Meloxicam Withdrawal: Quitting Mobic Abruptly
When someone stops meloxicam suddenly—especially after long-term use—the body may react. It’s not withdrawal in the addictive sense, because meloxicam doesn’t change brain reward pathways or create cravings.

Key Takeaways
-
Is withdrawal real? → Meloxicam doesn’t cause traditional “withdrawal,” but stopping abruptly can trigger rebound inflammation and discomfort that feels like withdrawal.
-
How should I stop safely? → Gradual reduction, medical guidance, and pain-management planning make the transition much smoother.
-
What helps recovery? → Gentle movement, anti-inflammatory nutrition, stress regulation, and supportive routines help the body recalibrate.
What Happens When You Stop Taking Meloxicam (Mobic)?
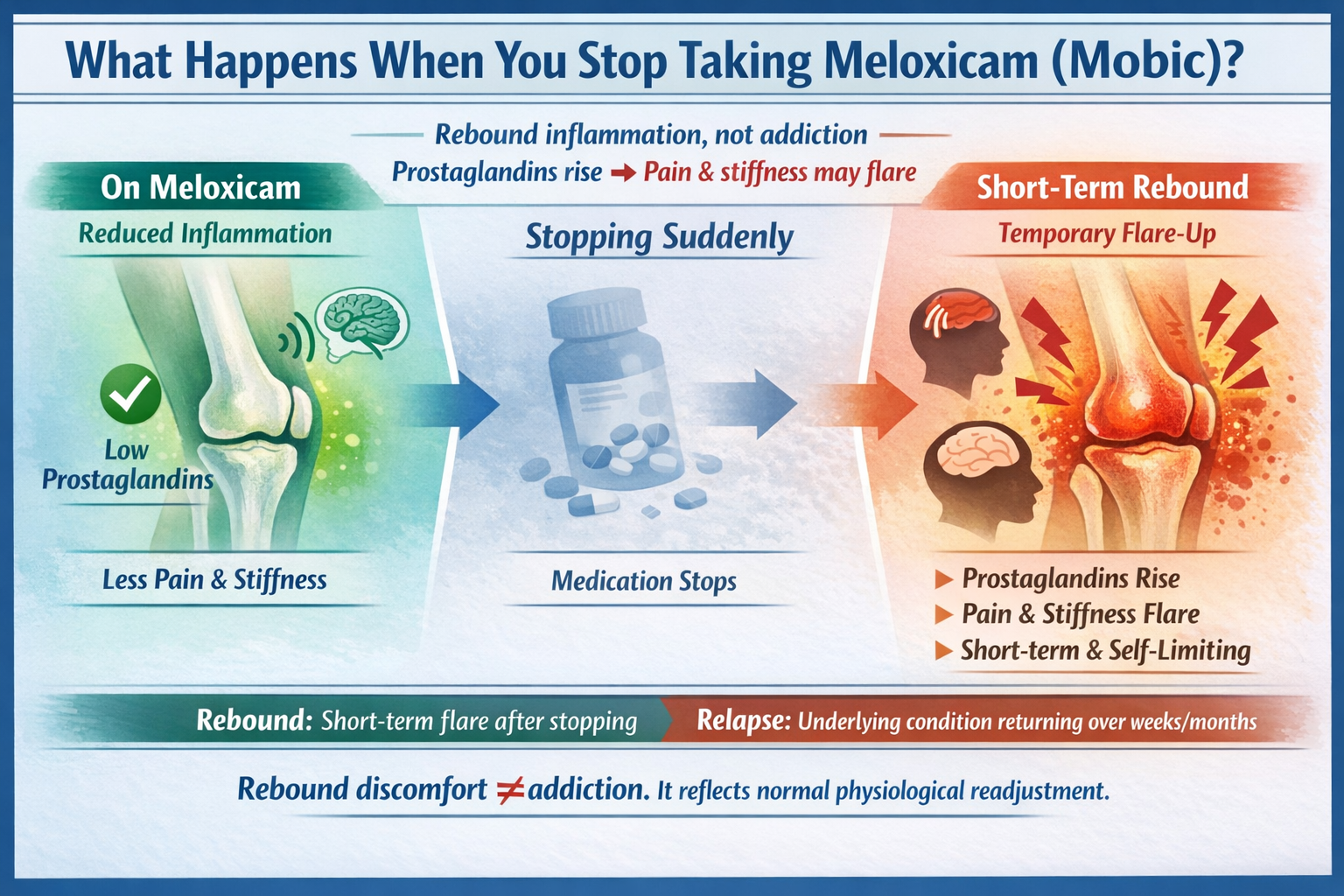
Meloxicam (brand name Mobic) is a nonsteroidal anti-inflammatory drug (NSAID) used to relieve pain, swelling, and stiffness. [1] It works by reducing inflammatory chemicals called prostaglandins.
When someone stops meloxicam suddenly—especially after long-term use—the body may react. It’s not withdrawal in the addictive sense, because meloxicam doesn’t change brain reward pathways or create cravings.
Instead, the body experiences physiological readjustment, including:
-
Inflammation is returning faster than expected
-
pain flaring as prostaglandins rise again
-
stiffness, swelling, or headaches
-
a sense that symptoms rush back.
This is called rebound inflammation, and it’s temporary.
It’s also important to distinguish rebound symptoms from a relapse of the original condition.
-
Relapse = the underlying arthritis or pain disorder returning over weeks to months
-
Rebound = a short-term flare triggered by stopping the medication
Understanding this difference helps families stay grounded and prevents unnecessary fear.
Most importantly:
Rebound discomfort ≠ addiction.
It simply reflects the body recalibrating after losing anti-inflammatory support.
What Are the Common Symptoms of Meloxicam Withdrawal?
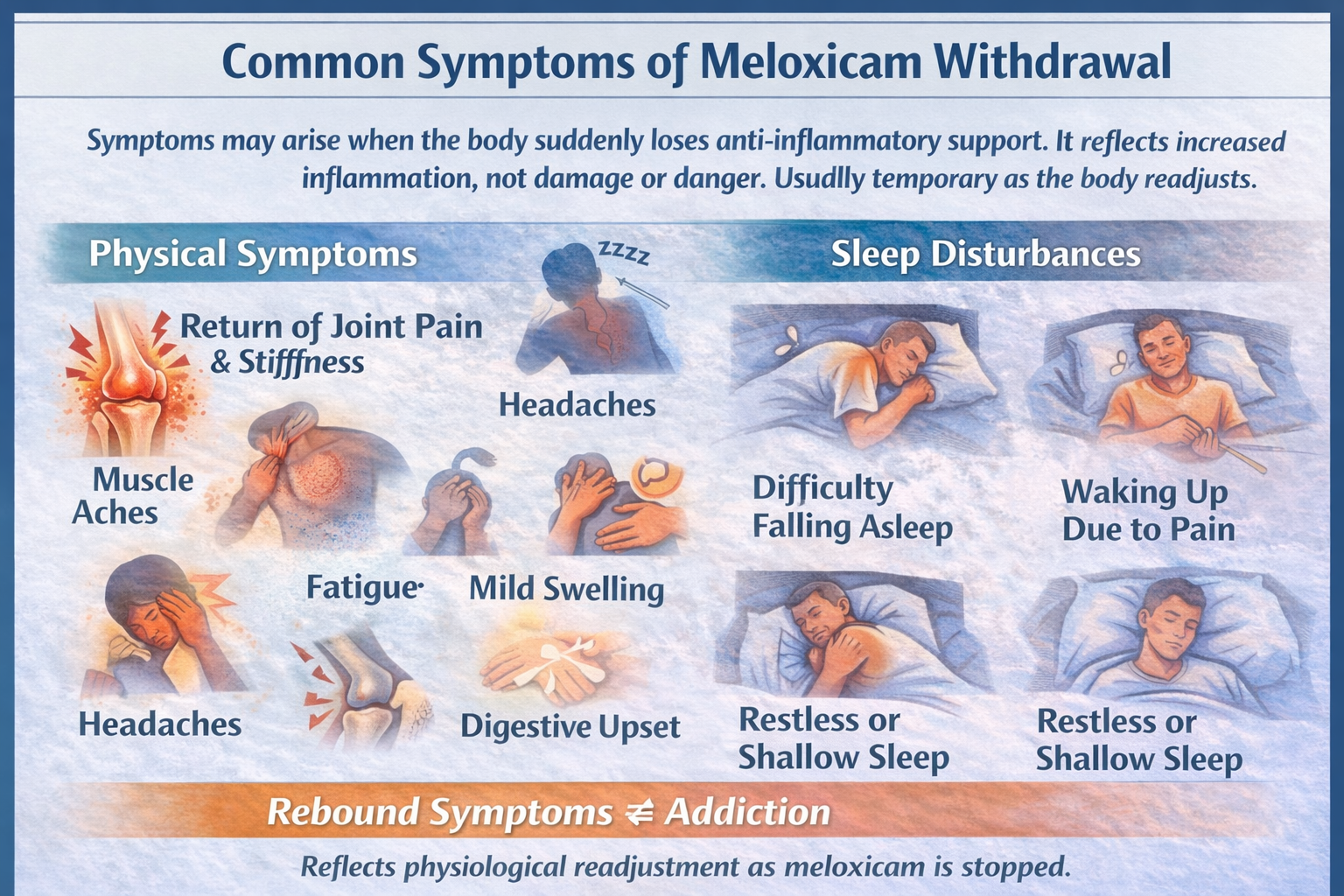
Physical Symptoms
Even though meloxicam doesn’t create classic withdrawal, many people feel uncomfortable when they stop abruptly because the body suddenly loses anti-inflammatory support. This abrupt change can make the return of symptoms feel sharper or more overwhelming than expected. Common physical symptoms include:
-
Return of joint pain or stiffness: When meloxicam is removed, prostaglandin levels rise again, triggering inflammation. [2] The joints that once felt manageable may suddenly ache, stiffen, or feel “heavier,” especially in the morning or after periods of inactivity.
-
Muscle aches: Inflammation doesn’t only affect joints—it can cause surrounding muscles to tighten and work harder to compensate. This leads to soreness or a “deep tissue ache” that feels similar to flu-like heaviness.
-
Headaches: Prostaglandin changes can create vascular shifts, leading to tension or throbbing headaches. These may feel more noticeable during the first week after stopping.
-
Fatigue: When the body is dealing with inflammation and disrupted sleep, energy levels dip. Fatigue is not a sign of something going wrong—it’s the body working harder to regain balance.
-
Mild swelling: Some people notice puffiness in the hands, knees, or feet as inflammation resurges. This swelling usually decreases as the body adjusts.
-
Digestive upset (nausea, bloating): NSAIDs influence the stomach lining and digestive enzymes. When stopped abruptly, the digestive system recalibrates, which may temporarily cause bloating, queasiness, or mild cramps.
These symptoms reflect an increase in inflammation—not damage or danger. They’re common, usually short-lived, and manageable with proper care such as gentle movement, heat/cold therapy, hydration, and anti-inflammatory nutrition.
Sleep Disturbances
Sleep is often one of the first things affected when someone stops taking meloxicam suddenly. Pain tends to surface more at night when the body is still, making discomfort harder to ignore. Some people experience:
-
Difficulty falling asleep: Flare-ups of stiffness or joint throbbing make it hard to settle into a comfortable position. The more someone focuses on the pain, the more alert and unsettled the brain becomes.
-
Waking up due to pain: Many individuals describe sleep that is repeatedly interrupted—waking up when rolling over, stretching out, or trying to shift positions. This “broken sleep” contributes to daytime fatigue.
-
Restless or shallow sleep: Even if one stays asleep, the brain may not fall into deeper sleep stages because the body is monitoring discomfort. People often say, “I slept, but I don’t feel rested.”
As inflammation settles and the nervous system adjusts—typically within 1–2 weeks—sleep becomes deeper, more consistent, and less disrupted by physical discomfort. Supportive sleep routines can speed this transition.
Emotional and Mental Health Symptoms
Pain and inflammation don’t just affect the body—they influence mood, patience, motivation, and resilience. The emotional impact can feel just as distressing as the physical symptoms. Some individuals report:
-
Irritability: When even small movements hurt or tasks take more effort, frustration builds quickly. This irritability isn’t “you being difficult”—it’s a natural response to discomfort.
-
Low mood: Persistent pain affects neurotransmitters tied to motivation and emotional stability. People may feel discouraged, sad, or mentally drained, especially if they expected a smoother transition off the medication.
-
Frustration: Many individuals worry, “Why does my body feel like it’s going backward?” This frustration can be heightened when flare-ups disrupt responsibilities or routines.
-
Anxiety about “pain coming back forever”: It’s common to fear that the rebound pain reflects permanent worsening. In reality, rebound inflammation is temporary and usually improves with supportive care and time.
These emotional responses are valid and human, not a sign of weakness or relapse. They often fade once the pain stabilizes and the individual regains a sense of control and predictability in their daily routine.
Sensory or Neurological Symptoms
While less common, some people experience sensory or nervous-system-related symptoms when stopping meloxicam abruptly. [3] This happens because the pain pathways that were “quieted” by the medication suddenly reactivate. Symptoms can include:
-
Heightened sensitivity to pain: The nervous system may temporarily overreact to normal aches, interpreting them as more intense than they are. This sensitivity often peaks during the first week.
-
Restlessness: Discomfort can make it hard to stay still. Some describe feeling jittery, tense, or unable to “get comfortable” in any position.
-
Tension headaches: These are often caused by a combination of muscle tightening, stress, and inflammatory changes. They may radiate from the neck to the temples.
-
A sense of being “on edge”: When the body experiences both discomfort and uncertainty, the stress response activates. This “wired but tired” feeling is temporary and usually improves as the nervous system recalibrates.
These symptoms are not signs of neurological decline—they’re simply the nervous system adjusting to a new internal environment. As inflammation decreases and routines stabilize, the body naturally settles.
What Is the Typical Meloxicam Withdrawal Timeline?
Although experiences vary, most people follow a similar pattern:
Note: Timelines shift based on dosage, how long you’ve been taking meloxicam, your underlying condition, and whether you tapered or quit abruptly.
Why Should Meloxicam Be Tapered Slowly?
Even though meloxicam is not addictive and doesn’t cause classic withdrawal, the body becomes accustomed to its anti-inflammatory support—especially when someone has been taking it daily for months or years.
Stopping suddenly can feel like the rug has been pulled out from under the body’s carefully balanced pain and inflammatory systems.
When meloxicam is discontinued abruptly, several challenges can arise:
-
Sudden return of pain: The prostaglandin-blocking effect of meloxicam disappears quickly, and the body may react with an abrupt surge of inflammation. Pain that had been controlled may come back more sharply than expected, creating the sense that symptoms are “rebounding.”
-
Intense inflammation: Without gradual adjustment, inflammatory pathways become more active almost overnight. This can lead to swollen joints, stiffness, headaches, or muscle aches that feel disproportionate to your usual symptoms.
-
Disrupted sleep: Pain flares often strike hardest at night, making it difficult to fall asleep or stay asleep. The exhaustion that follows can make pain feel even worse, creating a difficult cycle.
-
Emotional overwhelm: When pain intensifies suddenly, it’s natural to feel frustrated, scared, or discouraged. People may worry that their underlying condition has suddenly worsened or that they will “never be able to function without meloxicam.” These emotions are completely valid—and they often reflect the abrupt change, not the long-term outlook.
A slow, thoughtful taper helps avoid these sudden spikes and gives the body time to recalibrate. Gradual reduction allows the system to adjust to lower doses step by step, making the process far more manageable.
A careful taper allows:
-
The body adapts gradually: As the dose decreases, the body learns to regulate inflammation more naturally, rediscovering balance without shock or overload.
-
Inflammatory pathways to stabilize: The immune system adjusts its production of prostaglandins more smoothly, reducing the likelihood of painful flare-ups.
-
Fewer and milder flare-ups: People often report that a slower taper feels smoother, more predictable, and easier on both body and mind.
-
Better long-term comfort: Slow reduction supports sustainable recovery. Instead of battling intense symptoms for weeks, the body transitions in a controlled and supportive environment.
Key principle:
“Go slow to stay steady.”
Rushing the process rarely helps. A gradual taper respects the body’s pace and reduces unnecessary suffering.
Ultimately, let your doctor set the pace—not the calendar. Your body’s comfort, stability, and long-term function matter more than finishing the taper quickly.
What Helps Manage Meloxicam Withdrawal Symptoms?
Healthcare providers can support withdrawal by:
-
Monitoring pain levels and inflammatory symptoms
-
Adjusting taper speed if discomfort spikes
-
Distinguishing rebound inflammation from relapse
-
Recommending temporary alternatives (acetaminophen, topical NSAIDs, heat/ice therapy)
-
Guiding safe use of supplements if appropriate
-
Helping stabilize mood and sleep during the adjustment phase
Their goal is not just physical safety—it’s emotional reassurance, helping you feel supported through each step.
What Coping Strategies Help Manage Withdrawal Symptoms?

1. How Can I Improve My Sleep?
Sleep becomes harder when pain flares, but small, consistent habits can create a sense of comfort and predictability. These strategies help calm the body before bedtime and reduce nighttime awakenings:
-
Use a warm shower or heating pad before bed: Heat relaxes tense muscles, eases joint stiffness, and signals safety to the nervous system. Many people find that 10–15 minutes of warmth reduces the “settling in” pain that often delays sleep.
-
Try a supportive pillow or mattress adjustments: Even minor changes—adding a knee pillow, adjusting your sleep position, or using a firmer or softer surface—can reduce pressure on sensitive joints. The goal is to make your body feel supported, not strained.
-
Practice calming routines (breathing, gentle stretching): Slow breathing, meditation tracks, or light stretching tell your brain it’s time to unwind. This helps quiet the fight-or-flight response that often kicks in when pain is present.
-
Keep a consistent bedtime to reset your circadian rhythm: Going to bed and waking up at the same time—even on weekends—helps normalize sleep patterns disrupted by pain. Consistency builds momentum, even if sleep quality is imperfect at first.
Sleep disturbances during meloxicam withdrawal are temporary. As inflammation stabilizes, the body naturally returns to more restorative sleep.
2. What Should I Eat and Drink During Withdrawal?
Food becomes especially important when the body is adjusting to life without meloxicam. You’re not trying to “cancel” inflammation overnight—you’re creating an environment where the body can heal and self-regulate more smoothly.
Anti-inflammatory nutrition can soften rebound symptoms:
-
Omega-3-rich foods (salmon, walnuts, chia seeds): Omega-3s help calm inflammatory pathways and support joint mobility. [4]
-
Leafy greens, berries, turmeric, and ginger: These foods contain antioxidants that reduce oxidative stress and support overall recovery.
-
Adequate hydration: Water helps flush metabolic waste, supports joint lubrication, and reduces fatigue. Mild dehydration often makes pain feel worse.
-
Limit sugar, processed foods, and excess caffeine: These can spike inflammation, worsen energy crashes, and disrupt sleep.
While food alone won’t “cure” symptoms, it strengthens the body’s healing foundation, helping you feel more in control during the transition.
3. Should I Exercise?
Yes—gentle, consistent movement is one of the most helpful tools during meloxicam withdrawal. You don’t need intense workouts; you need low-impact movement that supports circulation, reduces stiffness, and improves overall mood.
Try:
-
Walking: Even 10–15 minutes can ease joint stiffness, boost endorphins, and lighten emotional strain.
-
Light stretching: Helps maintain flexibility and reduces tension in muscles, compensating for inflammation.
-
Yoga: Encourages breath control, relaxation, and gentle strengthening without overload.
-
Water exercises: Warm water takes pressure off joints and allows smoother, pain-free movement.
Movement reduces stiffness and supports emotional well-being without overwhelming the joints. The goal is consistency over intensity—listening to your body each day.
4. How Can I Reduce Stress and Anxiety?
Pain is not just a physical sensation—it affects the mind and the nervous system. When you’re in pain, stress hormones rise, making discomfort feel sharper and more overwhelming. Supporting your emotional health is just as important as any physical strategy.
Helpful approaches include:
-
Deep breathing exercises: Slow breathing lowers the body’s stress response and helps calm the nervous system.
-
Short mindfulness sessions: Even 3–5 minutes can reduce tension and help you reconnect with your body without panic.
-
Warm baths: Warmth relaxes muscles, softens joint tension, and lowers cortisol levels.
-
Journaling: Writing helps externalize fears and frustration instead of carrying them internally.
-
Talking through fears with a trusted person: Emotional connection reduces the sense of isolation and amplifies resilience during recovery.
When the mind feels less overwhelmed, the body often experiences pain as more manageable. Emotional care is not optional—it’s part of healing.
5. How Can I Stay Connected and Supported?
Withdrawal—physical or emotional—is harder when you feel alone. Social support acts as a buffer against stress and helps regulate the nervous system. Sharing what you’re experiencing often reduces fear and frustration.
Try:
-
Talking to family about what you’re experiencing: Let them know what symptoms feel like and what kind of support helps (e.g., patience, help with chores, or simply listening).
-
Connecting with others who’ve discontinued NSAIDs: Hearing that others have gone through it and improved can bring tremendous relief.
-
Involving your partner or support person in pain-management planning: A second set of eyes and ears can help you stay grounded if symptoms feel overwhelming.
You do not need to navigate discomfort alone. Support makes the transition more manageable and emotionally balanced.
6. Does Routine Matter?
Absolutely. Predictable routines act like an anchor for both your body and mind. When you’re going through discomfort, uncertainty amplifies stress. Structure restores a sense of safety and stability.
Routines help stabilize:
-
Sleep: Consistent wake and sleep times help regulate disrupted circadian rhythms.
-
Mood: Predictability reduces anxiety and improves emotional resilience.
-
Activity levels: Scheduled light exercise prevents inactivity-related stiffness and fatigue.
-
Pain perception: A routine helps the nervous system stay calmer, making sensations feel less intense.
Structure doesn’t eliminate symptoms, but it creates a supportive environment that makes them easier to handle. Small routines build big confidence over time.
When Should I Seek Medical Help During Withdrawal?
Reach out to a healthcare provider if you experience:
-
severe pain that interferes with mobility
-
swelling, redness, or warmth in joints
-
persistent insomnia
-
signs of gastrointestinal bleeding (dark stools, vomiting blood)
-
dizziness or fainting
-
Symptoms that worsen instead of improve
Medical guidance ensures safety—and often relieves fear by clarifying what is normal.
What Comes After Withdrawal? (Long-Term Recovery)
After meloxicam is tapered, many people rediscover:
-
more stable energy
-
clearer sleep patterns
-
improved emotional grounding
-
healthier long-term pain-management strategies
Recovery continues long after the last pill.
It’s a process of building habits that support the body naturally:
-
physical therapy
-
gentle exercise plans
-
anti-inflammatory nutrition
-
consistent routines
-
checking in with a provider regularly
Healing is gradual but absolutely possible—and you don’t have to rush it.
Conclusion
Meloxicam withdrawal isn’t a sign of addiction or failure—it’s simply your body readjusting. With a slow taper, medical support, and healthy daily habits, discomfort eases and stability returns.
If you stay patient, stay supported, and avoid quitting abruptly, the transition can be manageable and empowering.
Your body is capable of recalibration—and you don’t have to walk through it alone.
FAQs
You can, but many people experience discomfort. A gradual taper is safer and more comfortable.
Most rebound symptoms improve within 2–4 weeks.
For many, rebound pain fades. Long-term pain depends on your underlying condition—not the withdrawal process itself.
Heat, gentle exercise, anti-inflammatory foods, hydration, and stress-management practices.
By offering understanding, helping with routines, and validating the emotional difficulty of transitioning off a medication.
Contact your healthcare provider. A slower taper or alternative treatments can make a dramatic difference.
Resources
Related Articles
Treatment Centers in Virginia










