Paxil Withdrawal: How To Stop Taking Paroxetine Safely?
Paxil (paroxetine) is a selective serotonin reuptake inhibitor (SSRI) used to treat depression, anxiety disorders, panic disorder, PTSD, and related conditions. It works by increasing the availability of serotonin, a neurotransmitter involved in mood regulation, emotional balance, sleep, and stress response.
Key Takeaways
-
Paxil (paroxetine) withdrawal is a real but temporary process as the brain adjusts to lower medication levels. Because Paxil leaves the body quickly, symptoms may feel intense at first, but they usually ease with time.
-
The safest way to stop is through a slow, medically supervised taper, as stopping suddenly can worsen withdrawal and emotional instability.
-
Recovery is smoother with medical guidance, stable routines, healthy sleep, balanced nutrition, gentle activity, and emotional support.
What Happens When You Stop Taking Paxil?
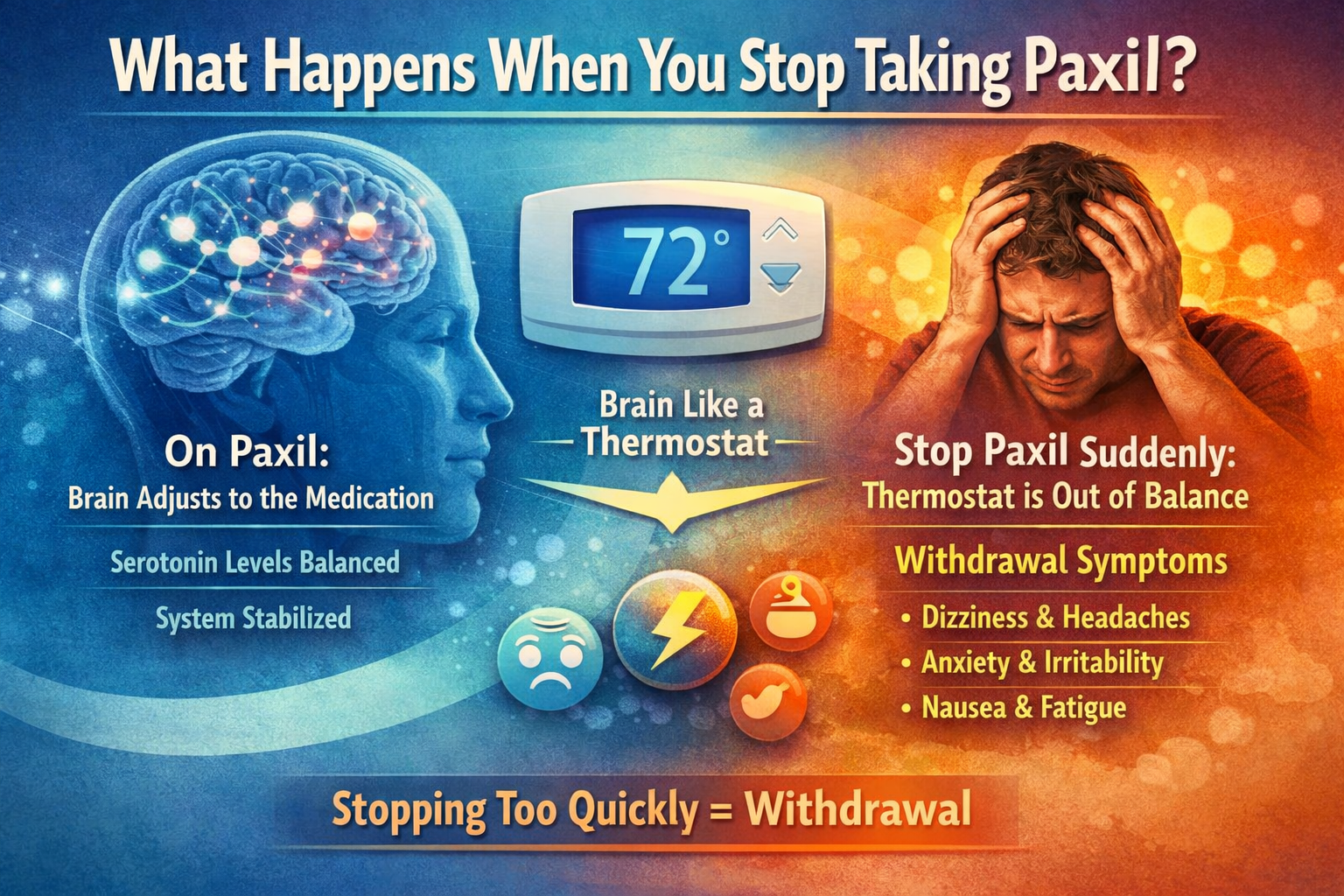
When someone takes Paxil consistently, the brain adapts to its presence. Serotonin receptors adjust their sensitivity, signaling pathways recalibrate, and the nervous system learns to function with the medication in place. This adaptation is gradual and automatic.
A helpful way to think about this process is like a thermostat. Over time, the brain resets its internal “temperature” to match the medication’s effects.
When Paxil is reduced too quickly—or stopped suddenly—the thermostat hasn’t had time to catch up. The result is withdrawal.
Why Does Paxil Withdrawal Happen?
Paxil has one of the shortest half-lives among SSRIs, meaning it leaves the body faster than medications like fluoxetine (Prozac). This rapid drop can stress the nervous system.
When Paxil levels fall abruptly, several changes occur at once:
-
Serotonin signaling drops, contributing to anxiety, low mood, and emotional sensitivity
-
Autonomic nervous system regulation fluctuates, affecting sleep, digestion, heart rate, and temperature
-
Sensory processing becomes unstable, leading to dizziness or “brain zaps” [1]
This cluster of effects is known as antidepressant discontinuation syndrome. It is well-documented and reflects physiological adjustment—not psychological dependence.
Withdrawal Is NOT Addiction
Families often worry that withdrawal symptoms mean their loved one is “dependent” or addicted. This is a common misconception.
Paxil withdrawal is not addiction:
-
There are no cravings
-
There is no compulsive drug-seeking
-
There is no loss of control over use
Withdrawal reflects the brain rebalancing after long-term serotonin modulation. It is a biological readjustment, not a behavioral disorder.
Withdrawal vs. Relapse: Why the Difference Matters?
One of the most distressing aspects of Paxil withdrawal is that symptoms can resemble returning anxiety or depression. [2]
Key differences help clinicians tell them apart:
Withdrawal
-
Begins within days to weeks of dose reduction
-
Includes physical and sensory symptoms
-
Fluctuates and improves over time
Relapse
-
Develops gradually over weeks to months
-
Is primarily emotional and cognitive
-
Does not steadily improve without treatment changes
Common Paxil Withdrawal Symptoms
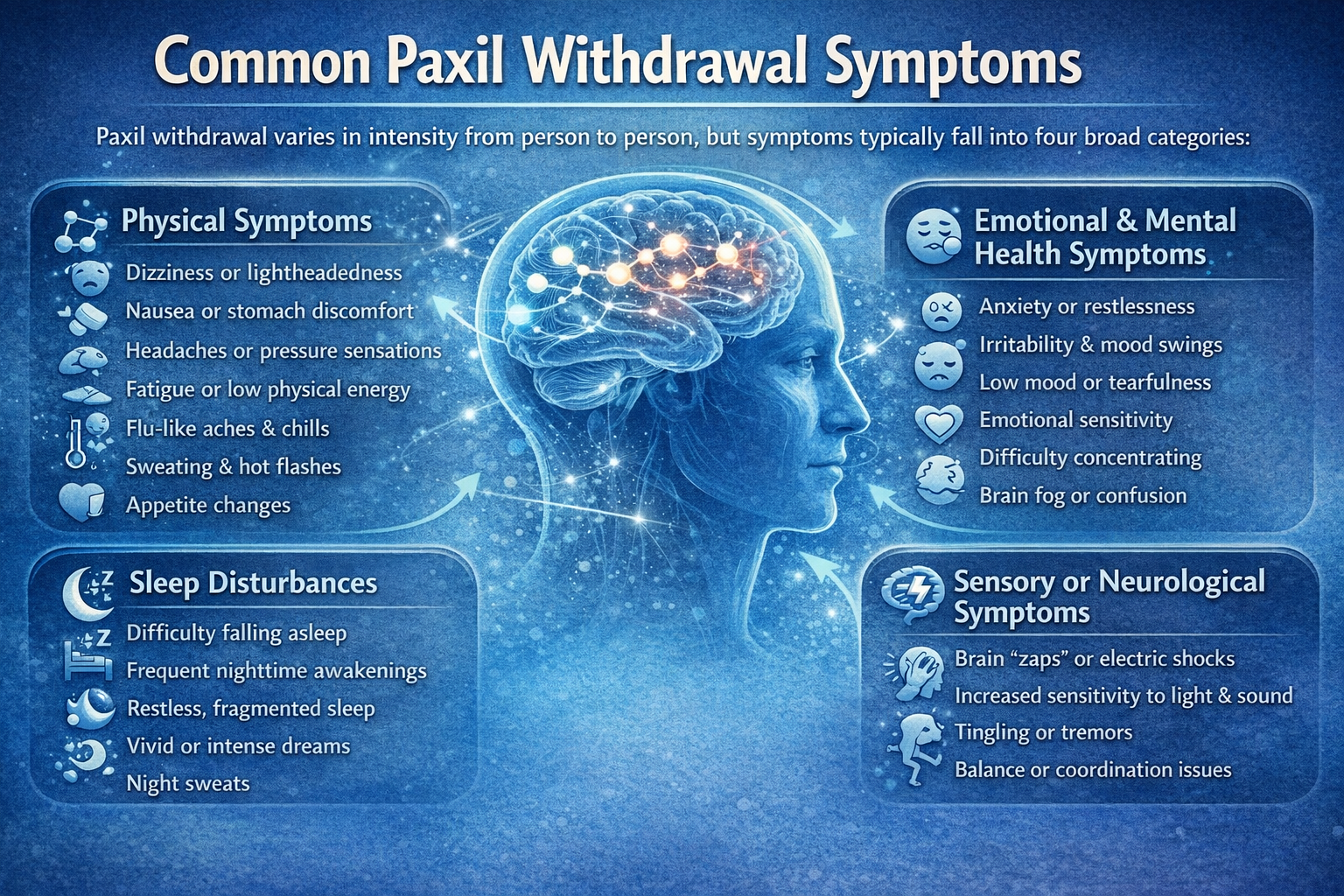
Paxil withdrawal varies in intensity from person to person, but symptoms typically fall into four broad categories. Each category reflects specific neurochemical adjustments taking place as serotonin signaling gradually rebalances during tapering.
While these symptoms can feel distressing, they are a known and temporary part of the withdrawal process.
Physical Symptoms
Because Paxil affects serotonin receptors throughout the body—not just in the brain—physical symptoms often appear early in withdrawal. These sensations can feel sudden or unfamiliar, which may increase anxiety if not anticipated.
Common physical symptoms include:
-
Dizziness or lightheadedness, especially when standing, caused by temporary blood pressure and autonomic regulation changes
-
Nausea or stomach discomfort, reflecting serotonin’s role in gut function
-
Headaches or pressure sensations, which may fluctuate throughout the day
-
Fatigue or low physical energy, even after adequate rest
-
Flu-like symptoms, including body aches, chills, or general malaise without infection
-
Sweating or temperature sensitivity, such as feeling hot or cold unexpectedly
-
Appetite changes, ranging from reduced hunger to increased cravings
-
Heart palpitations related to autonomic instability, often brief and anxiety-provoking but not dangerous
These symptoms can feel alarming, especially early on, but they are common and tend to ease as the nervous system adapts.
Sleep Disturbances
Paxil influences sleep architecture by altering serotonin pathways involved in circadian rhythm regulation.
When the dose is reduced, sleep patterns may temporarily become irregular as the brain relearns how to regulate sleep independently.
Common sleep-related symptoms include:
-
Difficulty falling asleep, despite feeling physically tired
-
Frequent nighttime awakenings, often with heightened alertness
-
Restless or fragmented sleep, leading to non-restorative rest
-
Vivid, intense, or emotionally charged dreams, sometimes remembered in detail
-
Night sweats, particularly during early withdrawal
-
Feeling wired at night but exhausted during the day, reflecting circadian disruption
The brain gradually restores natural sleep regulation. Most people notice improvement within 1–3 weeks, especially with slow tapering, consistent sleep schedules, and calming nighttime routines.
Emotional and Mental Health Symptoms
Emotional and cognitive symptoms tend to cause the most concern because they can closely resemble anxiety or depressive relapse. Understanding their timing and pattern is key to reducing fear.
Common emotional symptoms include:
-
Increased anxiety or inner restlessness, often described as nervous energy
-
Irritability or frustration, sometimes over minor stressors
-
Temporary low mood or emotional flatness, which comes and goes
-
Heightened emotional sensitivity or tearfulness, even without clear triggers
-
Mood swings, shifting rapidly throughout the day
-
Difficulty concentrating or mental fog, affecting focus and decision-making
These symptoms typically peak during weeks 1–2 and gradually soften as serotonin signaling stabilizes and the nervous system regains balance.
Sensory or Neurological Symptoms
Less common but often unsettling, sensory and neurological symptoms occur as neural signaling pathways recalibrate. Although they may feel intense, they do not indicate brain damage.
Possible symptoms include:
-
“Brain zaps” or electric shock sensations, often triggered by movement or eye shifts
-
Increased sensitivity to light or sound, making environments feel overwhelming
-
Tremors or internal shaking, especially during rest
-
Tingling sensations or restlessness, particularly in the limbs
-
Balance disturbances, sometimes described as feeling like walking on a boat
These sensations reflect temporary sensory misfiring during withdrawal and typically fade as neural communication stabilizes over time.
Paxil Withdrawal Timeline
Withdrawal unfolds in phases. While individual experiences vary, this general timeline helps families recognize expected patterns. [3]
Timelines vary based on:
-
Dose and duration of use
-
Individual sensitivity
-
Taper speed
-
Co-occurring mental health conditions
Clinicians may slow or pause tapering if symptoms become overwhelming.
Why Paxil Must Be Tapered Slowly?
Stopping Paxil abruptly places the nervous system under sudden strain. [4] Because Paxil strongly affects serotonin regulation, a rapid drop can overwhelm the brain’s adaptive capacity.
Cold turkey increases the risk of:
-
Severe withdrawal symptoms
-
Emotional destabilization
-
Sleep collapse
-
Panic-like episodes
-
ER visits driven by fear rather than danger
-
Confusion between withdrawal and relapse
Benefits of Slow Tapering
A gradual taper allows the brain to adjust in small, tolerable steps:
-
Neurotransmitters decline gradually
-
Withdrawal peaks are milder
-
Sleep disruption is reduced
-
Emotional swings are easier to manage
-
Relapse risk decreases
Families play an important role by reinforcing patience and discouraging impulsive dose changes during difficult days.
How Healthcare Providers Help During Paxil Withdrawal?
Healthcare providers play a key role in creating structure, safety, and reassurance throughout the tapering process. Their involvement helps reduce uncertainty and prevents unnecessary distress as the nervous system adjusts.
Clinicians support patients by carefully monitoring progress and responding to symptoms in a timely, informed way.
-
Monitoring symptom patterns: Providers track how symptoms appear, fluctuate, and resolve over time to identify normal withdrawal responses versus concerning changes. This pattern recognition helps guide safer taper decisions.
-
Distinguishing withdrawal from relapse: Clinicians assess timing, intensity, and symptom type to determine whether discomfort is part of withdrawal or a return of the original condition. This prevents premature conclusions and unnecessary medication changes.
-
Adjusting taper speed: Based on symptom severity and tolerance, providers may slow the taper, hold a dose longer, or make smaller reductions to allow the nervous system more time to stabilize.
-
Offering short-term symptom support if needed: When appropriate, clinicians may suggest temporary strategies or supportive treatments to ease sleep disruption, anxiety, or physical discomfort during difficult phases.
-
Tracking sleep and emotional stability: Regular assessment of sleep quality, mood, and stress tolerance helps ensure overall stability and catch issues early before they escalate.
Regular check-ins provide reassurance, reduce fear, and allow timely adjustments, helping patients move through withdrawal with greater confidence and less suffering.
What Coping Strategies Help Manage Withdrawal Symptoms?
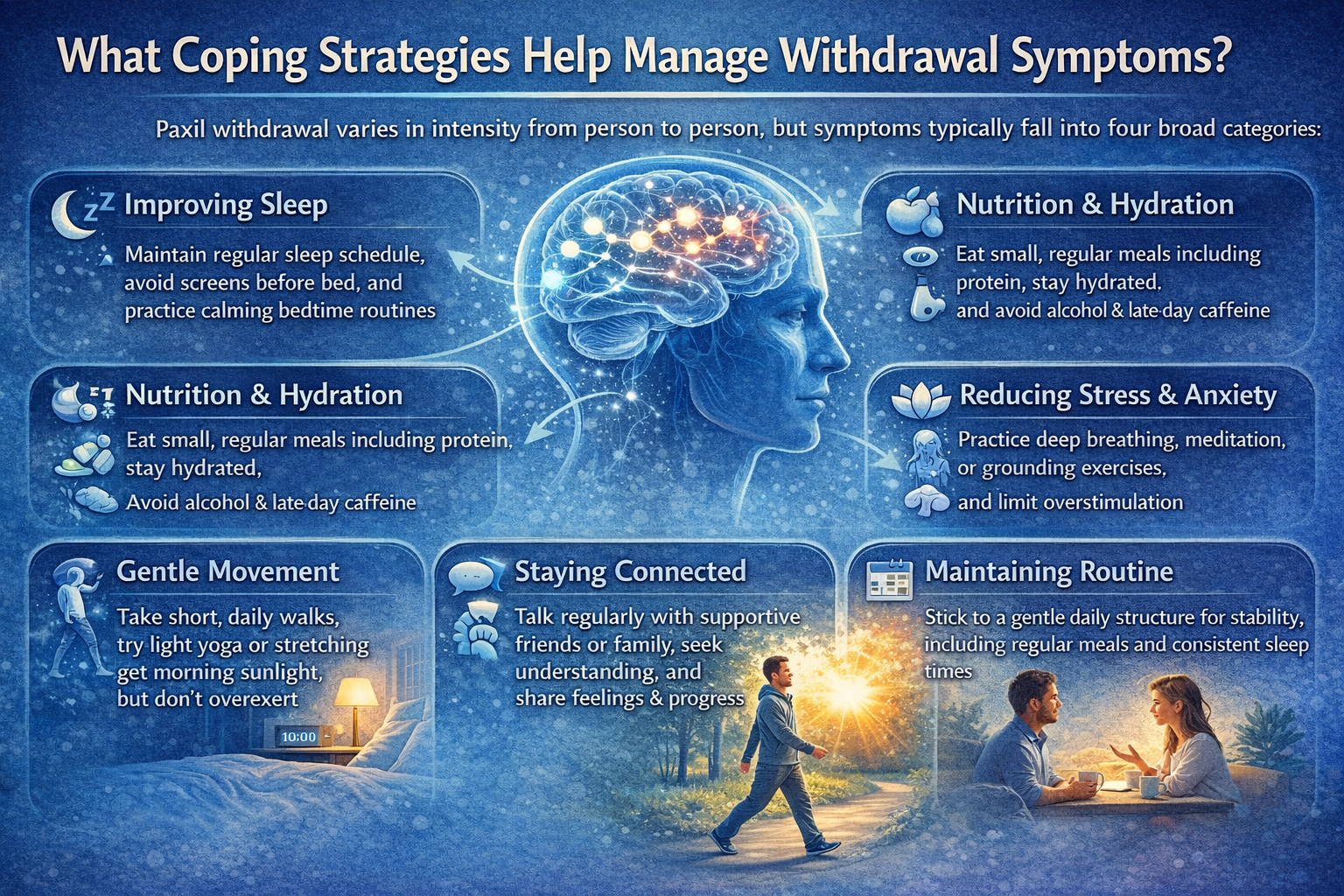
1. Improving Sleep
Sleep disruption is common during Paxil withdrawal, so focusing on gentle sleep support can make a meaningful difference. Try to go to bed and wake up at the same time each day to help reset your body clock.
Keep evenings calm and low-light, and avoid screens close to bedtime, as blue light can overstimulate the nervous system.
Gentle breathing, grounding exercises, or relaxation techniques before bed can help your body wind down. Creating a cool, dark, and quiet sleeping environment also supports deeper, more restorative rest.
2. Nutrition and Hydration
Eating and drinking consistently can help stabilize blood sugar and reduce withdrawal-related symptoms like dizziness, weakness, or anxiety. Small, frequent meals are often easier to tolerate than large ones.
Aim for balanced meals that include protein and complex carbohydrates to support steady energy and mood. Staying well hydrated is important, while alcohol and late-day caffeine are best avoided, as they can worsen sleep issues and nervous system sensitivity.
3. Gentle Movement
Light physical activity can support both mood and nervous system regulation without overwhelming your body. Short daily walks, especially outdoors, help with circulation and natural stress relief.
Gentle stretching or yoga can ease muscle tension and promote relaxation. Exposure to sunlight earlier in the day also helps regulate sleep-wake rhythms and may improve overall energy levels.
4. Reducing Stress and Anxiety
Withdrawal can heighten stress responses, so calming techniques are especially helpful. Slow breathing with a longer exhale signals safety to the nervous system and can reduce anxiety. Mindfulness practices or body scans help you stay grounded in the present moment.
Limiting overstimulation—such as excessive noise, screens, or multitasking—can prevent symptom flares. Journaling symptoms may also reduce fear by helping you track patterns and remind yourself that changes are temporary.
5. Staying Connected
Emotional support plays an important role during withdrawal. Regular check-ins with trusted friends or family members can provide reassurance and reduce feelings of isolation.
Low-pressure social contact, even brief conversations, can be comforting without feeling overwhelming. Letting family members know about symptom spikes can help them offer understanding and reassurance when you need it most.
6. Maintaining Routine
A predictable daily routine helps stabilize the nervous system by reducing uncertainty. Scheduling meals, maintaining consistent sleep times, and creating a gentle daily structure can make symptoms feel more manageable.
Regular follow-ups with a healthcare provider also provide guidance and reassurance, reinforcing that you are supported throughout the withdrawal process.
When to Seek Medical Help?
Seek immediate medical support if any of the following occur:
-
Suicidal thoughts or worsening depression
-
Severe or escalating anxiety
-
Confusion or hallucinations
-
Fainting or irregular heartbeat
-
Seizures
-
Persistent vomiting
-
Inability to sleep for several consecutive days
What Comes After Withdrawal: Long-Term Recovery
Withdrawal is not the end of healing—it is a transition phase. As the brain continues to rebalance and restore its natural rhythms, many people begin to notice meaningful improvements.
Emotional responses often feel more regulated, thinking becomes clearer, sleep patterns grow more predictable, and overall resilience to everyday stress gradually increases. These changes tend to emerge slowly, reinforcing that recovery is a process rather than an instant shift. [5]
The Role of Therapy
Therapy can play an important role in maintaining long-term stability after withdrawal. It helps individuals build practical coping skills and recognize the difference between normal emotional fluctuations and warning signs of relapse. Therapy also reduces the risk of misinterpreting temporary stress or low moods as failure, while supporting healthier lifestyle choices that protect mental well-being over time.
Long-Term Habits That Support Recovery
Sustained recovery is strengthened by consistent daily habits that support nervous system balance. Maintaining regular sleep routines, eating balanced and nourishing meals, and engaging in gentle, regular exercise all help stabilize mood and energy.
Ongoing stress-management practices and strong social connections further protect emotional health, while avoiding substances that can destabilize mood supports long-term resilience.
Family involvement remains valuable well beyond withdrawal, providing reassurance, understanding, and encouragement throughout continued healing.
Conclusion
Paxil withdrawal is temporary, manageable, and not a sign of failure. It reflects the brain and nervous system adjusting to change, not a setback or loss of progress. While symptoms can feel uncomfortable or discouraging at times, they are part of a healing transition rather than an indication that something is wrong.
With gradual tapering, proper medical supervision, and supportive daily habits, most people notice steady improvement over time. Small, consistent steps, such as protecting sleep, reducing stress, and maintaining routine, can significantly ease the process and build confidence as recovery unfolds.
Stay patient with your body, stay connected to supportive people, and never stop Paxil abruptly. Healing takes time, but it does happen. With the right guidance and self-care, you can move forward safely and regain a sense of stability, clarity, and control.
FAQs
No. Abrupt discontinuation significantly increases withdrawal severity and emotional instability. Paxil leaves the body quickly, which can shock the nervous system if stopped suddenly. A gradual, medically supervised taper is the safest approach and greatly reduces the risk of intense symptoms.
Most people improve within weeks, though full adjustment may take longer depending on taper speed and individual factors. Some symptoms can come and go in waves, which is a normal part of nervous system healing. Progress is often gradual rather than linear.
Not necessarily. Timing and symptom patterns help clinicians distinguish withdrawal from relapse. Withdrawal symptoms often feel physical and fluctuate rapidly, while relapse tends to develop more slowly. Careful monitoring during tapering helps clarify the difference.
Routine, sleep support, hydration, gentle movement, grounding techniques, and reassurance are key. Reducing stress and overstimulation can prevent symptom spikes. Consistency over time is more effective than trying many changes at once.
By staying patient, validating the experience, tracking symptoms, and encouraging medical guidance. Calm reassurance during symptom flares can significantly reduce fear. Practical support with daily tasks can also ease emotional strain.
Contact the prescriber. Slowing the taper often provides significant relief. In some cases, adjusting the dose or taper schedule can quickly stabilize symptoms and make the process more manageable.







