Lisinopril Withdrawal Risks of Stopping Lisinopril Suddenly
When Lisinopril is present consistently, it blocks the hormone angiotensin II—a chemical that narrows blood vessels and increases blood pressure. Removing the medication abruptly allows angiotensin II activity to spike, which can cause:
-
Rapid increases in blood pressure
-
Dizziness, headaches, neck pressure
-
Chest discomfort due to increased heart workload
-
Shortness of breath caused by elevated vascular resistance
Key Takeaways
-
Is withdrawal real? Not in the addiction sense. Lisinopril does not cause cravings or dependency. However, stopping it suddenly can lead to rebound hypertension, headaches, dizziness, elevated heart strain, and a rapid return of high blood pressure symptoms.
-
How should I stop safely? Lisinopril should be tapered or transitioned under medical supervision. Doctors may adjust dosing over several days or weeks to prevent sudden spikes in blood pressure and minimize cardiovascular risk.
-
What helps recovery? Close monitoring, healthy routines, stress management, family support, and consistent follow-up with a provider help stabilize blood pressure after discontinuation.
Lisinopril is an ACE inhibitor prescribed for hypertension, heart failure, and kidney protection in people with diabetes or chronic kidney disease. It works by relaxing blood vessels and lowering pressure within the cardiovascular system.
When someone stops Lisinopril abruptly, the protective effect on blood vessels is suddenly removed, and the body’s natural hormonal systems—especially the renin-angiotensin system, which raises blood pressure—reactivate quickly.
This leads to a physiological rebound rather than a traditional “withdrawal.” Instead of cravings or dependence, the core risk is that the body’s vasoconstrictive (vessel-tightening) hormones surge rapidly, causing blood pressure to rise.
This response can be uncomfortable for some people and dangerous for others, particularly those with a history of severe hypertension or cardiovascular disease.
Why does sudden stopping cause symptoms?
When Lisinopril is present consistently, it blocks the hormone angiotensin II—a chemical that narrows blood vessels and increases blood pressure. Removing the medication abruptly allows angiotensin II activity to spike, which can cause:
-
Rapid increases in blood pressure
-
Dizziness, headaches, neck pressure
-
Chest discomfort due to increased heart workload
-
Shortness of breath caused by elevated vascular resistance
Families often notice their loved one becoming flushed, irritable, or fatigued because the cardiovascular system is working harder than it should.
Withdrawal vs. hypertension rebound
It’s important to distinguish between two concepts:
-
Withdrawal: Symptoms caused by the body adapting to the absence of a medication that affects brain chemistry. Lisinopril does not cause this.
-
Rebound hypertension: A physiologic surge in blood pressure after stopping a blood pressure medication too quickly. This does happen and is the primary risk[1].
Stopping Lisinopril is not like stopping an antidepressant or benzodiazepine.
There are no neurological withdrawal symptoms. Instead, the concern is the cardiovascular instability created by the sudden absence of medication support.
What Are the Common Symptoms of Lisinopril Withdrawal?
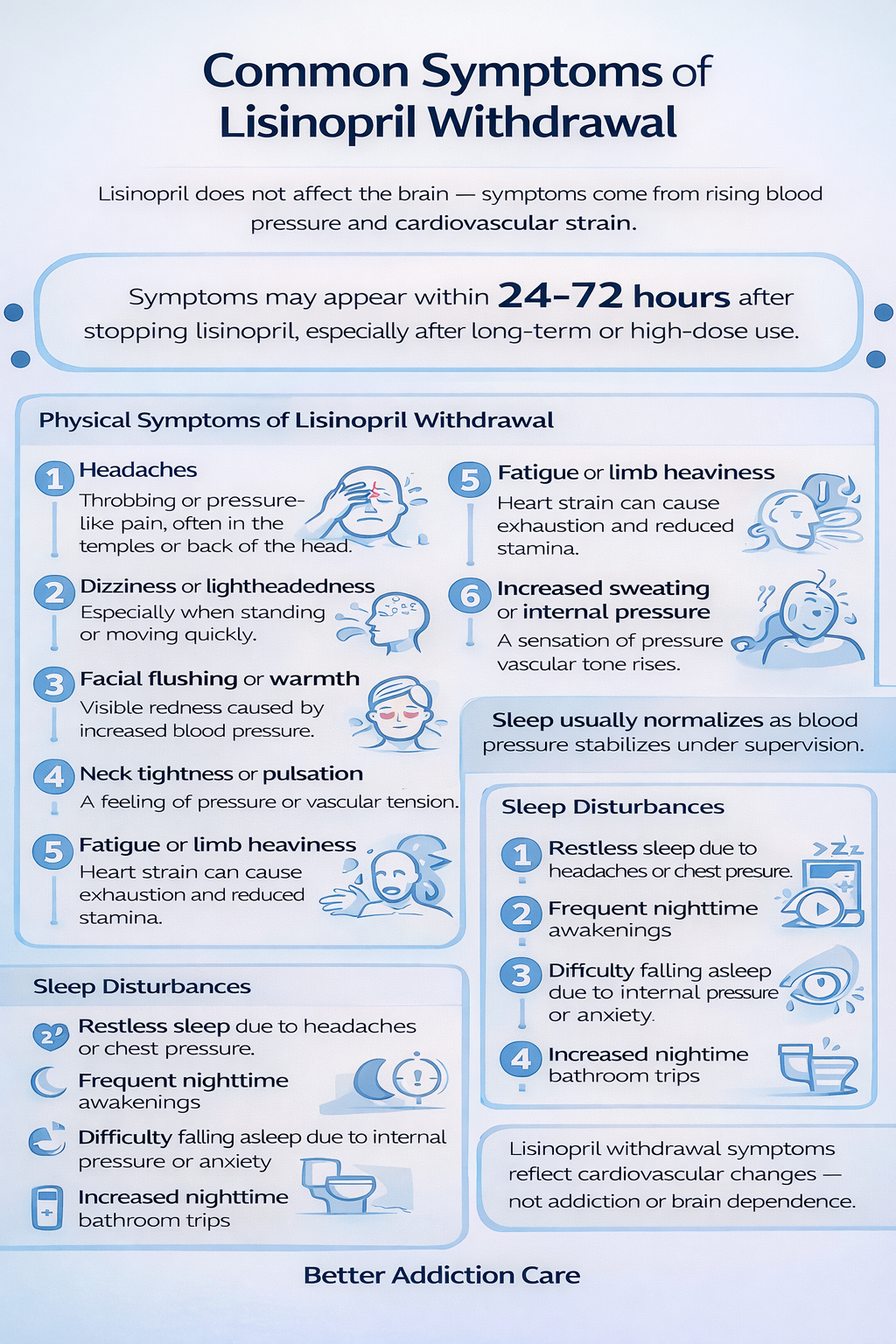
Because Lisinopril acts on blood vessels rather than the brain, symptoms stem from a rise in blood pressure or increased cardiovascular strain. These symptoms can appear within 24–72 hours of stopping the medication, especially if the dose was high or the person was using it long-term.
Physical Symptoms
People may experience noticeable physical changes when blood pressure rises:
-
Headaches, often throbbing or pressure-like, especially in the temples or back of the head
-
Dizziness or lightheadedness when standing or moving quickly
-
Facial flushing, warmth, or visible redness
-
Neck tightness or a feeling of pulsation
-
Fatigue or heaviness in the limbs due to heart strain
-
Increased sweating or a sensation of internal pressure
These physical sensations result from the sudden increase in vascular tone and blood pressure as the medication’s effect wears off.
Sleep Disturbances
Although Lisinopril itself does not directly alter sleep patterns, rebound hypertension can lead to:
-
Restless nights due to chest pressure or headaches
-
Frequent nighttime awakenings
-
Difficulty settling into sleep because of internal “pressure” or anxiety
-
Nighttime bathroom trips if blood pressure becomes elevated
As blood pressure stabilizes through a supervised taper, sleep patterns usually return to normal.
Emotional and Mental Health Symptoms
Cardiovascular instability often affects mood because discomfort and internal pressure can create distress. People may experience:
-
Irritability or agitation when blood pressure spikes
-
Anxiety, often triggered by physical symptoms
-
Difficulty staying focused due to headaches or chest pressure
-
Emotional sensitivity when symptoms interfere with daily tasks
These emotional responses are natural reactions to cardiovascular discomfort, not psychological withdrawal.
Sensory or Neurological Symptoms
Because high blood pressure affects blood flow to the brain and sensory pathways, some individuals notice:
-
Visual disturbances, such as blurriness
-
Light sensitivity during headache episodes
-
Ringing in the ears (pulsatile tinnitus)
-
Brief episodes of jitteriness or tremors
-
A feeling of “pressure” behind the eyes
These symptoms generally improve once blood pressure stabilizes under medical supervision.
What Is the Typical Lisinopril Withdrawal Timeline?
While experiences vary, especially depending on dose and health conditions, the progression follows predictable phases.
Withdrawal Progression (Phases & What to Expect)
Note: Timelines vary based on the dose being reduced, how long the medication was used, the individual’s health profile, and the speed of the taper.
First Few Days (Days 1–3): Early Physiological Shift
In the first 48–72 hours, the body begins adjusting to the absence of ACE inhibition. People often notice headaches, dizziness, neck pressure, or general discomfort. Blood pressure readings may start trending upward during this period.
Peak Discomfort (Weeks 1–2): Strongest Rebound Effects
This phase carries the greatest risk because blood pressure may fluctuate significantly. Individuals may experience:
-
Persistent headaches
-
Elevated systolic and diastolic pressures
-
Heightened anxiety due to physical symptoms
-
Fatigue from increased heart workload
-
Occasional chest tightness or breathlessness
This is when medical supervision is most important, and tapering adjustments may be needed[2].
Improvement Phase (Weeks 3–4): Cardiovascular Stabilization
As the taper continues or as a new medication takes effect, people typically notice steady improvement.
Symptoms such as headaches and dizziness lessen, blood pressure stabilizes, and emotional tension decreases. Many individuals report clearer thinking, improved sleep, and steadier daily functioning.
Adjustment Phase (1 Month+): Returning to Baseline Rhythm
Over the next month, the cardiovascular system adapts to the new routine.
Mild fluctuations in energy or blood pressure may still occur, especially during stress or poor sleep, but overall stability improves. Families often notice their loved one becoming more relaxed and comfortable as daily routines settle.
Why Should Lisinopril Be Tapered Slowly?
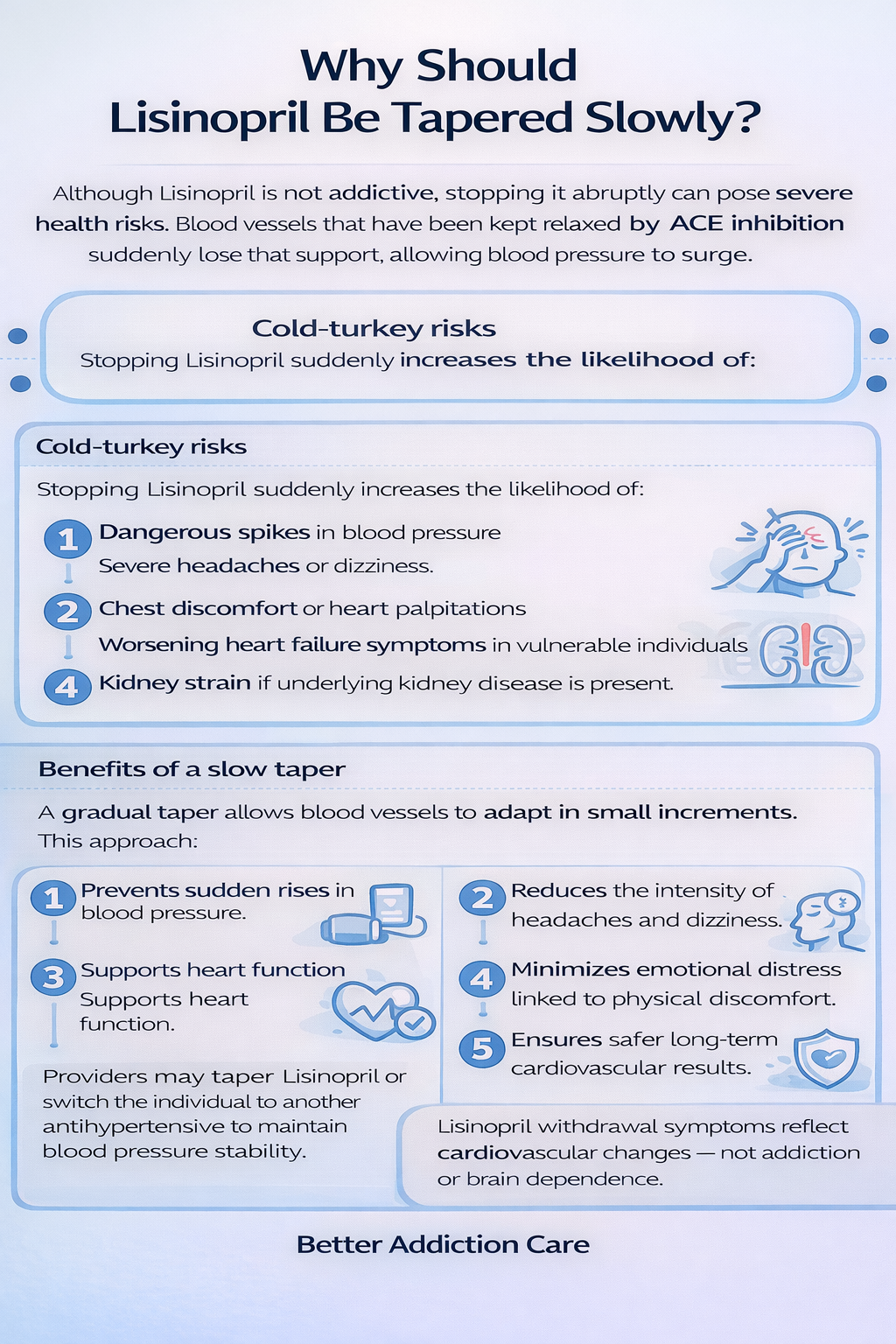
Although Lisinopril is not addictive, stopping it abruptly can pose severe health risks. Blood vessels that have been kept relaxed by ACE inhibition suddenly lose that support, allowing blood pressure to surge.
Cold-turkey risks
Stopping Lisinopril suddenly increases the likelihood of:
-
Dangerous spikes in blood pressure
-
Severe headaches or dizziness
-
Chest discomfort or heart palpitations
-
Worsening heart failure symptoms in vulnerable individuals
-
Kidney strain if underlying kidney disease is present
Benefits of a slow taper
A gradual taper allows blood vessels to adapt in small increments. This approach:
-
Prevents sudden rises in blood pressure
-
Reduces the intensity of headaches and dizziness
-
Supports heart function
-
Minimizes emotional distress linked to physical discomfort
-
Ensures safer long-term cardiovascular results
Providers may taper Lisinopril or switch the individual to another antihypertensive to maintain blood pressure stability.
What Helps Manage Lisinopril Withdrawal Symptoms?
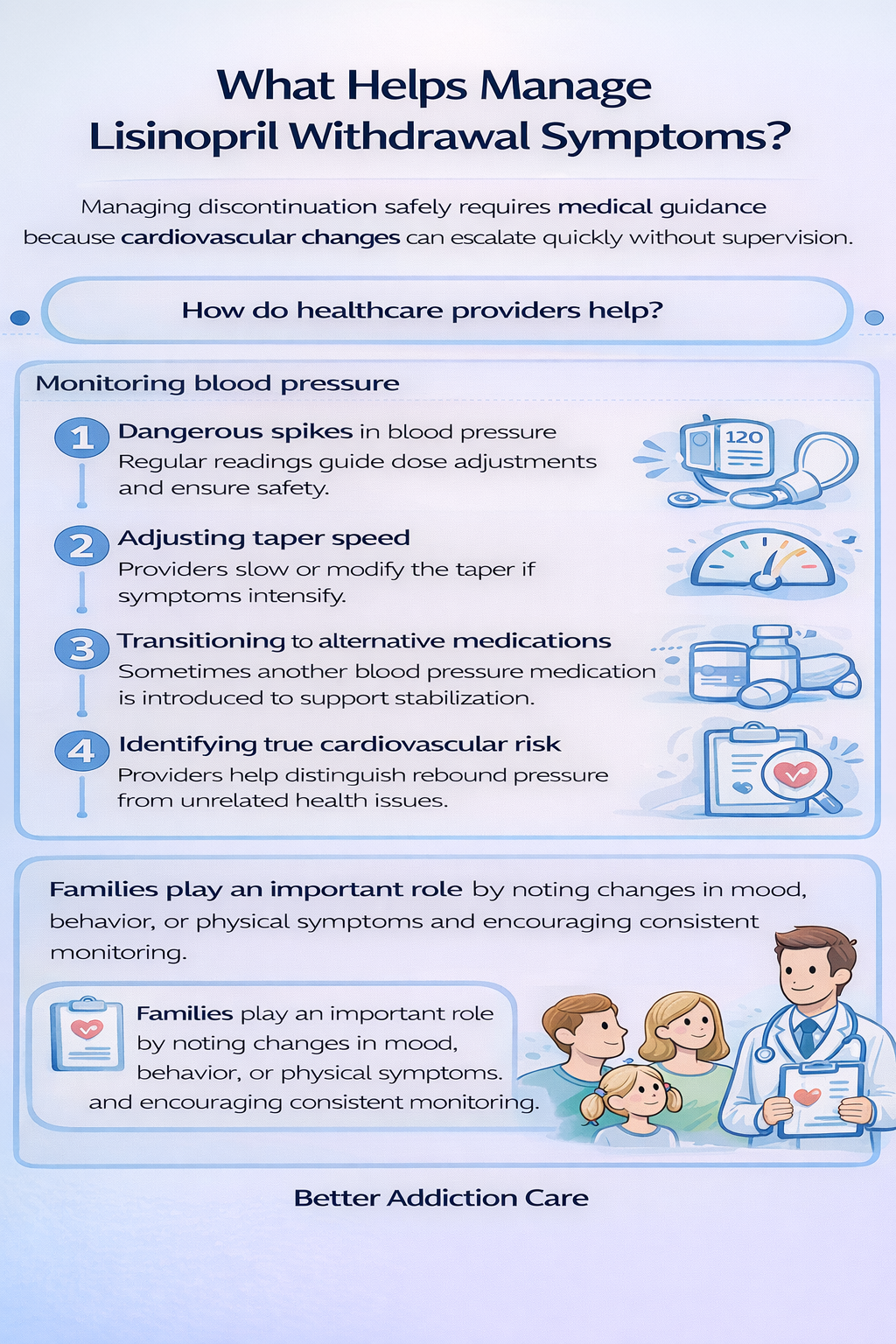
Managing discontinuation safely requires medical guidance because cardiovascular changes can escalate quickly without supervision.
How do healthcare providers help?
-
Monitoring blood pressure: Regular readings guide dose adjustments and ensure safety.
-
Adjusting taper speed: Providers slow or modify the taper if symptoms intensify.
-
Transitioning to alternative medications: Sometimes another blood pressure medication is introduced to support stabilization.
-
Identifying true cardiovascular risk: Providers help distinguish rebound pressure from unrelated health issues.
Families play an important role by noting changes in mood, behavior, or physical symptoms and encouraging consistent monitoring.
What Coping Strategies Help Manage Withdrawal Symptoms?
These strategies support cardiovascular stability, emotional steadiness, and daily functioning. They are most effective when practiced consistently and coordinated with medical supervision.
1. How Can I Improve My Sleep?
Stabilizing sleep helps regulate blood pressure. A consistent sleep schedule reinforces circadian rhythm, while minimizing screens and bright lights before bedtime helps calm the nervous system. Relaxation activities—gentle stretching, warm showers, or quiet reading—can ease tension.
If elevated nighttime pressure causes restlessness, deep breathing, weighted blankets, and a cool sleep environment may help. Families can support this by maintaining calm evening routines.
2. What Should I Eat and Drink During Withdrawal?
Hydration supports cardiovascular balance. Drinking 6–8 glasses of water daily helps blood flow and reduces fatigue. Meals should include steady protein sources, leafy greens, and foods rich in potassium—important for blood pressure stability. Reducing sodium and limiting caffeine may lower spikes in pressure or jitteriness.
3. Should I Exercise?
Gentle movement promotes healthy circulation. Walking for 20–30 minutes, stretching, or low-impact exercise can reduce tension and support cardiovascular function. Intense workouts that suddenly raise heart rate should be avoided during early stabilization unless approved by a provider. Families can join in daily walks, creating supportive routines.
4. How Can I Reduce Stress and Anxiety?
Cardiovascular symptoms can trigger emotional tension. Breathing exercises that extend the exhale—like inhaling for four seconds and exhaling for six—activate the parasympathetic nervous system. Journaling helps process fear or discomfort. Sensory grounding, such as warm tea, soft lighting, or quiet spaces, calms the body. Brief mindfulness practices help redirect attention away from physical symptoms.
5. How Can I Stay Connected and Supported?
Connection improves emotional stability. Daily check-ins with loved ones, shared meals, and regular conversation reduce isolation and help manage symptom-related stress. Peer support groups, online or in person, provide reassurance and normalize the experience of managing a blood pressure condition.
6. Does Routine Matter?
Routine plays a major role in stabilizing blood pressure. Consistent waking times, regular meals, moderate exercise, and planned daily activities regulate the nervous system. Predictability reduces anxiety and strengthens emotional steadiness during cardiovascular adjustment.
When Should I Seek Medical Help During Withdrawal?
Medical oversight is crucial when stopping or reducing Lisinopril. Seek immediate help if any of the following occur:
-
Severe headaches accompanied by high blood pressure
-
Chest pain, tightness, or shortness of breath
-
Sudden swelling in legs, feet, or hands
-
Vision changes or confusion
-
Repeated blood pressure readings in the hypertensive range
-
Persistent dizziness or fainting episodes
-
Extreme fatigue or signs of heart strain
These symptoms require urgent evaluation because they may signal significant blood pressure elevation or cardiovascular stress [3].
What Comes After Withdrawal?
Long-term recovery focuses on stabilizing cardiovascular health and establishing routines that protect blood pressure.
Over the next 1–3 months, people usually regain stability as their body adjusts to the new plan created by their provider.
Long-term strategies include:
-
Regular medical appointments
-
Blood pressure monitoring at home
-
Consistent exercise routines
-
Heart-healthy nutrition
-
Stress-management skills
-
Limiting alcohol and smoking
-
Supportive family communication
The goal is not just stabilizing blood pressure but creating sustainable habits that protect long-term cardiovascular health.
Conclusion
Lisinopril does not cause traditional withdrawal, but stopping it abruptly can lead to dangerous rebounds in blood pressure and cardiovascular strain. With a gradual taper, continuous monitoring, medical guidance, and strong family support, most individuals stabilize safely and return to healthy routines.
Patience, consistency, and collaboration with a healthcare provider are the keys to a safe and successful discontinuation process.
FAQs
No. Stopping Lisinopril suddenly can make blood pressure rise quickly, which may lead to headaches, dizziness, chest discomfort, and cardiovascular strain. These changes can be dangerous, especially if you already have heart or kidney issues. The safest approach is a gradual, medically supervised taper so blood vessels adjust slowly and blood pressure remains stable during the transition.
Rebound symptoms usually appear within the first few days and peak during the first one to two weeks. Most people notice improvement as their taper continues or when another medication is introduced. Mild fluctuations—such as brief headaches or pressure changes—may last several more weeks, depending on overall health, stress levels, and the original dose taken.
It can be if the medication is stopped abruptly. While Lisinopril does not cause addiction, sudden discontinuation can trigger rebound hypertension, which puts extra stress on the heart and blood vessels. This may be risky for individuals with conditions like heart disease or kidney problems. Tapering slowly and checking blood pressure regularly reduces these risks significantly.
Loved ones can support by helping track blood pressure, maintaining calm routines, encouraging gentle activity, and reminding the person to follow medical guidance. Their presence provides reassurance during physical discomfort and helps identify concerning symptoms early. Attending appointments together or sharing simple daily habits, such as walks or structured meals, makes the process feel more manageable.
It often will, especially if Lisinopril was keeping high blood pressure controlled. When the medication is removed suddenly, blood vessels tighten again, causing levels to rise. Doctors may taper the dose slowly or switch you to another medication to prevent spikes. Monitoring at home helps catch changes early so treatment can be adjusted safely.
Seek immediate medical attention if you experience intense headaches, chest pressure, rapid heartbeat, or very high blood pressure readings. These may signal a dangerous spike that needs urgent care. Do not wait for symptoms to settle on their own. A provider can determine whether medication needs to be restarted, tapered differently, or replaced to protect heart and kidney health.







