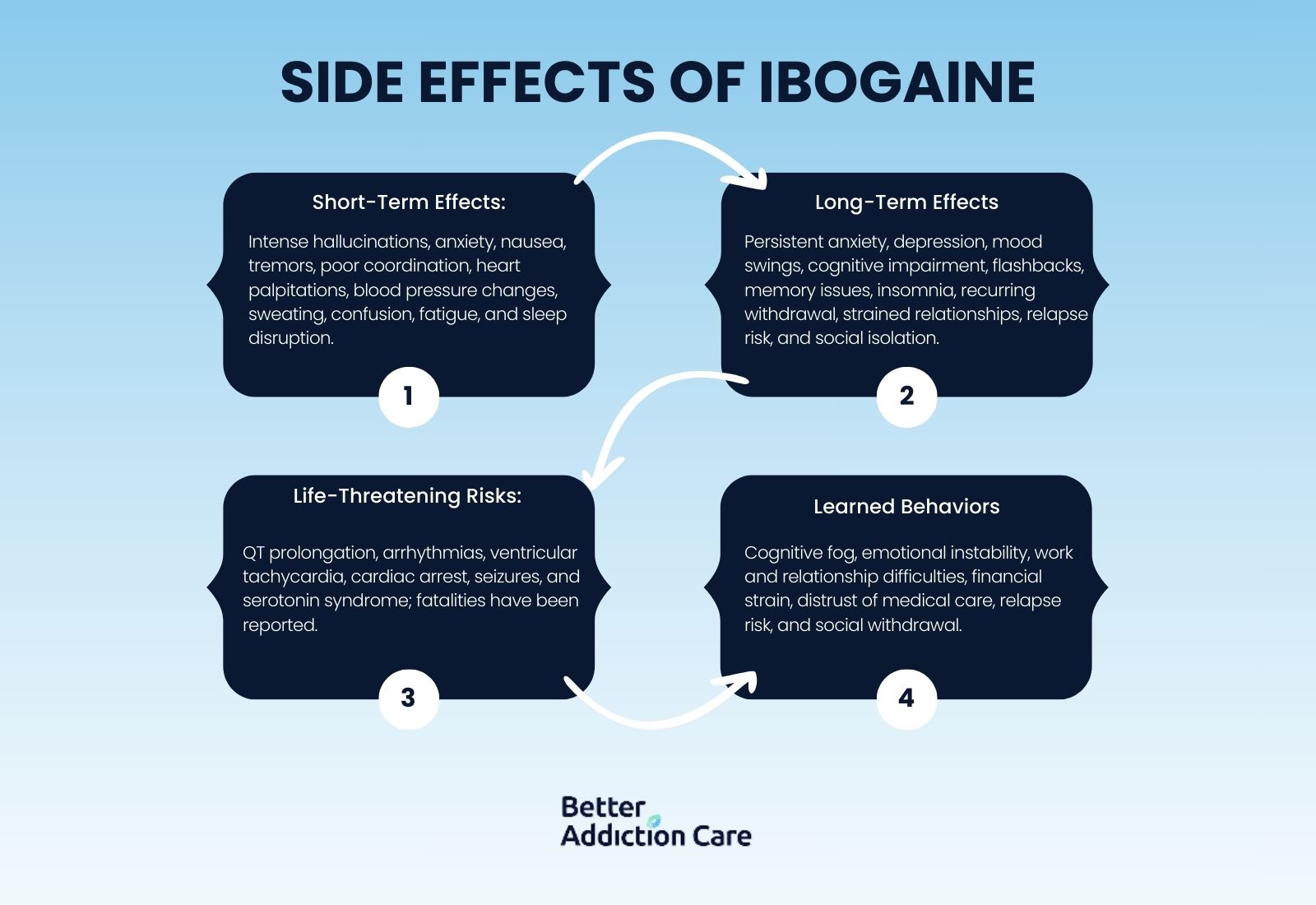
Short-Term Side Effects
These are the effects most commonly reported during or shortly after an ibogaine session:
-
Intense hallucinations (6–12 hours) — Ibogaine is strongly psychoactive, with long sessions of visions, introspection, and altered consciousness.
-
Anxiety, panic, or agitation — Users often report psychological distress, especially during the “come-up” or peak.
-
Vomiting/nausea — Common in many case reports.
-
Tremors or muscle stiffness — Some physical agitation or neuromotor disruption may occur.
-
Poor coordination/ataxia — Case notes and observational reports mention ataxia (lack of muscle coordination).
-
Heart palpitations/arrhythmias — Cardiovascular effects are well-documented.
-
Blood pressure fluctuations — Both hypotension and hypertension can occur.
-
Sweating, chills, or fever — Autonomic symptoms are common in intense psychedelic sessions.
-
Confusion or disorientation — The hallucinogenic experience, plus fatigue, can impair coherence.
-
Severe fatigue — After the session, many feel deeply exhausted.
-
Sleep disturbances — Disrupted sleep is frequently reported.
Long-Term Side Effects
Use caution when interpreting these:
-
Persistent anxiety or depression — Some people report long-lasting mood dysregulation after ibogaine.
-
Emotional blunting/mood swings — Emotional highs and lows, or feeling “flat,” are reported in user self-reports.
-
Cognitive impairment / “brain fog” — Difficulty concentrating, memory issues, or slower thinking are described.
-
Flashbacks or visual disturbances — There are anecdotal accounts of persistent perceptual changes.
-
Memory problems — Some users mention long-term memory deficits.
-
Post-treatment insomnia — Sleep problems can continue for days or weeks.
-
Recurrence of opioid withdrawal symptoms — Because ibogaine doesn’t eliminate dependence biologically, withdrawal may come back.
-
Strain on relationships — The intensity of the experience or changes in behavior can stress personal relationships.
-
Increased relapse risk — Without proper follow-up, some return to substance use.
-
Social/psychological isolation — Following treatment, some report feeling different, detached, or mistrustful of previous support systems.
Life-Threatening Risks
Ibogaine’s most dangerous effects occur in the cardiovascular system:
-
QT interval prolongation, raising arrhythmia risk
-
Ventricular tachycardia
-
Cardiac arrest
-
Sudden death
-
Seizures
-
Serotonin syndrome (when mixed with SSRIs)
Case reports document multiple fatalities linked to ibogaine use[2].
Impact on Daily Life
-
Difficulty returning to work
-
Cognitive fog interfering with decision-making
-
Emotional instability
-
Fear after experiencing hallucinations
-
Distrust of established medical care
-
Strained family relationships
-
Lost finances due to travel or repeated sessions
-
Confusion when ibogaine does not “cure” addiction
-
Increased relapse risk
-
Social withdrawal
-
Overinvolvement in psychedelic communities
These impacts can derail recovery if not addressed early.
Treatment Options
Medication-Assisted Treatment (MAT)
MAT is the gold standard for opioid use disorder and post-ibogaine stabilization:
Common Medications:
-
Buprenorphine — reduces cravings and withdrawal intensity.
-
Methadone — long-acting opioid agonist to stabilize daily function.
-
Naltrexone (Vivitrol) — opioid antagonist that blocks effects and supports relapse prevention.
Benefits of MAT:
-
Reduces cravings and withdrawal discomfort
-
Stabilizes mood and functioning
-
Lowers overdose risk
-
Supports long-term recovery and relapse prevention
-
Improves retention in structured treatment programs (NIDA, 2023)
MAT is medically regulated, widely available, and safe when monitored.
Behavioral Therapies
Behavioral interventions help rebuild coping skills and prevent relapse:
-
Cognitive Behavioral Therapy (CBT) — identifies triggers and rewires unhealthy patterns.
-
Motivational Interviewing (MI) — strengthens commitment to change.
-
Acceptance and Commitment Therapy (ACT) — promotes mindfulness and value-driven actions.
-
Trauma-Informed Therapy — addresses co-occurring PTSD or past trauma.
-
Contingency Management — uses positive reinforcement for recovery milestones.
-
Relapse-Prevention Planning — prepares for high-risk situations and cravings.
Therapy helps individuals restore routines, manage triggers, and build psychological resilience.
Levels of Care
Depends on the intensity of support needed:
-
Medical Detox — stabilizes withdrawal symptoms, often before therapy or MAT.
-
Residential Treatment — 24/7 supervision and intensive therapy.
-
Partial Hospitalization Programs (PHP) — daily structured treatment without overnight stay.
-
Intensive Outpatient Programs (IOP) — multiple weekly therapy sessions with continued home living.
-
Standard Outpatient Counseling — weekly therapy and follow-up.
-
Peer Support Groups — ongoing community-based support to maintain recovery.
Light Family Involvement
Family support enhances recovery outcomes:
-
Encouraging medically supervised treatment
-
Helping with appointment scheduling
-
Supporting adherence to medication routines
-
Reducing household stressors
-
Providing safe transportation to care facilities
Peer Support & Recovery Capital
Recovery networks strengthen accountability and social support:
-
SMART Recovery — science-based, non-religious support group
-
NA / AA — peer-led support for substance use disorders
-
Online Recovery Communities — virtual meetings and forums
-
Medication-Friendly Peer Groups — support for MAT users
-
Sober Coaching — individualized guidance and encouragement
-
Harm-Reduction Programs — education and safe-practice strategies
Holistic Supports
Lifestyle interventions complement medical and behavioral care:
-
Regular exercise (3+ times per week)
-
Sleep stabilization and circadian regulation
-
Adequate hydration and nutrition for brain and body health
-
Stress reduction techniques — meditation, yoga, breathing exercises
-
Psychoeducation — understanding addiction and relapse risks
-
Mindfulness-Based Relapse Prevention — awareness of cravings and emotional triggers
Detox / Withdrawal Management After Ibogaine
Although ibogaine does not cause chemical withdrawal, post-treatment care is often required:
Common Challenges Post-Ibogaine:
-
Return of opioid withdrawal symptoms
-
Anxiety and emotional crashes
-
Sleep disturbances
-
Confusion after hallucinogenic effects
-
Cardiac concerns or palpitations
-
Increased relapse risk
Medical Support Focuses On:
-
Stabilizing opioid withdrawal through MAT or medications
-
Monitoring cardiac function after ibogaine exposure
-
Managing psychiatric symptoms and emotional instability
-
Connecting patients to structured outpatient or residential care
-
Providing psychoeducation and coping strategies for long-term recovery
Withdrawal or Post-Ibogaine Adjustment Timeline (What to Expect?)
Although ibogaine does not cause withdrawal, people often experience temporary physical and emotional symptoms as their body and mind recover:
0–24 hours
-
Fatigue and muscle weakness
-
Nausea or digestive upset
-
Cognitive fog or slowed thinking
-
Mild disorientation
24–72 hours
-
Emotional swings or mood lability
-
Sleep disturbances or insomnia
-
Anxiety or restlessness
-
Return of pre-existing opioid withdrawal symptoms
3–7 days
-
Cravings for opioids or other substances
-
Irritability or low frustration tolerance
-
Physical discomfort (aches, fatigue)
-
Heightened relapse risk without structured support
1–2 weeks
-
Cognitive fatigue or concentration difficulties
-
Mood instability
-
Difficulty reintegrating into normal routines
-
Ongoing need for psychological or social support
Dosing & Safety / Overdose Risks
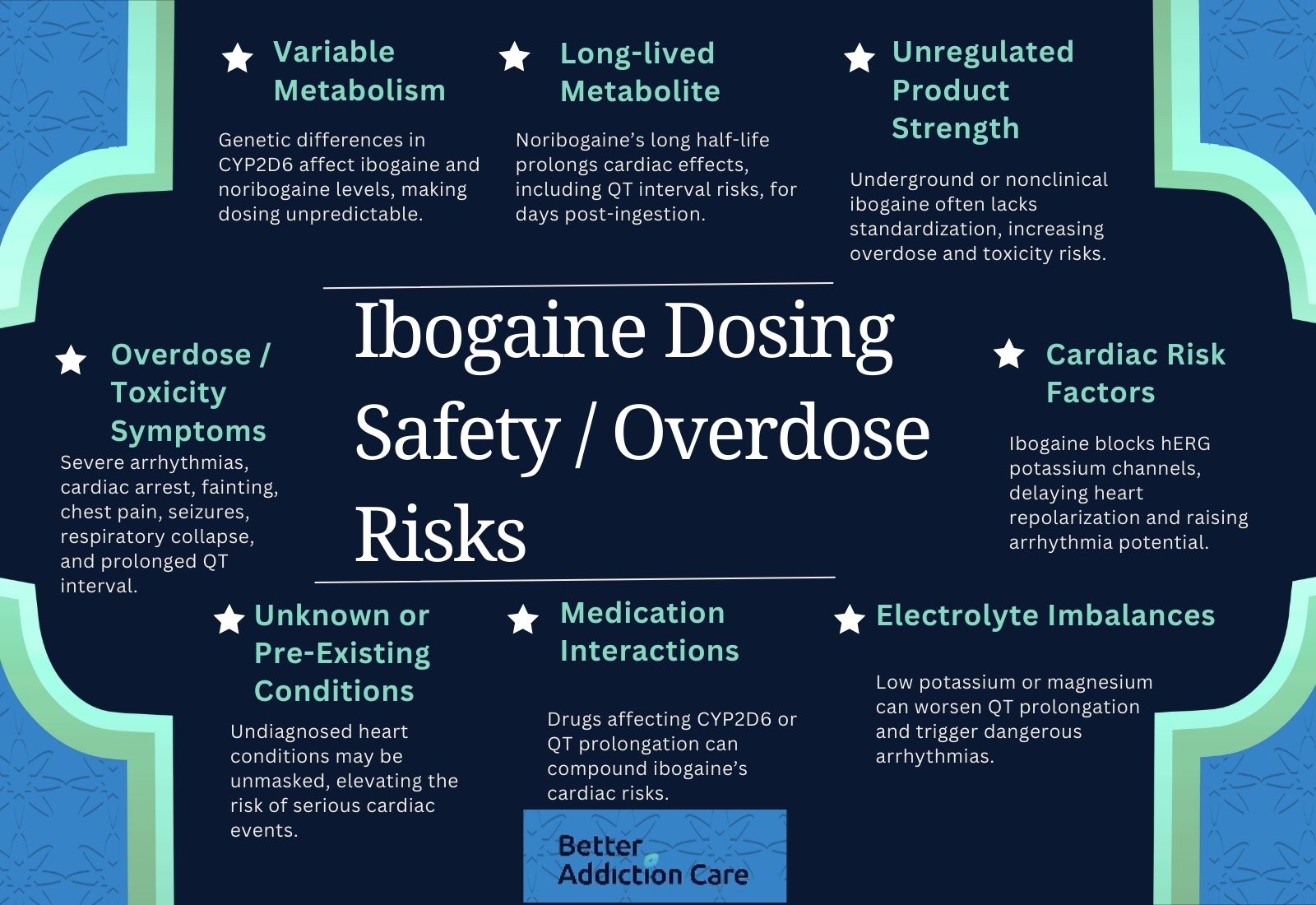
Why is Ibogaine Dosing Unpredictable and Risky?
-
Variable Metabolism: Ibogaine is metabolized primarily by the enzyme CYP2D6 into noribogaine, its active metabolite. Genetic differences in CYP2D6 activity can significantly affect how much ibogaine and noribogaine build up in the body.
-
Long-lived Metabolite: Noribogaine has a long plasma half-life, meaning cardiac effects (like QT prolongation) may persist for days after ingestion.
-
Unregulated Product Strength: In non-clinical or underground settings, the purity, concentration, or formulation of ibogaine is often not standardized, increasing risk.
-
Cardiac Risk Factors: Ibogaine and noribogaine block hERG potassium channels (ion channels in the heart), which can delay repolarization and prolong the QT interval — a known risk factor for arrhythmias.
-
Electrolyte Imbalances: Low potassium (hypokalemia) and low magnesium have been reported in fatal cases, which may worsen QT prolongation and arrhythmia risk.
-
Medication Interactions: Drugs that affect CYP2D6 or also prolong QT (e.g., some psychotropics, methadone) can compound risk.
-
Unknown or Pre-Existing Conditions: People may have undiagnosed cardiac issues (e.g., latent long-QT syndrome) that are unmasked by ibogaine.
Overdose / Toxicity Symptoms
These are the dangerous or life-threatening signs linked to ibogaine toxicity, especially when used in unregulated contexts:
-
Severe arrhythmias — Cases of ventricular flutter, ventricular tachycardia, and torsades de pointes have been reported.
-
Cardiac arrest / sudden death — There are documented fatal and near-fatal cases.
-
Fainting or syncope — As a consequence of dangerous heart rhythms.
-
Chest pain/discomfort — Possible with ischemia or arrhythmia.
-
Seizures — Reported in case studies following ibogaine ingestion.
-
Respiratory collapse — Secondary to severe cardiac dysfunction.
-
Prolonged QT interval — Even after “standard” doses, QT prolongation has been observed and can persist.
Why Medical Emergencies Are Common in Unsupervised Settings
-
Lack of cardiac monitoring: Without ECG monitoring before, during, and after treatment, dangerous arrhythmias can go undetected.
-
Inadequate screening: Patients may not be screened for electrolyte imbalances, existing heart conditions, or medication interactions.
-
Delayed risk window: Because noribogaine remains in the body for days, cardiac monitoring needs to extend well beyond the treatment session. PubMed Central+1
-
Low medical oversight in “clinics”: Many alternative ibogaine providers operate without the level of medical supervision (electrolyte checks, continuous ECG, emergency readiness) that clinical trials or regulated medical settings provide.
Conclusion
Ibogaine is not addictive, but its medical risks, legal status, and unpredictable effects make it unsafe and unsuitable for addiction treatment in the U.S. While some individuals pursue ibogaine out of desperation or fear of withdrawal, safer, evidence-based treatments exist.
Medication-assisted treatment, behavioral therapy, and structured recovery services consistently provide better outcomes without the life-threatening dangers associated with ibogaine.
If you or your loved one is considering ibogaine, connect with a licensed provider who can offer safe, effective, and medically verified care.
Treatment works; recovery is possible.
FAQs
No, ibogaine does not create chemical dependence. It does not stimulate the brain’s reward system, so it does not produce cravings or physical withdrawal symptoms. However, some individuals may develop a psychological reliance on the hallucinogenic or introspective effects, leading them to repeat sessions despite health risks. Such behavioral patterns are driven by emotion and expectation, not biology.
No, ibogaine is classified as a Schedule I controlled substance under U.S. federal law. This means it is illegal to manufacture, possess, or use for medical purposes in the United States. Its legal status restricts clinical research and prevents regulated medical use, which increases the prevalence of unregulated or underground treatments with a higher risk of adverse effects.
Ibogaine can temporarily reduce opioid withdrawal symptoms, including anxiety, nausea, and cravings, by affecting neurological pathways and perception. However, these effects are short-lived and do not provide a lasting solution. Long-term treatment with FDA-approved therapies, counseling, and follow-up support is required to safely manage opioid dependence and prevent relapse after ibogaine sessions.
Ibogaine carries serious cardiovascular and neurological risks. It can prolong the QT interval, trigger ventricular arrhythmias, provoke seizures, and has been linked to documented fatalities, particularly in unsupervised or unregulated clinics. Other complications may include severe fatigue, nausea, and cognitive disruption. Risk is heightened when pre-existing heart conditions, electrolyte imbalances, or interacting medications are present.
Safer, evidence-based alternatives include FDA-approved medications like buprenorphine, methadone, and naltrexone. These treatments are medically regulated, reduce cravings, stabilize withdrawal, lower the risk of overdose, and improve retention in long-term recovery programs. Combining medications with behavioral therapies, counseling, and peer support offers a structured, effective path toward sustainable opioid recovery.
No, ibogaine can interact dangerously with multiple medications. It is particularly risky when combined with SSRIs, methadone, stimulants, or cardiac drugs, potentially triggering arrhythmias, serotonin syndrome, or other life-threatening complications. Medical supervision is required for anyone taking prescription medications, which is rarely available in unregulated ibogaine settings.
No, ibogaine itself does not cause physical withdrawal. Any symptoms experienced after a session—such as anxiety, cravings, or fatigue—reflect the return of untreated opioid withdrawal or psychological rebound. Supportive care and evidence-based treatment are necessary to manage these post-treatment effects safely and reduce the risk of relapse.







