Methocarbamol Addiction: Signs, Symptoms, Withdrawal, and Treatment
Methocarbamol is a muscle relaxant prescribed to treat muscle pain and spasms. Methocarbamol addiction develops when individuals misuse the drug, taking it in higher doses or using it for longer than prescribed. This leads to physical and psychological dependence, where the user craves its sedative effects, leading to compulsive use. Methocarbamol is not classified as an opioid even though it has a risk of psychological dependency.
Methocarbamol is a muscle relaxant prescribed to treat muscle pain and spasms. Methocarbamol addiction develops when individuals misuse the drug, taking it in higher doses or using it for longer than prescribed. This leads to physical and psychological dependence, where the user craves its sedative effects, leading to compulsive use. Methocarbamol is not classified as an opioid even though it has a risk of psychological dependency.
Methocarbamol abuse has become more prevalent increasing three fold in long-term usage between 2005 and 2016. While new prescriptions remained stable at around 6 million annually, office visits for ongoing therapy jumped from 8.5 million to 24.7 million. Notably, older adults made up 22.2% of these visits in 2016, surpassing their 14.5% representation in the population according to Penn Medicine, in "Long-term Use of Muscle Relaxants Has Skyrocketed Since 2005". Methocarbamol is not classified as a controlled substance by the U.S. Drug Enforcement Administration (DEA). Although it has a low potential for abuse and addiction, its use carries risks, particularly for individuals with a history of substance use disorders.
Signs of methocarbamol addiction include noticeable behavioral changes. People who are addicted to methocarbamol begin taking larger doses than prescribed and engage in "doctor shopping" to acquire additional prescriptions. They withdraw from social activities, neglect personal and professional responsibilities, and take risks to obtain the drug. Increased tolerance is a key sign, as users require higher doses to achieve the same effects.
Methocarbamol addiction leads to a range of physical and psychological symptoms. Physically, users experience drowsiness, dizziness, and confusion due to the drug’s sedative properties. Long-term use results in cognitive impairment, memory issues, and impaired motor coordination. Psychologically, individuals experience cravings, anxiety, depression, and an inability to stop using methocarbamol despite its harmful impact on their lives. Combining methocarbamol with other substances is dangerous. Nearly half of users experience side effects from muscle relaxants, primarily dizziness and sedation according to Daniel J. Mazanec and Russell C. DeMicco’s 2017 Benzel’s Spine Surgery, 2-Volume Set.
Withdrawal from methocarbamol results in symptoms such as anxiety, insomnia, muscle aches, nausea, irritability, and heightened sensitivity to pain. The body experiences these reactions as it adjusts to functioning without the drug. Users also experience headaches, tremors, and restlessness during the withdrawal process.
Treatment for methocarbamol addiction requires a structured approach, beginning with medically supervised detox to manage withdrawal symptoms safely. After detox, behavioral therapies like cognitive-behavioral therapy (CBT) address the underlying reasons for addiction and provide strategies for relapse prevention. Depending on the severity of the addiction, inpatient or outpatient rehabilitation programs offer comprehensive support for long-term recovery.
What is Methocarbamol Addiction?
Methocarbamol addiction is the compulsive use of methocarbamol (Robaxin), a medication classified as a skeletal muscle relaxant. This drug is typically prescribed to alleviate muscle pain and spasms, but when used inappropriately—such as in higher doses or for prolonged periods—it leads to psychological dependence. Methocarbamol is not classified as a controlled substance by the U.S. Drug Enforcement Administration (DEA), and it is considered to have a lower potential for abuse compared to other muscle relaxants, opioids, or benzodiazepines. Individuals with a history of substance use disorders are more prone to misusing methocarbamol due to its sedative properties.
Methocarbamol has a low risk for physical dependence but psychological addiction is possible when the drug is taken beyond its prescribed purpose. Misuse arises from attempting to intensify its sedative effects or combining it with other substances, such as alcohol, which is dangerous. While skeletal muscle relaxants are used less often than medications like pain relievers, they remain a significant concern in the U.S. In 2011, an estimated 53,000 emergency department visits were attributed to the misuse or abuse of muscle relaxants, with 18% involving alcohol, according to Witenko et al.'s 2014 study, “Considerations for the Appropriate Use of Skeletal Muscle Relaxants for the Management of Acute Low Back Pain” . The study also revealed that 44.5% of individuals used muscle relaxants for over a year, despite recommendations for short-term use only.
The misuse of methocarbamol leads to increased tolerance, cravings, and a growing inability to control intake. Over time, this addiction disrupts daily functioning and presents serious health risks, making it important to recognize and address methocarbamol misuse before it escalates into severe dependency.
What is Methocarbamol?
Methocarbamol, a centrally acting muscle relaxant, is typically used to relieve muscle pain and discomfort associated with acute musculoskeletal conditions. It works by depressing the central nervous system (CNS), which helps reduce muscle spasms without directly affecting the muscles themselves.
The usual initial dosage for adults is 1500 mg, taken three to four times daily. The initial dosage is achieved by taking two 750 mg tablets per dose. For severe conditions, the dosage is increased up to 7500 mg per day, but the dose is generally reduced after the first 48 to 72 hours of treatment to maintain around 4000-4500 mg per day according to “Methocarbamol (Oral Route)” published by the Mayo Clinic. It's important to follow a healthcare provider’s instructions for proper use
What Are the Signs, Symptoms, and Side Effects of Methocarbamol?
The signs, symptoms and side effects of methocarbamol are neurological, gastrointestinal, respiratory, musculoskeletal and severe allergic reactions. These effects become more severe depending on the dosage or severity of the misuse.

The signs, symptoms and side effects of methocarbamol are detailed below:
- Drowsiness: Drowsiness is a neurological side effect resulting from methocarbamol’s CNS depressant action, which slows brain activity. This reduction in brain function causes users to feel unusually sleepy or lethargic, especially at higher doses. The sedative nature of methocarbamol, while helpful for relaxing muscles, impairs daytime alertness and productivity.
- Dizziness and Balance impairment: Dizziness and balance impairment is a neurological side effect that occurs when methocarbamol affects the brain's balance centers, causing a feeling of unsteadiness or spinning. Methocarbamol slows neural activity, impacting balance and coordination. Dizziness also arises during withdrawal as the brain readjusts to normal functioning without the drug. Methocarbamol’s sedative effects can impair balance and hinder the safe operation of vehicles and machinery, particularly in older adults who are more vulnerable to these side effects according to a 2004 study by Charles Dillon et al., titled “Skeletal Muscle Relaxant Use in the United States,”
- Lightheadedness: Lightheadedness is a neurological symptom characterized by a faint or dizzy sensation, due to methocarbamol’s impact on blood circulation and blood pressure regulation. As the drug slows CNS activity, it affects cardiovascular responses, leading to a temporary reduction in blood flow to the brain.
- Blurred Vision: Blurred vision is a neurological side effect caused by methocarbamol’s influence on the brain’s visual processing centers. By depressing the CNS, the drug interferes with how the brain interprets visual information, leading to difficulty focusing on objects or experiencing blurred images.
- Double Vision: Double visions is a neurological side effect where methocarbamol impairs the coordination of the eyes. Methocarbamol disrupts the normal control of eye muscles, making it difficult to focus properly, resulting in seeing double images.
- Mood or Mental Changes: Mood or mental changes are psychological symptoms caused by methocarbamol’s influence on neurotransmitter balance in the brain. These changes include mood swings, irritability, or confusion, as the drug alters normal brain chemistry, particularly in long-term users or during withdrawal.
- Headaches: Headaches are neurological symptoms and physical side effects that occur both during methocarbamol use and withdrawal. The drug’s impact on the CNS and vascular system causes tension or pressure in the head, especially when the body is adjusting to the absence of methocarbamol.
- Feeling of Constant Movement (Vertigo): Vertigo is a neurological symptom where methocarbamol interferes with the vestibular system, causing users to feel as though they are moving even when stationary. This sensation is linked to the drug’s depressive effects on brain regions controlling balance and spatial orientation.
- Seizures: Seizures are a severe neurological side effect that requires immediate attention. Seizures have been documented in individuals with a history of epilepsy after receiving intravenous methocarbamol. Additionally, seizures have been reported in cases involving polysubstance toxicity, indicating a heightened risk in such situations according to a November 2022 study in the StatPearls titled “Methocarbamol.”
- Stomach Upset: Stomach upset is a gastrointestinal side effect that results from methocarbamol irritating the stomach lining. The drug's impact on the digestive system, particularly when taken on an empty stomach, leads to discomfort or mild pain in the abdomen.
- Nausea: Nausea is a gastrointestinal symptom and side effect of methocarbamol, occurring when the drug disrupts the normal functioning of the stomach and intestines. Nausea is also common during withdrawal, as the body reacts to the absence of the drug.
- Vomiting: Vomiting is a severe gastrointestinal symptom that occurs after methocarbamol use, especially at high doses. Methocarbamol affects the brain’s vomiting center, and vomiting also happens during withdrawal as the body detoxifies.
- Heartburn: Heartburn is a gastrointestinal side effect where methocarbamol relaxes the muscles in the digestive tract, allowing stomach acid to flow back into the esophagus, causing burning pain or discomfort.
- Indigestion: Indigestion is a gastrointestinal side effect resulting from methocarbamol’s relaxing effect on the digestive system. Slowed digestion leads to feelings of fullness, bloating, and discomfort.
- Diarrhea: Diarrhea is a gastrointestinal side effect that occurs when methocarbamol disrupts normal bowel movements, during withdrawal, when the digestive system becomes unbalanced as it adjusts to the absence of the drug.
- Metallic Taste in Mouth: Metallic taste in mouth is a general side effect that occurs as methocarbamol interacts with saliva and digestive enzymes, creating a metallic or unpleasant taste. This taste lingers during and after methocarbamol use.
- Difficulty Swallowing: Difficulty swallowing is a gastrointestinal symptom caused by methocarbamol’s muscle-relaxing properties. Methocarbamol affects the muscles involved in swallowing, making it difficult for some users to properly consume food or liquid.
- Fast Heartbeat (Tachycardia): Tachycardia is a cardiovascular side effect where methocarbamol accelerates heart rate due to its influence on the CNS and the body’s autonomic functions. This increased heart rate occurs as the body compensates for the drug’s sedative effects.
- Chest Tightness: Chest tightness is a cardiovascular symptom where methocarbamol affects the muscles around the chest, leading to discomfort or a feeling of constriction. It is caused by the drug’s impact on the central nervous system’s regulation of muscle function.
- Feeling of Warmth: Feeling of warmth is a cardiovascular side effect caused by methocarbamol’s vasodilatory effects, where blood vessels widen, increasing blood flow and causing a sensation of warmth or flushing.
- Swelling (Edema): Swelling is a cardiovascular side effect that occurs due to fluid retention, particularly in the extremities. Methocarbamol’s influence on blood circulation causes excess fluid to accumulate, leading to swelling.
- Difficulty Breathing: Difficulty breathing is a severe respiratory symptom that occurs when methocarbamol depresses the respiratory centers in the brain. This effect is particularly dangerous when methocarbamol is combined with other CNS depressants, leading to shallow or slow breathing.
- Fever: Fever is a general symptom that occurs during methocarbamol withdrawal. As the body detoxifies from the drug, it responds with a mild fever, as part of the immune response to the changes in the body’s homeostasis.
- Joint or Muscle Pain: Muscle pain is a musculoskeletal symptom that arises during methocarbamol withdrawal. Though the drug is intended to relieve muscle spasms, its absence causes the body to experience pain or discomfort, particularly during the detox process.
- Urine discoloration: Urine Discoloration is a general side effect of methocarbamol use, where individuals notice their urine turning black, blue, or green. This is mentioned in a MedlinePlus study on “Methocarbamol,” in August 2017. The change in urine color occurs as the body processes and eliminates the medication, and while unusual, it is generally not harmful.
- Angioneurotic Edema: Angioneurotic Edema is a severe allergic reaction to methocarbamol where the deeper layers of the skin swell, particularly around the face and throat. This side effect requires immediate medical attention as it is life-threatening.
- Overdose Symptoms: Overdose is a severe side effect that includes extreme drowsiness, confusion, slow breathing, and loss of consciousness. Overdose occurs when methocarbamol is taken in excessive amounts, leading to respiratory depression and the need for emergency medical intervention. A retrospective study analyzing data from the National Poison Data System between 2010 and 2020 identified 2,605 cases of single-agent exposures to skeletal muscle relaxants, including methocarbamol, in patients aged 6 to 19. Of these cases, 75.74% were intentional exposures, with over half of them being suicide attempts. Additionally, 81.04% of these incidents resulted in referral to or management at healthcare facilities, highlighting the serious nature of muscle relaxant misuse in this age group according to Sibrack, J. “Methocarbamol” published by Stat Pearls.
- Fatal Overdose: Fatal overdose is a severe side effect that results from combining methocarbamol with other CNS depressants, such as alcohol or opioids. The drug’s depressive effects on the brain cause respiratory failure, leading to death if not treated promptly. Methocarbamol enhances the effects of other CNS depressants like alcohol, barbiturates, anesthetics, and appetite suppressants, increasing the risk of severe side effects, including respiratory depression and potentially fatal outcomes. It also intensifies the effects of anticholinergics and psychotropic drugs, while reducing the effectiveness of pyridostigmine bromide, used to treat myasthenia gravis. Due to these risks, especially the potential for dangerous interactions, methocarbamol should be used with caution according to “Robaxin-750, 750 mg Film-coated Tablets” published by Medicines.org.
When Does Methocarbamol Consumption Cause Addiction?
Methocarbamol consumption causes addiction when it is misused. Misuse occurs when individuals take the medication in higher doses or for longer periods than prescribed, seeking its sedative effects. The risk of addiction significantly increases when methocarbamol is combined with other central nervous system (CNS) depressants such as alcohol, opioids, or benzodiazepines. These combinations enhance the drug’s depressant effects, increasing the likelihood of dependence. Regular misuse of methocarbamol, particularly over several weeks, increases the likelihood of developing dependence. While there is no exact timeline for addiction, prolonged misuse—especially when methocarbamol is used in excessive amounts beyond the recommended 6 to 8 grams per day—raises the risk significantly.
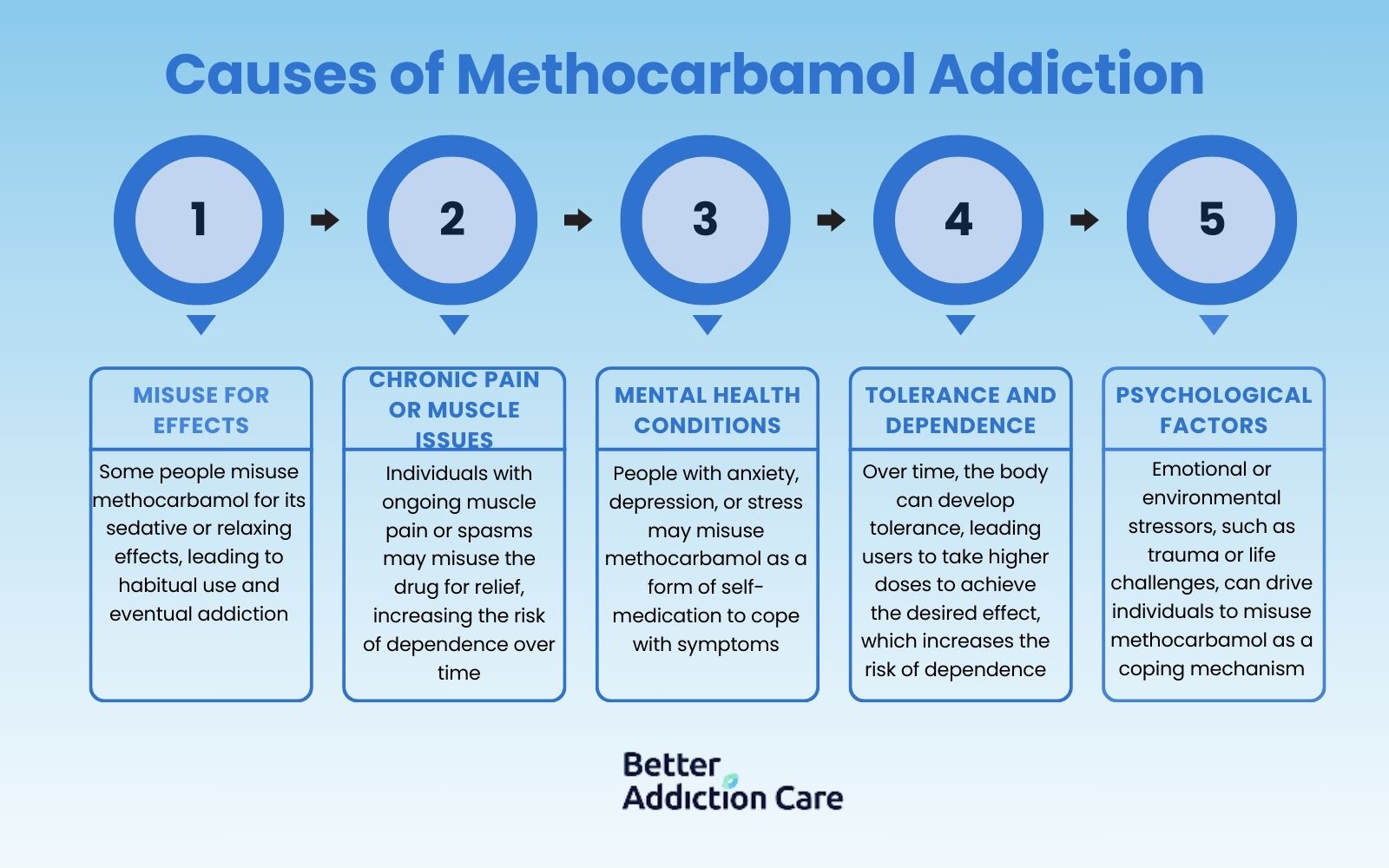
Individuals with a history of substance abuse are particularly at risk of developing methocarbamol addiction. Their past misuse of substances makes them more susceptible to seeking similar effects from methocarbamol, especially when used inappropriately or in combination with other CNS depressants. Prolonged misuse leads to both psychological dependence and the compulsive need to continue using the drug despite negative consequences.
What is the Withdrawal Timeline for Methocarbamol?
The withdrawal timeline for methocarbamol typically begins around 72 hours after the last dose, with symptoms peaking within the first few days. The duration of withdrawal varies depending on factors like dosage, duration of use, and individual differences. In most cases, withdrawal symptoms last from a few days up to two weeks. The acute withdrawal phase tends to resolve within one week, but psychological symptoms, such as anxiety or cravings, persist for a longer period. Withdrawal symptoms are minimal when methocarbamol is taken as prescribed. Pain returns within one to two hours after stopping the medication as its effects wear off according to Ferarra, D. in “Methocarbamol Withdrawal – What Are The Symptoms & How Long Do They Last?” .
There is no conclusive evidence to suggest a significant difference in the withdrawal timeline between males and females. However, individual metabolism, body composition, and overall health influences the severity and duration of withdrawal symptoms. People with a history of substance abuse or high-dose methocarbamol use, experience more intense withdrawal periods.
How to Treat Methocarbamol Addiction?
To treat methocarbamol addiction requires a comprehensive approach that includes both medical and psychological support. The most effective treatments combine therapy, medication, and treatment at a specialized center, among other options.
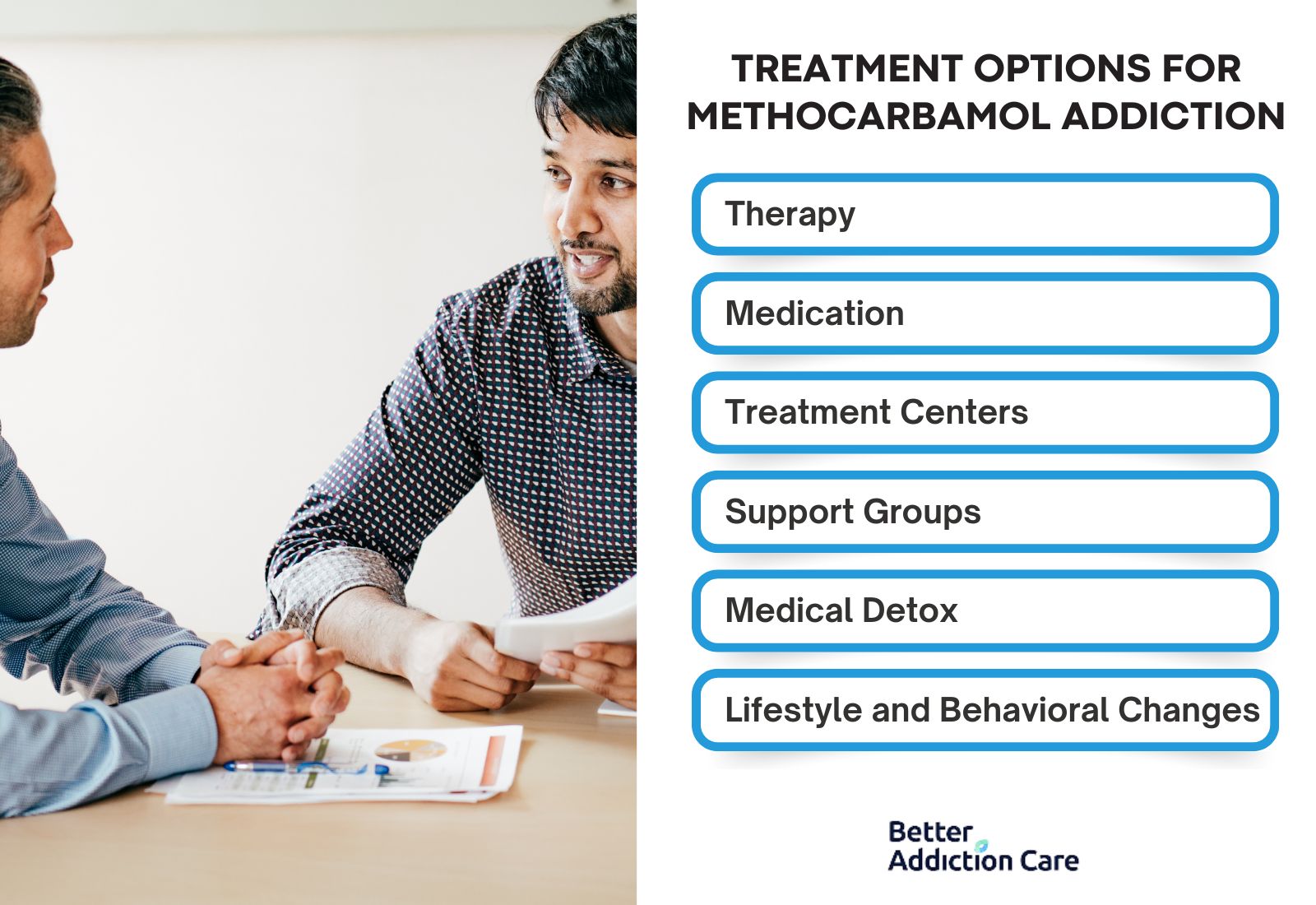
The treatment options for methocarbamol addiction include:
- Therapy: Cognitive Behavioral Therapy (CBT) and other forms of counseling help individuals address the psychological triggers of their addiction. Therapy helps users recognize harmful patterns of behavior, develop coping mechanisms, and prevent relapse. This form of treatment has been shown to be effective in managing drug dependency by reshaping thought processes and behaviors that contribute to addiction.
- Medication: Although there are no specific medications approved for treating methocarbamol addiction, doctors prescribe medications to manage withdrawal symptoms, such as anxiety, insomnia, or muscle pain. This makes the withdrawal process more bearable, reducing the risk of relapse during detoxification.
- Treatment Centers: Inpatient and outpatient treatment centers offer structured environments for recovery, providing access to medical care, therapy, and peer support. These centers are highly effective for individuals with severe addictions as they offer a supportive and controlled environment for recovery, reducing external triggers that could lead to relapse.
- Support Groups: Peer support groups like Narcotics Anonymous (NA) offer emotional support and accountability, which are important for long-term recovery. Sharing experiences with others who face similar struggles fosters community and reduces isolation, a common barrier to recovery.
- Medical Detox: In cases of severe dependency, a medically supervised detox program ensures safe withdrawal from methocarbamol. This option is highly efficient in minimizing the health risks associated with withdrawal, such as seizures or severe muscle pain, by offering around-the-clock medical care.
- Lifestyle and Behavioral Changes: Long-term recovery requires lifestyle changes, such as improving diet, increasing physical activity, and finding new hobbies or social circles to replace drug-seeking behavior. These changes are critical for maintaining sobriety and are very effective when combined with other forms of treatment.
How is Methocarbamol Regulated in the U.S.?
Methocarbamol is not classified as a controlled substance by the U.S. Drug Enforcement Administration (DEA). It has a relatively low potential for abuse compared to other muscle relaxants or opioids. Despite this, methocarbamol still requires a prescription from a licensed healthcare provider due to potential risks of misuse, especially when combined with other CNS depressants like alcohol or opioids. It is FDA-approved and requires a prescription in the U.S., though in Canada, lower doses are available over-the-counter. According to the Anatomical Therapeutic Chemical (ATC) Classification System, it falls under M03BA (Carbamic acid esters).
What is Methocarbamol Used For?
Methocarbamol is used for relieving muscle spasms and pain, particularly in cases of acute musculoskeletal injuries such as neck pain, lower back pain, and sprains. It helps ease discomfort by acting on the central nervous system (CNS) to relax muscles indirectly, without directly affecting muscle tissue. Methocarbamol is prescribed for short-term relief and is used in conjunction with rest, physical therapy, and sometimes other medications like NSAIDs to maximize pain reduction and improve mobility during recovery.
What is the Chemical Composition of Methocarbamol?
The chemical composition of methocarbamol is C₁₁H₁₅NO₅, which is its empirical formula. It is classified as a carbamate derivative of guaifenesin, making it a centrally acting muscle relaxant with properties that depress CNS activity to reduce muscle tension and pain. This classification aligns methocarbamol with other skeletal muscle relaxants used for short-term pain management.
What Does Robaxin Look Like?
Robaxin-750 look like white, capsule-shaped tablets, while the 500 mg Robaxin tablets are light orange and round with a film coating. These formats allow for dosing adjustments based on patient needs and treatment plans.
Can You Overdose on Robaxin?
Yes, you can overdose on Robaxin (methocarbamol) if you exceed the recommended dosage, which is generally 6 to 8 grams per day for short-term use. Taking amounts significantly above this range, especially 10 grams or more, increases the risk of severe side effects. The risk is even greater when Robaxin is combined with other central nervous system depressants, such as alcohol, opioids, or benzodiazepines, which amplifies the drug’s depressant effects on the brain and respiratory system.
What Happens if You Take Too Much Methocarbamol?
If you take too much methocarbamol, it leads to symptoms of overdose, such as extreme drowsiness, dizziness, confusion, slow reflexes, and even loss of consciousness. Overdosing also results in respiratory depression, where breathing becomes dangerously slow or shallow, potentially leading to coma or death. Severe overdose cases require hospitalization and even death. Immediate medical attention to prevent life-threatening complications is necessary.
Can Methocarbamol Cause an Overdose?
Yes, methocarbamol can cause an overdose if taken in excessive amounts. Muscle relaxants like methocarbamol, while generally less addictive than opioids, still lead to overdose when misused or combined with other CNS depressants. Overdosing on methocarbamol specifically affects the central nervous and respiratory systems, increasing the risk of fatal respiratory depression. From 2010 to 2020, there were 2,605 cases reported to the National Poison Data System and over half were suicide attempts.
What is the Dosage for Methocarbamol?
The typical adult dosage of methocarbamol for oral administration averages 1500 mg, taken three to four times per day, for both men and women. This dosage is increased initially, where two 750 mg tablets (totaling 1500 mg per dose) are taken four times daily during the first 48–72 hours of treatment to establish muscle relaxation. After this initial period, the dose is typically adjusted to 1000 mg three or four times per day for ongoing relief.
Methocarbamol is also available in intravenous (IV) form for medical use in hospital settings, particularly for acute cases. For pediatric patients under 16, methocarbamol is not recommended, as its safety and efficacy in younger populations have not been fully established.
Does Methocarbamol Treat Opiate Withdrawal?
No, methocarbamol does not treat opiate withdrawal. First, it does not interact with opioid receptors, which are crucial for addressing opiate withdrawal symptoms. Second, while it provides relief for muscle spasms, it does not alleviate core withdrawal symptoms such as nausea, cravings, or psychological distress. Third, methocarbamol lacks the targeted effects of medications like buprenorphine or methadone, which are specifically designed to reduce opiate dependence and withdrawal symptoms.
Does Methocarbamol Make You High?
No, methocarbamol does not make you high. It is designed to relax muscles rather than induce euphoria. Its action as a muscle relaxant does not affect dopamine levels, which are typically responsible for producing a high. Additionally, its calming effects primarily lead to drowsiness or mild sedation rather than euphoria, particularly at prescribed doses.
Is Methocarbamol Meth?
No, methocarbamol is not meth. "Meth" refers to methamphetamine, a powerful stimulant that is illegal in most contexts. Methamphetamine is known for its high potential for abuse and its intense stimulant effects on the central nervous system, leading to increased energy and euphoria. In contrast, methocarbamol is a CNS depressant, used medically to relieve muscle discomfort without the euphoric or stimulant effects associated with methamphetamine.
Is Robaxin a Narcotic?
No, Robaxin (methocarbamol) is not a narcotic. It is classified as a muscle relaxant rather than a narcotic because it does not produce the intense pain-relieving effects or addictive properties associated with narcotics like opioids. Robaxin works by depressing the central nervous system to reduce muscle spasms but lacks the opioid-based mechanism and euphoria that narcotics induce.
Is Methocarbamol a Benzodiazepine?
No, methocarbamol is not a benzodiazepine. Methocarbamol is a muscle relaxant that primarily targets skeletal muscle discomfort, while benzodiazepines are a class of drugs that act on the central nervous system to relieve anxiety, insomnia, and seizures. While both have sedative effects, benzodiazepines affect the GABA receptors in the brain to reduce anxiety and induce relaxation, whereas methocarbamol’s action focuses on relieving muscle tension through CNS depression without significant anti-anxiety effects.
Does Methocarbamol Interact with Other Medications?
Yes, methocarbamol does interact with other medications, especially those affecting the central nervous system (CNS).
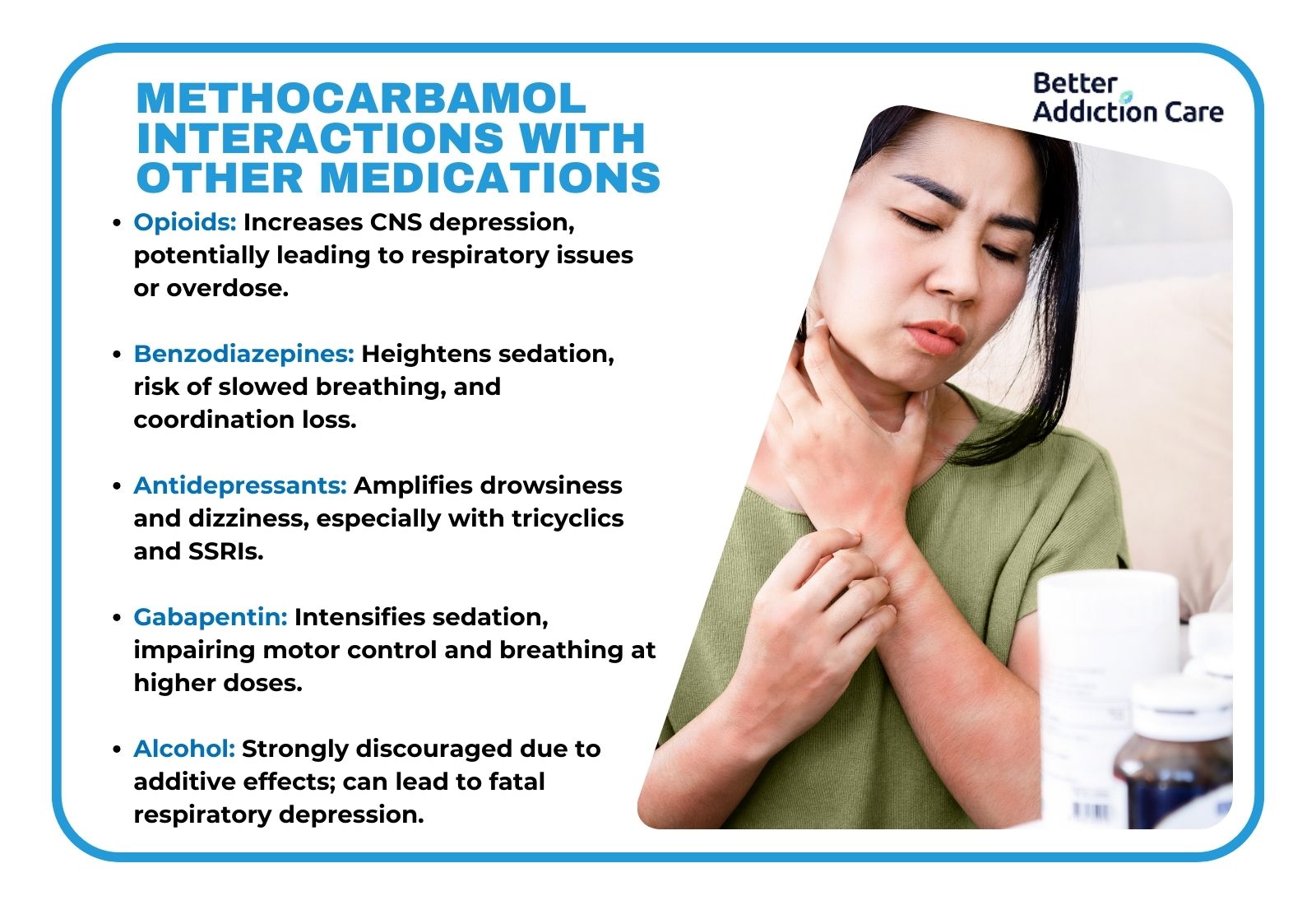
- Opioids: Combining methocarbamol with opioids increases the risk of severe CNS depression, potentially leading to extreme drowsiness, respiratory depression, or even overdose. Caution is advised, particularly with drugs like morphine or oxycodone.
- Benzodiazepines: When taken with benzodiazepines, methocarbamol intensifies sedation and depresses CNS function, heightening risks of confusion, slowed breathing, and loss of coordination. This is especially risky with medications like diazepam or lorazepam. The U.S. Food and Drug Administration (FDA) issued a strong warning in August 2008 about serious risks, including respiratory depression and fatalities, when combining muscle relaxers with benzodiazepines. The concurrent use of these CNS depressants greatly increases sedative effects, leading to life-threatening outcomes.
- Antidepressants: Certain antidepressants, particularly tricyclics and SSRIs, have their sedative effects enhanced when combined with methocarbamol, increasing drowsiness and dizziness.
- Gabapentin: Combining methocarbamol with gabapentin amplifies sedative effects and impair motor control, raising risks of severe drowsiness or respiratory problems, especially in higher doses.
- Alcohol: Methocarbamol and alcohol together produce additive CNS depressant effects, increasing the likelihood of confusion, respiratory depression, and even unconsciousness. This combination is strongly discouraged due to the high risk of serious side effects. There is a documented fatal case due to the combined use of methocarbamol and alcohol. This interaction occurred because both substances produced a synergistic effect, significantly increasing the risk of respiratory depression and fatal overdose according to a 1990 study published in the Journal of Forensic Sciences titled “A Fatal Interaction of Methocarbamol and Ethanol in an Accidental Poisoning”.
Is Methocarbamol a Strong Muscle Relaxer?
No, methocarbamol is not a strong muscle relaxer. It primarily works as a centrally acting muscle relaxant, indirectly reducing muscle spasms through CNS depression rather than directly affecting the muscles themselves. Compared to stronger muscle relaxants like baclofen or cyclobenzaprine, methocarbamol has milder sedative effects, making it more suitable for patients who need lower sedation levels. While higher doses (e.g., 1500 mg) increase its muscle-relaxing effects, it remains less potent than other muscle relaxants commonly prescribed for severe spasms.
Is Methocarbamol a Strong Painkiller?
No, methocarbamol is not a strong painkiller. It is classified as a muscle relaxant, so it addresses muscle pain indirectly by reducing spasms rather than providing direct pain relief. Methocarbamol lacks the analgesic properties found in NSAIDs or opioids, which target pain pathways. While increasing the dosage (such as up to 1500 mg) enhances its muscle relaxation effects, it does not increase its effectiveness as a painkiller.
Is Methocarbamol a Controlled Drug?
No, methocarbamol is not a controlled drug. It is not classified by the DEA as a controlled substance because it has a low potential for abuse compared to drugs in the controlled categories, such as opioids or benzodiazepines. This classification applies to both methocarbamol and its brand version, Robaxin, allowing it to be prescribed without the strict regulations that apply to controlled substances.
What are the types of Methocarbamol Pills?
The types of methocarbamol pills available include various formulations distinguished by their markings, color, and dosage levels. Each pill type represents a specific appearance and identification code, helping to differentiate between manufacturers and strengths.
The types of methocarbamol pills include:
H 115 pill
B134 pill
G 500 pill
S226 pill
Orange G 750 pill
ASC 750 pill
G750 pill
G 500 orange pill
H 114 pill







