Meloxicam Interactions Alcohol, Drugs & Safety Concerns
With meloxicam, interactions often involve increased strain on organs or heightened risk of side effects rather than immediate intoxication.

People search for medication interactions because they want to stay safe—not because they’re trying to misuse a drug.
For individuals managing pain, supporting a loved one, or navigating recovery, understanding how meloxicam interacts with alcohol and other substances can prevent unnecessary harm.
Interactions aren’t just theoretical risks; they can affect judgment, physical safety, emotional stability, and long-term health. Being informed allows people to make decisions rooted in protection, not fear.
What Is Meloxicam?
Meloxicam is a prescription nonsteroidal anti-inflammatory drug (NSAID). It is commonly used to treat pain, stiffness, and inflammation associated with conditions such as osteoarthritis, rheumatoid arthritis, joint injuries, and other musculoskeletal disorders[1]. Its primary function is to reduce inflammation by inhibiting enzymes involved in the body’s inflammatory response.
Unlike opioid pain medications, meloxicam does not act on the brain’s reward system and does not produce euphoria or sedation as its primary effect. It is also different from muscle relaxants, which directly affect neuromuscular activity. Because of this, meloxicam is often viewed as a safer long-term option for pain management.
However, “safer” does not mean “risk-free.” Meloxicam affects multiple systems in the body, particularly the gastrointestinal tract, kidneys, cardiovascular system, and—indirectly—the nervous system.
Understanding this broader impact is essential when considering how it may interact with alcohol, other medications, or non-prescribed substances.
How Meloxicam Affects the Central Nervous System?
Meloxicam does not directly depress the central nervous system (CNS) in the way opioids, benzodiazepines, or sleep medications do. That distinction is important—but it can also be misleading. While meloxicam’s primary mechanism targets inflammation, it can still contribute to CNS-related side effects such as dizziness, fatigue, headaches, or impaired concentration.
These effects are usually mild when meloxicam is taken alone. However, when combined with substances that do affect the CNS, the overall impact can become more pronounced.
The brain and nervous system do not experience drugs in isolation; they respond to the cumulative effect of everything in the body at that time.
For individuals already managing anxiety, depression, trauma-related symptoms, or substance use recovery, even subtle cognitive or balance changes can increase vulnerability.
A medication that slightly increases dizziness or slows reaction time may not seem significant—until it is combined with alcohol, cannabis, or sedating medications.
Why Drug and Alcohol Interactions Occur?
Drug interactions occur when substances influence each other’s absorption, metabolism, or effects on the body. These interactions can happen in several ways:
-
Additive effects, where two substances cause similar side effects that stack together
-
Synergistic effects, where one substance amplifies the impact of another
-
Metabolic interference, where one drug affects how another is processed by the liver or kidneys
With meloxicam, interactions often involve increased strain on organs or heightened risk of side effects rather than immediate intoxication[2]. This makes them easier to overlook. The danger is not always dramatic or immediate; it may develop quietly over time.
For people in behavioral health treatment or recovery, this slow escalation can be particularly risky. Subtle symptoms may be dismissed as anxiety, stress, or normal pain fluctuations, delaying medical attention until complications become severe.
Meloxicam and Alcohol Interactions
Alcohol is one of the most significant and commonly underestimated interaction risks with meloxicam. Both substances can irritate the gastrointestinal lining, and when combined, this effect becomes stronger. Over time—or sometimes suddenly—this irritation can lead to ulcers, internal bleeding, or perforation of the stomach or intestines.
Alcohol also affects judgment, coordination, and balance. When paired with meloxicam-related dizziness or fatigue, the risk of falls, injuries, and accidents increases.
This is especially concerning for older adults, people with chronic pain-related mobility issues, or individuals whose mental health symptoms already affect concentration or impulse control.
For individuals in recovery, alcohol use may also reawaken patterns of risk-taking or emotional distress. Even if alcohol use is occasional, combining it with medication can undermine stability and increase the likelihood of harm, both physically and psychologically.
Importantly, there is no universally “safe” amount of alcohol to consume with meloxicam. Risk varies based on dose, duration, individual health, and concurrent medications. When safety is the priority, avoidance is the most protective option.
Prescription Drug Interactions With Meloxicam

Meloxicam can interact with a wide range of prescription medications. These interactions do not mean the medications cannot be used together, but they do require careful monitoring and professional oversight.
High-risk categories include:
Opioid Pain Medications
While meloxicam is often prescribed to reduce reliance on opioids, some individuals may use both. Opioids can impair alertness and coordination, increasing accident risk when combined with meloxicam-related dizziness or fatigue.
This combination may also mask symptoms of internal bleeding, delaying recognition of serious complications.
Blood Thinners and Antiplatelet Medications
Meloxicam can increase bleeding risk by affecting platelet function and gastrointestinal integrity. When combined with medications that prevent blood clotting, the risk of serious bleeding events rises significantly. [3]
Corticosteroids
Steroids and NSAIDs both increase gastrointestinal risk. Together, they substantially raise the likelihood of ulcers and bleeding, particularly with long-term use.
Certain Antidepressants
Some antidepressants can affect platelet aggregation or increase bleeding tendencies. When combined with meloxicam, this may further elevate gastrointestinal or internal bleeding risk, even without obvious warning signs.
For individuals managing both physical pain and mental health conditions, coordination between providers is essential. No one should have to choose between pain relief and emotional stability.
Over-the-Counter Medication Interactions
Over-the-counter medications are often viewed as harmless, but they can pose real risks when combined with meloxicam.
-
Other NSAIDs: Many common pain relievers fall into the NSAID category. Taking them together can dramatically increase the risk of stomach ulcers, kidney damage, and cardiovascular complications.
-
Cold, Flu, and Allergy Medications: Some OTC products contain ingredients that cause drowsiness, dizziness, or increased blood pressure. When combined with meloxicam, these effects may intensify, particularly in older adults or those with anxiety-related sensitivity to physical symptoms.
-
Sleep Aids: OTC sleep medications often have sedating properties. Combined use can worsen daytime fatigue, confusion, and coordination issues, increasing accident risk.
OTC misuse is sometimes overlooked. People may self-medicate for sleep, anxiety, or pain without realizing the cumulative burden on their bodies.
Meloxicam and Recreational or Non-Prescribed Substances
Using meloxicam alongside recreational or illicit substances increases unpredictability and risk. Cannabis, for example, may amplify dizziness, impair judgment, or alter perception of pain. Opioids—whether prescribed or illicit—introduce significant safety concerns, particularly related to respiratory function and delayed recognition of bleeding or injury.
Illicit substances can also interfere with medication adherence and awareness. Someone under the influence may miss early warning signs, skip doses, or take additional substances impulsively.
For individuals in recovery, these combinations can be especially destabilizing. Even when meloxicam itself is not addictive, mixing substances can erode the structure and safety on which recovery depends.
Who Is at Higher Risk From Interactions?
Certain populations face increased vulnerability to meloxicam interactions:
-
Older adults: Age-related changes in metabolism, kidney function, and balance make side effects like dizziness, confusion, or GI bleeding more likely, raising fall and injury risk.
-
Polypharmacy (multiple medications): Taking several prescriptions, OTC products, or supplements can cause overlapping side effects—fatigue, nausea, or mental fog—that may escalate into serious complications if unchecked.
-
Kidney, liver, or GI conditions: These organs handle drug processing and are vulnerable to NSAID irritation; even standard doses can increase bleeding, toxicity, or organ strain.
-
History of substance use or recovery: Past substance use can alter tolerance and sensitivity. Alcohol, cannabis, or unprescribed medications may raise interaction risks, and side effects can act as psychological triggers, requiring recovery-informed care.
Recognizing higher risk is not about restriction—it is about protection. Tailoring care to individual circumstances supports dignity and safety.
Common Side Effects That May Worsen With Interactions
Meloxicam is generally well tolerated, but combining it with alcohol, other medications, or substances can make side effects stronger, longer-lasting, or more disruptive. [1]
-
Drowsiness and fatigue: Can intensify when combined with alcohol, sleep aids, or anxiety medications, affecting daily tasks and driving.
-
Dizziness and lightheadedness: May increase fall risk, especially in older adults or those with pain-related mobility issues.
-
Confusion or difficulty concentrating: Cognitive effects can interfere with decision-making and daily functioning, sometimes triggering distress in individuals in recovery.
-
Other symptoms: Nausea, headaches, stomach discomfort, or general unwellness may compound, impacting both physical and emotional well-being.
Recognizing that interactions can amplify side effects allows for early action. Sudden, persistent, or severe changes should prompt medical guidance to prevent complications.
Warning Signs of a Dangerous Interaction
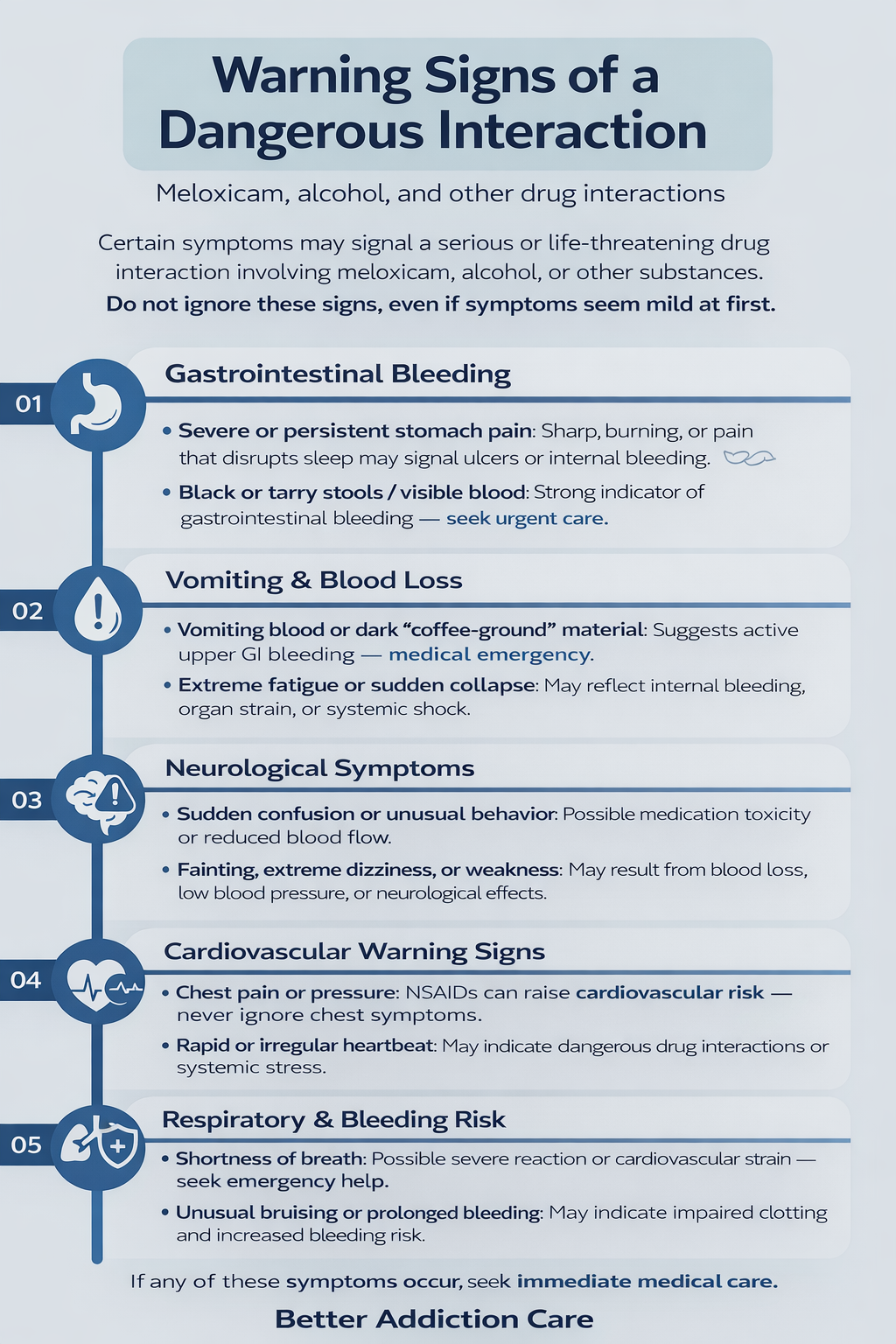
Certain symptoms may signal a serious or life-threatening interaction involving meloxicam, alcohol, or other substances. These signs should never be ignored, even if the medication has been taken before without problems or the symptoms seem mild at first. Early recognition and prompt medical care can prevent severe complications.
-
Severe or persistent stomach pain: May signal ulcers or internal bleeding; urgent evaluation needed if sharp, burning, or sleep-disrupting.
-
Black/tarry stools or visible blood: Could indicate gastrointestinal bleeding; seek immediate medical care.
-
Vomiting blood or dark “coffee-ground” material: Suggests active upper GI bleeding; treat as an emergency.
-
Sudden confusion or unusual behavior: May reflect medication toxicity or reduced blood flow; prompt assessment is important.
-
Fainting, extreme dizziness, or weakness: Could result from blood loss, low blood pressure, or neurological effects; urgent attention required.
-
Chest pain or pressure: NSAIDs may raise cardiovascular risk; never ignore chest symptoms.
-
Shortness of breath: May indicate serious reaction or cardiovascular strain; seek emergency help.
-
Rapid or irregular heartbeat: Could signal systemic stress or drug interactions; medical evaluation needed.
-
Unusual bruising or prolonged bleeding: May reflect impaired clotting and increased bleeding risk.
-
Extreme fatigue or sudden collapse: Could indicate severe interaction effects, internal bleeding, or organ strain; seek immediate care.
Safe Use and Risk-Reduction Guidelines
Using meloxicam safely is not just about following a prescription—it’s about understanding how daily choices, other medications, and substances can influence risk. These general precautions can help reduce the likelihood of harmful interactions while supporting long-term physical and emotional well-being.
-
Communicate openly with providers: Share all prescriptions, OTC products, supplements, and herbal remedies to prevent interactions.
-
Disclose alcohol and substance use: Honest reporting ensures safety-focused guidance, especially in recovery.
-
Avoid combining NSAIDs: Multiple anti-inflammatories raise risks of ulcers, bleeding, kidney, and heart issues.
-
Use caution with sedatives: Sleep aids, anxiety meds, and certain cold/allergy drugs may increase dizziness or fatigue.
-
Limit or avoid alcohol: Reduces GI bleeding risk and protects coordination and judgment.
-
Follow prescribed instructions: Overuse increases side effects; more is not safer.
-
Monitor for symptoms: Watch for stomach pain, dizziness, fatigue, confusion, or unusual bleeding.
-
Avoid self-medicating: OTC sleep aids or pain relievers can compound risks; non-medication strategies help.
-
Stay hydrated: Adequate fluids support kidney health and safer NSAID use.
-
Schedule regular check-ins: Ongoing monitoring allows dose adjustments and early side effect management.
-
Involve support systems: Family, caregivers, or sponsors can help monitor safety during stress or illness.
Safe use is not about restriction or fear—it’s about informed choice.
By prioritizing communication, awareness, and thoughtful decision-making, individuals can reduce interaction risks while preserving both physical health and recovery stability.
Meloxicam and Dependency or Misuse Considerations
-
Misuse potential often stems from pain and desperation, not intent.
Chronic pain can be physically exhausting and emotionally draining. When relief feels inconsistent, some individuals may take meloxicam more frequently or for longer periods than recommended, believing it will provide greater benefit. While this does not create addiction in the traditional sense, it can increase the risk of gastrointestinal bleeding, kidney damage, or cardiovascular strain.
-
Tolerance concerns can emerge over time.
Although meloxicam does not cause tolerance in the same way opioids do, people may perceive that it becomes “less effective” with long-term use. This perceived tolerance can lead to dose stacking, combining it with other pain relievers, or adding alcohol or sedating substances—behaviors that significantly increase interaction risk.
-
Psychological reliance can develop, especially during recovery.
For individuals in recovery from substance use, medications may take on emotional significance. A drug that reliably reduces pain may also become associated with comfort, control, or relief from stress. This psychological reliance does not mean failure in recovery, but it does warrant awareness and support to prevent unhealthy patterns from forming.
-
Risk increases when meloxicam is combined with other substances.
While meloxicam alone is not intoxicating, combining it with alcohol, cannabis, opioids, or non-prescribed medications can increase physical harm and blur boundaries that are important in recovery. These combinations may also mask early warning signs of relapse or medical complications.
-
Recovery-informed care emphasizes balance, not avoidance.
Using meloxicam safely does not mean rejecting pain treatment. It means integrating medication into a broader plan that may include physical therapy, behavioral pain management strategies, mental health support, and regular medical check-ins. When pain and emotional distress are both addressed, the risk of misuse decreases.
When to Speak With a Doctor or Specialist?
Professional guidance is essential in many situations involving meloxicam, especially when safety, recovery, or long-term health may be affected. Individuals should consider speaking with a doctor, pharmacist, or specialist in the following circumstances:
-
Multiple medications (polypharmacy): Taking several prescriptions, OTC drugs, or supplements can increase interaction risks. A provider can review your list for safety.
-
Alcohol, cannabis, or other substances: Even occasional use can affect meloxicam. Honest disclosure helps ensure safe guidance.
-
Chronic pain with mental health conditions: Depression, anxiety, or sleep issues can affect medication tolerance. Coordinated care helps balance relief and stability.
-
History of substance use or recovery: Medical and behavioral oversight reduces reliance risks and supports safe pain management.
-
Kidney, liver, stomach, or heart issues: These conditions can change how meloxicam is processed, raising complication risks.
-
New or worsening symptoms: Persistent stomach pain, dizziness, unusual bleeding, or fatigue should prompt evaluation.
-
Adding new medications or supplements: OTC drugs, sleep aids, or herbs can interact unexpectedly with meloxicam.
-
Inadequate pain control: Don’t increase doses without guidance; providers can suggest safer alternatives.
-
Uncertainty or concern: If something feels off, ask your provider early to prevent problems.
Speaking with a healthcare professional is not about restriction or blame—it is about informed care. Timely guidance helps individuals manage pain safely while protecting physical health, emotional well-being, and long-term recovery.
Final Takeaway
Meloxicam can offer meaningful relief from pain, but informed use is essential. Understanding interactions with alcohol, medications, and other substances empowers people to protect their health without fear.
With honest information, open communication, and realistic expectations, individuals and families can navigate pain management in a way that supports both physical well-being and long-term recovery.
FAQs
Alcohol increases bleeding and injury risk, even with occasional use. Combining alcohol with meloxicam can also worsen dizziness, fatigue, and stomach irritation. For individuals in recovery, even small amounts may trigger relapse-related thoughts or behaviors. Avoiding alcohol while on this medication is the safest option.
Some combinations require monitoring. Always consult a provider before taking meloxicam alongside antidepressants, anxiety medications, or sleep aids. Interactions may increase bleeding risk, dizziness, or cognitive side effects. A healthcare professional can help safely coordinate both physical and mental health treatment.
It can be used safely, but oversight helps prevent unintended risks. Medication management should be integrated into a broader recovery plan that addresses pain, emotional well-being, and relapse prevention. Open communication with providers and support networks ensures meloxicam supports recovery rather than complicating it.
Many OTC medications, including other NSAIDs, cold, flu, and allergy products, can interact with meloxicam. Even common remedies may increase bleeding risk, kidney strain, or dizziness. Always check labels and consult a healthcare provider before combining medications.
Any new or worsening symptoms—such as stomach pain, unusual bleeding, dizziness, or confusion—should be reported immediately. Early recognition and professional guidance can prevent minor issues from becoming serious. Never ignore changes or assume they are “normal” side effects.







