Is Lisinopril Addictive? Abuse Potential, Side Effects, and Safe Use
Lisinopril is an ACE inhibitor (angiotensin-converting enzyme inhibitor) prescribed to:
-
Lower high blood pressure

- Improve heart function after a heart attack
- Protect the kidneys in individuals with diabetes
- Reduce long-term cardiovascular risk
It works by relaxing blood vessels, lowering pressure on the heart, and supporting healthy circulation.
High blood pressure medications often cause worry when people notice symptoms if they miss a dose. Some assume this means they are “dependent” or “addicted.” In reality, these experiences come from normal blood-pressure physiology—not addiction.
-
Tolerance: needing more of a drug to feel its effects
→ Lisinopril does not produce tolerance related to mood or reward. -
Dependence: withdrawal when stopping
→ Lisinopril does not create withdrawal symptoms or cravings. -
Addiction: compulsive use despite harm
→ This pattern has not been documented with lisinopril. [1]
Lisinopril does not stimulate dopamine receptors or the prefrontal cortex involved in the reward cycle, meaning it cannot create reinforcement or cravings.
Key Takeaways
-
Lisinopril is not addictive and has no chemical abuse potential, as it does not affect the brain’s reward system or produce euphoria.
-
Misuse can still occur through incorrect dosing, self-adjustment, or using prescriptions unsafely, even though addiction does not develop.
-
Lisinopril does not cause tolerance or withdrawal, but stopping suddenly can result in rebound blood-pressure elevations, which may feel alarming.
-
Treatment works; recovery is possible.
-
Safe use, medical monitoring, and lifestyle changes reduce risks and support long-term cardiovascular health.
Signs & Symptoms of Lisinopril Misuse

While lisinopril is not addictive, it can still be misused, especially when individuals are anxious about their blood pressure, confused about dosing instructions, or mixing medications without guidance.
Misuse patterns tend to develop slowly and often begin with uncertainty—not intentional harm.
Physical Signs of Lisinopril Misuse
-
Dizziness or faintness from medication stacking
Taking extra doses “just in case” can push blood pressure too low. People may experience sudden dizziness when standing, lightheadedness after meals, or brief episodes of blurred vision. These symptoms indicate the dose is not being taken as intended, not addiction.
-
Headaches or neck pressure after missed doses
When doses are skipped, blood pressure may rebound upward. This tension-based headache is often mistaken for “withdrawal,” but it’s simply the circulatory system returning to its untreated state.
-
Consistently low blood pressure readings
A pattern of readings significantly below the usual range may indicate that a person is doubling doses, adjusting the timing on their own, or mixing lisinopril with other BP-lowering substances, such as alcohol or diuretics.
-
Fatigue or reduced stamina
Overuse can cause excessive fatigue, slow recovery from physical activity, and difficulty concentrating. Individuals may describe feeling “wiped out” after even mild exertion.
-
Elevated potassium (hyperkalemia)
Misuse can interrupt kidney balance and increase potassium levels, causing muscle weakness, irregular heartbeat sensations, and tingling in the hands and feet.
-
Dry, persistent cough caused by unreported overuse
The classic ACE-inhibitor cough may worsen if dosing is inconsistent. Many individuals increase their dose without realizing this intensifies side effects.
-
Swelling of lips or face (angioedema — a medical emergency)
Although rare, angioedema requires immediate attention. It may appear after dose stacking or interactions with other medications.
Emotional & Psychological Signs of Misuse
-
Anxiety centered around daily blood-pressure readings
Individuals may check their numbers repeatedly throughout the day, reacting to minor fluctuations with unnecessary extra medication.
-
Fear of missing or delaying a dose
Some people believe that even being an hour late will cause dangerous spikes. This fear can lead to taking more than prescribed or taking doses too close together.
-
Distorted beliefs about “needing more” for safety
Rather than taking lisinopril as maintenance therapy, individuals may treat it like an emergency rescue medication—using extra doses during stress or after arguments, workouts, or caffeine.
-
Stress responses driven by normal BP variations
Heart rate increases, tension, and mild symptoms may be misinterpreted as “signs they need another pill,” leading to misuse patterns over time.
Behavioral Signs of Lisinopril Misuse
-
Overmonitoring blood pressure multiple times per hour
This creates a feedback loop: anxiety → BP spike → more checking → more anxiety → dose stacking.
-
Adjusting doses without medical oversight
People may cut tablets in half, take multiple tablets, or shift dosing times according to how they “feel,” rather than following a structured medical plan.
-
Doubling or tripling doses after missed tablets
This is a common misuse pattern and increases the risks of hypotension and kidney strain.
-
Using someone else's medication or sharing prescriptions
Individuals may use a spouse’s or family member’s prescription when they run out, or vice versa, creating inconsistent strength and timing.
-
Avoiding follow-ups due to fear of judgment or confusion
Skipping appointments often leads to deteriorating dose control and side-effect management.
-
Mixing lisinopril with alcohol or interacting medications
Alcohol, NSAIDs, and certain diuretics can cause dangerous BP drops or kidney heaviness.
How Common Is It?
Lisinopril remains one of the most commonly prescribed medications in the United States, with tens of millions of prescriptions written annually. [2] Its wide use means dosing misunderstandings are more frequent than true misuse or abuse.
General prevalence:
Lisinopril is one of the most commonly prescribed medications in the United States, with an estimated ~76 million prescriptions written in 2023 [2]. Because it is used so widely, dosing confusion is far more common than intentional misuse.
Most cases involve skipped doses, doubling doses after stressful events, or adjusting timing based on symptoms, not addiction. Importantly, no national database lists lisinopril as a drug with abuse or dependence potential, and there are zero documented cases of chemical addiction.
Clinical settings:
ACE inhibitors—including lisinopril—were used by 11.4% of U.S. adults ages 40–59 who took prescription medications in national survey data from 2015–2016 [3]. In these clinical environments, certain groups show higher rates of misuse patterns due to misunderstanding or inconsistent routines, including:
-
Individuals newly diagnosed with hypertension
-
Adults managing multiple chronic conditions (diabetes, kidney disease, heart failure)
-
Recently discharged ER or cardiac patients who may “panic-dose”
-
Older adults (60+) with memory or medication-management challenges
-
People without regular follow-up, who self-adjust doses based on home readings
These patterns reflect behavioral responses to health anxiety or confusion, not dependence or drug-seeking behavior.
Withdrawal frequency:
A study on ACE-inhibitor discontinuation found that blood pressure begins rising within 48 hours and reaches a 5-day plateau after stopping treatment [3]. This is classified as rebound physiology, not withdrawal.
-
True withdrawal frequency: 0%
-
Rebound symptom frequency: occasionally reported, especially after sudden discontinuation
Rebound symptoms—such as headaches, tension, or rising blood pressure—represent the body returning to its untreated state, not addictive withdrawal.
Causes: Why Does Lisinopril Misuse Happen?
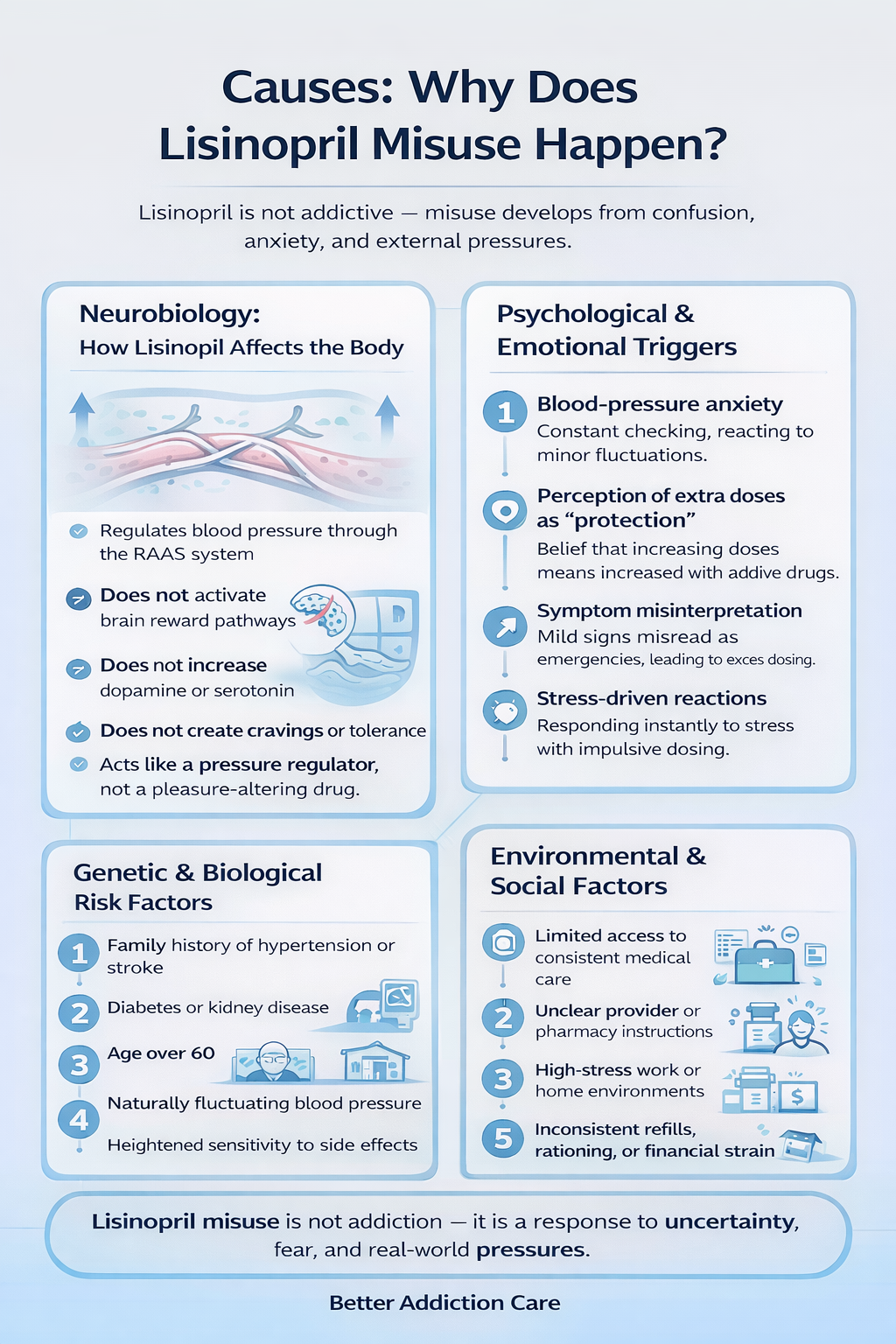
Since lisinopril cannot create addiction, the root causes of misuse are typically related to confusion, anxiety, medical misunderstanding, or environmental pressures.
Neurobiology (How Lisinopril Affects the Body?)
Lisinopril works through the renin-angiotensin-aldosterone system (RAAS), reducing the hormone (angiotensin II) that normally tightens blood vessels. As vessels relax, blood pressure drops.
Key Neurobiological Distinctions
Lisinopril:
-
Does not enter or stimulate the brain’s reward pathway
→ No reinforcing “high,” no cravings. -
Does not increase dopamine or serotonin
→ No mood-related activation associated with addictive drugs. -
Does not cause tolerance in the reward system
→ Dose does not escalate to maintain “effect.” -
Does not alter the brain’s reinforcement circuits
→ No compulsion loop can develop.
Lisinopril acts like a built-in pressure regulator for your blood vessels—not like a substance that changes how your brain experiences pleasure or reward.
Genetic & Biological Factors
Although the medication itself is not addictive, certain biological factors increase the likelihood of misuse or inconsistent dosing:
-
Family history of severe hypertension or stroke: Individuals may panic when readings rise slightly and self-adjust doses.
-
Coexisting diabetes or kidney disease: These conditions may complicate symptoms, making people misinterpret normal BP changes.
-
Age above 60: Older adults may forget doses or take extra unintentionally.
-
Natural BP variability: People with fluctuating readings may overreact to small spikes.
-
Heightened sensitivity to side effects: Fatigue, cough, or dizziness may cause individuals to reduce or stop medication abruptly without guidance.
Psychological & Emotional Triggers
Misuse often begins with fear, uncertainty, or a lack of confidence in the body’s stability.
-
Blood-pressure anxiety: Individuals may believe their numbers are “dangerously high” when they’re within normal fluctuation, leading to self-adjusted dosing.
-
Belief that extra doses offer more protection: Stress or past medical scares can make people feel safer taking more than prescribed.
-
Misinterpreting symptoms: A mild headache after a missed dose may be mistaken for a medical emergency.
-
Stress-driven responses: Stress spikes blood pressure naturally; some people take medication immediately rather than using non-medication coping strategies.
Environmental & Social Factors
Real-world pressures often influence how lisinopril is taken.
-
Limited access to a consistent prescriber: Individuals may ration medication or take someone else’s supply.
-
Unclear pharmacy or provider instructions: Leads to doubling doses or inconsistent timing.
-
High-stress job or home environment: Encourages impulsive dosing choices when BP feels elevated.
-
Inconsistent refill schedules: Can lead to skipped doses, rationing, or borrowing medicine.
-
Low health literacy: Makes it challenging to understand how BP medications should work.
-
Financial strain: May cause delays in follow-up care, resulting in unsupervised medication adjustments.
From Medical Use to Misuse (Progression)
The “progression” of misuse with lisinopril is behavioral—not chemical:
-
Starting lisinopril for hypertension, often after a concerning BP reading or medical event.
-
Feeling better after a few weeks, leading some to skip doses.
-
Blood pressure rises again, causing worry or panic.
-
Taking extra doses to counter the spike without medical guidance.
-
Experiencing dizziness or low BP due to overcorrection.
-
Anxiety increases, especially around readings or symptoms.
-
A misuse cycle forms, driven by fear or inconsistent dosing, not addiction.
This reinforces the importance of stable routines and consistent monitoring—not dependency language.
Who Is Most at Risk of Developing Misuse Patterns?
Expanded profiling improves clarity for readers and SEO value.
-
Newly diagnosed individuals who are still learning how BP fluctuations work
-
People recently hospitalized for heart or blood-pressure issues
-
Adults with significant health anxiety or a family history of stroke
-
People taking multiple cardiac medications, increasing dosing confusion
-
Older adults managing complex medication schedules
-
Individuals monitoring BP several times a day, which elevates anxiety
-
People lacking regular medical follow-up, creating uncertainty
-
Individuals using interacting medications (diuretics, NSAIDs, potassium supplements)
Side Effects of Lisinopril
Short-Term Side Effects
-
Headache, especially if doses are missed or stopped
-
Low blood pressure, causing dizziness or lightheadedness
-
Fatigue, often due to initial blood-pressure stabilization
-
Dry cough, a hallmark of ACE inhibitor effect
-
Nausea, occurring in some users during early treatment
-
Potassium level changes, more common when combined with diuretics or supplements
Long-Term Side Effects (Expanded)
-
Persistent cough, leading to dose changes or medication switches
-
Kidney function shifts, requiring periodic monitoring
-
Hyperkalemia, particularly in those with kidney disease
-
Rare angioedema, a potentially serious swelling reaction
-
Blood-pressure variability, especially if dosing is inconsistent
-
Mood impacts related to health stress or BP monitoring
-
Drug interactions, including harmful combinations with NSAIDs
Impact on Daily Life
-
Reduced stamina or energy, affecting work and activity levels
-
Episodes of faintness, especially after exertion
-
Missed workdays due to symptoms or anxiety
-
Increased stress around medication routines
-
More ER visits, often related to rebound BP changes or side effects
Treatment Options
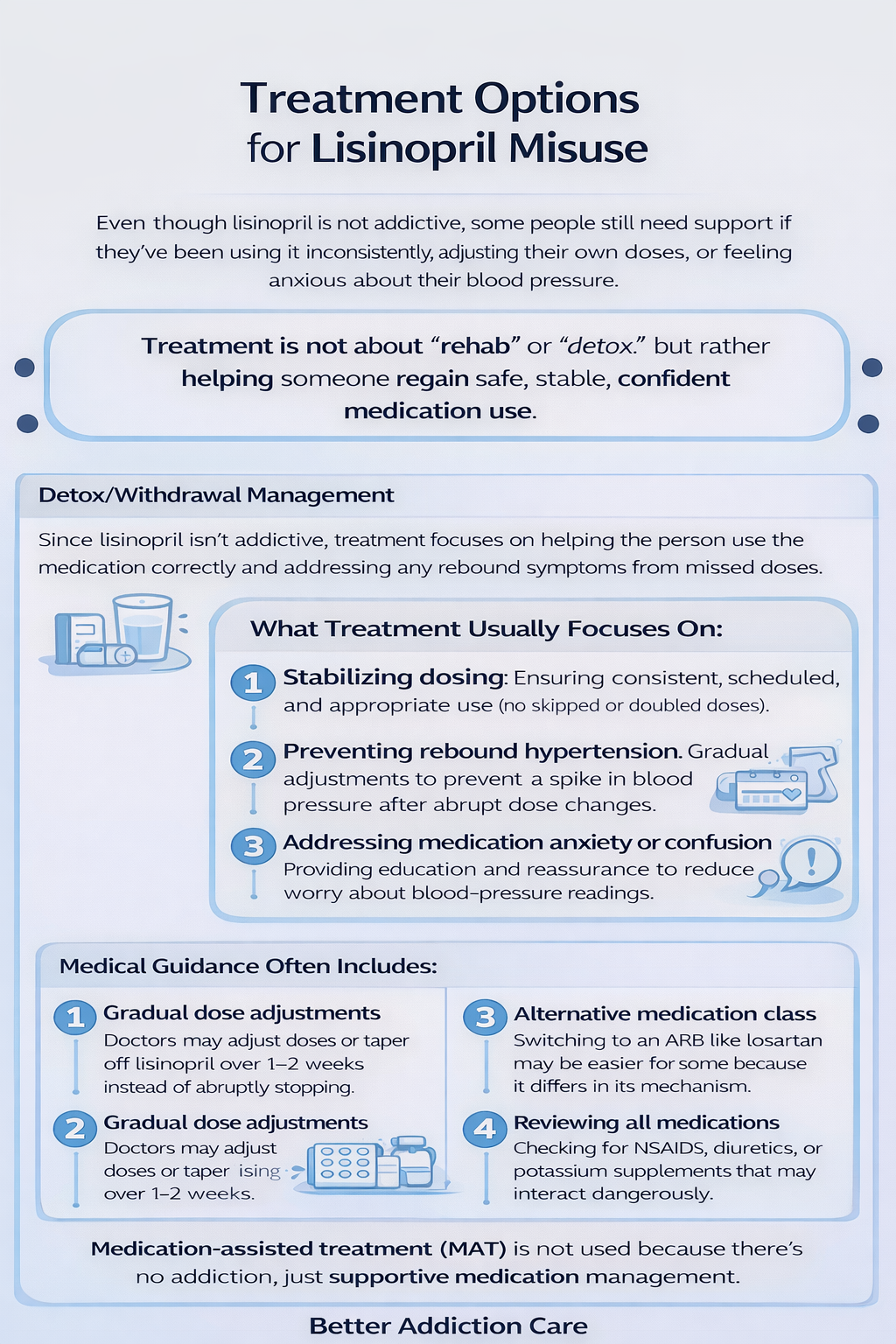
Even though lisinopril is not addictive, some people still need support when they’ve been using it inconsistently, adjusting their own doses, or feeling anxious about their blood pressure.
Treatment in this context is not about “rehab” or “detox,” but about helping the individual get back to safe, stable, and confident use of the medication with proper medical guidance.
Detox / Withdrawal Management
Because lisinopril has no addictive properties, there is no detox process like you would see with substances that affect the brain. Instead, clinicians focus on helping the individual use the medication correctly and managing any rebound blood-pressure changes that occur when doses have been missed or stopped suddenly.
What Treatment Usually Focuses On?
-
Stabilizing dosing: Making sure the person takes the medication consistently, at the same time each day, without skipping or doubling doses. Consistency prevents blood-pressure swings that can feel scary or uncomfortable.
-
Preventing rebound hypertension: When someone stops lisinopril abruptly, their blood pressure may rise again. Doctors help gradually return the body to a stable range without sudden spikes.
-
Addressing anxiety or confusion around medication use: Some individuals worry excessively about blood-pressure readings or believe they need extra doses. Education and reassurance reduce this stress.
Medical Guidance Often Includes:
To help stabilize medication use and ensure safety, clinicians may recommend:
-
Gradual dose adjustments over 1–2 weeks: If someone has been taking the wrong dose or wants to stop the medication, doctors usually adjust slowly instead of abruptly. This prevents sudden blood-pressure changes.
-
Switching medication class (ACE inhibitor → ARB): For people who struggle with side effects like persistent cough, an ARB (such as losartan) may be a safer, easier alternative.
-
Regular monitoring of kidney function and potassium: Because lisinopril affects the kidneys and electrolyte levels, occasional blood tests help ensure the medication is working safely.
-
Reviewing all interacting medications: Many people unknowingly take NSAIDs, diuretics, or potassium supplements that interfere with lisinopril. A medication review helps prevent dangerous interactions.
Medication-Assisted Treatment (MAT)
MAT is not used for lisinopril because there is no addiction or withdrawal to treat. Instead, providers focus on:
-
Ensuring the individual understands proper dosing
-
Managing physical or emotional symptoms related to high blood pressure
-
Helping the person develop confidence in their medication routine
-
Addressing any anxiety that contributes to unsafe use
Think of this stage less like addiction treatment and more like supportive medication management.
Levels of Care
The level of care depends on the person’s symptoms, blood-pressure patterns, and any coexisting health concerns. Because this is not addiction treatment, levels of care focus on medical safety and long-term heart health.
-
Primary Care
This is where most people receive ongoing management for lisinopril.
-
Follow-up visits happen every 3–6 months
-
Blood pressure is monitored over time
-
Kidney function and potassium are checked
-
Doses may be adjusted
-
Side effects and misuse patterns are discussed openly
Primary care is usually sufficient for most individuals.
-
Cardiology Care
Referral to a cardiologist may be recommended when:
-
Someone has severe or difficult-to-control hypertension
-
There is a history of heart failure, heart attack, or arrhythmias
-
Lisinopril is part of a larger heart-health treatment plan
-
Multiple BP medications are needed for stability
Cardiologists can provide more detailed monitoring and tailored treatment.
Behavioral Health Support
Some individuals misuse lisinopril because of psychological factors—particularly anxiety, stress, or fear related to blood pressure. In these cases, behavioral health support can be extremely helpful.
This type of support may address:
-
Anxiety and racing thoughts about blood pressure readings
-
Stress-related BP spikes, which may tempt a person to self-adjust doses
-
Catastrophic thinking, such as believing minor symptoms indicate an emergency
-
Obsessive checking of blood pressure multiple times a day
These factors don’t indicate addiction, but they can lead to misuse that affects overall health.
Therapies
Cognitive Behavioral Therapy (CBT)
CBT helps the individual:
-
Understand the difference between normal BP fluctuations and emergencies
-
Challenge anxious thoughts (“My BP rose 5 points, I need extra medication”)
-
Build predictable medication routines
-
Reduce over-monitoring and reassurance-seeking behaviors
Motivational Interviewing (MI)
MI is ideal for individuals who:
-
Frequently skip doses
-
Are unsure about staying on long-term BP medication
-
Have inconsistent routines
-
Feel frustrated with the idea of “lifelong medication”
Light Family Involvement
Family or loved ones do not need to be heavily involved, but small forms of support can make a positive difference:
-
Coordinating appointments so the person never runs out of medication
-
Providing calm reminders rather than pressure
-
Reducing environmental stress, which can lower blood-pressure spikes
-
Helping monitor interactions, such as remembering to avoid NSAIDs or alcohol
Peer Support & Recovery Capital
These supports are not addiction-focused. Instead, they help people build confidence, routines, and health-friendly habits:
-
Hypertension management groups where people share strategies
-
Chronic disease support networks to promote resilience
-
Anxiety or stress management groups
-
Heart-health education classes
(many are hospital- or community-based)
Holistic Supports
Lifestyle adjustments are one of the most powerful tools for reducing BP fluctuations and preventing misuse of lisinopril.
-
Regular exercise (3 times a week)
Helps stabilize heart function, reduce anxiety, and support healthy BP. -
Low-sodium diet
Salt directly impacts BP; reducing it improves medication effectiveness. -
Proper hydration
Dehydration can increase BP and make side effects feel more severe. -
Mindfulness and relaxation techniques
Simple practices like deep breathing, meditation, or guided relaxation reduce stress-driven BP spikes. -
Limiting caffeine
Too much caffeine can cause jitteriness, anxiety, and BP elevation. -
Consistent sleep routine
Poor sleep is linked to higher BP, increased stress, and medication misuse.
These natural supports help individuals feel more in control and reduce the urge to self-adjust medication.
Withdrawal Timeline (What to Expect)
Lisinopril does not cause withdrawal because it does not act on the brain or create any form of dependence. However, when someone stops the medication suddenly or misses doses for several days, the body responds to the loss of blood-pressure control.
These symptoms can look like withdrawal, but are simply the blood pressure rising to its untreated level.
What Actually Happens Instead of Withdrawal?
-
Blood pressure begins to climb back up, sometimes within a day or two.
This can feel like pounding in the head, tension behind the eyes, or general pressure. -
Headaches develop, especially at the base of the skull or around the temples.
These are “rebound headaches” caused by the return of higher BP. -
Tension in the neck or shoulders
This is common when blood vessels tighten again after the ACE inhibitor is removed. -
Chest discomfort or tightness
Not usually dangerous in healthy individuals, but concerning in those with heart disease. -
Anxiety increases, especially when symptoms are misinterpreted as an emergency.
Many people feel a rush of fear simply from seeing a higher BP reading.
When These Symptoms Appear?
-
Usually begin within 24–72 hours of stopping lisinopril
-
More noticeable in people with high baseline blood pressure
-
Can be worsened by stress, caffeine, dehydration, or poor sleep
How do These Symptoms Improve?
Once lisinopril is restarted or replaced with another medication, the body usually stabilizes again within:
-
24–48 hours for headaches and tension
-
3–7 days for blood-pressure readings to return to baseline
This is not withdrawal, but rather the circulatory system returning to its untreated state.
When to Seek Immediate Help?
Although lisinopril is safe, there are times when a person needs urgent medical attention. These red flags relate to dangerous blood-pressure changes or rare reactions, not addiction.
Seek immediate help for:
-
Severe swelling of the lips, tongue, face, or throat: This may be angioedema—a rare allergic reaction linked to ACE inhibitors.
-
Difficulty breathing: Swelling or extremely low BP can cause shortness of breath or chest tightness.
-
Sudden, crushing chest pain: Especially in individuals with a heart history. This could signal a cardiac event.
-
Extremely high blood pressure readings, especially above
-
180/120 mmHg with symptoms
-
160–180 systolic with chest pressure or headache
These may require urgent medication adjustment. -
Severe dizziness or fainting: Very low BP can result from taking too much lisinopril or mixing it with alcohol/diuretics.
-
Confusion, disorientation, or severe weakness: These can indicate electrolyte imbalance, kidney issues, or dangerously low BP.
Dosing & Safety / Overdose Risks
Understanding dose ranges and safety guidelines helps individuals avoid common misuse patterns and reduces the risk of complications.
Typical Dosage
-
5–40 mg taken once daily, depending on the individual’s condition
-
Most people start at 5–10 mg
-
Doses may be increased gradually based on:
-
Blood-pressure response
-
Kidney function
-
Side effects
-
Coexisting medical issues
High-Risk Combinations
Some substances interfere with lisinopril’s effects or increase side-effect risks.
-
Alcohol
It can cause severe drops in blood pressure, dizziness, or fainting. -
Potassium supplements or salt substitutes (KCl-based)
These can drastically raise potassium levels, risking heart rhythm problems. -
Diuretics (water pills)
May intensify the blood-pressure-lowering effect, especially if doses are doubled. -
NSAIDs (ibuprofen, naproxen, etc.)
Can reduce lisinopril’s effectiveness and strain the kidneys. -
Other blood-pressure medications used unsupervised
Taking extra pills from another prescription can cause dangerously low BP.
Overdose Symptoms
Lisinopril overdose is uncommon but can happen when someone:
-
Doubles up on doses after forgetting
-
Takes additional doses due to anxiety
-
Mixes it with other BP medications
-
Drinks heavily and takes the medication
-
Mistakenly takes someone else’s prescription
Signs of Overdose Include:
-
Very low blood pressure, causing fainting or collapse
-
Extreme dizziness, especially when standing
-
Slow or irregular heartbeat
-
Cold, clammy skin from inadequate circulation
-
Confusion or trouble staying alert
-
Kidney strain, shown by decreased urination or swelling
Conclusion
Lisinopril is a safe and effective medication with no addictive potential, yet it must be used consistently and correctly to protect long-term cardiovascular health. Misuse typically stems from confusion, anxiety, or inconsistent routines—not dependency.
Next Steps
-
Speak with a medical provider if your dosing feels unclear.
-
Review interactions, side effects, and lifestyle changes that support stable blood pressure.
-
If you are experiencing stress around your medication, behavioral support can help regulate routines and reduce anxiety.
FAQs
No. Lisinopril does not interact with brain pathways linked to addiction and cannot create cravings, dependence, or withdrawal. It regulates blood pressure only, so the body does not develop the type of reinforcement that addictive substances produce.
Your blood pressure rises back to its untreated level, which causes headaches, tension, and pressure sensations. This is not a withdrawal. Once you resume your regular dose schedule, those symptoms typically subside as your blood pressure stabilizes again.
Not for addiction reasons. However, doctors may reduce or switch the medication slowly to prevent rebound hypertension. A gradual change helps ensure your blood pressure stays controlled and avoids sudden spikes.
Yes—mainly through incorrect dosing, doubling up, mixing with interacting substances, or adjusting doses without guidance. These patterns are usually accidental and linked to confusion or anxiety rather than intentional misuse.
Take it once daily, avoid doubling doses, limit alcohol, and attend regular checkups to monitor kidney function and BP. Consistency is the key to preventing blood-pressure swings and maximizing the medication’s safety.
Yes. Alcohol can exaggerate the blood-pressure-lowering effect and increase dizziness or fainting. This combination can make it harder to predict how your blood pressure will respond, which raises the risk of sudden drops.







