Klonopin Addiction: Signs, Symptoms & Withdrawal
Klonopin (clonazepam), a medication prescribed to manage anxiety, seizures, and panic disorders, may initially offer relief but can gradually lead to dependence and addiction.
Klonopin addiction develops when the brain becomes dependent on the drug’s calming effects, leading to tolerance, escalating use, and difficulty stopping.

Withdrawal can begin within 1–2 days of the last dose, often peaking in the first week and sometimes lasting weeks or even months. The process is not only uncomfortable but can also be dangerous without medical supervision.
Key Takeaways
- Klonopin addiction often begins with prescribed use, but over time, the brain adapts and dependence develops. Recognizing the difference between normal reliance and harmful addiction is vital, especially since tolerance and withdrawal can appear even when the medication is taken as directed.
- Withdrawal from Klonopin can be dangerous without medical support, but safe detox and tapering protocols are available. Understanding the withdrawal timeline, symptoms, and potential complications allows individuals and families to prepare realistically while reducing fear.
- Recovery is possible when treatment includes both medical and emotional support. Programs that combine detox, therapy, family involvement, and relapse-prevention strategies significantly improve long-term outcomes, helping individuals and their loved ones rebuild stability and hope together.
Understanding Klonopin and Its Uses
What is Klonopin (Clonazepam)?
Klonopin, the brand name for clonazepam, is a prescription medication in the benzodiazepine class. Benzodiazepines are central nervous system (CNS) depressants, meaning they slow down brain activity to produce a calming effect.
Doctors typically prescribe Klonopin for conditions such as panic disorder, anxiety, seizures, and sometimes insomnia. While the medication can be effective for short-term relief, its calming properties also make it highly addictive if not used exactly as directed[1].
Medical Uses and Prescription Guidelines
Clonazepam is approved by the U.S. Food and Drug Administration (FDA) for seizure disorders and panic disorder. In clinical practice, it is sometimes prescribed off-label for sleep issues or other anxiety-related conditions.
Standard prescriptions are meant to be short-term, usually a few weeks, because the risk of dependence grows quickly with continued use. Physicians often recommend the lowest effective dose for the shortest duration possible[1].
Despite these guidelines, many people remain on the drug for months or even years. For some, this long-term use happens because symptoms return when they try to stop.
For others, their bodies adapt to the medication so strongly that reducing or discontinuing it without professional help feels nearly impossible.
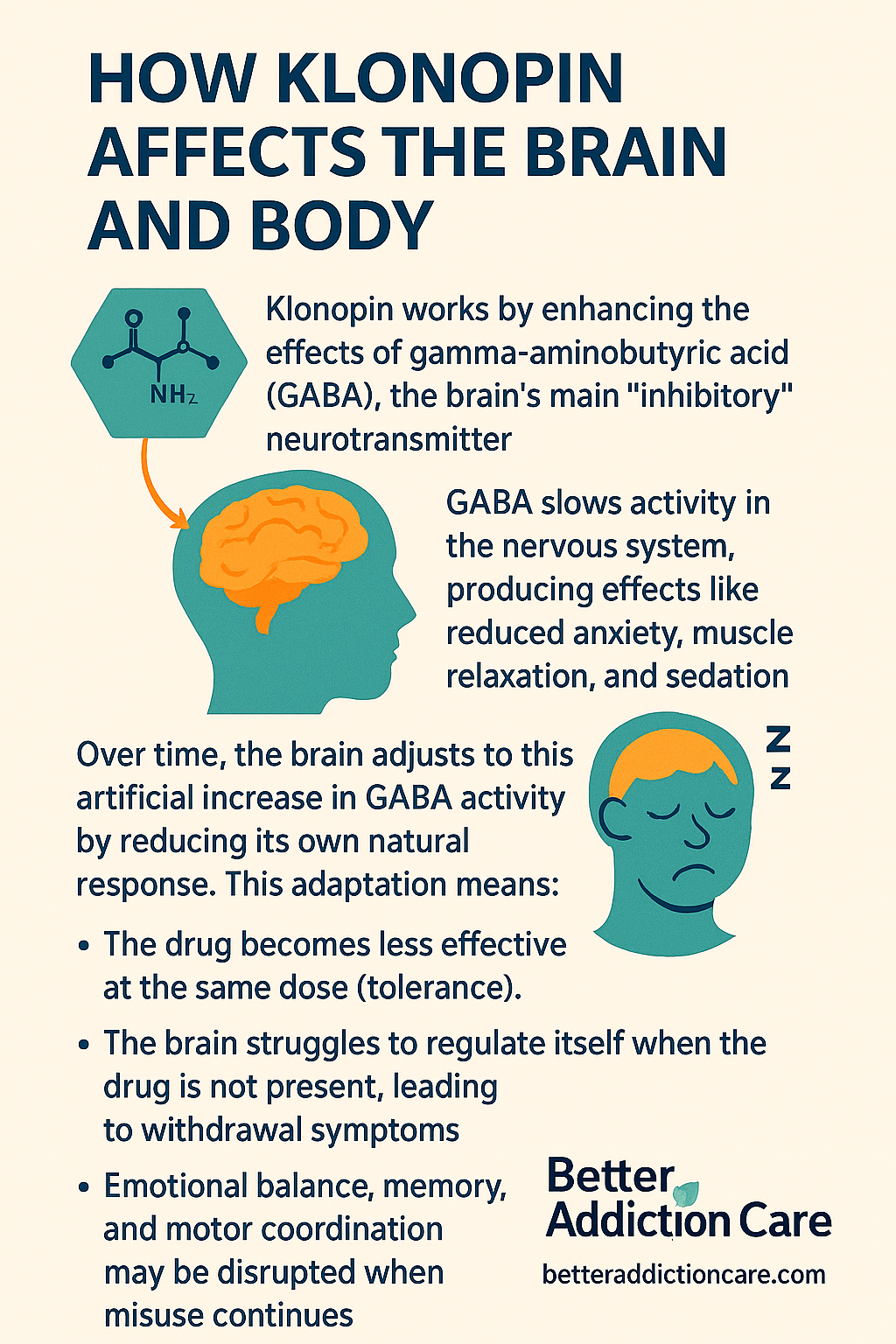
How Klonopin Affects the Brain and Body?
Klonopin works by enhancing the effects of gamma-aminobutyric acid (GABA), the brain’s main “inhibitory” neurotransmitter. GABA slows activity in the nervous system, producing effects like reduced anxiety, muscle relaxation, and sedation.
Over time, the brain adjusts to this artificial increase in GABA activity by reducing its own natural response. This adaptation means:
- The drug becomes less effective at the same dose (tolerance).
- The brain struggles to regulate itself when the drug is not present, leading to withdrawal symptoms.
- Emotional balance, memory, and motor coordination may be disrupted when misuse continues[1].
For families, this often shows up as a loved one who seems increasingly drowsy, forgetful, or emotionally detached. What starts as prescribed use can shift into a cycle where the person feels unable to function without Klonopin.
How Klonopin Addiction Develops?
Dependence and Addiction: A Brief Explanation
Klonopin (clonazepam) has a high potential for dependence because of how it alters brain chemistry.
- Dependence occurs when the body adapts to the drug’s presence, leading to withdrawal symptoms if the dose is reduced or stopped.
- Addiction, on the other hand, involves not just physical reliance but also compulsive drug-seeking and continued use despite harm[1].
This distinction matters because many people who start Klonopin with a legitimate prescription never intend to misuse it.
Yet over time, the brain’s adaptation blurs the line between needing the medication for symptom relief and being unable to stop even when negative consequences emerge.
Role of Tolerance and Misuse
Tolerance is one of the earliest warning signs of developing dependence. As the brain downregulates its response to GABA, individuals need higher or more frequent doses to achieve the same calming effect[1].
For someone prescribed Klonopin for panic attacks, this may look like their original dose “stops working,” prompting requests for stronger prescriptions. Others may start taking the medication outside of prescribed limits — for example, doubling a dose before a stressful event.
In some cases, misuse extends to combining Klonopin with alcohol or opioids to intensify sedation, which can be extremely dangerous[2].
Psychological and Physical Addiction Mechanisms
Benzodiazepines like Klonopin do more than calm the nervous system — they also tap into the brain’s reward pathways.
Over time, the relief from anxiety or stress becomes psychologically reinforcing. People may begin to associate daily functioning or emotional stability with having the drug in their system.
Physically, prolonged use disrupts the brain’s ability to regulate inhibitory and excitatory signals on its own. This creates a cycle where stopping feels unbearable, and continued use seems like the only option [1][3].
For loved ones, these changes can be confusing and alarming. The person may appear “checked out,” prioritize the medication over responsibilities, or become secretive about their use. These behavioral patterns often mark the shift from medical reliance to full-blown addiction.
Signs and Symptoms of Klonopin Addiction
Klonopin (clonazepam) is often prescribed to relieve anxiety, seizures, or panic disorders—but its calming effects also make it highly addictive.
People rarely notice addiction forming all at once. Instead, the shift from therapeutic use to harmful dependence is gradual, marked by behavioral changes, physical decline, and emotional disruption. Recognizing these signs early can prevent escalation and open the door to recovery.
1. Behavioral Red Flags
Behavioral changes are usually the earliest and most visible signals of Klonopin misuse:
- Doctor shopping and refill manipulation — requesting higher doses, running out of medication early, or visiting multiple prescribers. Loved ones may notice frequent “urgent” appointments or unexplained pharmacy visits.
- Secretive usage patterns — hiding pills, lying about dosage, or isolating to take the medication in private. This secrecy often breeds tension in relationships.
- Neglect of responsibilities — reduced performance at work, missing classes, or abandoning family commitments. Deadlines are missed not because of a lack of skill, but because sedation interferes with focus.
- Risk-taking behaviors — driving while drowsy, mixing Klonopin with alcohol or opioids, or attempting to buy pills illegally. The FDA’s updated boxed warning[4] stresses that combining benzodiazepines with opioids can result in life-threatening respiratory depression.
From a family’s perspective, these behavioral shifts are often the first signs that something is wrong. A reliable, organized person may suddenly appear distracted, withdrawn, or unreliable—changes that can’t easily be explained away.
2. Physical Symptoms
As tolerance develops, the body starts signalling its growing dependence:
- Persistent drowsiness — nodding off during conversations or falling asleep at inappropriate times.
- Poor coordination and slurred speech — stumbling, slower reaction times, and impaired motor control, similar to alcohol intoxication.
- Cognitive lapses — difficulty recalling recent events, misplaced items, or forgetting appointments.
- Increasing tolerance — needing larger or more frequent doses to feel relief. This “dose creep” is one of the clearest indicators of dependence.
- Withdrawal avoidance — noticeable irritability or flu-like symptoms if a dose is missed.
The FDA-approved prescribing information for Klonopin[5] emphasizes that abrupt discontinuation can cause seizures, hallucinations, and severe withdrawal—clear medical proof that dependence develops at the physiological level.
3. Psychological and Emotional Warning Signs
Addiction to Klonopin isn’t only about physical dependence—it changes how a person feels, thinks, and relates to others:
- Rebound anxiety and panic — instead of reducing anxiety, the absence of Klonopin can intensify it, making the person feel they “need” the drug to function.
- Flattened emotions — emotional blunting, loss of joy in hobbies, or a general sense of numbness. Families may describe their loved one as “not themselves.”
- Mood swings and irritability — sudden anger or withdrawal that disrupts household stability.
- Obsessive focus on medication — preoccupation with the next dose or fear of running out, which mirrors patterns seen in other substance addictions.
Research confirms that benzodiazepine misuse can paradoxically worsen mental health over time[1][3]. For many, this creates a cruel cycle: Klonopin is used to manage distress, yet prolonged use amplifies emotional instability.
4. Social and Family Consequences
Perhaps the most painful signs are those that ripple through relationships:
- Isolation — withdrawing from family gatherings, avoiding friends, or canceling plans to stay home and use.
- Financial strain — unexplained expenses related to doctor visits, pharmacy bills, or illicit pill purchases.
- Broken trust — repeated lies about usage damage bonds with partners, children, and parents.
- Emotional exhaustion — family members often feel caught between wanting to help and fearing confrontation. Over time, this burnout may cause loved ones to distance themselves.
Addiction is rarely an individual problem; it reshapes entire family dynamics. The FDA and clinical literature alike stress the importance of recognizing these external effects early, as families are often the first to notice subtle but persistent changes[2][4].
Why Do These Signs Matter?
Identifying these warning signs is not about judgment—it’s about protection. Klonopin addiction is medically recognized, dangerous, and treatable.
The FDA’s heightened warning in 2020[4] underlines the urgency of early recognition: untreated dependence increases the risk of overdose, severe withdrawal, and life-altering consequences.
Withdrawal from Klonopin: What to Expect?
Stopping Klonopin after prolonged or heavy use can feel overwhelming, both physically and emotionally.
Withdrawal from benzodiazepines like clonazepam is often more complex than with other substances because the brain becomes accustomed to the drug’s calming effects on the central nervous system.
When it is suddenly removed, the brain’s activity rebounds, leading to uncomfortable — and sometimes dangerous — symptoms.
Recognizing what withdrawal looks like, how long it lasts, and why medical supervision is critical can help individuals and families prepare for the recovery journey.
Common Withdrawal Symptoms
Klonopin withdrawal symptoms vary in severity depending on dose, duration of use, and individual health factors. Commonly reported effects include:
- Anxiety and panic attacks (often more intense than the original condition treated)
- Insomnia and disturbed sleep patterns
- Irritability, restlessness, and agitation
- Physical discomforts such as headaches, muscle stiffness, sweating, nausea, or tremors
- Cognitive problems like poor concentration and memory issues
- Perceptual changes such as heightened sensitivity to light or sound
In severe cases, withdrawal can lead to seizures or hallucinations, especially if the drug is stopped abruptly[1][4].
Detailed Timeline: Acute and Protracted Withdrawal
Withdrawal unfolds in phases, and knowing what to expect helps reduce fear and uncertainty:
- Early Withdrawal (1–3 days after last dose): Rebound anxiety, restlessness, and difficulty sleeping typically appear first.
- Acute Phase (1–2 weeks): Symptoms peak, including intense anxiety, tremors, sweating, nausea, and mood swings. This is the stage of highest risk for seizures.
- Protracted Withdrawal (weeks to months): While many symptoms fade after 2–4 weeks, some people experience lingering problems such as anxiety, insomnia, or cognitive “fog.”
Research suggests a subset may face post-acute withdrawal syndrome (PAWS), where symptoms come and go for months[2][3].
This variability means one person’s recovery may look very different from another’s.
Potential Risks and Complications
Attempting to quit Klonopin without medical guidance carries significant risks. The most concerning are:
- Seizures – potentially life-threatening events requiring emergency care.
- Severe rebound anxiety or panic – can be destabilizing and increase relapse risk.
- Hallucinations and psychosis – rare but documented in cases of abrupt withdrawal.
- Medical emergencies if the individual has co-occurring conditions such as epilepsy, heart disease, or polysubstance use[1][4].
These risks highlight why self-detox is dangerous and why tapering under supervision is strongly recommended.
Managing Withdrawal Safely
Safe withdrawal is possible with the right medical support. Evidence-based strategies include:
-
Importance of Medical Supervision and Detox
Professional oversight ensures dosage is gradually reduced, minimizing risks. The FDA and clinical guidelines recommend a tapering schedule rather than abrupt cessation to allow the brain to adapt slowly[4].
-
Common Detox Approaches and Tapering Protocols
Doctors may reduce the daily dose incrementally over weeks or months, depending on individual tolerance. In some cases, switching to a longer-acting benzodiazepine before tapering may ease symptoms[2].
-
When Emergency Help is Needed
Families should seek immediate medical attention if withdrawal includes seizures, hallucinations, suicidal thoughts, or uncontrolled vomiting/dehydration. These are red-flag symptoms that cannot be managed at home[1][4].
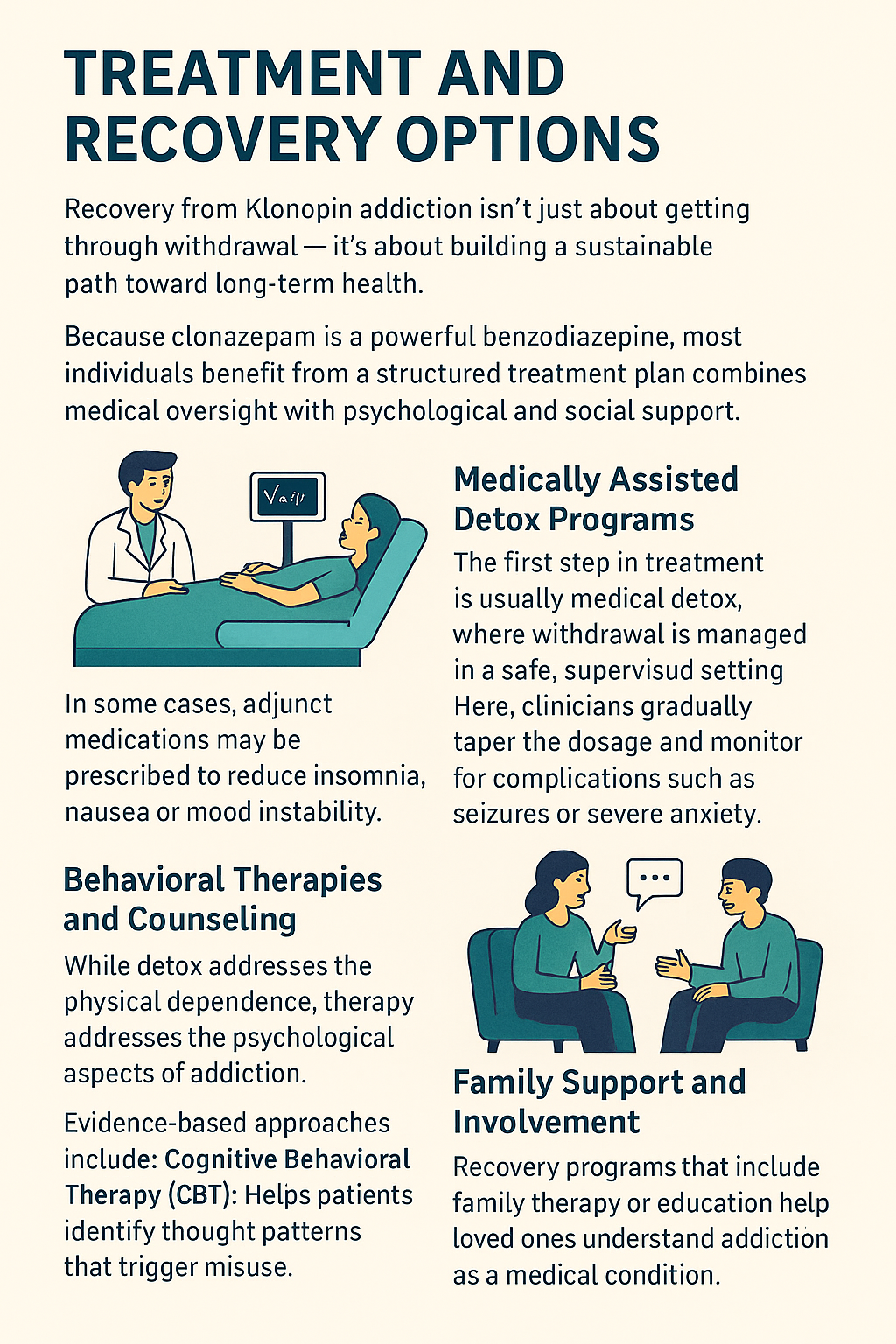
Treatment and Recovery Options
Recovery from Klonopin addiction isn’t just about getting through withdrawal — it’s about building a sustainable path toward long-term health.
Because clonazepam is a powerful benzodiazepine, most individuals benefit from a structured treatment plan that combines medical oversight with psychological and social support.
1. Medically Assisted Detox Programs
The first step in treatment is usually medical detox, where withdrawal is managed in a safe, supervised setting. Here, clinicians gradually taper the dosage and monitor for complications such as seizures or severe anxiety.
In some cases, adjunct medications may be prescribed to reduce insomnia, nausea, or mood instability[1]. This stage gives individuals the safest foundation for ongoing recovery[4].
2. Behavioral Therapies and Counselling
While detox addresses the physical dependence, therapy addresses the psychological aspects of addiction. Evidence-based approaches include:
- Cognitive Behavioral Therapy (CBT): Helps patients identify thought patterns that trigger misuse and develop healthier coping strategies.
- Motivational Interviewing (MI): Supports ambivalence about quitting by helping individuals align recovery with their personal goals.
- Trauma-informed therapy: For patients whose anxiety or substance use stems from past trauma.
These therapies not only reduce relapse risk but also give individuals tools to rebuild confidence[2] and stability[3].
3. Family Support and Involvement
Addiction often damages trust within families. Recovery programs that include family therapy or education help loved ones understand addiction as a medical condition, not a moral failing.
Families can learn how to set boundaries, reduce enabling behaviors, and create an environment that supports healing. This shared approach strengthens the recovery process and reduces feelings of isolation for both the patient and their loved ones.
Addressing Polysubstance Use and Co-occurring Disorders
Many people struggling with Klonopin addiction also face other substance use disorders (such as alcohol or opioids) or mental health conditions like depression or PTSD.
Effective treatment requires integrated care that addresses all conditions together rather than in isolation. Coordinated treatment teams — including psychiatrists, therapists, and primary care physicians — provide a more holistic and sustainable recovery plan[1][3].
Preventing Relapse and Supporting Long-Term Recovery
- Addiction recovery does not end after detox or rehab. Sustaining sobriety requires a long-term plan that includes ongoing therapy, peer support, and lifestyle changes.
Strategies for Maintaining Sobriety:
- Stress management, exercise, meditation, and consistent sleep routines help restore balance.
Role of Support Groups and Resources:
- Groups such as Narcotics Anonymous (NA) or SMART Recovery give individuals a safe place to share experiences, learn strategies, and stay accountable.
Mental Health Integration and Overcoming Stigma:
- Addressing the underlying anxiety or panic disorder that may have led to the initial prescription is critical.
- At the same time, individuals and families must confront stigma, which can discourage treatment-seeking.
- Education and open dialogue help normalize recovery as a courageous and medical process[2][4].
Relapse Rates and Long-Term Success
Recovery from Klonopin addiction is a long journey, and relapse can sometimes be part of the process rather than a sign of failure.
Research on benzodiazepine use shows that relapse rates can be as high as 40–60% within the first year if individuals attempt to quit without structured support[2][3].
These numbers may feel discouraging, but they also highlight why professional treatment and ongoing care make such a difference.
When individuals participate in comprehensive treatment programs — including supervised detox, therapy, and family involvement — success rates improve significantly. Studies show that structured tapering protocols combined with behavioral therapies can cut relapse risk nearly in half[2].
The addition of peer support and aftercare planning further increases the likelihood of long-term recovery.
Families and individuals need to understand that:
- Setbacks are common but not final. A relapse signals that treatment needs to be adjusted, not abandoned.
- Long-term engagement matters. Recovery outcomes are strongest when treatment continues for at least 12 months with ongoing therapy or support group participation.
- Holistic support improves results. Individuals who have stable housing, supportive family relationships, and access to mental health services consistently show higher rates of sustained sobriety[3][4].
Framing relapse as a manageable obstacle rather than an endpoint helps individuals stay motivated and reduces shame, keeping the focus on progress and resilience.
Conclusion
Klonopin addiction can quietly develop, even for people who began using the medication exactly as prescribed. Recognizing the early signs of dependence and addiction, understanding the serious risks of withdrawal, and knowing the available treatment paths can make the difference between ongoing struggle and a safe recovery journey.
If you or your loved one is showing signs of Klonopin addiction, remember:
- You are not alone. Millions of people in the U.S. have struggled with benzodiazepine misuse, and many have found lasting recovery through treatment[3].
- Recovery is possible with the right support. While relapse can occur, structured treatment that combines detox, therapy, and family involvement greatly improves long-term success[2][4].
- Taking the first step matters most. Whether that means reaching out to a healthcare provider, exploring detox options, or joining a support group, every action builds momentum toward healing.
Addiction affects the whole family, not just the individual. By approaching the situation with compassion, seeking professional help, and staying engaged in the process, families can play a powerful role in recovery.
Common Questions Related to Klonopin
Yes. Even when taken exactly as prescribed, Klonopin can lead to physical dependence because the brain adapts to the drug’s calming effects. Dependence does not always mean addiction, but it can progress into addiction if higher doses are needed or if use continues for long periods.
There is no universal timeline. Some people may develop dependence in as little as a few weeks, especially at higher doses, while others may take longer. Factors like dosage, frequency, medical history, and whether Klonopin is combined with other substances all influence the speed of addiction.
No. Stopping abruptly can cause dangerous withdrawal symptoms such as seizures, severe anxiety, or hallucinations. A medically supervised taper is the safest method of discontinuation.
The best step is to approach with compassion, not confrontation. Encourage an open conversation and suggest professional help, such as a doctor’s evaluation or a treatment program. Families can also benefit from joining support groups like Al-Anon or SMART Recovery for Loved Ones.
Therapy is essential, but usually not enough by itself. Because withdrawal can be physically dangerous, most individuals need medical detox first, followed by therapy and relapse prevention strategies for long-term success.
While there is no single FDA-approved medication specifically for benzodiazepine withdrawal, clinicians sometimes use adjunct medications (like anticonvulsants or antidepressants) to ease symptoms. However, the most effective approach remains a gradual taper under medical supervision.
Resources
Related Articles
Treatment Centers in Iowa