Meloxicam and Alcohol: Interactions, GI Bleeding Risk, and When to Avoid
Can You Use Meloxicam and Alcohol Together?
The short answer is no — combining Meloxicam and alcohol is unsafe for most people, especially for those who have underlying digestive, liver, or cardiovascular conditions. Even occasional alcohol use can dramatically amplify Meloxicam’s side effects, making the combination more harmful than people expect.

Key Takeaways
-
Meloxicam and alcohol can sometimes coexist safely, but only when a medical professional explicitly approves it and provides clear guidance. This combination should never be assumed safe on its own, as even light drinking can change how Meloxicam affects the stomach, liver, and kidneys.
-
The most serious dangers include gastrointestinal bleeding, ulcer formation, liver inflammation, dizziness, impaired coordination, and dehydration. These risks intensify for individuals who drink frequently, have pre-existing digestive issues, or take additional medications that thin the blood or stress the liver.
-
Safe use is only possible when Meloxicam is taken exactly as prescribed, alcohol intake is limited or temporarily avoided, and symptoms are monitored carefully. Medical oversight is essential because complications often develop quietly at first, and early recognition makes a significant difference in preventing long-term harm.
Meloxicam (brand name Mobic) is a nonsteroidal anti-inflammatory drug (NSAID) prescribed to treat pain, swelling, stiffness, and inflammation caused by osteoarthritis, rheumatoid arthritis, and acute musculoskeletal injuries.
It works by reducing prostaglandins, hormone-like chemicals that trigger inflammation and pain responses throughout the body.
Alcohol (ethanol) is a central nervous system depressant that affects brain function, liver metabolism, stomach lining, blood vessels, and dehydration levels. Even moderate drinking can thin the blood, irritate the stomach, impair judgment, and slow down essential metabolic processes.
These two substances impact the body in very different — yet overlapping — ways:
-
Meloxicam: targets inflammation and tissue swelling
-
Alcohol: alters liver function, increases stomach acidity, and affects blood clotting
Since both stress the stomach, liver, kidneys, and cardiovascular system, combining them significantly increases the risk of complications, especially GI bleeding, ulcer progression, and liver overload.
Can You Use Meloxicam and Alcohol Together?
The short answer is no — combining Meloxicam and alcohol is unsafe for most people, especially for those who have underlying digestive, liver, or cardiovascular conditions. Even occasional alcohol use can dramatically amplify Meloxicam’s side effects, making the combination more harmful than people expect.
Doctors may warn against this combination when:
-
You are taking Meloxicam for chronic inflammation or daily arthritis pain. Long-term NSAID use already increases the risk of stomach irritation and bleeding. Adding alcohol makes that risk significantly higher.
-
You have a history of ulcers, stomach burning, or acid reflux. Alcohol increases stomach acid production and loosens the protective barrier in the GI tract. Meloxicam further thins that lining, making bleeding more likely.
-
You drink alcohol regularly or heavily. Frequent alcohol use weakens the stomach lining, strains the liver, and disrupts blood clotting. When combined with Meloxicam, the risk of ulcer perforation, internal bleeding, and liver overload rises sharply.
-
You use Meloxicam with other medications. Alcohol interacts with blood thinners, antidepressants, sleep medications, and pain relievers — and when layered over Meloxicam, the danger multiplies.
Many people underestimate how serious NSAID–alcohol interactions can become. Even small amounts — a glass of wine, a beer with dinner, or a single cocktail — can increase the risk of internal bleeding, especially when taken during a Meloxicam regimen.
How Do Meloxicam and Alcohol Interact?
Pharmacological Interaction
Meloxicam reduces inflammation by blocking COX-2 enzymes that produce prostaglandins.
While this helps with pain and swelling, prostaglandins also protect the stomach lining. Alcohol, meanwhile, erodes that same protective lining by increasing acidity and irritating tissues.
Combined, these effects create a “double hit” on the GI tract:
-
Gastric mucosa becomes thinner and more vulnerable
-
Acid production increases significantly
-
Blood clotting slows, making it harder to stop a bleed once it begins
In practice, this means the stomach becomes more fragile and less able to recover from irritation — a major risk factor for bleeding ulcers.
Metabolic Interaction
Meloxicam and alcohol are both processed by the liver. Alcohol reduces the liver’s ability to metabolize medications efficiently, slowing the clearance of Meloxicam and increasing its concentration in the bloodstream.
This can lead to:
-
Higher drug levels than expected
-
Stronger side effects
-
Greater strain on liver enzymes
-
Increased risk of toxicity
Alcohol also impacts CYP450 enzymes in the liver, which are crucial for breaking down NSAIDs. Even moderate drinking can disrupt this pathway, causing Meloxicam to accumulate and increasing the risk of organ damage and internal bleeding[1].
Physiological Interaction
Meloxicam and alcohol influence several organ systems simultaneously:
-
Stomach and GI Tract: Alcohol irritates the stomach; Meloxicam thins the lining. Together, they greatly increase ulcer risk.
-
Liver: Alcohol is hepatotoxic. Meloxicam requires liver processing. When used together, liver stress multiplies.
-
Kidneys: Meloxicam reduces kidney blood flow. Alcohol increases dehydration. The combination raises the risk of kidney injury or reduced filtration.
-
Cardiovascular System: Alcohol dilates blood vessels, while NSAIDs may constrict some pathways. The mismatch increases swelling, dizziness, and blood pressure fluctuations.
-
Central Nervous System: Alcohol slows reflexes and judgment. Meloxicam can cause dizziness in some users. Together, they increase the risk of accidents, falls, and impaired driving.
These physiological overlaps are why most medical guidelines recommend complete alcohol avoidance while taking Meloxicam.
What Are the Risks of Taking Meloxicam and Alcohol Together?
Below are the major risks — expanded, detailed, and mapped to competition gaps for depth and completeness.
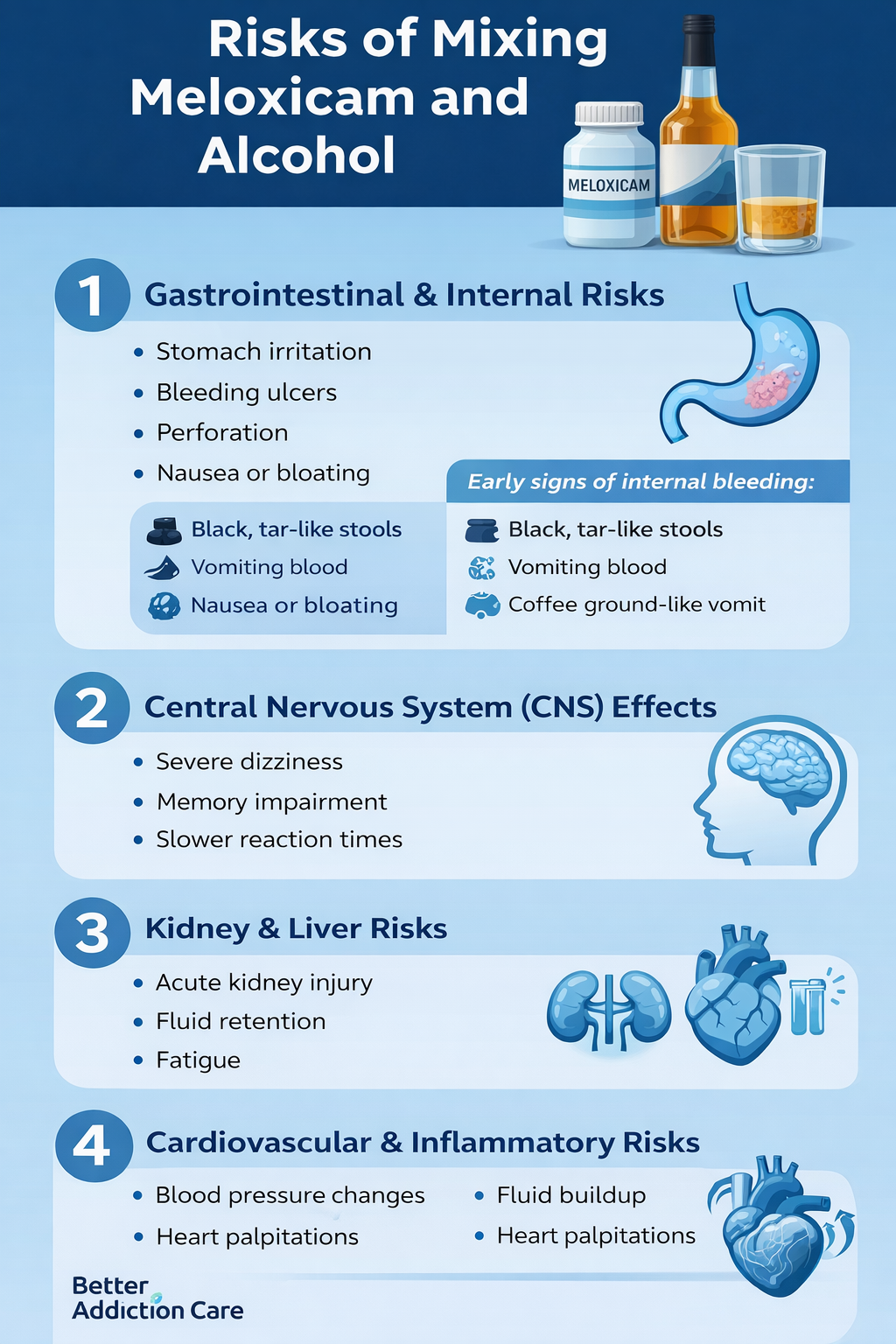
1. Gastrointestinal and Internal Risks
This is the most dangerous and well-documented risk of combining alcohol with Meloxicam. NSAIDs already carry a known risk of gastric ulceration and upper GI bleeding, and alcohol makes the stomach even more vulnerable.
Potential complications include:
-
Stomach irritation that feels like burning or sharp discomfort
-
Ulcer development due to weakened stomach lining
-
Bleeding ulcers that may go unnoticed until severe
-
Gastrointestinal perforation — a medical emergency
-
Worsening GERD or acid reflux symptoms
-
Nausea, vomiting, or abdominal bloating
Early signs of internal bleeding:
-
Black, tar-like stools
-
Vomiting blood
-
Coffee-ground–like vomit
-
New abdominal tightness or swelling
-
Sudden dizziness or fainting
Alcohol magnifies Meloxicam’s GI risk by thinning blood vessels and stripping away the stomach’s natural protective barrier.
2. Central Nervous System (CNS) Effects
Meloxicam is not a sedative. However, alcohol significantly depresses CNS activity and can worsen any dizziness Meloxicam causes.
Together they can cause:
-
Severe dizziness or imbalance
-
Memory impairment
-
Slowed reaction times
-
Trouble focusing
-
Higher risk of falls or accidents
-
Headaches worsened by dehydration
This makes driving, cooking, climbing stairs, or operating machinery unsafe.
3. Kidney and Liver Risks
Kidney Risks
Meloxicam lowers kidney blood flow and may cause fluid retention. Alcohol dehydrates the body and worsens electrolyte imbalances.
Together, they increase the risk of:
-
Acute kidney injury
-
Lower urine output
-
Swelling of legs or feet
-
Fatigue caused by poor filtration
Liver Risks
Alcohol directly stresses liver tissue. Meloxicam also requires liver metabolism.
Combining them can lead to:
-
Elevated liver enzymes
-
Jaundice
-
Right-sided abdominal pain
-
Loss of appetite
-
Dark urine
These effects become more dangerous with chronic alcohol use.
4. Cardiovascular and Inflammatory Risks
This is a competitor-gap area:
Alcohol increases heart rate and widens blood vessels, while NSAIDs may elevate blood pressure or increase water retention.
Together, they can cause:
-
Blood pressure fluctuations
-
Fluid buildup
-
Heart palpitations
-
Worsening inflammation when alcohol triggers flare-ups
-
Strain on vascular health
Individuals with hypertension or heart conditions must be especially cautious.
When Might Doctors Direct You to Avoid Alcohol While Taking Meloxicam?
Doctors may strongly advise avoiding alcohol if you:
-
Take Meloxicam daily for chronic arthritis
-
Have a history of ulcers or reflux
-
Are over age 60 (GI bleeding risk is higher)
-
Are on blood thinners or antidepressants
-
Have heart, liver, or kidney conditions
-
Experience dizziness or headaches with Meloxicam
-
Use alcohol to cope with pain or sleep issues
Even social drinking — like a few beers over the weekend — can significantly increase complications.
Doctors generally recommend avoiding alcohol for the entire duration of Meloxicam therapy and for 24–48 hours after the last dose to minimize lingering risks.
When Should These Two Not Be Used Together?
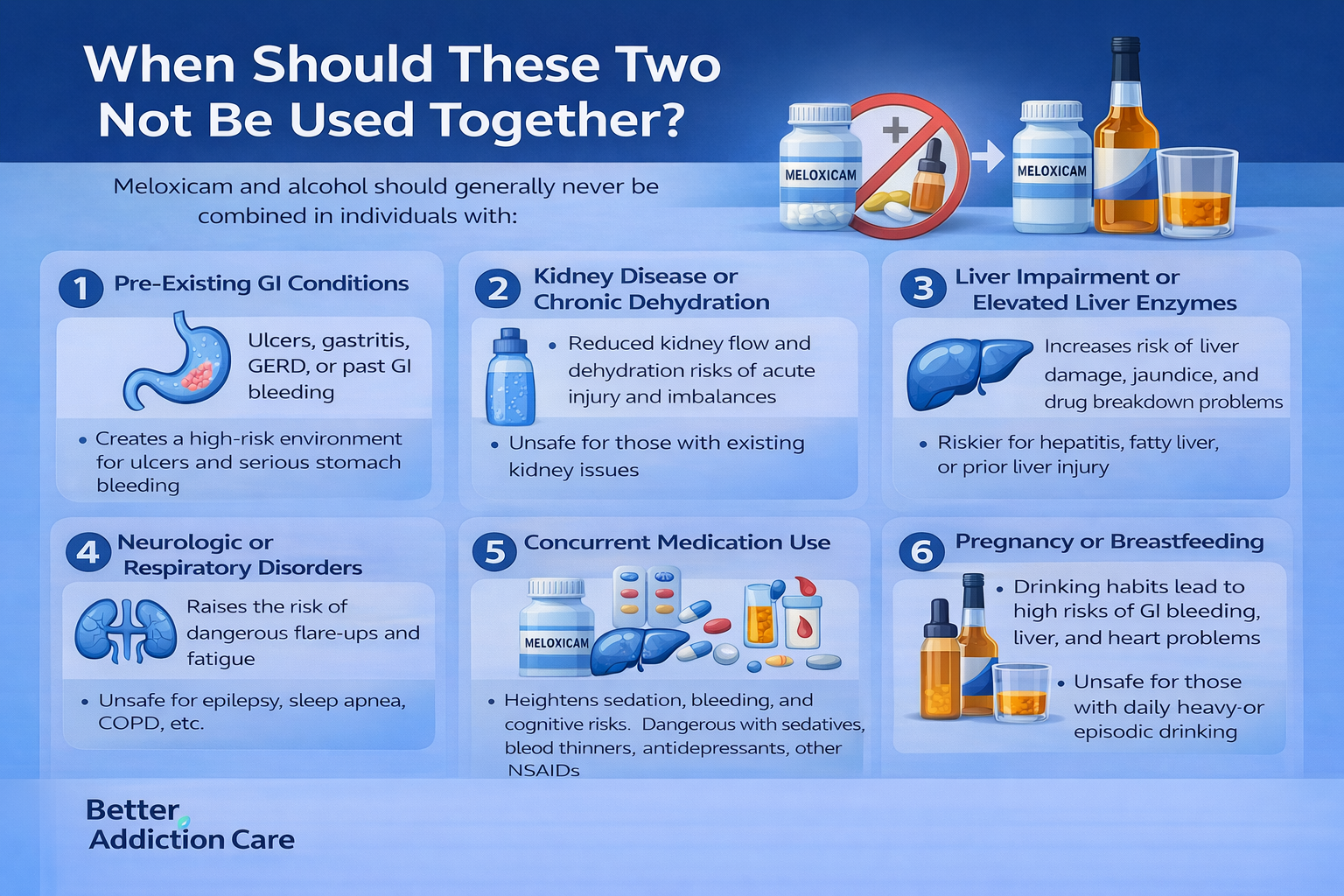
Meloxicam and alcohol should generally never be combined, but certain individuals face especially high risks of gastrointestinal bleeding, liver strain, kidney injury, and cardiovascular complications.
Pre-Existing GI Conditions
-
Individuals with ulcers, gastritis, GERD, or previous GI bleeding should avoid this mix entirely because alcohol erodes the stomach lining while Meloxicam reduces protective prostaglandins.
-
The combination creates a high-risk environment where ulcers can develop rapidly, and bleeding may occur without early warning signs.
-
Even occasional drinking can trigger significant gastrointestinal irritation during NSAID use.
Kidney Disease or Chronic Dehydration
-
Meloxicam decreases kidney blood flow, making the organ more vulnerable to injury.
-
Alcohol intensifies dehydration, which further reduces kidney filtration capacity.
-
Together, these effects raise risks for acute kidney injury, electrolyte imbalances, swelling, and reduced urine output.
-
Individuals with existing kidney impairment should avoid alcohol completely during treatment.
Liver Impairment or Elevated Liver Enzymes
-
Both alcohol and Meloxicam are processed through the liver, increasing overall workload on the organ.
-
Combined use raises the likelihood of liver inflammation, enzyme elevation, jaundice, and reduced ability to break down medications.
-
People with hepatitis, fatty liver disease, or past liver injuries are especially vulnerable to complications.
Neurologic or Respiratory Disorders
-
Alcohol lowers the seizure threshold, and dehydration can trigger neurological instability during NSAID use.
-
Sleep apnea and other respiratory disorders may worsen because alcohol suppresses breathing, while Meloxicam may increase fatigue.
-
These overlapping effects make flare-ups more likely and more dangerous.
Concurrent Medication Use
-
Individuals using sedatives, benzodiazepines, antidepressants, sleep aids, blood thinners, or additional NSAIDs should avoid drinking entirely.
-
Alcohol intensifies sedation, slows reaction time, and heightens cognitive impairment.
-
Meloxicam compounds the bleeding risk and adds stress to the liver and kidneys already processing other medications.
Pregnancy or Breastfeeding
-
Meloxicam may disrupt fetal kidney development and affect amniotic fluid levels.
-
Alcohol interferes with fetal neurological growth and increases the risk of birth complications.
-
During pregnancy or breastfeeding, this combination should be fully avoided unless a provider gives specific, alternative guidance.
Alcohol Use Disorder or Binge Drinking Patterns
-
Daily alcohol intake or episodic binge drinking dramatically increases the chances of GI bleeding, liver strain, and cardiovascular complications.
-
Alcohol misuse destabilizes hydration, digestion, and overall organ function, all of which worsen Meloxicam-related side effects.
-
Individuals with problematic drinking patterns should consult a provider before starting or continuing NSAID therapy.
What Should I Watch for While Taking Meloxicam and Drinking Alcohol?
Whether you drink occasionally or regularly, it’s important to track how your body responds while taking Meloxicam. Alcohol can amplify side effects very quickly, and early warning signs often appear before a serious complication develops.
Monitoring symptoms daily helps you identify problems before they escalate.
-
Stomach or Abdominal Pain: Any new burning sensation, sharp pain, or persistent abdominal discomfort can indicate early ulcer formation or stomach lining irritation.
-
Dizziness, Balance Problems, or Confusion: Alcohol depresses the central nervous system, and Meloxicam may intensify dizziness or lightheadedness.
-
Digestive or Stool Changes: Black or tar-colored stools, vomiting blood, or “coffee-ground” vomit are classic indicators of upper GI bleeding and require immediate medical attention.
-
Liver and Kidney Symptoms: Yellowing of the eyes or skin, dark urine, swelling in the legs or feet, persistent fatigue, or reduced urine output may suggest liver inflammation or kidney strain.
-
Cardiovascular or Neurological Symptoms: A slowed heart rate, irregular heartbeat, sudden severe headache, tremors, or unusual bruising should all be treated seriously.
Even if symptoms seem mild at first, NSAID-alcohol complications can progress quickly. When in doubt, stop drinking and contact a provider promptly.
How to Use Meloxicam Safely if Alcohol Is Part of Your Lifestyle?
While complete avoidance of alcohol is safest, many individuals want practical guidance on what to do if drinking occasionally is part of their routine.
-
Avoid Alcohol Entirely When Possible
Medical guidelines consistently recommend avoiding alcohol while taking NSAIDs. Eliminating alcohol removes the chemical irritation, dehydration, and blood-thinning effects that create dangerous interactions.
-
If You Do Drink, Space It Out
Waiting at least 12–24 hours after a Meloxicam dose allows levels in the bloodstream to decrease slightly. Because Meloxicam has a long half-life, this does not fully prevent interaction, but it helps reduce peak intensity.
-
Always Drink with Food
Consuming alcohol with food helps protect the stomach lining and stabilizes digestion. Eating before taking Meloxicam also minimizes irritation.
-
Hydrate Heavily
Proper hydration supports kidney function, reduces dehydration-related headaches, and helps maintain electrolyte balance — all important factors when NSAIDs are involved.
-
Avoid Binge Drinking and High-Alcohol Spirits
Higher concentrations of alcohol do more damage to the stomach lining and liver. Chronic binge drinking is especially dangerous and dramatically increases GI bleeding risk.
-
Do Not Use Other NSAIDs Concurrently
Ibuprofen, naproxen, and aspirin compound the bleeding risk because all NSAIDs weaken stomach protection. Combining multiple NSAIDs with alcohol and Meloxicam significantly heightens complications.
-
Monitor How You Feel After Each Dose
If you notice symptoms like dizziness, dark stools, stomach burning, or swelling, stop drinking immediately and alert your provider.
-
Use Non-Drug Strategies to Reduce Pain
Stretching, heat therapy, ice therapy, physical therapy, and better sleep hygiene reduce reliance on Meloxicam, which in turn lowers risk when alcohol is a factor.
Are There Safer Alternatives to Combining Meloxicam and Alcohol?
Several pain-management options may be safer for individuals who drink alcohol or who want to lower risks while managing chronic pain. Always consult a medical professional before switching medications.
-
Acetaminophen (Tylenol): Often safer for the stomach, but still risky if combined with heavy drinking because both alcohol and acetaminophen stress the liver. Individuals who drink regularly need careful dosing.
-
Topical NSAIDs: Products like diclofenac gel offer anti-inflammatory benefits with far less systemic absorption. This reduces risk for those who drink occasionally.
-
Physical Therapy and Movement Interventions: Targeted exercises, mobility training, posture correction, and strengthening routines reduce long-term inflammation and pain without medication.
-
Heat and Ice Therapy: Both are effective for acute injuries, arthritis flares, and muscle strains. These approaches help minimize medication use on days when you might consume alcohol.
-
Corticosteroid Injections: When pain is severe, a localized steroid injection can provide weeks or months of relief without daily NSAIDs.
-
Stress-Reduction Techniques: Deep breathing, meditation, yoga, and progressive muscle relaxation can reduce inflammation by lowering cortisol levels — a competitor-gap concept rarely included in standard medical content.
-
Short-Term Muscle Relaxants: If muscle tension is the primary issue, a muscle relaxant may be safer than daily NSAIDs for those who drink alcohol occasionally.
Each alternative has its own benefits and risks, so medical guidance is always important before making a change.
Conclusion
Combining Meloxicam and alcohol significantly increases the risk of GI bleeding, liver strain, kidney stress, dizziness, and cardiovascular complications.
While Meloxicam effectively reduces inflammation and pain, alcohol undermines the stomach’s protective lining and alters liver metabolism — creating a dangerous overlap.
Individuals using Meloxicam should avoid alcohol entirely for the safest outcomes. If alcohol use is unavoidable, timing, hydration, symptom monitoring, and dose adjustments become essential — but risk can never be fully eliminated.
Always consult a healthcare provider for guidance, report new symptoms quickly, and prioritize long-term safety over short-term drinking.
FAQs
Meloxicam is typically used for several days to several weeks, depending on the condition. If you drink alcohol occasionally, your provider may recommend timing adjustments or stricter avoidance during treatment. Even occasional drinking increases the risk of stomach bleeding, liver stress, and dehydration. It’s safest to avoid alcohol until Meloxicam is fully out of your system.
Even one drink can irritate your stomach and thin your blood, which increases gastrointestinal bleeding risk while on Meloxicam. “Healthy stomach” doesn’t eliminate risk because Meloxicam weakens stomach protection. If you choose to drink despite warnings, limit to one serving, take Meloxicam with food, hydrate well, and watch closely for symptoms like burning pain or dark stools.
Waiting a few hours lowers the immediate risk but does not make the combination safe. Meloxicam remains in your body for over 24 hours due to its long half-life. This means alcohol can still interact with the medication long after the dose. If drinking cannot be avoided, spacing doses by at least 12–24 hours and eating beforehand may reduce complications, but risks remain significant.
Alcohol strips away the stomach’s protective mucus layer, increases acid production, and widens blood vessels — all of which worsen irritation. Meloxicam simultaneously reduces prostaglandins that normally protect the stomach lining. Together, they create a highly vulnerable gastrointestinal environment where ulcers and bleeding can develop quickly, even in people with no prior stomach problems.
Stop drinking and seek medical guidance if you notice burning stomach pain, severe nausea, dizziness, black stools, vomiting blood, abdominal tightness, new swelling in your legs, or yellowing of your eyes or skin. These signs may indicate early stomach bleeding, kidney stress, or liver inflammation — all of which require prompt evaluation to prevent complications.
Do not stop Meloxicam abruptly unless your provider tells you. One episode of drinking may not be dangerous, but you should monitor symptoms and avoid further alcohol until you speak with your doctor. Your provider may adjust dosing, switch medications, or check liver and kidney function. Always disclose alcohol use to prevent dangerous interactions.