Prozac Addiction: Symptoms, Withdrawal & Treatment
Prozac can provide meaningful relief for depression, but some people may gradually misuse it—raising doses, doubling missed doses, or taking it to feel emotionally numb.
While not physically addictive, it can create psychological dependence, making daily functioning feel impossible without the medication.

Key Takeaways
-
Prozac (fluoxetine) is not traditionally classified as an “addictive” drug, but psychological dependence, misuse, and difficult withdrawal can develop in vulnerable individuals—especially when doses are increased without guidance or stopped abruptly.
-
Dependence is not a moral failure. It reflects the interaction of brain chemistry, underlying mental health conditions, trauma history, and environmental stressors.
-
Recovery is possible. Supervised tapering, emotional regulation skills, therapy, and appropriate medication adjustments greatly improve outcomes.
Families may notice personality changes, emotional detachment, or withdrawal symptoms that resemble relapse. Understanding these warning signs and knowing how misuse develops can help guide safe treatment, withdrawal management, and support a realistic path to recovery.
What Is Prozac Addiction?
Prozac (fluoxetine) is an SSRI antidepressant approved for:
-
major depressive disorder,
-
generalized anxiety,
-
obsessive–compulsive disorder,
-
panic disorder,
-
premenstrual dysphoric disorder (PMDD),
-
bulimia nervosa.
It works by increasing serotonin availability, gradually stabilizing mood and reducing anxiety.
Tolerance
Tolerance with SSRIs is not as common as with sedatives or opioids. Still, some individuals notice that:
-
The emotional “lift” they experienced early on diminishes,
-
They need higher doses to feel stable,
-
They rely on the medication as their primary coping mechanism.
Dependence
Dependence develops when the body adapts to Prozac’s presence. When doses are reduced or stopped, the person may experience:
-
dizziness,
-
headaches,
-
flu-like sensations,
-
emotional instability,
-
anxiety spikes,
-
sleep disturbances.
Though Prozac has a long half-life (which reduces abrupt withdrawal), significant symptoms can still occur—especially after long-term or high-dose use.
Addiction
Addiction involves compulsive use despite harm.
With Prozac, addiction may present as:
-
taking excessive doses for emotional numbing or “mood boosting,”
-
inability to cut down despite wanting to stop,
-
hiding medication use,
-
continuing use despite negative consequences on mood, sleep, or functioning.
It is less about intoxication and more about compulsive emotional reliance.
Signs & Symptoms of Prozac Misuse
Physical Symptoms
While not identical to substance withdrawal, symptoms of Prozac misuse or discontinuation can manifest physically, including: [1]
-
headaches or migraines
-
nausea, gastrointestinal upset
-
dizziness or vertigo
-
increased sweating
-
insomnia or excessive sleep
-
fatigue
-
tremors
-
“brain zaps” or electrical-sensation symptoms (common in SSRI discontinuation)
-
sexual dysfunction
-
appetite changes
-
flu-like symptoms during withdrawal
Emotional and Psychological Symptoms
Prozac alters serotonin levels, which can lead to emotional dysregulation when misused or stopped abruptly. Psychological indicators include:
-
intense anxiety or agitation
-
severe mood swings
-
irritability or anger outbursts
-
emotional blunting or detachment
-
depressive crashes between doses
-
cravings for the emotional stabilization the medication provides
-
panic attacks
-
heightened sensitivity to stress
-
feelings of “not being able to function without it.
Behavioral Symptoms
Behavioral changes often provide the clearest signs of misuse:
-
Taking higher doses than prescribed
-
Stockpiling medication “just in case.”
-
Doctor shopping or requesting early refills
-
Using Prozac during periods of emotional stress rather than on a stable schedule
-
Withdrawing from family or responsibilities
-
Using the medication to cope rather than alongside therapy
-
Mixing Prozac with alcohol or other substances to influence its effect
-
Hiding pill use, counting pills obsessively, or feeling panic when doses are missed
How Common Is It? (Prevalence & Epidemiology)
General prevalence
Prozac (fluoxetine) remains one of the most commonly prescribed SSRIs, but most national surveys report antidepressant use overall rather than drug-by-drug counts.
In the United States, 2020 data show 16.5% of adults had taken prescription medication for a mental health condition in the past 12 months (which includes SSRIs like fluoxetine). [2]
Clinical settings
In clinical practice, the groups with higher antidepressant exposure (and therefore greater representation among Prozac users) include: older adults, women, and people receiving ongoing mental-health treatment or long-term maintenance therapy.
For example, antidepressant use is consistently higher in women and in middle-to-older age groups in national surveys, so these groups are more commonly represented among fluoxetine users in clinic populations. [3]
People more likely to experience problems when stopping or changing antidepressants in clinical settings include:
-
Those on long-term therapy (years).
-
Those stopping abruptly rather than tapering.
-
Patients on multiple serotonergic drugs or with prior sensitivity to dose changes.
Withdrawal frequency
A 2024 meta-analysis reported substantial rates of discontinuation symptoms overall, with estimates that can reach roughly one in three patients experiencing some discontinuation symptoms after stopping antidepressants. [4]
Where fluoxetine (Prozac) fits in?
Fluoxetine’s longer half-life generally lowers the immediate risk of discontinuation symptoms compared with SSRIs or SNRIs that have shorter half-lives (for example, paroxetine or venlafaxine/desvenlafaxine).
Several recent reviews and clinical summaries list fluoxetine among the antidepressants associated with lower discontinuation risk, though it is not zero; some people stopping fluoxetine still report symptoms, especially after long-term use or abrupt cessation. [5]
Causes: Why Does Prozac Misuse Happen?
Neurobiology: How SSRIs Affect the Brain
Prozac (fluoxetine) works by blocking the reuptake of serotonin, increasing the amount available in the synaptic space. At first, this boost changes the communication between mood-regulating circuits such as the prefrontal cortex, amygdala, and limbic pathways.
Over time, however, the brain begins to adapt. Serotonin receptors gradually adjust their sensitivity, certain receptor sites down-regulate, and secondary neurotransmitter systems—like dopamine and norepinephrine—shift to accommodate the long-term presence of elevated serotonin.
These adaptations explain why the drug can create:
-
Emotional stability and reduced reactivity when taken consistently
-
Irritability, dizziness, or emotional swings when serotonin levels drop after missed or delayed doses
-
A “shock-like” discontinuity sensation in some users during rapid changes
Long-term exposure can also shape emotional expectations. Some individuals develop psychological reinforcement, believing that Prozac is their only protective barrier against instability, depression, or emotional overwhelm. This isn’t addiction in a classic sense, but it can create dependence-like thinking and a strong fear of stopping or reducing the medication.
Genetic & Biological Factors
Biological predispositions can significantly influence how someone responds to fluoxetine. Research suggests genetics may account for 40–60% of vulnerability to mood disorders, anxiety, and substance-misuse tendencies.[6]
These inherited factors shape how the brain regulates serotonin, stress hormones, and reward pathways.
Key contributors include:
-
Family history of depression, anxiety, or mood instability, which increases SSRI responsiveness but also sensitivity to dose changes
-
A personal or family history of substance use disorder, which raises the likelihood of turning to medications for emotional regulation
-
Differences in CYP2D6 metabolism affect how quickly fluoxetine is processed and how strongly side effects or withdrawal sensations appear
-
Baseline neurotransmitter imbalances, such as low serotonin tone or impaired stress-response pathways
-
Co-existing psychiatric conditions like PTSD, OCD, chronic anxiety, or bipolar depression, which make emotional disruptions feel more threatening
These factors can create a situation where Prozac feels essential for daily functioning, raising the risk of dependence-like behaviors even when taken as prescribed.
Psychological & Emotional Triggers
Misuse or overreliance on Prozac is often driven by emotional rather than chemical factors. For many people, the medication becomes tied to a sense of safety and predictability. When life becomes overwhelming, they may increase doses on their own or take it inconsistently to manage shifting emotions.
Common psychological drivers include:
-
Seeking relief from intense stress or emotional overload
-
Using the medication for emotional blunting or numbing difficult memories
-
Avoiding uncomfortable emotions, especially when therapy is unavailable
-
Managing unresolved trauma or long-term grief
-
A deep fear of relapse, particularly in people who have had severe depressive episodes
In these situations, Prozac becomes a coping mechanism, not just a treatment tool—raising the risk for psychological dependence.
Environmental & Social Factors
Environmental pressure often shapes medication behavior. People under chronic stress or unstable conditions are more likely to self-adjust their Prozac dose, skip days, or take extra amounts to regain stability quickly.
Key external risk factors include:
-
Chronic workplace stress, high productivity demands, or burnout
-
Social isolation, which amplifies anxiety and rumination
-
Relationship conflict making emotional regulation harder
-
Financial strain, which fuels anxiety and depressive relapse fears
-
Limited access to mental-health support leads people to rely solely on medication
-
Unstable or chaotic home environments, increasing emotional volatility
In these scenarios, Prozac becomes a “control tool” people use to manage external chaos. This does not represent classic addiction, but it does increase the likelihood of dose manipulation, dependence-like patterns, and withdrawal discomfort if the medication is interrupted.
From Relief to Dependence
The path is gradual:
-
Symptoms improve
-
Emotional relief becomes a safety signal
-
Tolerance or diminished effect leads to increased dosing
-
Withdrawal emerges between doses
-
The person feels unable to function without Prozac
-
Compulsive use develops
Families often recognize this final stage before the individual does.
Who Is Most at Risk of Developing Prozac Dependence or Misuse?
Long-Term or High-Dose Users
People who take Prozac for years—especially in the 40–80 mg/day range—may experience:
-
Emotional reliance,
-
withdrawal when doses are missed,
-
and difficulty tapering after long-term use. [5]
The brain becomes accustomed to steady serotonin modulation, making changes destabilizing.
Individuals with Chronic Depression or Anxiety
Those with long-standing mood disorders may rely heavily on the medication to maintain emotional baseline functioning. The fear of relapse can encourage misuse, such as:
-
taking extra doses during triggers,
-
refusing to taper despite medical recommendations,
-
staying on high doses indefinitely.
People with Co-Occurring Substance Use Disorders
Prozac is sometimes used by individuals with SUD histories as a way to:
-
stabilize mood between substance use episodes,
-
self-medicate emotional crashes,
-
counterbalance stimulant “comedowns.”
This creates a cycle of reliance that is more psychological than pharmacological.
Trauma Survivors or Individuals with Significant Stress
Trauma increases vulnerability to both mental health challenges and medication misuse. Prozac may serve psychologically as:
-
An emotional buffer,
-
a numbing agent,
-
a stabilizer during overwhelming memories or triggers.
Socially Isolated Individuals
Isolation increases the risk of depending heavily on medication for emotional regulation, especially when lacking access to therapy, supportive relationships, or consistent medical follow-up.
Side Effects of Prozac Misuse
Short-Term Effects
Short-term misuse often amplifies common SSRI side effects:
-
Insomnia or sleep cycle disruption: overstimulation due to serotonergic effects.
-
Agitation or restlessness: sometimes mistaken for worsening anxiety.
-
Nausea, gastrointestinal upset, or diarrhea: especially when doses are raised too quickly.
-
Sweating or heat intolerance: due to serotonergic activation.
-
Mild euphoria (rare): may encourage some individuals to escalate doses.
-
Dry mouth, headaches, or dizziness: particularly common during dose changes.
-
Emotional blunting: used by some as a coping mechanism, but can worsen over time.
When these symptoms appear, individuals may increase or decrease doses without guidance, unintentionally creating a cycle of instability.
Long-Term Effects
Long-term misuse produces deeper biological and psychological impacts.
Chronic Serotonin Disruption
Consistently taking the medication outside prescribed boundaries may lead to:
-
reduced serotonin receptor sensitivity
-
emotional dysregulation
-
exaggerated withdrawal symptoms
-
periods of severe irritability or emotional numbness
The brain begins to rely heavily on external serotonin modulation rather than its own regulatory systems.
Cognitive and Memory Impacts
Individuals may experience:
-
cognitive fog
-
difficulty concentration
-
slowed processing
-
memory lapses
-
problems with decision-making
These symptoms often arise during withdrawal or after inconsistent dosing patterns.
Worsening Mood or Anxiety Over Time
Ironically, misuse can eventually worsen the conditions Prozac was intended to treat. This may manifest as:
-
rebound anxiety
-
depressive crashes
-
increased irritability
-
panic episodes
-
emotional hypersensitivity
-
episodes of dysphoria
These changes are often misinterpreted as “the illness coming back,” rather than destabilization due to irregular medication patterns.
Sexual Dysfunction
Long-term SSRI use is associated with:
-
reduced libido
-
delayed orgasm
-
erectile dysfunction
-
reduced sexual sensitivity
When doses are escalated beyond prescribed limits, these effects may intensify, contributing to interpersonal strain.
Increased Risk of Serotonin Syndrome
Misuse—especially combining Prozac with:
-
MAOIs,
-
tramadol,
-
certain anti-migraine medications,
-
recreational substances,
-
other antidepressants,
-
high amounts of alcohol—
can elevate serotonin to dangerous levels.
Symptoms include:
-
confusion or agitation
-
tremors
-
muscle rigidity
-
rapid heart rate
-
fever or sweating
-
shivering
-
diarrhea
-
seizures (in severe cases)
This condition requires immediate emergency care.
Impact on Daily Life
Prozac misuse creates a ripple effect that touches work, relationships, physical health, and self-esteem.
Work and Academic Performance
Irregular dosing and withdrawal can impair:
-
focus
-
memory
-
cognitive flexibility
-
emotional stability
-
motivation
Missed days, performance drops, or increased errors can lead to job instability or academic struggles.
Relationships and Family Dynamics
Families often misinterpret personality changes related to misuse as:
-
moodiness
-
irresponsibility
-
emotional distance
-
loss of interest
-
declining communication
Loved ones can feel confused, hurt, or helpless—especially when they believed Prozac was supposed to “fix” things.
Financial and Legal Consequences
While Prozac is not expensive, misuse sometimes leads to:
-
multiple doctor visits
-
early refill attempts
-
emergency room trips during withdrawal
-
risky behaviors due to emotional instability
These indirect effects contribute to a broader pattern of functional impairment.
Treatment Options for Prozac Addiction
Finding the right treatment for Prozac dependency is not about judgment.
It’s about rebuilding stability, protecting mental health, and guiding the body back to balance. A personalized plan works best because recovery is not “one-size-fits-all.”
The most effective approach blends medical care, psychological therapy, and social support, allowing individuals and families to move forward with clarity and hope.
Detox & Withdrawal Management
Prozac withdrawal can be uncomfortable, but it can be managed safely with the right support. Treatment may happen in an outpatient setting for stable individuals, or inpatient care if symptoms become overwhelming or safety is a concern.
Stopping Prozac “cold turkey” is not recommended. A supervised tapering plan allows the brain to adjust slowly, lowering the risk of severe mood crashes or flu-like symptoms.
During detox, clinicians may use adjunct medications to ease anxiety, nausea, sleep issues, or agitation.
Withdrawal is temporary, and with proper guidance, it becomes manageable rather than frightening.
Medication-Assisted Treatment (MAT)
(Used when Prozac misuse occurs alongside opioids or other substances)
-
Methadone: Stabilizes the brain’s opioid receptors and prevents severe cravings.
-
Buprenorphine: Reduces withdrawal symptoms while providing a “ceiling effect” that lowers overdose risk.
-
Naltrexone: Blocks the rewarding effects of opioids and alcohol, helping prevent relapse.
Levels of Care
Inpatient / Residential Treatment (30–90 days)
Provides structure, 24/7 supervision, and a safe space to stabilize.
This environment is especially helpful for complex withdrawal, co-occurring mental health issues, or limited home support.
Outpatient or Intensive Outpatient (IOP)
Allows individuals to continue work or family life while attending therapy several times per week.
Medical oversight ensures medications, mood, and withdrawal symptoms remain stable.
Each level is chosen based on safety, severity, and support at home.
Therapeutic Approaches
Therapy helps individuals understand why the dependence formed and how to break the cycle.
-
Cognitive Behavioral Therapy (CBT): Reframes negative thinking patterns and builds coping tools.
-
Motivational Interviewing (MI): Strengthens motivation for change without pressure or shame.
-
Family Therapy: Helps rebuild trust, improve communication, and strengthen the recovery environment.
These therapies teach skills for handling triggers, cravings, emotional swings, and relapse prevention.
Peer Support & Recovery Capital
Recovery grows stronger when people don’t walk it alone. Peer support groups—such as NA, SMART Recovery, or other community programs—offer connection, accountability, and shared experience.
Recovery capital includes relationships, health, routines, employment, and community resources. The more we build it, the more stable the recovery becomes.
Holistic (Adjunct) Supports
Prozac withdrawal affects both mind and body.
Holistic practices help regulate mood and rebuild resilience:
-
Gentle exercise or walking
-
Mindfulness or breathing routines
-
Consistent sleep schedule
-
Balanced nutrition to support energy and mood
These tools don’t replace medical care, but they strengthen the recovery foundation.
Withdrawal Timeline: What to Expect?
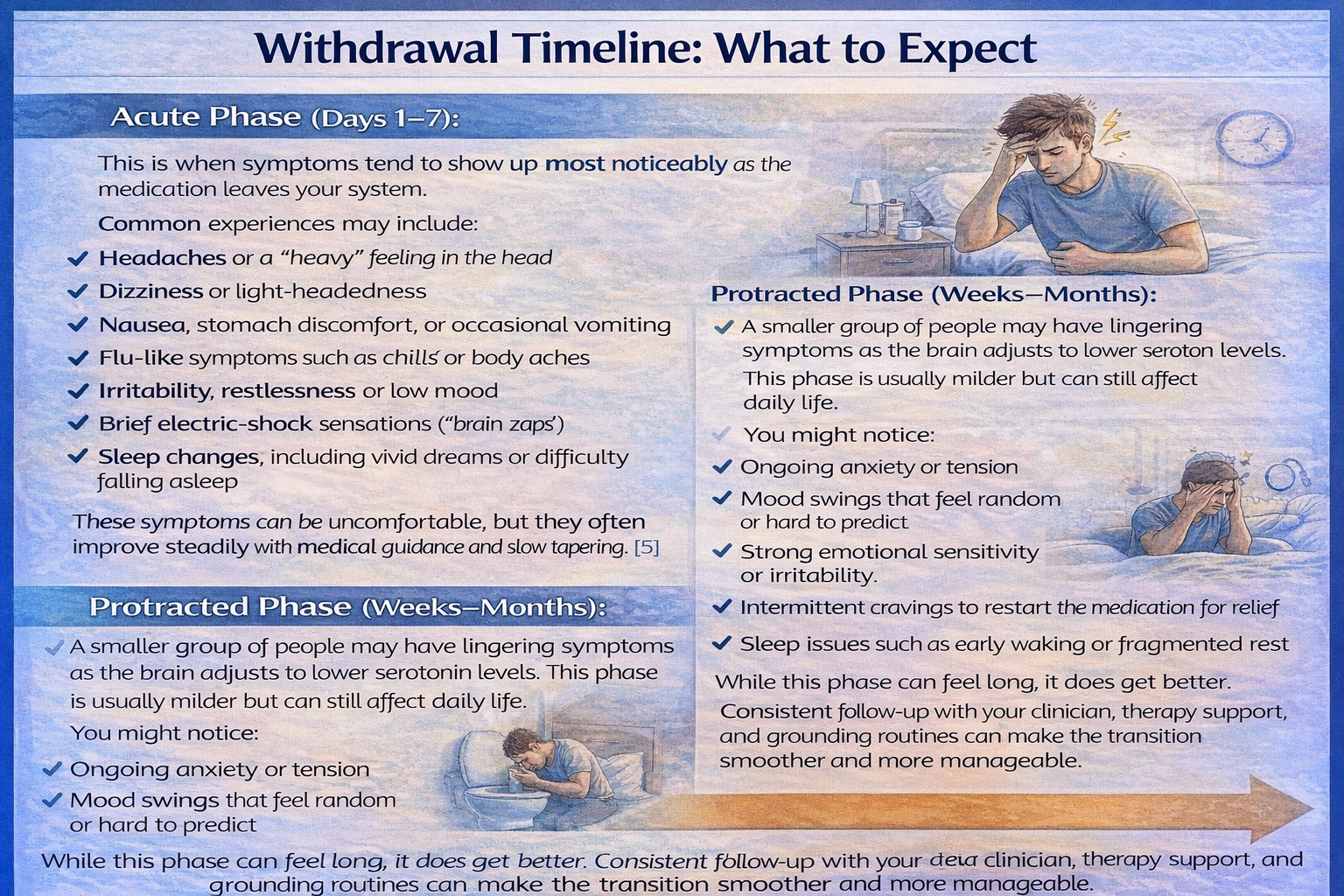
Acute Phase (Days 1–7):
This is when symptoms tend to show up most noticeably as the medication leaves your system.
Common experiences may include:
-
Headaches or a “heavy” feeling in the head
-
Dizziness or light-headedness
-
Nausea, stomach discomfort, or occasional vomiting
-
Flu-like symptoms such as chills or body aches
-
Irritability, restlessness, or low mood
-
Brief electric-shock sensations (“brain zaps”)
-
Sleep changes, including vivid dreams or difficulty falling asleep
These symptoms can be uncomfortable, but they often improve steadily with medical guidance and slow tapering. [5]
Protracted Phase (Weeks–Months):
A smaller group of people may have lingering symptoms as the brain adjusts to lower serotonin levels. This phase is usually milder but can still affect daily life.
You might notice:
-
Ongoing anxiety or tension
-
Mood swings that feel random or hard to predict
-
Strong emotional sensitivity or irritability
-
Intermittent cravings to restart the medication for relief
-
Sleep issues such as early waking or fragmented rest
While this phase can feel long, it does get better. Consistent follow-up with your clinician, therapy support, and grounding routines can make the transition smoother and more manageable.
When to Seek Immediate Help?
Some symptoms go beyond “watch and wait” and require urgent medical attention. These warning signs can escalate quickly, and getting help right away can prevent serious complications.
-
Persistent vomiting or signs of dehydration: If you can’t keep fluids down, experience dizziness, dry mouth, or dark urine, this may indicate a medical emergency. Dehydration can progress rapidly and shouldn’t be ignored.
-
Hallucinations or sudden confusion: Seeing, hearing, or believing things that aren’t real—or suddenly feeling disoriented—can signal severe reactions to medication, overdose, or a mental health crisis. Immediate evaluation is critical.
-
Suicidal thoughts or urges to self-harm: Any shift toward hopelessness, impulsive behavior, or self-harm thoughts requires fast intervention. Call emergency services or reach out to a crisis helpline right away. You deserve safety and support in that moment.
-
Overdose signs: Slowed breathing, blue or pale lips, extreme drowsiness, or unresponsiveness indicate a life-threatening emergency. Don’t wait it out—call for help right away.
If opioid use is also involved, naloxone may reverse dangerous breathing problems and save a life, but emergency care is still essential. When in doubt, it’s always safer to reach out. Getting help quickly can make all the difference.
Dosing, Safety & Overdose Risks (For Legitimate Prescribing)
Typical therapeutic dosing:
Prozac is usually prescribed in a controlled range, starting low and gradually increasing based on symptoms and response. Most adults fall within 20–60 mg per day, depending on the condition being treated and how they tolerate the medication.
High-risk combinations:
Mixing Prozac with alcohol, benzodiazepines, opioids, or other sedatives can increase impairment, slow breathing, and raise the risk of dangerous reactions. These combinations should always be avoided unless a clinician explicitly guides the plan.
How overdose works:
A Prozac overdose can overwhelm the central nervous system. Severe cases may lead to confusion, seizures, dangerously fast heart rate, and respiratory depression.
If opioids are involved, naloxone can reverse breathing problems and save lives, but emergency care is still required.
Safe-use guidance:
Store medication securely, never share prescriptions, and dispose of unused doses through a pharmacy take-back program or other approved method. Proper handling keeps the medication effective—and keeps your household safe.
Conclusion
Prozac addiction can be treated, and recovery is absolutely within reach.
With the right mix of medical guidance, structured therapy, and steady emotional support, people truly do heal.
Your next steps can start now:
-
Get a professional evaluation to understand what you need.
-
Select the right level of care, whether it’s supervised detox, medication support, or ongoing therapy.
-
Strengthen your support network by involving trusted family, peers, and consistent follow-ups with your care team.
You’re not expected to do this on your own.
Help is here. Healing is possible. And you deserve both.
FAQs
True “addiction” to Prozac is rare, because it does not create the same dopamine-driven reward cycle as opioids or benzodiazepines. However, dependence and withdrawal symptoms can still occur, especially if doses are changed too quickly or stopped abruptly. The safest path is consistent medical monitoring to prevent dose escalation or emotional reliance on the medication.
Serious risks include serotonin syndrome, extreme agitation, and—in rare cases—overdose if Prozac is taken in very high amounts or mixed with other substances. Combining Prozac with alcohol, benzodiazepines, or opioids increases sedation and breathing problems. Any sudden mental health changes, suicidal thoughts, or severe physical symptoms require immediate medical attention.
Relapse doesn’t mean failure. It often means the brain is still readjusting after long-term use or that stressors have resurfaced. A relapse simply signals that the treatment plan needs adjustment—maybe slower tapering, more therapy, or better support at home. Recovery is a process, and each setback is a chance to refine the plan.
Self-detox is not recommended. Stopping Prozac without medical guidance can trigger severe withdrawal symptoms like mood crashes, panic spikes, dizziness, and “brain zaps.” A supervised taper is safer, more comfortable, and reduces the risk of emotional instability or relapse into misuse.
Families can make a powerful difference. Start with education—understanding withdrawal, mood changes, and relapse triggers. Offer non-judgmental support, encourage consistency with treatment, and participate in family therapy when possible. A calm, compassionate home environment reduces stress and strengthens recovery.
Resources
Related Articles
Treatment Centers in Virginia









