What Is Paroxetine? Paxil Addiction, Abuse Signs, and Treatment
Paroxetine (brand name Paxil) is an SSRI antidepressant that increases serotonin availability in the brain by blocking its reabsorption at nerve synapses. Serotonin plays a central role in mood regulation, anxiety control, sleep, and emotional processing. [1]
Key Takeaways
-
Paroxetine (Paxil) is a prescription antidepressant classified as a selective serotonin reuptake inhibitor (SSRI), used to treat depression, anxiety disorders, PTSD, OCD, and panic disorder.
-
Paxil is not addictive in the traditional sense like opioids or benzodiazepines, but it has a higher risk of dependence and discontinuation symptoms compared to many other SSRIs.
-
Misuse typically develops through long-term reliance, dose escalation without supervision, or fear of emotional relapse, not through euphoria or intoxication.
-
Safe tapering, medical oversight, and emotional support are essential to prevent withdrawal distress and relapse when stopping Paxil.
Many people first encounter Paxil during a period of emotional vulnerability—after panic attacks begin, depression disrupts daily life, or anxiety becomes overwhelming.
For some, it offers life-changing stability. For others, stopping it later feels far harder than expected.
People may begin to wonder: Can you get addicted to Paxil? Why does missing a dose feel so uncomfortable?
This article explains what paroxetine is, how it affects the brain, how misuse or dependence can develop, and what safe treatment and discontinuation look like—so individuals and families can make informed, confident decisions.
What Is Paxil Addiction?
Paroxetine (brand name Paxil) is an SSRI antidepressant that increases serotonin availability in the brain by blocking its reabsorption at nerve synapses. Serotonin plays a central role in mood regulation, anxiety control, sleep, and emotional processing. [1]
Unlike addictive substances, Paxil does not stimulate dopamine-driven reward pathways associated with cravings, compulsive use, or intoxication. It does not create a “high,” intoxication, or reinforcement loop based on pleasure.
However, Paxil does strongly influence brain chemistry, and over time, the nervous system adapts to its presence. When the medication is reduced or stopped abruptly, the brain may struggle to rebalance serotonin signaling.
In clinical terms:
-
Tolerance is uncommon, but some patients feel reduced emotional benefit over time.
-
Dependence refers to the brain adapting to Paxil, leading to withdrawal symptoms when doses are missed.
-
Addiction involves compulsive use despite harm, which is rare with SSRIs.
Paxil is not addictive, but it has one of the highest discontinuation symptom rates among SSRIs, which can cause dependence-like patterns if not managed carefully.
Signs & Symptoms of Paxil Misuse

Physical Signs
-
Withdrawal symptoms between doses: Because Paxil has a short half-life, even a delayed or missed dose can trigger symptoms such as dizziness, nausea, electric-shock sensations (“brain zaps”), sweating, tremors, or flu-like discomfort. These symptoms often appear quickly and resolve after taking the next dose, reinforcing continued use.
-
Headaches or gastrointestinal upset: Recurrent headaches, stomach pain, diarrhea, bloating, or appetite changes may occur during dose adjustments or missed doses. These physical reactions can increase anxiety about altering the medication.
-
Sleep disturbances: Individuals may experience insomnia, frequent nighttime awakenings, vivid or disturbing dreams, or excessive daytime drowsiness. Sleep disruption can worsen mood and anxiety, further tying emotional stability to the medication.
-
Sexual dysfunction worsening over time: Reduced libido, delayed orgasm, or an inability to experience sexual pleasure may gradually intensify. Despite growing distress or relationship strain, the fear of stopping Paxil often outweighs concerns about these side effects.
-
Dose escalation without guidance: Some individuals increase their dose on their own to regain emotional stability or suppress withdrawal sensations, especially during stressful periods.
Emotional / Psychological Signs
-
Fear of stopping the medication: The idea of tapering can provoke intense anxiety, panic, or intrusive thoughts, even when symptoms are well-controlled or side effects are significant.
-
Emotional blunting: A persistent sense of numbness, detachment, or reduced emotional range may develop. People may describe feeling “flat,” disconnected, or unable to experience joy, grief, or excitement fully.
-
Irritability or agitation between doses: Mood swings, restlessness, or sudden anxiety may emerge as blood levels drop, particularly late in the dosing cycle.
-
Using Paxil for emotional safety: The medication is taken primarily to prevent discomfort, anxiety, or withdrawal rather than to actively treat current symptoms. Paxil becomes associated with safety, control, and emotional containment.
-
Catastrophic thinking about relapse: Individuals may believe that stopping Paxil will inevitably lead to emotional collapse, loss of control, or a return to their worst mental health state, regardless of current stability or supports.
Behavioral Signs
-
Requesting early refills: Often driven by fear of running out, missing a dose, or experiencing withdrawal rather than increased symptom severity.
-
Refusal to consider tapering: Resistance to discussing dose reduction persists even in the presence of side effects, emotional blunting, or medical recommendations to reassess treatment.
-
Stockpiling medication “just in case”: Keeping extra pills for emergencies or travel reflects anxiety around availability rather than misuse for intoxication.
-
Hiding dose increases or missed doses from providers: Shame, fear of judgment, or concern about being advised to taper may lead to incomplete disclosure.
-
Long-term use without reassessment: Remaining on Paxil for years without periodic evaluation of ongoing need, dose appropriateness, or alternative treatments.
How Common Is It?
General Prevalence
Large pharmacovigilance analyses of adverse event reporting systems show that paroxetine is disproportionately associated with dependence-related signals among SSRIs.
In U.S. databases, dependence-related reports were significantly more frequent for paroxetine than for several other SSRIs, indicating clinicians and patients report these issues more often for Paxil than for many alternatives. [2]
According to the WHO spontaneous reporting data on antidepressant withdrawal, paroxetine was the most frequently implicated drug in withdrawal syndrome cases out of all antidepressants reported, with nearly 10 000 cases identified globally. [3]
Clinical Settings
In outpatient psychiatry and primary care, long-term Paxil (paroxetine) use is common for depression and anxiety disorders, but adherence and discontinuation challenges are frequently reported.
Real-world studies show that paroxetine has higher rates of treatment interruption and discontinuation compared with several other SSRIs, largely due to tolerability issues and withdrawal symptoms. [3]
Older adults are particularly vulnerable; paroxetine is classified in multiple geriatric guidelines as potentially inappropriate in patients aged 60+ because of its anticholinergic effects, sedation, and higher risk of adverse reactions, often leading to dose changes or discontinuation. [4]
Misuse in these settings is usually unintentional, involving abrupt stopping, skipped doses, or unsupervised dose adjustments driven by side effects or fear of withdrawal. Education, slow tapering, and close clinical monitoring are central to prevention and safer long-term use. [5]
Withdrawal Frequency
Unlike typical withdrawal syndromes seen with opioids or benzodiazepines, Paxil’s antidepressant discontinuation syndrome is not an addiction per se but can be very distressing and clinically significant.
-
Analyses indicate that paroxetine is disproportionately represented in antidepressant withdrawal reports, far more than many other SSRIs. [3]
-
Withdrawal symptoms can range from dizziness, insomnia, and agitation to more severe effects such as sensory disturbances and psychological discomfort. [6]
-
Research suggests that abrupt discontinuation of paroxetine markedly increases the risk of experiencing these symptoms, and gradual tapering reduces the incidence.
Causes: Why Does Paxil Misuse Happen?

Neurobiology
Paxil (paroxetine) works by increasing the availability of serotonin in the brain, a neurotransmitter involved in mood regulation, anxiety control, sleep, and emotional processing.
With long-term use, the brain adapts to this artificial elevation. Serotonin receptors gradually downregulate, and neural pathways begin to rely on the medication to maintain equilibrium rather than producing balance independently.
When Paxil is reduced too quickly or stopped abruptly:
-
Serotonin signaling drops sharply, creating an immediate neurochemical imbalance.
-
Neural communication becomes unstable, especially in areas governing mood, sensory perception, and autonomic regulation.
-
Sensory, cognitive, and emotional symptoms emerge, including dizziness, brain zaps, emotional volatility, panic, and depersonalization.
Unlike euphoria-producing substances, Paxil reinforces use through relief, not pleasure. It prevents distress rather than creating a “high.” Over time, the brain associates stopping Paxil with discomfort and continuing it with stability. While this is not classic addiction, this avoidance-based reinforcement can mirror dependency by conditioning fear around discontinuation.
Genetic & Biological Factors
Individual biology plays a significant role in why some people struggle more with Paxil dependence than others. Genetic differences in serotonin transporters and liver enzymes can influence how strongly the drug affects the brain and how quickly it is cleared from the body.
-
Some individuals are genetically more sensitive to serotonin fluctuations, making even small dose changes feel overwhelming.
-
People with panic disorder, OCD, or PTSD often experience exaggerated rebound anxiety, as their nervous systems are already hyperreactive.
-
Slow drug metabolism can cause drug levels to build up, increasing side effects and reinforcing the fear of dose changes.
-
Hormonal shifts, aging, and polypharmacy (use of multiple medications) can alter Paxil’s effects, increase nervous system instability, and complicate tapering.
Psychological & Emotional Triggers
Psychological factors often sustain long-term Paxil use even after symptoms have improved. The fear of what might return can become stronger than the original condition itself.
-
Fear of relapse is a major driver of continued use, especially after severe or prolonged depressive episodes.
-
Past mental health crises increase emotional reliance, making the medication feel protective rather than optional.
-
Trauma history heightens sensitivity to internal distress, making withdrawal sensations feel threatening or intolerable.
-
Paxil may become a perceived emotional “anchor”, associated with safety, stability, and survival during difficult periods.
Environmental & Social Factors
External circumstances can unintentionally reinforce long-term use and discourage reassessment.
-
Extended prescriptions without regular review may normalize indefinite use.
-
Limited access to psychotherapy leaves medication as the primary coping tool.
-
Cultural narratives often frame antidepressants as lifelong necessities rather than time-limited supports.
-
Chronic life stressors—work pressure, caregiving, financial strain—make experimentation without medication feel unsafe.
From Treatment to Dependence (Progression)
-
Diagnosis: Anxiety, depression, panic disorder, or PTSD prompts treatment.
-
Stabilization: Paxil provides emotional relief, symptom reduction, and improved daily functioning.
-
Adaptation: The brain adjusts to sustained serotonin modulation and reduces its independent regulation.
-
Missed-dose distress: Withdrawal symptoms appear rapidly due to Paxil’s short half-life.
-
Avoidance: Medication is taken to prevent discomfort rather than solely to treat symptoms.
-
Psychological dependence: Stopping feels unsafe, destabilizing, or emotionally dangerous—even when medically appropriate.
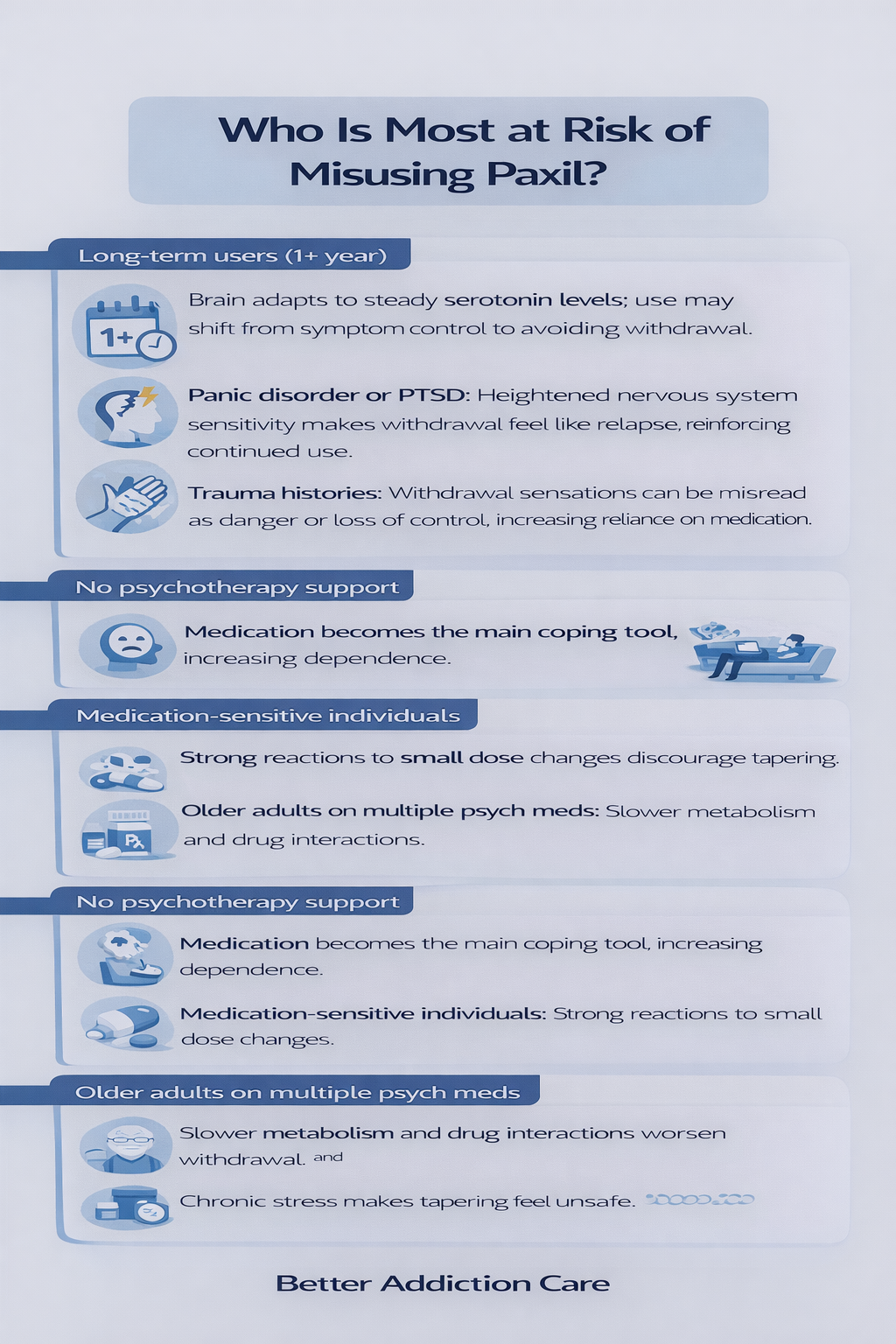
Who Is Most at Risk of Misusing Paxil?
-
Long-term users (1+ year): Brain adapts to steady serotonin levels; use may shift from symptom control to avoiding withdrawal.
-
Panic disorder or PTSD: Heightened nervous system sensitivity makes withdrawal feel like relapse, reinforcing continued use.
-
Trauma histories: Withdrawal sensations can be misread as danger or loss of control, increasing reliance on medication.
-
No psychotherapy support: Medication becomes the main coping tool, increasing dependence.
-
Medication-sensitive individuals: Strong reactions to small dose changes discourage tapering.
-
Older adults on multiple psych meds: Slower metabolism and drug interactions worsen withdrawal and side effects.
Side Effects of Paxil Misuse
Short-Term Effects
-
Nausea, dizziness, or headaches: These symptoms often emerge during dose changes, missed doses, or timing inconsistencies. Because they improve after the next dose, they can reinforce continued use to avoid physical discomfort rather than address underlying symptoms.
-
Emotional flattening: Individuals may notice a reduced emotional range, feeling less sadness but also less joy, excitement, or emotional responsiveness. This effect can appear early and is often subtle at first.
-
Sexual side effects: Decreased libido, delayed orgasm, or difficulty achieving sexual satisfaction can occur even at stable doses. These effects may cause distress but are often tolerated due to fear of symptom return.
-
Sleep disruption: Insomnia, frequent awakenings, vivid dreams, or excessive drowsiness can interfere with daily functioning and emotional regulation.
-
Anxiety spikes with dose changes: Even small adjustments or delayed doses can provoke anxiety, agitation, or panic-like symptoms, particularly in sensitive individuals.
Long-Term Effects
-
Persistent emotional numbness: Over time, emotional blunting may become more pronounced, affecting the ability to experience connection, motivation, or pleasure.
-
Weight gain or metabolic changes: Long-term use may be associated with appetite changes, weight gain, or altered metabolic regulation, which can affect self-image and physical health.
-
Cognitive fog: Difficulty concentrating, slowed thinking, memory lapses, or reduced mental clarity may develop, especially in older adults or those on multiple medications.
-
Reduced stress tolerance: Reliance on Paxil for emotional regulation can make everyday stressors feel more overwhelming without medication support.
-
Difficulty discontinuing despite motivation: Even when individuals want to stop, withdrawal symptoms and fear of destabilization can delay or prevent tapering.
Impact on Daily Life
-
Relationship strain: Emotional blunting, sexual side effects, or irritability can affect intimacy, communication, and connection with partners and family.
-
Reduced emotional engagement: People may feel less present or responsive in social, professional, or family roles.
-
Fear-based decision-making: Choices may revolve around avoiding missed doses, travel disruptions, or medication changes rather than personal goals.
-
Dependence on routines and refills: Daily life may become structured around medication timing, prescription access, and refill anxiety.
-
Financial and healthcare burden: Ongoing prescriptions, frequent appointments, and management of side effects can create long-term financial and logistical strain.
Treatment Options for Paxil Dependence
Recovery from Paxil dependence prioritizes stability, reassurance, and gradual nervous system recalibration rather than abrupt medication cessation.
The goal is not to force discontinuation, but to reduce fear, minimize withdrawal distress, and restore confidence in emotional regulation over time.
Detox / Withdrawal Management
-
Slow tapering: Gradual dose reductions—often 10–25% every few weeks—allow the brain time to adapt to changing serotonin levels. Some individuals require even smaller reductions, especially after long-term use or at lower doses.
-
Liquid formulations: Liquid Paxil or compounded doses enable precise, incremental reductions that tablets cannot provide. This flexibility is especially important for people who experience symptoms with small dose changes.
-
Symptom monitoring: Taper schedules are adjusted based on physical and emotional responses rather than rigid timelines. Temporary pauses or slower reductions are common and appropriate when symptoms intensify.
-
Temporary supports: Non-addictive medications may be used short-term to manage sleep disruption, nausea, headaches, or gastrointestinal discomfort. These supports are intended to reduce suffering—not replace Paxil or prolong dependence.
Medication-Assisted Support
-
Switching to longer half-life SSRIs in select cases: Some individuals benefit from transitioning to a medication with a longer half-life to smooth withdrawal effects. This approach is individualized and not required for most patients.
-
Short-term use of supportive medications: Agents targeting anxiety, sleep, or autonomic symptoms may be used cautiously and temporarily during tapering.
-
Avoiding sedative substitutions unless necessary: Replacing Paxil with benzodiazepines or other sedatives can introduce new dependence risks. These are generally avoided unless clinically justified and closely monitored.
Levels of Care
-
Outpatient care: Most individuals successfully taper Paxil under outpatient supervision with regular check-ins, education, and emotional support.
-
Intensive outpatient programs (IOP): For those with severe anxiety, panic symptoms, or repeated taper setbacks, structured programs provide therapeutic intensity without full hospitalization.
-
Inpatient care: Rarely required and reserved for complex psychiatric presentations, severe destabilization, or co-occurring conditions requiring close monitoring.
Therapies
-
Cognitive Behavioral Therapy (CBT): Helps identify and reframe catastrophic thoughts related to withdrawal, relapse fears, and emotional instability.
-
Acceptance-based therapies: Focus on reducing symptom avoidance and fear-driven responses to discomfort, helping individuals tolerate temporary sensations without escalation.
-
Trauma-informed therapy: Addresses underlying trauma that may amplify withdrawal distress or emotional reliance on medication.
-
Family therapy: Educates loved ones about dependence versus addiction, builds empathy, and reduces pressure or misunderstanding during recovery.
Peer Support & Recovery Capital
-
SSRI withdrawal support groups: Provide normalization, shared experiences, and reassurance that symptoms are temporary and manageable.
-
Mental health peer communities: Offer encouragement and reduce isolation during tapering and emotional adjustment.
-
Anxiety recovery programs: Teach coping skills that replace medication-based avoidance with confidence and self-regulation.
-
Education-based support networks: Understanding the neurobiology of withdrawal often reduces fear and improves outcomes.
Holistic Supports
-
Mindfulness and nervous system regulation: Practices such as breathing exercises, grounding techniques, and gentle meditation help stabilize autonomic responses.
-
Gentle exercise and movement: Walking, stretching, or yoga can support mood regulation without overstimulating the nervous system.
-
Sleep routine stabilization: Consistent sleep-wake schedules improve emotional resilience during tapering.
-
Anti-inflammatory and balanced nutrition: Stable blood sugar and adequate nutrients support brain recovery and energy levels.
-
Stress-reduction techniques: Limiting overstimulation, managing workloads, and building predictable routines reduce withdrawal-related distress.
Withdrawal Timeline (What to Expect)
Acute Phase (Days 1–14)
-
Dizziness and balance issues, especially when standing or moving quickly
-
“Brain zaps” or electric shock–like sensations in the head
-
Increased anxiety, restlessness, or sudden mood swings
-
Irritability, agitation, or emotional instability
-
Sleep disturbances, including insomnia, vivid dreams, or frequent waking
-
Flu-like symptoms such as headaches, nausea, chills, muscle aches, and fatigue
-
Difficulty concentrating or feeling mentally foggy
Protracted Phase (Weeks 3–12+)
-
Gradual stabilization of mood and nervous system function
-
Lingering emotional sensitivity or heightened stress response
-
Slow but steady improvement in sleep quality and sleep cycles
-
Improved cognition, including focus, memory, and mental clarity
-
Reduced frequency and intensity of withdrawal-related physical symptoms
-
Return of a more natural emotional range, including motivation and enjoyment
-
Occasional symptom “waves,” followed by longer periods of relief
Important Note
-
Paxil withdrawal is not dangerous, but it can be uncomfortable and disruptive
-
Symptoms are more manageable with a slow, supervised taper
-
Medical guidance and emotional support significantly improve recovery outcomes
When to Seek Immediate Help?
-
Severe or worsening depression that interferes with daily functioning
-
Thoughts of self-harm or suicide, or feelings of hopelessness or despair
-
Intense anxiety, panic attacks, or agitation that feels unmanageable
-
Confusion, disorientation, or significant cognitive changes
-
Persistent vomiting, dehydration, or inability to keep food or fluids down
-
Severe insomnia lasting several days and causing extreme exhaustion
-
Uncontrolled mood swings, aggression, or impulsive behavior
-
Neurological symptoms such as seizures, fainting, or loss of consciousness
-
Any withdrawal symptom that feels overwhelming, frightening, or rapidly worsening
Dosing & Safety / Overdose Risks (For Legit Prescribing)
Typical Therapeutic Ranges & Formulations
-
Starting dose: 10–20 mg once daily (usually taken in the morning)
-
Common therapeutic range: 20–40 mg per day
-
Maximum dose: up to 50–60 mg/day (indication-dependent)
-
Formulations:
-
Immediate-release tablets
-
Controlled-release (Paxil CR)
-
Oral suspension
Dosing is individualized based on diagnosis, age, tolerability, and response.
High-Risk Combinations
-
Alcohol: increases sedation, dizziness, impaired judgment, and accident risk
-
Benzodiazepines: additive CNS depression, increased fall and overdose risk
-
Other sedatives or sleep medications: enhanced drowsiness and cognitive impairment
-
MAOIs, triptans, St. John’s wort, other SSRIs/SNRIs: increased risk of serotonin syndrome
Overdose Risks & Mechanism
-
Paxil overdose is rarely fatal when taken alone, but the risk increases with other substances
-
Overdose may cause:
-
Severe nausea and vomiting
-
Tremor, agitation, confusion
-
Rapid heart rate and blood pressure changes
-
Seizures or serotonin syndrome in severe cases
-
Naloxone does NOT reverse Paxil overdose (it only works for opioids)
-
Emergency care focuses on supportive treatment and monitoring
Safe Use Guidelines
-
Take exactly as prescribed; do not stop or change dose abruptly
-
Store medication securely and out of reach of children
-
Never share Paxil with others
-
Dispose of unused medication through pharmacy take-back programs
-
Report worsening mood, suicidal thoughts, or unusual side effects promptly
Conclusion
Paxil can be life-saving when used appropriately—but long-term reliance without reassessment can lead to dependence-like patterns.
It isn’t addictive in the classical sense, yet stopping without preparation can be challenging.
With informed tapering, emotional support, and comprehensive care, most people regain stability and confidence without overreliance on medication.
Next Steps:
-
Talk to your provider before changing your dose
-
Plan a gradual, supported taper
-
Address emotional and psychological factors
-
Involve family or support systems
Recovery isn’t about rejecting medication—it’s about regaining autonomy, balance, and emotional resilience.
FAQs
No. Paxil does not cause intoxication, cravings, or compulsive drug-seeking behavior. However, long-term use can lead to physical dependence, meaning the body adapts to the medication. Stopping suddenly may trigger withdrawal symptoms, which is why medical tapering is recommended.
Paxil has a short half-life, so it leaves the body quickly. This can cause abrupt serotonin changes, leading to more intense discontinuation symptoms. Other SSRIs with longer half-lives tend to produce milder, slower withdrawal effects.
Tapering timelines vary from several weeks to several months. The dose, length of use, and individual sensitivity all affect how slowly Paxil should be reduced. A gradual taper lowers withdrawal severity and supports nervous system stability.
In many cases, therapy can be an effective alternative, especially for mild to moderate conditions. Therapy helps build coping skills, emotional regulation, and relapse prevention strategies. It is often most effective when combined with a slow, supervised taper.
Families can support recovery by being patient and avoiding pressure to stop medication quickly. Providing emotional reassurance during withdrawal symptoms can reduce distress. Encouraging professional guidance and consistent therapy improves long-term outcomes.







