Pristiq Addiction Dangers and Risks of Abuse
Many people first start Pristiq after a major depressive episode, a difficult postnatal period, or when anxiety and persistent low mood begin to interfere with daily life. It can feel like a lifeline: sleep stabilizes, thoughts quieten, and routines become manageable again.

Key Takeaways
-
Pristiq (desvenlafaxine) treats major depression and does not create a drug “high,” so it isn’t considered addictive.
-
People can still face issues like discontinuation symptoms if they stop too fast. These can feel physical or emotional.
-
Pristiq is known for having a higher chance of withdrawal symptoms, so doctors recommend slow, supervised tapering.
-
Misuse usually happens when someone tries to feel stable or manage anxiety, not to get high. Mixing Pristiq with alcohol or other mood-related drugs can be dangerous.
-
With proper guidance, most people can stop Pristiq safely by tapering slowly and getting the right mental-health support.
But as weeks and months pass, confusion sometimes sets in. Patients say things like “I can’t imagine getting through my day without it,” or “what if my depression comes back if I stop?” These are understandable reactions — not proof of classic addiction — yet they can lead to patterns of overreliance that cause harm.
This article explains what “Pristiq addiction” really means, how risk arises, what to watch for, and how clinicians and families can help people stop safely when it’s appropriate.
What Is Pristiq Addiction?
Pristiq (desvenlafaxine) is an SNRI antidepressant used to treat major depressive disorder. It does not produce a “high,” so it isn’t considered addictive in the traditional sense.
However, people can still experience dependence-like issues, especially if they stop the medication too quickly.
-
Tolerance: Some people may feel like Pristiq becomes less effective over time, leading them to think they need a higher dose for the same mood-stabilizing effect.
-
Dependence: The body can become used to Pristiq. If someone suddenly stops taking it, they may develop withdrawal symptoms, also known as discontinuation syndrome (dizziness, irritability, flu-like feelings, mood swings).
-
Addiction: Traditional addiction (cravings, compulsive use, seeking a high) is not typical with Pristiq. However, some people may feel psychologically dependent — for example, relying on the medication to feel emotionally stable or avoid rebound symptoms.
Signs & Symptoms Of Pristiq Misuse
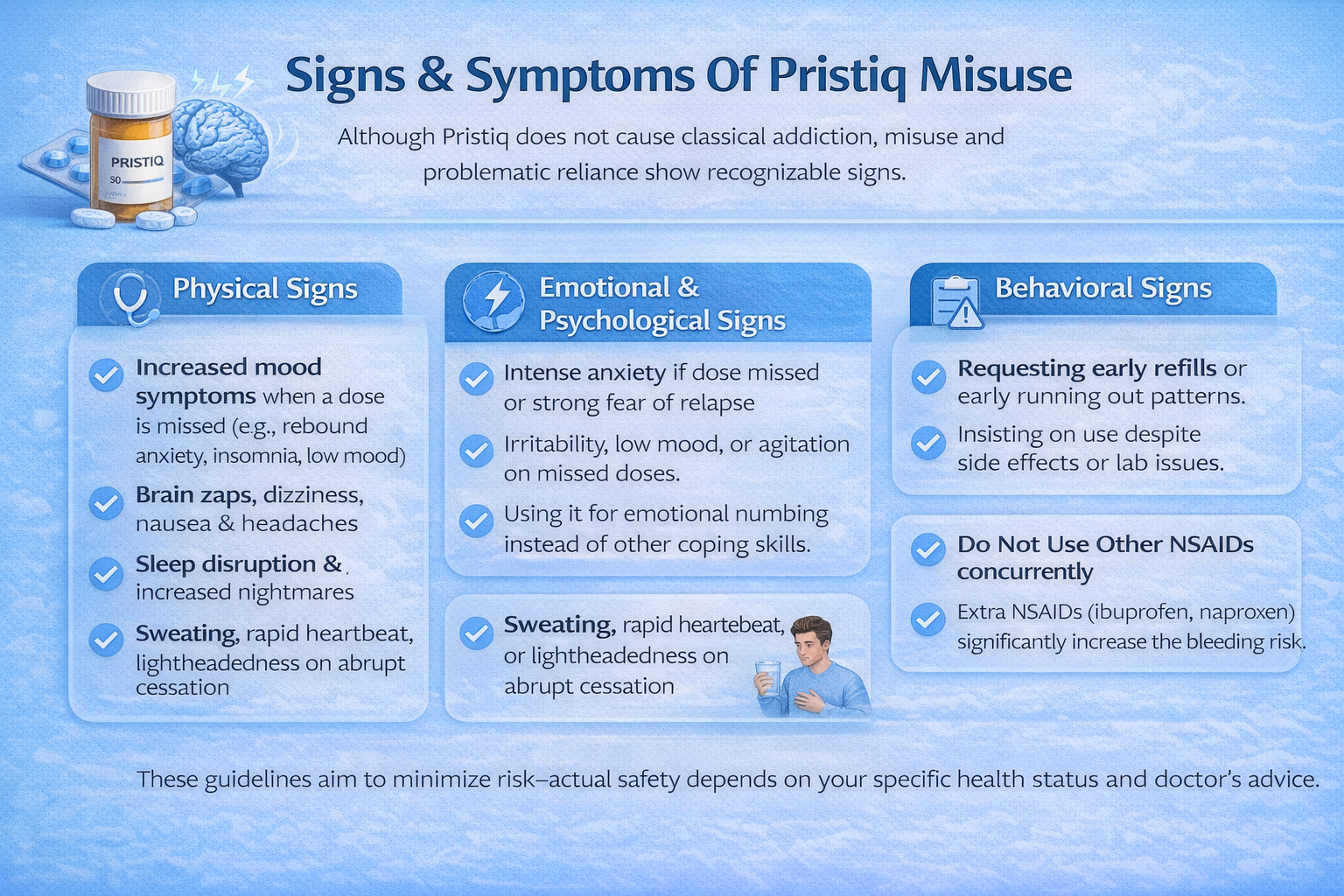
Although Pristiq does not cause classical addiction, misuse, and problematic reliance show recognizable signs.
Physical Signs
-
Rebound or worsening mood symptoms when doses are missed (rapid return of anxiety, insomnia, or low mood). This can be rebound illness or discontinuation-related.
-
Dizziness, “brain zaps,” paresthesias (electric shock–like sensations), nausea, vomiting, headaches — common discontinuation symptoms.
-
Sleep disruption — increased nightmares or insomnia when dosing changes.
-
Autonomic symptoms — sweating, lightheadedness, tachycardia in some individuals during abrupt cessation.
Emotional And Psychological Signs
-
Intense anxiety about missing a dose or strong fear of relapse; constant checking of medication supply.
-
Low mood, irritability, or agitation that emerges when the medication is reduced.
-
Over-reliance on medication for emotional regulation — using Pristiq instead of addressing coping skills, therapy, or lifestyle changes.
Behavioral Signs
-
Requesting early refills or reporting lost/stolen prescriptions in patterns that suggest running out early.
-
Insisting on continuing a prescription against medical advice after side effects or lab abnormalities emerge.
-
Combining Pristiq with other serotonergic agents or recreational drugs without medical oversight (dangerous — increases risk of serotonin syndrome).
How Common Is Problematic Pristiq Use?
General Prevalence
Antidepressant withdrawal is more common than many people expect. Recent research shows that around 15% of people who stop antidepressants experience some level of discontinuation symptoms. [1] These symptoms can range from mild dizziness and headaches to emotional changes like irritability or anxiety.
This number includes all antidepressants, but it helps set the stage: withdrawal-type reactions are not rare, and Pristiq fits within this larger pattern.
Clinical Settings
In real-world clinical practice, certain groups are more likely to struggle when stopping Pristiq.
Studies show that SNRIs, including desvenlafaxine, tend to cause more frequent and more intense withdrawal symptoms than many SSRIs. [2]
People at higher risk include:
-
Those taking Pristiq for a long period of time
-
Those who stop suddenly instead of tapering
-
Patients using SNRIs with a shorter half-life — research shows desvenlafaxine withdrawal symptoms occur in approximately 17.2% to 55% of users [2]
-
Patients using other serotonergic medications
-
People with a history of sensitivity to medication changes
Because of this, doctors usually treat Pristiq tapers carefully and check in more often with patients who are stopping or reducing their dose.
Withdrawal Frequency
A large meta-analysis of 79 studies, including over 21,000 patients, found that 31% of people who stop antidepressants report at least one discontinuation symptom. Of these, about 15% of symptoms are likely directly caused by stopping the medication rather than other factors. [3]
For severe symptoms, roughly 3% of people who stop taking antidepressants experience effects strong enough to disrupt daily life. Desvenlafaxine (Pristiq) was identified as one of the antidepressants associated with a higher risk of severe discontinuation symptoms.
Some of the most common symptoms reported in the analysis included:
-
Dizziness
-
Headache
-
Nausea
-
Insomnia or sleep trouble
-
Irritability or nervousness
This data shows that withdrawal-like or discontinuation symptoms are relatively common for antidepressants — including Pristiq — but most people do not experience extreme effects. Still, gradual tapering and medical supervision are essential to minimize discomfort and prevent complications.
Causes: Why Does Pristiq Addiction Happen?
How Pristiq Affects the Brain?
Pristiq works by increasing serotonin and norepinephrine levels in the brain — chemicals that regulate mood, stress response, and emotional stability.
For many people, the first noticeable shift is a sense of emotional leveling: fewer dips, less reactivity, and a smoother overall mood.
That emotional steadiness can feel deeply rewarding. Even though Pristiq doesn’t cause intoxication, the brain still interprets relief from sadness, anxiety, or rumination as a reward. This activates parts of the dopamine-based motivation system, subtly reinforcing continued use.
Over time, the brain adapts to these steady serotonin–norepinephrine levels. When Pristiq use is interrupted, the sudden drop can trigger withdrawal symptoms — dizziness, irritability, “electric shock” sensations — which makes the brain crave stabilization again.
Repeated cycles of relief → withdrawal → reinstatement can create a powerful psychological dependence, even when the medication is taken exactly as prescribed.
Studies show that SNRIs like desvenlafaxine are among the antidepressants most associated with discontinuation symptoms, especially after long-term or high-dose use — making consistent reliance more likely.
Genetic & Biological Factors
Biology plays a meaningful role in how strongly someone depends on mood-regulating medications. Antidepressant response and metabolism are 30–50% heritable, meaning family patterns of depression, anxiety, or medication sensitivity can influence vulnerability.
People with naturally lower baseline serotonin or norepinephrine levels may feel “normal” only while on Pristiq, making the idea of stopping feel threatening.
Co-occurring mental health conditions — such as generalized anxiety, panic disorder, PTSD, or chronic stress dysregulation — raise the likelihood of becoming emotionally reliant on their stabilizing effects.
Metabolic differences also matter. Some individuals metabolize desvenlafaxine more slowly, causing stronger effects and more intense withdrawal when doses fluctuate. Others clear the drug quickly, leading to “crash” sensations between doses that mimic dependency patterns.
Age, hormone fluctuations, and chronic health issues (thyroid imbalance, chronic pain, fatigue syndromes) further increase sensitivity to discontinuation, reinforcing long-term reliance.
Psychological & Emotional Triggers
Many people turn to Pristiq not only for depression symptoms but for emotional overwhelm, overthinking, or difficulty managing stress. When Pristiq reduces these burdens, it can become more than a treatment — it becomes a psychological anchor.
The pattern often looks like this:
Stress or emotional pain → dose brings relief → brain associates the medication with safety.
For individuals who fear their symptoms returning, each pill becomes a reassurance. Pristiq may start functioning as a coping mechanism rather than a therapeutic tool.
Longstanding emotional wounds — trauma, loneliness, burnout, perfectionism, or unstable relationships — can magnify this cycle. When daily functioning feels fragile, the emotional quieting that Pristiq provides feels essential.
Over time, stopping the medication can feel risky, not because of addiction, but because the person fears losing their emotional balance.
Environmental & Social Factors
Life context heavily shapes how Pristiq is used.
-
Easy access and long-term prescribing make SNRIs simple to continue indefinitely without dose reassessment.
-
Limited education about withdrawal symptoms can lead people to mistake discontinuation for relapse, prompting long-term reliance.
-
Work pressure, caregiving roles, or financial stress push individuals to manage symptoms quickly rather than explore therapy or lifestyle options.
-
Isolation or lack of support can make medication feel like the only reliable emotional stabilizer.
-
Cultural norms around productivity sometimes reinforce the idea that “as long as I'm functional, I should stay on my meds,” discouraging careful tapering.
From Treatment to Dependence (Progression)
-
Diagnosis: Depression, anxiety, or stress-driven symptoms lead to a Pristiq prescription. Early improvements bring relief and renewed stability.
-
Emotional reliance: As mood levels out, the person begins associating Pristiq with safety, confidence, and the ability to function.
-
Adaptation: Over months, the brain adjusts to the medication’s chemical balance. Missing even one dose may trigger discontinuation symptoms — dizziness, sensitivity, irritability — creating a fear of skipping doses.
-
Heightened vigilance: The individual starts closely monitoring timing, carries extra pills “just in case,” or becomes anxious about running out.
-
Withdrawal avoidance: Attempts to taper lead to uncomfortable symptoms, often mistaken for a relapse. This reinforces the belief that the medication is indispensable.
-
Dependence pattern: The person continues using Pristiq not to feel “better,” but to avoid destabilization. The fear of withdrawal or emotional regression solidifies psychological dependence — even though Pristiq is not addictive in the classical, intoxicating sense.
Who Is Most At Risk?
Certain groups are more vulnerable to problematic reliance or severe discontinuation symptoms:
-
People with long-standing depression or recurrent episodes who fear relapse.
-
Those taking higher doses or who have been on treatment for months to years without review.
-
Patients with co-occurring anxiety disorders, insomnia, or trauma histories, for whom symptom relief is closely tied to medication stability.
-
Older adults and people with medical comorbidities (renal, hepatic impairment) — because side effects and interactions complicate management. [4]
-
Individuals with limited access to psychotherapy or social supports, who rely on medication as a primary coping tool.
Side Effects of Pristiq Addiction
Short-Term Effects
-
Acute discontinuation symptoms: dizziness, nausea, vomiting, headache, irritability, paresthesia, insomnia — can cause functional impairment and distress.
-
Serotonin syndrome, if combined inappropriately with other serotonergic drugs, can be a potentially life-threatening emergency (agitation, hyperthermia, autonomic instability, rigidity).
-
Return of underlying depression or anxiety, sometimes indistinguishable from withdrawal, risking self-harm or suicide in vulnerable individuals. FDA warnings emphasize monitoring for worsening mood and suicidality, especially early in treatment and in younger adults. [5]
Long-Term Effects
-
Prolonged or protracted withdrawal: A small but significant subset of patients may experience lingering discontinuation symptoms that stretch on for weeks or even months. [6] These symptoms — emotional volatility, sensory disturbances, or cognitive fog — can persist long after the drug has left the bloodstream, making recovery feel unpredictable and discouraging.
-
Risky self-medication behaviors: When withdrawal becomes overwhelming, some individuals attempt to blunt the discomfort with alcohol, sedatives, or other substances. This can trigger serious medical complications, such as heightened sedation, dangerous drug interactions, liver strain, or, in severe cases, overdose — especially when alcohol is combined with CNS-affecting medications.
-
Functional and social disruption: Repeated mood crashes, unplanned medical consults, or abrupt medication stops can erode daily functioning. People may struggle with work performance, family responsibilities, or social connections. Over time, this instability can create a cycle of avoidance, shame, or relationship strain tied directly to unmanaged withdrawal episodes.
Impact On Daily Life
Even when not life-threatening, the pattern of reliance and the experience of discontinuation can disrupt work, relationships, and daily activities:
-
Reduced work productivity from dizziness, insomnia, or cognitive slowing during withdrawal.
-
Social withdrawal and irritability that strain family relationships.
-
Increased healthcare utilization — emergency visits for severe discontinuation or interactions, repeated medical appointments, repeated prescriptions.
-
Financial strain if multiple treatment changes, therapy, or hospital care are needed.
Treatment Options
Treatment focuses on stabilizing mood, reducing withdrawal symptoms, and building non-drug coping skills.
Medical Management And Tapering
-
Planned, individualized tapering is the first-line approach. Tapers can be linear (reduce dose by a fixed amount every 1–2 weeks) or hyperbolic (small proportional reductions, especially near low doses), depending on risk. Recent expert guidance emphasizes longer tapers for higher-risk patients — sometimes spanning months.
-
Symptomatic treatments: short-term use of antiemetics, sleep aids (brief), or non-addictive anxiolytics may ease acute distress during taper. Use cautiously and under supervision.
-
Switching strategies: in some cases, transitioning to a longer-half-life antidepressant (e.g., fluoxetine) before tapering can reduce discontinuation symptoms — though this is individualized and not always preferred. Discuss risks/benefits with a prescriber.
Medication-Assisted Approaches
-
Unlike opioid use disorder, there is no standard “medication-assisted treatment” (MAT) for antidepressant dependence. However, adjunctive medications (antidepressants with different mechanisms, certain anticonvulsants, or low-dose atypical antipsychotics) may be used to treat persistent depressive symptoms or specific syndromes under psychiatric oversight.
Levels of Care (Matching Support to Severity)
Different patients need different intensities of care:
Inpatient or Residential Treatment (30–90 days)
Best for individuals with:
-
Co-occurring severe psychiatric symptoms
-
Safety concerns (suicidality, self-harm, severe instability)
-
Failed outpatient tapers
Provides structure, medication oversight, intensive therapy, and a controlled environment.
Outpatient / IOP (Intensive Outpatient Program)
Therapy several times per week with psychiatric monitoring. Ideal for:
-
Significant withdrawal distress
-
Co-occurring anxiety or depressive relapse
-
Need for structured support without full hospitalization
Standard Outpatient Care
Most patients discontinue Pristiq safely with:
-
Regular prescriber appointments
-
Weekly or biweekly therapy
-
Gradual tapering
Psychosocial Therapies
-
Cognitive Behavioral Therapy (CBT) helps reframe catastrophic thinking about relapse and trains behavioral activation. CBT is effective both for acute depressive symptoms and for relapse prevention.
-
Acceptance and Commitment Therapy (ACT) or Mindfulness-Based Cognitive Therapy (MBCT) builds distress tolerance and reduces safety-seeking behaviors (like reliance on medication for non-medical reasons).
-
Motivational Interviewing (MI) can help patients explore ambivalence about stopping and strengthen commitment to a taper plan.
-
Family therapy can help relatives support tapering without enabling safety behaviors.
Peer Support & Recovery Capital
Peer-based support reduces isolation and normalizes the discontinuation experience.
-
Online and local groups for antidepressant withdrawal
-
Chronic illness or mental health support networks
-
Recovery groups (NA alternatives for medication issues)
-
Skills-sharing communities with practical taper experiences
Holistic & Lifestyle Supports (Adjunct Tools That Matter)
Non-drug strategies can significantly reduce withdrawal intensity and improve resilience.
-
Mindfulness and breathwork: Reduce anxiety spikes and emotional reactivity.
-
Regular exercise: Stabilizes mood, improves sleep, and supports neurochemical balance.
-
Sleep hygiene practices: Counteract withdrawal-related insomnia.
-
Nutrition: Anti-inflammatory, steady-glycemic diets support energy and mood stability.
-
Stress management: Yoga, grounding techniques, and structured routines help reduce symptom sensitivity.
These approaches enhance the brain’s natural ability to regulate itself during and after tapering.
Withdrawal Timeline
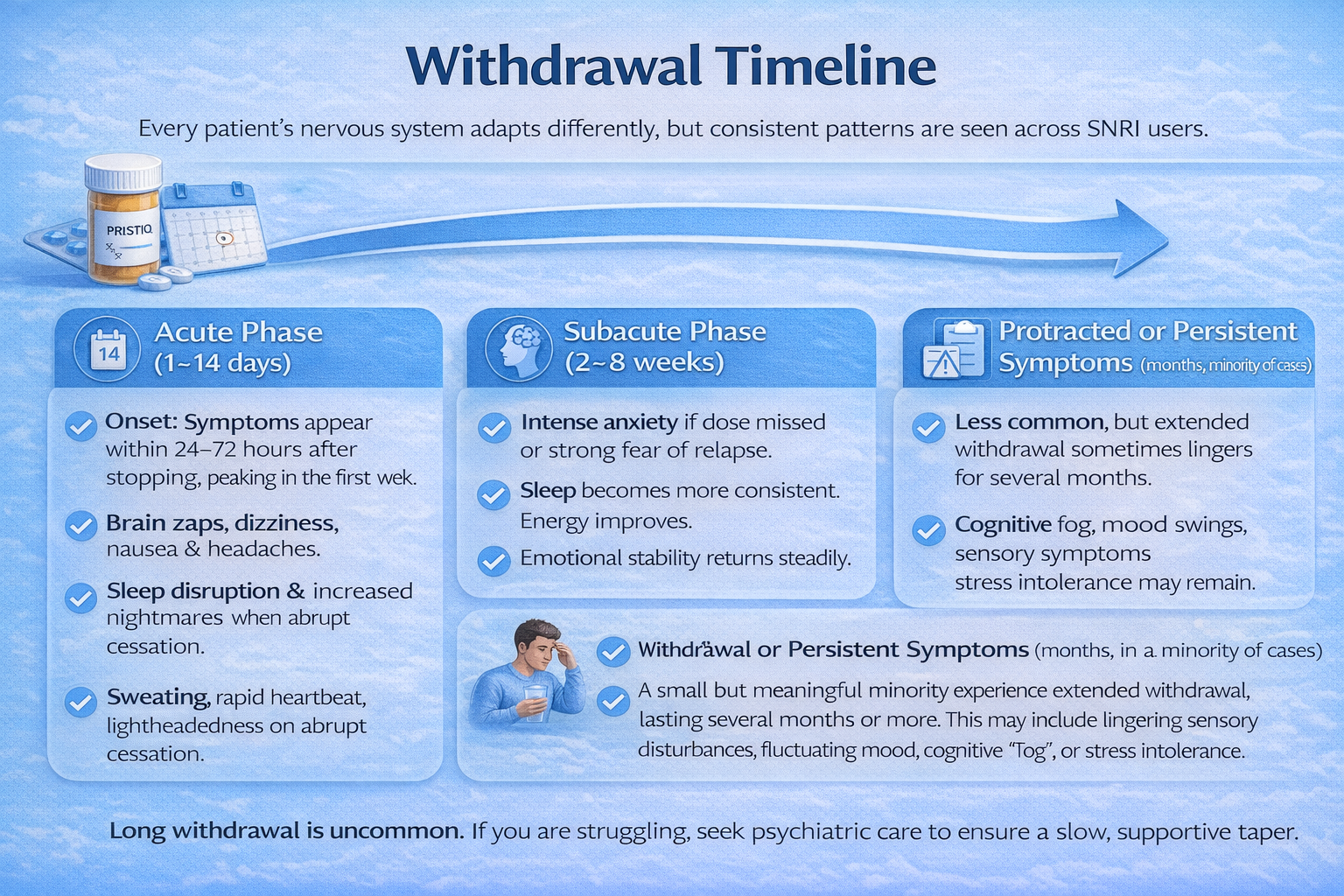
Every patient’s nervous system adapts differently, but consistent patterns are seen across SNRI users.
Acute Phase (first 1–14 days after dose reduction or cessation)
-
Onset: Symptoms typically appear within 24–72 hours for short–half-life medications. Because desvenlafaxine leaves the system relatively quickly, abrupt cessation often triggers rapid, early-onset withdrawal.
-
Common symptoms: Patients may experience dizziness, nausea, headaches, “electric shock” sensations, vivid dreams or nightmares, irritability, anxiety spikes, and temporary mood worsening.
These symptoms tend to peak during the first week, especially if the taper was too fast.
Subacute Phase (2–8 weeks)
-
Many people begin to re-stabilize as the brain recalibrates its serotonin and norepinephrine regulation.
-
Discontinuation effects gradually diminish: sleep becomes more consistent, energy begins to improve, and emotional reactivity settles.
-
For most patients, this phase marks a steady return to baseline functioning — though sensitivity to stress may temporarily remain higher.
Protracted or Persistent Symptoms (months, in a minority of cases)
-
A small but meaningful minority experience extended withdrawal, lasting several months or more. This may include lingering sensory disturbances, fluctuating mood, cognitive “fog,” or stress intolerance.
-
While uncommon, these long-duration symptoms are clinically significant, and recent reviews identify desvenlafaxine as one of the SNRIs with a relatively higher likelihood of prolonged discontinuation effects.
-
In such cases, specialty psychiatric guidance is recommended — often involving micro-tapering strategies or temporary reinstatement with a slower taper.
When To Seek Immediate Help?
Seek urgent medical attention if any of the following occur:
-
Severe suicidal ideation or self-harm behaviors (call emergency services or a crisis line immediately).
-
Signs of serotonin syndrome: high fever, severe agitation or delirium, muscle rigidity, rapid heart rate, unstable blood pressure — particularly if starting or combining serotonergic drugs.
-
Severe dehydration, vomiting, or inability to keep fluids down.
-
Protracted, disabling neurological symptoms (severe persistent vertigo, profound gait instability, or sensory loss) — urgent neurologic/psychiatric review is warranted.
Dosing, Safety, And Overdose Risks
-
Typical therapeutic dosing: Pristiq is commonly prescribed as 50 mg once daily, with 50–100 mg used in some cases; maximum recommended dosing is noted on the product label — always follow prescriber guidance.
-
Do not combine with MAOIs, certain triptans, or other serotonergic agents without consulting a prescriber. Combining increases the risk of serotonin syndrome.
-
Overdose: desvenlafaxine alone is seldom fatal in typical overdoses, but toxicity can occur, especially when combined with alcohol, tricyclics, or other CNS-active medications. Treatment is supportive; seek emergency care in overdoses.
-
Older adults and renal impairment: dose adjustments and close monitoring are often required; side effects (orthostatic dizziness, hyponatremia) are more likely.
Practical safety tips:
-
Keep an up-to-date medicine list and share it with all clinicians.
-
Store medications securely and avoid stockpiling multiple overlapping antidepressants.
-
Schedule regular follow-ups to reassess need and plan tapering if indicated.
Conclusion
Pristiq (desvenlafaxine) can be a life-changing medication, restoring stability and emotional clarity when people need it most. While it isn’t addictive in the traditional sense, its discontinuation symptoms can feel overwhelming — and that experience often creates understandable fear about stopping.
What matters is recognizing the distinction between safe medical dependence, emotional reliance, and true addiction, because each path requires a different kind of support.
The good news: recovery is absolutely possible, whether your goal is smoother tapering, symptom relief, or learning how to manage mood without relying on the medication long-term. With a thoughtful plan and the right team, most people can step down safely and confidently.
Next Steps: What to Do Now?
-
Act now: Reach out for a professional assessment. A clinician can determine whether symptoms reflect withdrawal, relapse, or both — and guide you to the safest next step.
-
Choose the right care level: Some people only need a structured taper; others benefit from therapy, medication adjustments, or (rarely) supervised detox. Tailoring care to what you are experiencing makes all the difference.
-
Build your support system: Stay connected. Family encouragement, peer support, and consistent follow-up visits reduce the risk of setbacks and make tapering far more manageable.
FAQs
No, Pristiq does not produce the euphoria or brain reward activation typical of opioids or benzodiazepines. However, physical dependence and psychological reliance can make stopping hard, and discontinuation symptoms can feel very distressing.
Dizziness, nausea, headaches, “brain zaps,” insomnia, irritability, and sensory disturbances are commonly reported after abrupt stopping or rapid dose reduction. Symptoms usually start within days and often improve over 1–4 weeks, though a minority experience prolonged symptoms.
There’s no one-size-fits-all answer. Tapers can range from a few weeks for low-risk patients to several months for those who have been on high doses or long durations. Recent guidance supports individualized, often slower tapers for higher-risk people. Discuss a plan with your prescriber.
Sometimes clinicians switch patients to a longer-acting antidepressant (like fluoxetine) before tapering, but this is individualized and not always necessary or advisable. The decision depends on history, side effects, and clinical judgment.
Contact your prescriber promptly. Options include pausing the taper, increasing to the previous dose, slowing the taper, or using short-term symptomatic treatments while reassessing the plan. If you have suicidal thoughts or signs of serotonin syndrome, seek emergency care immediately.
Resources
Related Articles
Treatment Centers in New Jersey










