Methocarbamol Interactions Drugs, Alcohol & Safety Concerns
Drug and alcohol interactions occur because the brain and body have finite safety limits for how much suppression or stimulation they can safely manage at once.
When two or more substances act on the same physiological systems—especially the central nervous system—their effects don’t simply add up. Instead, they can compound or multiply, overwhelming the brain’s ability to regulate alertness, coordination, decision-making, and breathing.
Understanding interaction risks helps people avoid dangerous sedation, impaired judgment, accidents, and medical emergencies that can occur when substances affect the same systems in the body.
It’s also about recognizing subtle warning signs early—like unusual drowsiness, confusion, or slowed reactions—before they escalate into serious harm.
In short, people look up interactions to protect themselves, maintain daily functioning, and reduce real-world risks that don’t always show up on a prescription label but can have lasting consequences.
What Is Methocarbamol?
Methocarbamol is a prescription muscle relaxant commonly used to relieve muscle spasms and discomfort caused by injuries or musculoskeletal conditions.[1]
Rather than acting directly on the muscles themselves, it works by influencing the nervous system, reducing the brain’s signals that contribute to muscle tension and pain.
It is often prescribed for short-term use, but some people may take it longer due to chronic pain conditions or repeated injuries. While it is not classified as a controlled substance, its effects on alertness and coordination mean it still requires caution—especially when combined with other substances.
How Methocarbamol Affects the Central Nervous System?
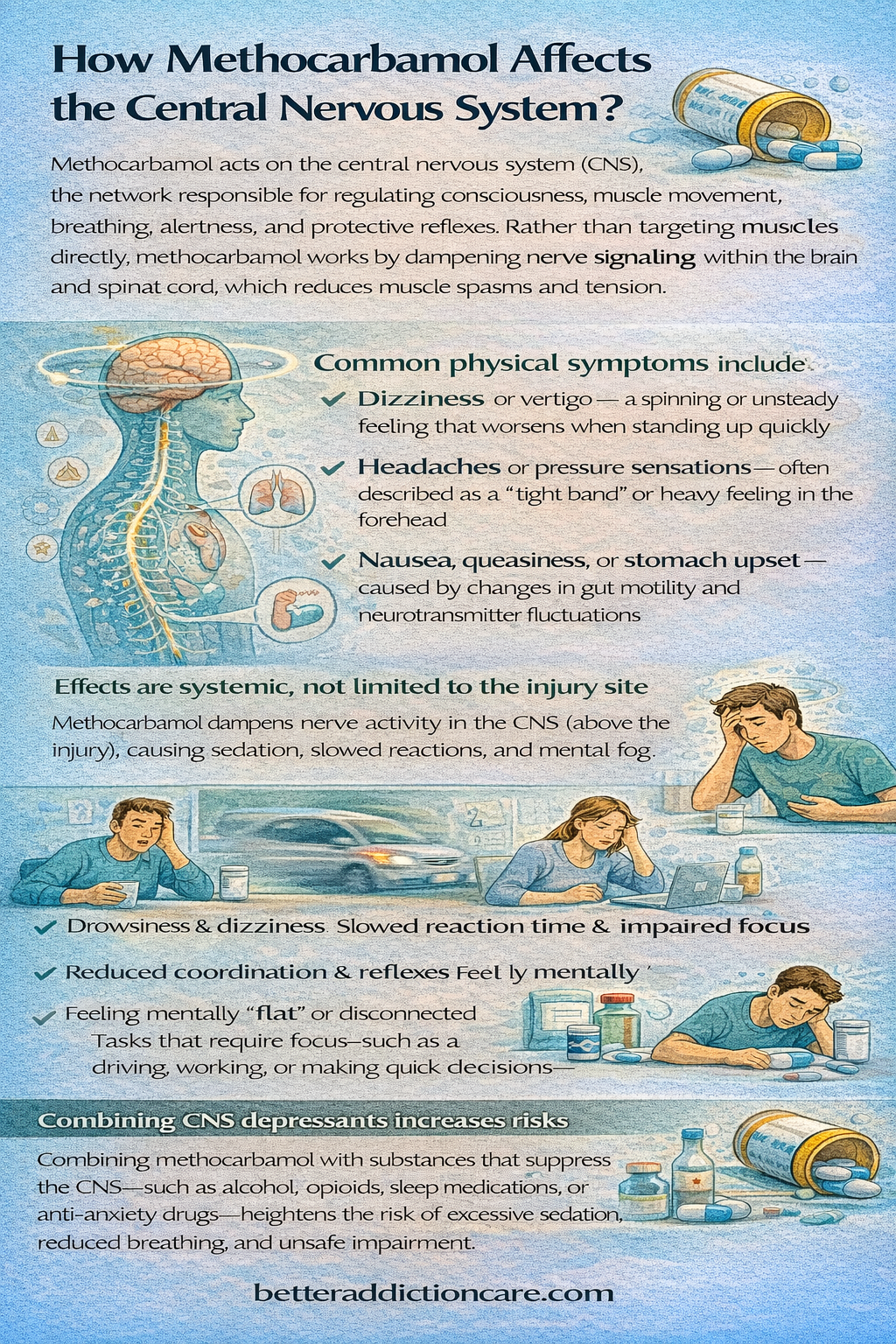
Methocarbamol acts on the central nervous system (CNS), the network responsible for regulating consciousness, muscle movement, breathing, alertness, and protective reflexes. Rather than targeting muscles directly, methocarbamol works by dampening nerve signaling within the brain and spinal cord, which reduces muscle spasms and tension.
While this mechanism can be effective for pain relief, it also means the medication’s effects are systemic—not localized to the site of injury.
As a result, many people experience sedation, slowed reaction time, dizziness, lightheadedness, or mental fog, particularly when starting the medication, increasing the dose, or taking it more frequently.
Tasks that require focus—such as driving, working, or making quick decisions—may feel noticeably harder. Some individuals also report feeling emotionally “flat” or disconnected, which reflects broader CNS suppression rather than muscle relaxation alone.[2]
Because the CNS also regulates breathing, awareness, and arousal, any additional substance that suppresses this system—such as alcohol, opioids, sleep medications, or anti-anxiety drugs—can significantly magnify methocarbamol’s effects. This overlap increases the risk of excessive sedation, reduced respiratory drive, and impaired safety awareness.
This CNS involvement is the core reason interactions matter and why methocarbamol must be used cautiously in combination with other substances.
Why Drug and Alcohol Interactions Occur?
Drug and alcohol interactions occur because the brain and body have finite safety limits for how much suppression or stimulation they can safely manage at once.
When two or more substances act on the same physiological systems—especially the central nervous system—their effects don’t simply add up. Instead, they can compound or multiply, overwhelming the brain’s ability to regulate alertness, coordination, decision-making, and breathing.
The CNS is particularly vulnerable because it controls automatic functions we don’t consciously monitor, such as respiratory rhythm and wakefulness. When these systems are pushed beyond their limits, the body may not give clear warning signs before impairment becomes dangerous.
Common interaction outcomes include:
-
Excessive sedation or sudden, overwhelming fatigue, even at low doses
-
Impaired judgment, slowed thinking, and reduced situational awareness
-
Loss of coordination and increased fall or injury risk, especially in older adults
-
Respiratory suppression, particularly during rest or sleep, when breathing is already naturally slower
These risks are not theoretical. They appear regularly in emergency rooms as falls, motor vehicle accidents, episodes of unresponsiveness, and breathing emergencies.
In many cases, individuals did not realize they were combining substances considered “mild,” “prescribed,” or “safe when used alone.” The danger often lies not in a single substance, but in the interaction between them—especially when CNS depressants are involved.
Methocarbamol and Alcohol Interactions
Alcohol is one of the most dangerous substances to combine with methocarbamol, and this interaction is widely considered high-risk. Both substances act as central nervous system (CNS) depressants, meaning they slow brain activity, suppress alertness, and reduce coordination. When taken together, their effects don’t just add up—they amplify each other in unpredictable ways.
This combination can significantly intensify:
-
Drowsiness, extreme fatigue, or blackouts, making it difficult to stay awake or remember events
-
Poor balance, slowed reflexes, and impaired coordination increase the likelihood of slips, falls, or motor vehicle accidents.
-
Confusion, disorientation, and impaired judgment, which may resemble intoxication or acute cognitive impairment
-
Delayed reaction times make everyday tasks—especially driving or operating machinery—dangerous.
For some individuals, even small amounts of alcohol can trigger unexpected over-sedation when combined with methocarbamol. This risk is higher in older adults, people taking other medications such as benzodiazepines, opioids, or sleep aids, and individuals who are particularly sensitive to CNS depressants. In severe cases, excessive sedation can suppress breathing, lower blood pressure, and require medical attention.
For people in recovery, the risks extend beyond physical safety. Alcohol use—whether intentional, social, or accidental—can disrupt emotional regulation, impair impulse control, and increase vulnerability to relapse.
Mixing alcohol with methocarbamol may also dull self-awareness, making it harder to recognize warning signs or maintain coping strategies. The combination isn’t just physically dangerous; it can undermine stability, confidence, and hard-won progress in recovery.
Because of these risks, healthcare providers typically recommend avoiding alcohol entirely while taking methocarbamol, even in small amounts.
Prescription Drug Interactions With Methocarbamol
Several categories of prescription medications pose an elevated risk when combined with methocarbamol due to overlapping CNS effects:
-
Opioid pain medications: When methocarbamol is taken with opioids, their sedating effects can reinforce each other, leading to extreme drowsiness, slowed reaction time, and dangerously suppressed breathing[3]. This combination significantly increases overdose risk, especially at higher doses or in individuals with reduced tolerance or underlying respiratory conditions.
-
Benzodiazepines: Medications commonly prescribed for anxiety, panic, or insomnia can intensify methocarbamol’s effects on memory, coordination, and alertness. Together, these drugs may cause pronounced confusion, delayed response time, and respiratory depression—effects that may not be immediately noticeable but can escalate rapidly.
-
Sleep medications or sedating antidepressants: Combining methocarbamol with sleep aids or sedating antidepressants often results in excessive next-day grogginess and impaired balance. This is particularly concerning for older adults or individuals who need to drive, work, or manage daily responsibilities safely the following day.
-
Other muscle relaxants: Using more than one muscle relaxant rarely improves pain control and often leads to compounded nervous system suppression. The added sedation can increase fall risk, impair cognition, and place unnecessary strain on the body without meaningful therapeutic benefit.
When multiple CNS-active medications are prescribed together, interaction risk rises sharply—especially without close monitoring and ongoing reassessment.
Over-the-Counter Medication Interactions
Many people underestimate over-the-counter (OTC) products, assuming they are always safe. In reality, several common OTC medications can quietly increase interaction risk, including:
-
Antihistamines used for allergies or sleep: First-generation antihistamines are especially sedating and can dramatically increase drowsiness when combined with methocarbamol. This may result in mental fog, delayed reaction time, and difficulty staying awake—effects that are often underestimated until impairment occurs.
-
Cold and flu medications with sedating ingredients: Multi-symptom cold and flu products often contain ingredients that depress the central nervous system. When combined with methocarbamol, these products can amplify confusion, dizziness, and coordination problems, particularly when taken during illness or physical exhaustion.
-
Nighttime pain relievers or sleep aids: These products are designed to induce sleep and relaxation, which can dangerously overlap with methocarbamol’s calming effects. Combined use increases the risk of over-sedation, nighttime disorientation, and next-day impairment—especially if alcohol is also involved.
These products can worsen drowsiness, slow reaction time, and increase confusion—particularly when taken at night or mixed without medical guidance.
Methocarbamol and Recreational or Non-Prescribed Substances
Combining methocarbamol with recreational or non-prescribed substances significantly increases unpredictability and potential harm, particularly when use occurs outside medical supervision.
Methocarbamol acts as a central nervous system (CNS) depressant, and when paired with other substances that have sedating or psychoactive effects, those effects can compound in dangerous ways [1].
Substances such as:
-
Illicit opioids
-
non-prescribed sedatives
can intensify CNS depression, leading to excessive drowsiness, slowed reaction times, impaired coordination, and reduced cognitive function. Judgment and decision-making may become compromised, increasing the risk of accidents, falls, or unsafe behaviors.
In more severe cases, combined use may suppress breathing, raise overdose risk, or contribute to loss of consciousness—especially at higher doses or in individuals with underlying medical vulnerabilities.
For individuals with a history of substance use disorder, these combinations pose additional concerns beyond immediate physical effects.
Mixing methocarbamol with recreational substances can reactivate craving pathways in the brain, weaken coping mechanisms, and destabilize recovery efforts. Even intermittent or “casual” use may erode progress by reintroducing patterns of polysubstance use, increasing the likelihood of relapse over time.
Because of these risks, methocarbamol should be used only as prescribed, and any use of recreational substances should be openly discussed with a healthcare provider. Careful monitoring, clear boundaries around substance use, and recovery-informed medical guidance are essential to reducing harm and maintaining long-term stability.
Who Is at Higher Risk From Interactions?
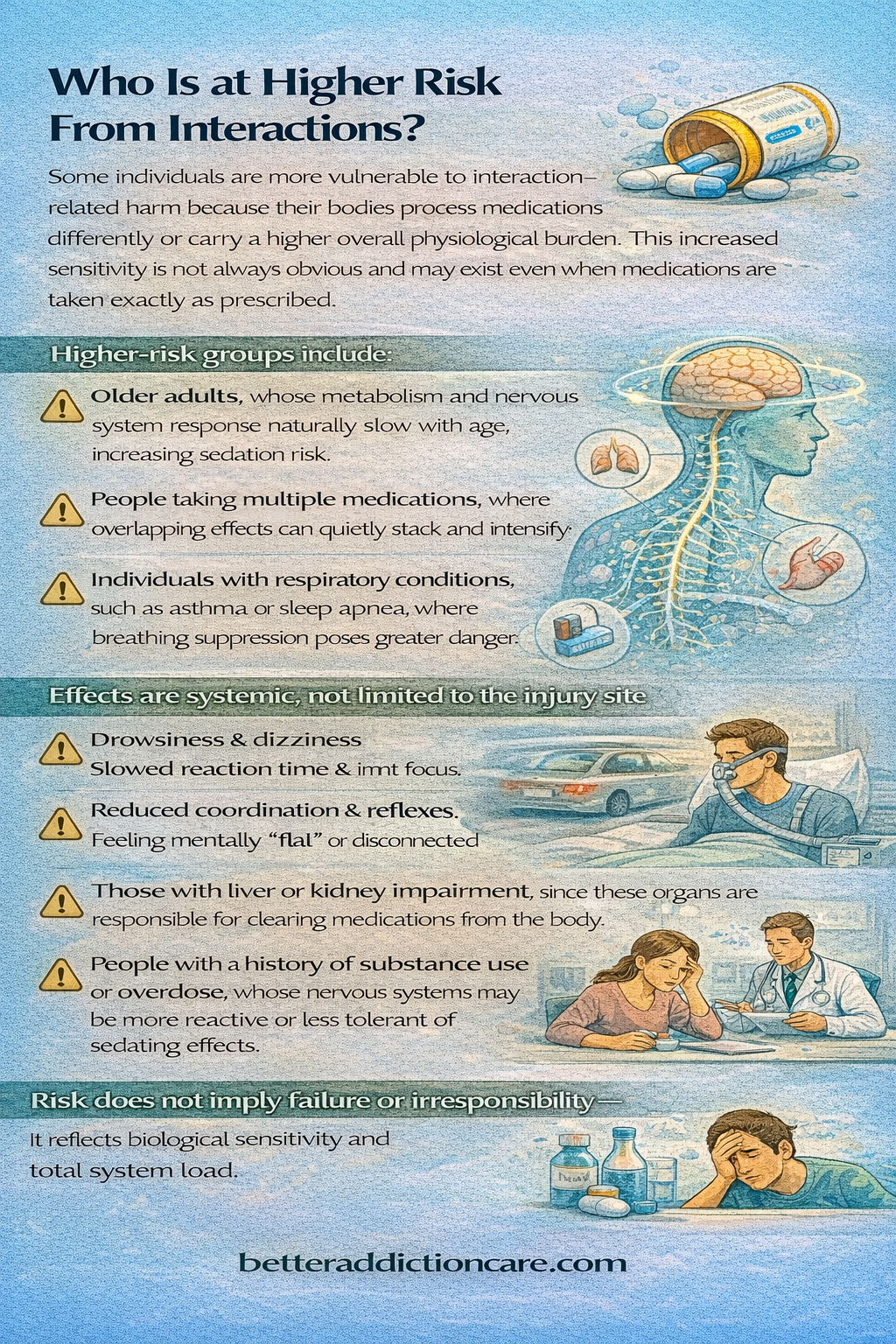
Some individuals are more vulnerable to interaction-related harm because their bodies process medications differently or carry a higher overall physiological burden. This increased sensitivity is not always obvious and may exist even when medications are taken exactly as prescribed.
Higher-risk groups include:
-
Older adults, whose metabolism and nervous system response naturally slow with age, increasing sedation risk.
-
People taking multiple medications, where overlapping effects can quietly stack and intensify.
-
Individuals with respiratory conditions, such as asthma or sleep apnea, where breathing suppression poses greater danger.
-
Those with liver or kidney impairment, since these organs are responsible for clearing medications from the body.
-
People with a history of substance use or overdose, whose nervous systems may be more reactive or less tolerant of sedating effects.
Risk does not imply failure or irresponsibility—it reflects biological sensitivity and total system load.
Common Side Effects That May Worsen With Interactions
Methocarbamol has known side effects on its own, but interactions can magnify these effects far beyond what a person expects. What begins as mild discomfort can escalate quickly when substances overlap in the body.
When interactions occur, side effects may intensify, including:
-
Extreme drowsiness is making it difficult to stay alert or function safely.
-
Dizziness or lightheadedness, which raises the risk of falls and injury.
-
Blurred vision, affecting coordination and reaction time.
-
Confusion or memory problems, which may feel sudden or disorienting.
What feels like “just being tired” can cross into unsafe impairment, especially during daily activities like driving, working, or caring for others.
Warning Signs of a Dangerous Interaction
Certain symptoms signal that the body is struggling to manage the combined effects of medications or substances. These warning signs should never be ignored or minimized[4].
Seek urgent medical attention if any of the following occur:
-
Trouble staying awake or difficulty being awakened
-
Slowed, shallow, or irregular breathing
-
Severe confusion or disorientation
-
Loss of coordination or repeated falls
-
Unresponsiveness or inability to communicate
These symptoms reflect nervous system overload—not personal weakness. Prompt medical care can prevent serious injury and save lives.
Safe Use and Risk-Reduction Guidelines
Safe use of methocarbamol begins with understanding how it affects the central nervous system and how easily risks increase when substances are combined.
Even when prescribed appropriately, poor coordination between medications, alcohol, or supplements can amplify side effects in unexpected ways.
General safety practices include:
-
Avoiding alcohol while taking methocarbamol, as even small amounts can intensify sedation and impair judgment.
-
Reviewing all medications—including over-the-counter pain relievers, sleep aids, and herbal products—with a healthcare provider, since many have hidden sedating effects.
-
Using only one CNS-active medication at a time when possible, to reduce cumulative suppression of alertness and breathing.
-
Not mixing substances without medical guidance, even if each product feels “mild” on its own.
-
Consistency, transparency, and caution significantly reduce harm. Open communication saves lives.
Methocarbamol and Dependency or Misuse Considerations
Methocarbamol is not typically associated with classic addiction or compulsive drug-seeking behavior. However, psychological reliance can still develop—particularly when physical relief becomes closely linked to emotional comfort, stress reduction, or avoidance of distressing feelings.
For individuals in or considering recovery, this distinction matters. Repeated reliance on sedating relief can quietly shift coping patterns, especially during periods of pain, anxiety, or sleep disruption.
Over time, tolerance, combined sedation from other medications, or habitual use during emotional discomfort may raise concern.
These risks deserve attention—not judgment. Awareness allows individuals and providers to adjust treatment early, reinforce healthier coping strategies, and ensure pain management supports long-term stability rather than undermining it.
When to Speak With a Doctor or Specialist?
Professional guidance becomes especially important when complexity increases or uncertainty arises. Even mild symptoms can signal a need for adjustment when medications affect the nervous system.
You should speak with a doctor or specialist if:
-
Multiple medications are involved, especially those affecting mood, sleep, or anxiety.
-
There is a history of substance use disorder, even if recovery has been long-term or stable.
-
Side effects feel stronger or different than expected, such as confusion, excessive fatigue, or emotional blunting.
-
Alcohol use is difficult to avoid, increasing the risk of unintended interactions.
Early conversations prevent crisis-driven decisions. Reaching out before problems escalate is a sign of strength, not failure—and often leads to safer, more sustainable care.
Final Takeaway
Methocarbamol interactions matter because they affect the systems that keep people awake, breathing, and safe. Understanding these risks empowers individuals and families to make informed decisions—without fear, shame, or false reassurance.
Safety isn’t about being perfect—it’s about staying aware, communicating openly, and taking proactive steps, especially during recovery.
FAQs
Timing does not eliminate interaction risk. Methocarbamol can stay active in your system longer than you expect. When combined with alcohol, even hours later, side effects like dizziness, slowed reactions, and impaired judgment can intensify. For safety, it’s best to avoid alcohol entirely while using this medication.
Some anxiety medications—especially benzodiazepines or sedating antidepressants—can amplify drowsiness when taken with methocarbamol. This combination may increase the risk of confusion, poor coordination, or breathing suppression. A healthcare provider should always review these combinations before use.
Methocarbamol can be used safely during recovery when it’s carefully monitored and taken as prescribed. The main concern is its sedating effect, which may mask warning signs or trigger cravings in some individuals. Open communication with a healthcare provider helps ensure it supports healing rather than interferes with it.
Yes, drowsiness and mental slowing are common side effects, especially in the first few days. These effects can impact focus, reaction time, and daily functioning. Avoid driving or demanding tasks until you know how your body responds.
Combining methocarbamol with sleep aids or calming drugs can increase excessive sedation. This may lead to deeper-than-expected sleep, confusion, or breathing suppression. Always check with a healthcare provider before using them together.
Early recovery is a sensitive period where sedating medications require extra caution. Methocarbamol may dull physical or emotional signals that are important during stabilization. Close medical supervision helps ensure safety during this stage.







