Remeron Addiction: Definition, signs, causes, effects, and treatment options
Remeron, or mirtazapine, is a prescription medication classified as a tetracyclic antidepressant. It is used to treat major depressive disorder (MDD). Remeron affects the brain’s neurotransmitters and helps individuals mitigate symptoms of depression. It is also used to treat other disorders such as PTSD, GAP, and OCD due to its sedative appetite stimulant, anxiolytic, and antiemetic effects.

Remeron, or mirtazapine, is a prescription medication classified as a tetracyclic antidepressant. It is used to treat major depressive disorder (MDD). Remeron affects the brain’s neurotransmitters and helps individuals mitigate symptoms of depression. It is also used to treat other disorders such as PTSD, GAP, and OCD due to its sedative appetite stimulant, anxiolytic, and antiemetic effects.
The signs of remeron addiction include physical health issues such as cardiac arrest, low blood pressure, seizures, taking Remeron for a long time, increased dosage need, inability to avoid medication, social withdrawal, and changes in behavior and appearance.
The main causes of remeron addiction include self-medication, misuse, peer influence, coping mechanisms, and environment.
The side effects of Remeron addiction are categorized into two types i.e. mild effects and serious effects. Mild effects include weight gain, drowsiness, constipation, abdominal pain, vomiting, and anxiety. Serious effects include acute psychosis, suicidal thoughts, serotonin syndrome, and compulsive behavior.
The treatment options for remeron addiction include detoxification, cognitive behavioral therapies, medication, long-term rehabilitation programs, and aftercare.
What is Remeron Addiction?
Remeron is a TeCA (tetracyclic antidepressant) drug used primarily for treating major depressive disorder, according to the study “Mirtazapine” by Talha N. Jilani, Jonathan R. Gibbons, Rubina M. Faizy, published by the National Institutes of Health. Remeron is used for post-traumatic stress disorder, generalized anxiety disorder, and obsessive-compulsive disorder. Remeron addiction works by increasing the levels of dopamine and serotonin and blocking 5-HT receptors which improves mood, reduces anxiety, increases appetite, stabilizes mood, and improves sleep quality.
54% of patients while taking Remeron experienced excessive sedation and drowsiness, according to the Addiction Center, in US-controlled studies. The data shows that more than half of the patients observed this negative side effect of Remeron.
The number of deaths from mirtazapine drug poisoning from 2002 to 2022 in England and Wales, according to the study on “Death by Mirtazapine drug” published by Conor Stewart. Data indicates a high number of deaths i.e. 152 death records occurred in 2022.
What is Remeron used for?
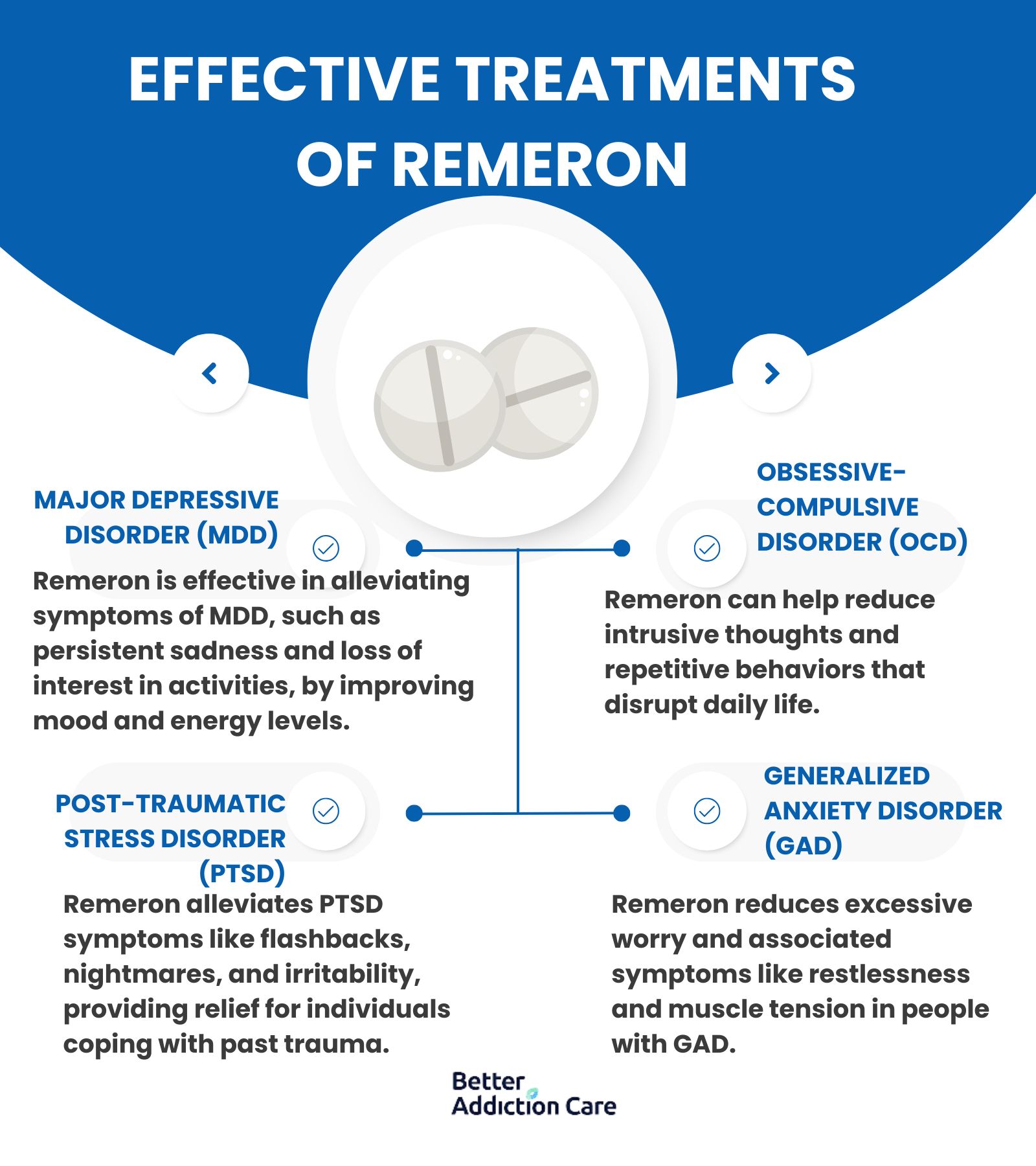
The Remeron is used for treating major depressive disorder (MDD), obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), and generalized anxiety disorder (GAD).
These effective treatments of remeron are elaborated below:
-
Major depressive disorder (MDD): Major Depressive Disorder (MDD) is a common mental condition that occurs due to persistent feelings of sadness, hopelessness, or emptiness. MDD disorder is triggered by a combination of psychological, biological, and environmental factors. It affects anyone, regardless of age, gender, or background. People with this disorder often experience symptoms like feelings of worthlessness, weight changes, loss of interest in activities, change in appetite, sleep disturbance, and lack of focus and control.
Mirtazapine is an approved medication in many countries for treating Major depressive disorder (MDD), according to the article titled “Mirtazapine: a review of its use in major depression and other psychiatric disorders” published in the journal CNS Drugs in 2009. This provides an effective and quick reduction in depressive symptoms.
-
Obsessive-Compulsive Disorder (OCD): Obsessive-compulsive disorder is a chronic disorder defined by unwanted thoughts and repetitive behaviors that individuals think necessary to function according to the research titled “Obsessive-Compulsive Disorder” by NIH. These obsessions and compulsions greatly interfere with individual life and cause distress. Common symptoms include organizing things, excessive cleaning and hand washing, ordering, and experiencing anxiety. Mirtazapine effectively treats patients experiencing OCD, according to the study “Mirtazapine for obsessive-compulsive disorder: an open trial followed by double-blind discontinuation” published by NIH.
-
Post-traumatic stress disorder (PTSD): Post-traumatic stress Disorder (PTSD) is a common mental condition characterized by experiencing a traumatic life event and is often due to genetic inheritance. Individuals with PTSD often experience intense thoughts, nightmares, flashbacks, sleep difficulties, irritability, and guilt. Mirtazapine is a beneficial and well-tolerated medication for treating patients with PTSD, according to the study “Effects of mirtazapine in patients with post‐traumatic stress disorder in Korea” by Won-Myong Bahkin in 2022.
-
Generalized Anxiety Disorder (GAD): Generalized Anxiety Disorder (GAD) is a long-lasting mental condition triggered by excessive worry about various life aspects such as finances, health, or relationships. Individuals with GAD have symptoms like fatigue, restlessness, irritability, muscle tension, and nausea. Open-label study proves that mirtazapine is an effective treatment option for patients with a generalized anxiety disorder (GAD), according to the study on “Mirtazapine treatment of generalized anxiety disorder: a fixed dose”.
How is Remeron consumed?
Remeron is consumed in the form of oral tablets, mixed with food, or through injection. Remeron is commonly prescribed with oral tablets in various dosages i.e. 15 mg, 30 mg, and 45 mg. Remeron is swallowed with water or by putting orally disintegrating tablets (ODT) on the tongue and allowing it to dissolve. Another way of consuming remeron is by crushing or mixing it with food. This method is used by individuals having difficulty swallowing tablets. A less preferred way is through injection which is not a standard method for administering remeron. The injection method is usually used in hospitals for patients who are unable to take medication orally.
How does Remeron Addiction affect the brain?
Remeron addiction affects the brain by altering how it regulates mood-related chemicals, such as serotonin and norepinephrine. Remeron (mirtazapine) is an antidepressant that increases these neurotransmitters to relieve depression. Remeron leads to dependency when misused, as the brain becomes addicted to these heightened levels. This dependency causes the brain to struggle in naturally balancing these chemicals, leading to withdrawal symptoms like anxiety, mood swings, or insomnia if the drug is stopped suddenly.
What are the Signs of Remeron Addiction?
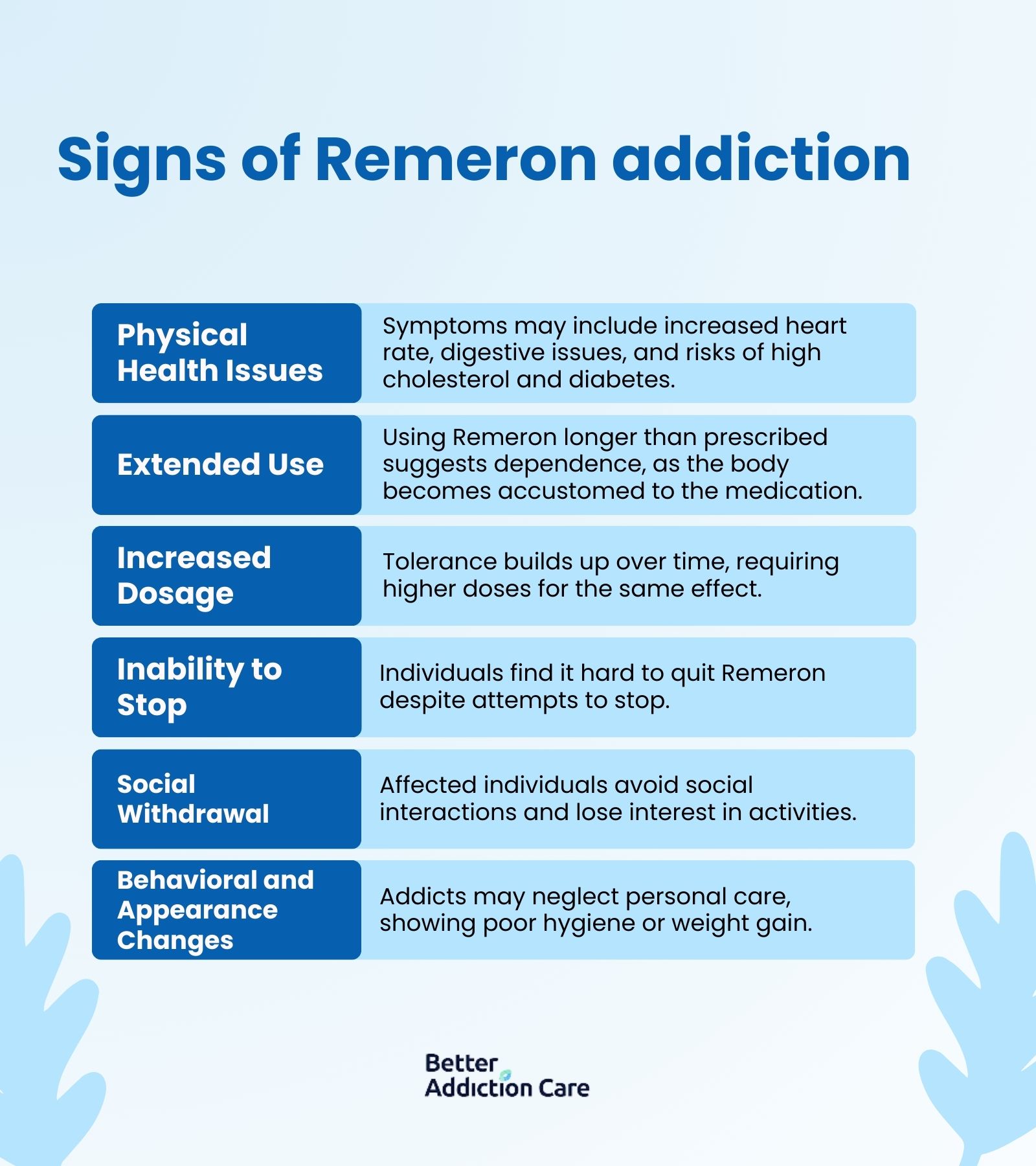
The signs of remeron addiction are physical health issues, taking it for a long time, increased dosage need, inability to avoid, social withdrawal, and changes in behavior and appearance.
The signs and symptoms of remeron addiction are described below:
-
Physical Health Issues: Physical health issues like increased heart rate, blood pressure, change in sleep patterns, constipation, and digestive issues are persistent with Remeron Addiction. Remeron also leads to high cholesterol, increased risk of diabetes, and muscle pain.
-
Taking Medication for a Long Time: Taking Remeron for a longer time than prescribed or needed indicates addiction and physical dependence. Remeron addiction occurs when an individual's body becomes habitual to the medication. Long-term use of medication leads to an increase in dosage without consultation.
-
Increased Dosage Need: Increased dosage need is known as tolerance which occurs when an individual's body adapts to the effect of the medication. Users need higher doses to get the same effect over time.
-
Inability to Avoid: Inability to avoid means the individual addicted to the medication is unable to discontinue despite their best efforts.
-
Social Withdrawal: Social withdrawal is when individuals with Remeron addiction lose interest in activities and avoid family, friends, and social gatherings. These behavioral shifts are warning signs that an individual is struggling with addiction.
-
Change in Behavior and Appearance: Individuals with Remeron addiction show a change in their behavior and appearance by neglecting self-care, leading to poor hygiene, lack of interest in clothing, or gaining weight.
What are the Causes of Remeron Addiction?
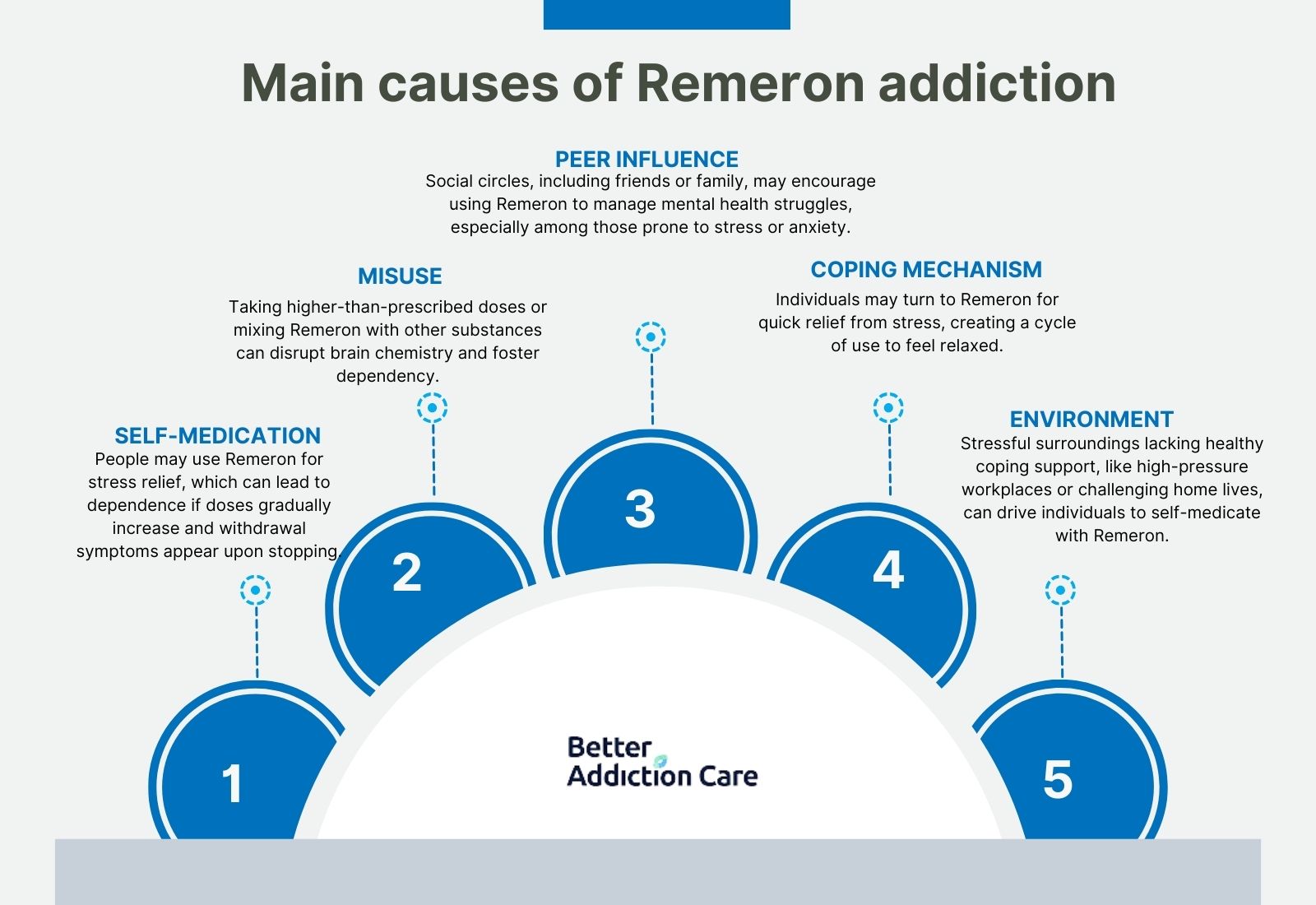
The causes of remeron addiction are self-medication, misuse, peer influence, coping mechanisms, and environment.
These causes are elaborated below:
-
Self-Medication: Individuals use Remeron as a self-medication for temporary relief from stress or anxiety, their body adapts and develops a risk of dependence. Gradual increase in dosage makes the individual reliant on the medication, and withdrawal symptoms occur when they try to stop.
-
Misuse: Misuse of Remeron creates tolerance, psychological dependence, and withdrawal symptoms. Individuals who take more than prescribed by a doctor to support sleep or combine it with other substances disrupt the brain's chemical balance and develop physical dependence.
-
Peer Influence: Peer influence, such as family, friends, and other social connections pushes others to consider Remeron for stress reduction. Individuals, especially young ones who are dealing with mental health issues, are easily influenced by their social circle to try this medication to manage their stress, anxiety, insomnia, and other mental health problems.
-
Coping Mechanism: Some individuals consider Remeron as a coping mechanism to get quick relief from stress and other health problems. Remeron helps them feel relaxed, but later on, they continue using it to achieve the same relief.
-
Environment: A stressful environment, such as facing pressure at work, school, or home pushes people to handle their emotions through self-medication. Environments that do not encourage healthy strategies or coping mechanisms leave individuals feeling helpless and more likely to use drugs for relief.
What are the Side Effects of Remeron Addiction?
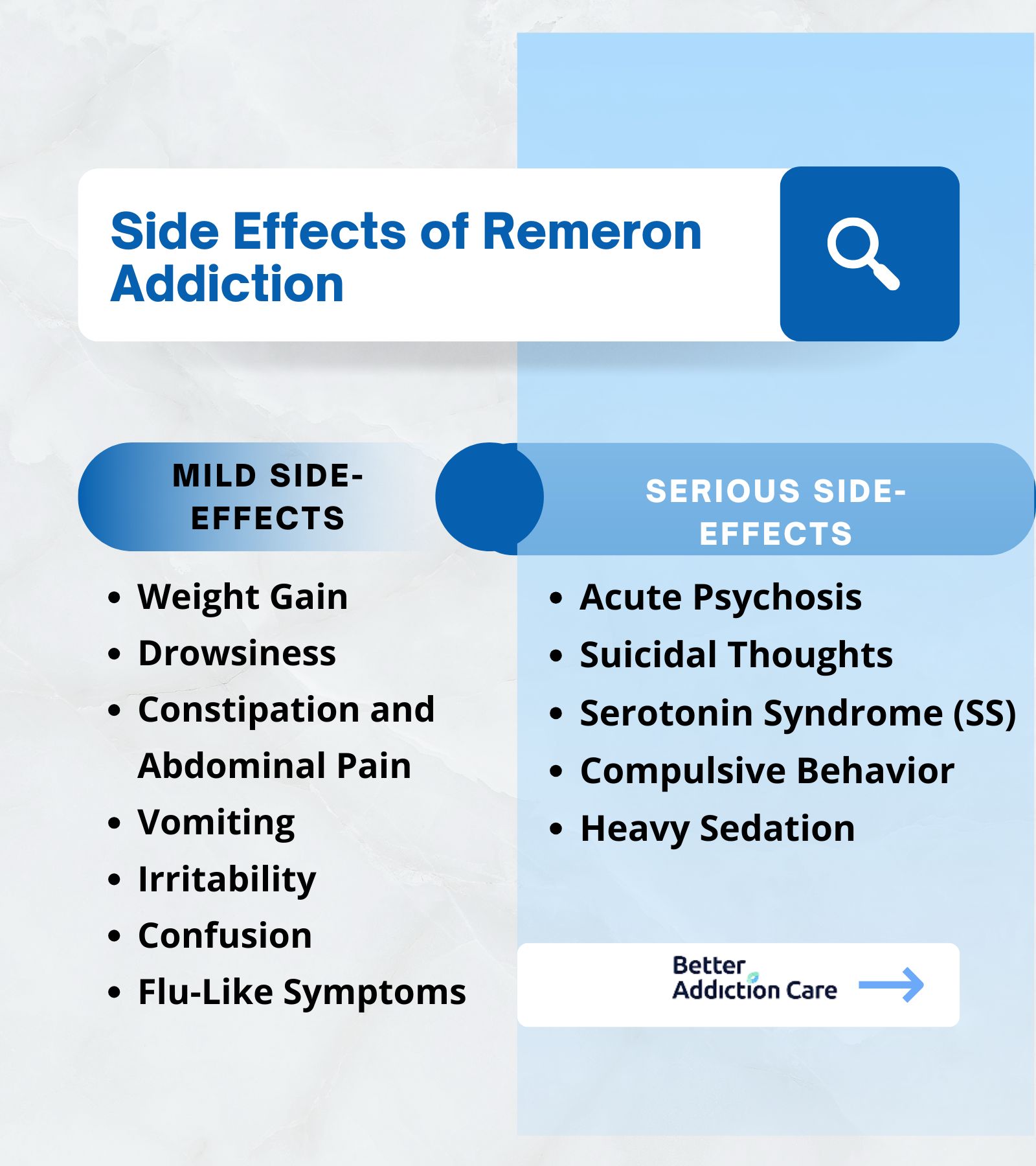
The side effects of Remeron addiction include two categories, which are mild and serious side effects.
Mild Side-Effects
Some mild side-effects of remeron addiction are weight gain, drowsiness, constipation and abdominal pain, vomiting, anxiety, irritability, confusion, and flu-like symptoms.
These mild side effects are explained below:
-
Weight Gain: Remeron use leads to an increased appetite, which eventually results in unhealthy weight gain. Remeron stimulates cravings, and individuals can gain weight easily if foods are high in calories or rich in carbohydrates. Mirtazapine treatment increases body fat, body weight, and levels of leptin, according to the study “Effect of mirtazapine treatment on body composition and metabolism” published by NIH.
-
Drowsiness: Remeron makes individuals feel drowsiness, usually in the initial days of use. Excessive sleep may interfere with regular activities and make it harder to remain active and focused. The remeron medication increases appetite, weight gain, and excessive sleepiness, according to the study “Mirtazapine versus other antidepressive agents for depression” published by the National Library of Medicine.
-
Constipation and Abdominal Pain: Remeron affects the digestive system and results in constipation and abdominal discomfort. Remeron interacts with the neurotransmitters that control bowel movements, and individuals feel symptoms like bloating, cramps, infrequent stools, or even difficulty in passing stool.
-
Vomiting: Remeron causes nausea that eventually leads to vomiting. The sedative properties of remeron slow down the digestive process, which causes food to remain in the stomach for an extended time. The accumulated food in the stomach potentially increases pressure and causes individuals to vomit. This effect is temporary but leads to dehydration if it persists.
-
Irritability: Irritability means a sudden shift in mood, such as anger and frustration. Remeron initially causes mood changes that increase frustration and irritability. This arises due to the body‘s adjustment to the effect of the medication. The use of medication makes individuals feel lethargic and tired, and due to this, they become more easily irritated.
-
Confusion: Remeron temporarily affects cognitive functions and disturbs normal brain activity. It contributes further to the sense of mental fog, memory lapses, and greater confusion. This confusion impacts an individual’s various life aspects. They may struggle to remember important information, conversations, and events, which are more frustrating.
-
Flu-Like Symptoms: Remeron causes flu-like symptoms, like chills, muscle pain, and headache. These effects are usually resolved within weeks as the individual’s body adapts to the medication.
Serious Side-Effects
Serious side-effects of remeron addiction are acute psychosis, suicidal thoughts, serotonin syndrome, compulsive behavior, and heavy sedation.
These side effects are described below:
-
Acute Psychosis: Remeron causes alarming acute psychosis effects, especially for individuals with pre-existing psychotic disorders, or whose dosage alters in some way. Remeron interacts with norepinephrine and serotonin, which causes delusions, hallucinations, disorganized behaviors, or even combinations of these. A 43-year-old man with major depressive disorder who started taking mirtazapine and experienced vivid dreams are also serious side-effects, according to the case study titled “Acute Psychosis Associated with Dissociated Sleep‐Wakefulness State After Mirtazapine Treatment." This confused him to differentiate these from reality and led to acute paranoia.
-
Suicidal Thoughts: Remeron medication increases suicidal thoughts, especially for young individuals as they become more sensitive to the effects of antidepressants. This sensitivity increases anxiety, agitation, and hopelessness, leading to thoughts of suicide. A comparison of remeron to venlafaxine and selective serotonin reuptake inhibitors (SSRIs) found no difference in self-harm after adjusting for patients' baseline information, according to the study on the Association between mirtazapine use and serious self-harm in people with depression in 2022. The study indicates that mirtazapine showed a high risk of self-harm as compared to amitriptyline.
-
Serotonin Syndrome (SS): Remeron potentially causes life-threatening serotonin conditions when individuals take higher than recommended doses or take it alongside other serotonergic medications. The symptoms may include high blood pressure, increased heart rate, dilated pupils, or seizures. Serotonin syndrome occurs due to overstimulation of serotonin receptors, according to the study titled, “Serotonin Syndrome—what have we learned? Published in Clinical Pediatric Emergency Medicine”. The noncurrent use of multiple serotonergic medications increases the risk of developing SS.
-
Compulsive Behavior: Remeron interacts with the brain system and develops behaviors, such as the urge to do specific tasks, organize items, and check things repeatedly, which disturb their daily life functioning.
-
Heavy Sedation: Remeron creates a state of heavy sedation among patients, mainly due to the medication’s antihistaminergic properties. The medication blocks H1 receptors, which causes difficulty in sleeping and maintaining activeness. As a result, users feel overly sedated, which complicates their ability to perform daily activities. Remeron is a serotonergic and noradrenergic antidepressant that affects sleep, according to the study titled “Dose-dependent sedating and stimulating effects of mirtazapine” by Leonard and Karlamangla in 2015. The 15 mg dose supports sleep, but low doses, such as 7.5 mg, primarily cause sedation in older adults.
What are the treatment options for Remeron Addiction?
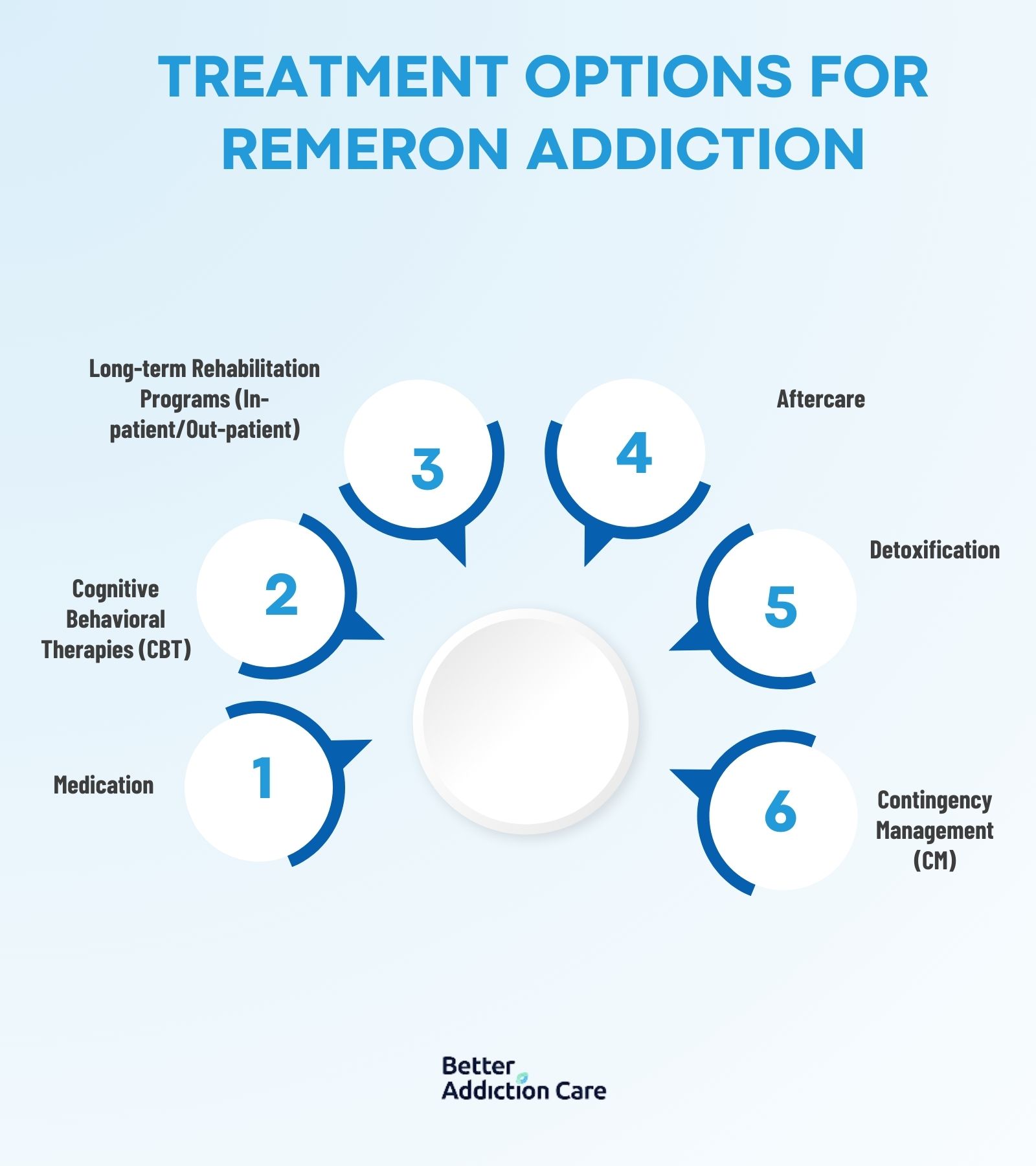
The treatment options for remeron addiction are detoxification, cognitive behavioral therapies, medication, long-term rehabilitation programs (in-patient/out-patient), and aftercare.
These treatment options for remeron addiction are described below:
-
Detoxification: Detoxification helps manage withdrawal symptoms by clearing the drug from the body. Detox typically lasts 5-7 days and reduces cravings and stabilizes the patient. Medical supervision is important to manage potential severe side effects such as mood swings or nausea.
-
Cognitive Behavioral Therapies (CBT): CBT aims to change negative thought patterns linked to addiction and help identify triggers, manage cravings, and build coping strategies. CBT is effective in 12-16 weeks to treat remeron addiction, according to the study, "Cognitive-Behavioral Therapy for Substance Use Disorders: A Review of Its Clinical Efficacy." The advantages of CBT include long-term relapse prevention, but it involves the need for strong patient engagement.
-
Medication: Medications, such as antidepressants or anxiolytics, are prescribed to reduce withdrawal symptoms or treat co-occurring disorders. Combining medication with therapy improves outcomes for addicts, according to the study titled "Medication-Assisted Treatment for Substance Use Disorders." Treatment duration with medication varies and takes several months. Medications provide symptom relief but increase dependency risks on substitute drugs.
-
Long-term Rehabilitation Programs (In-patient/Out-patient): Long-term rehabilitation programs, such as in-patient and outpatient programs provide support throughout the recovery process. In-patient programs require patients to stay in a medically supervised environment for 30 - 90 days, while out-patient programs offer the flexibility to stay at home but attend regular counseling and therapy sessions. Patients of remeron addiction achieve recovery in 30-90 days through outpatient rehabilitation programs, according to the study "Comparative Effectiveness of Outpatient Treatment for Substance Use Disorders.”
-
Aftercare: Aftercare involves support groups, follow-ups, or therapy to maintain self-control over oneself. It lasts for months or years and reduces relapse risk for remeron addicts with long-term follow-up, according to a study titled "Impact of Continuing Care on Recovery From Substance Use Disorder" published in NIH. The advantages of this treatment include continuous support but involve dependency on external support.
-
Contingency Management (CM): Contingency management uses rewards for positive behaviors like attending therapy sessions. CM helps in behavioral modification and relapse prevention in patients, according to the study, "Contingency Management in Substance Use Treatment” published by the National Library of Medicine. The average duration of this treatment is 12 weeks but they are costly.
What are the Withdrawal Symptoms of Remeron Addiction?
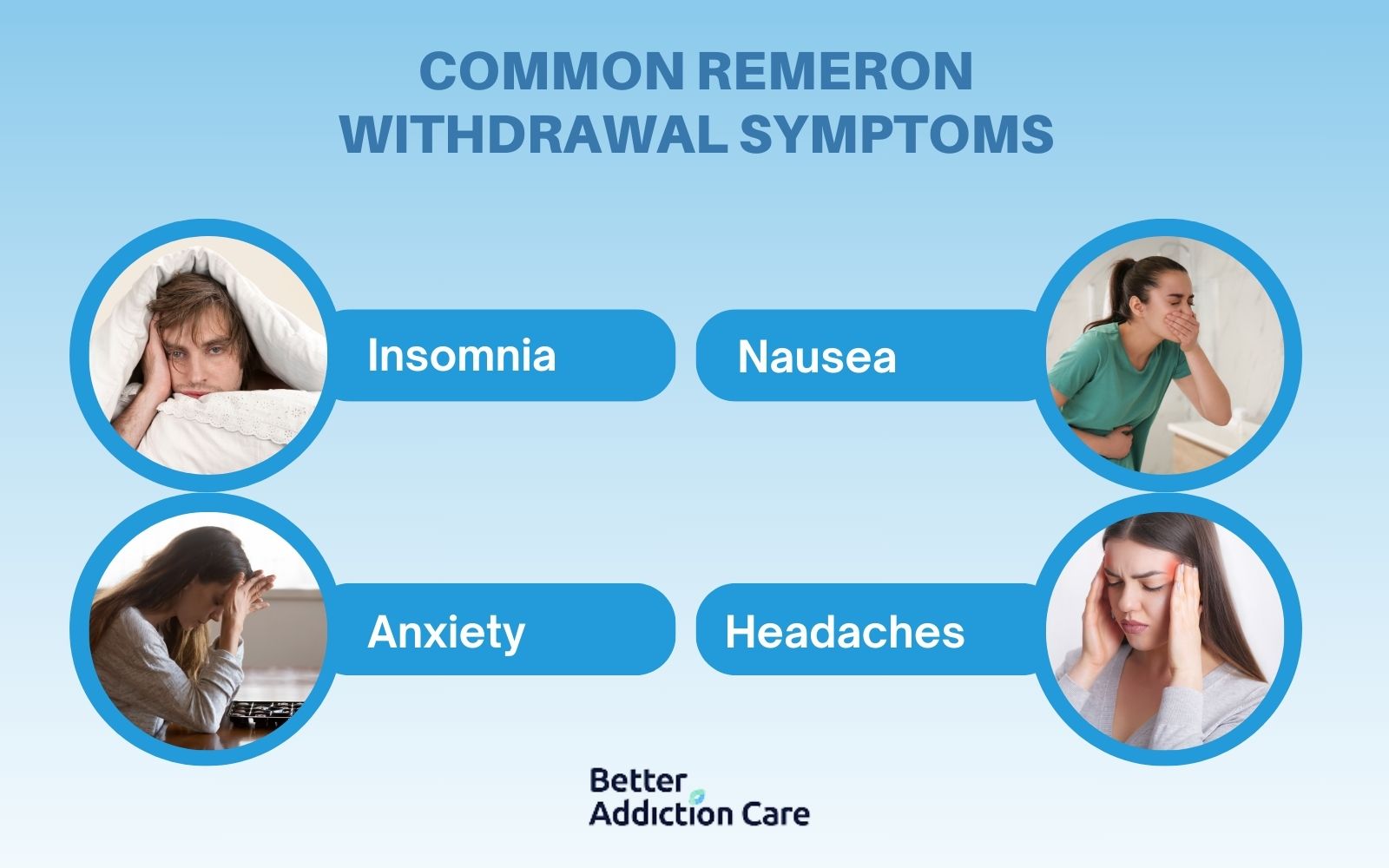
Withdrawal symptoms of remeron addiction include insomnia, nausea, anxiety, and headaches.
Remeron withdrawal occurs when its use is abruptly reduced or stopped after dependence. This happens due to sudden changes in neurotransmitters, particularly serotonin and norepinephrine. Doctors recommend reduced usage, which helps to lower withdrawal symptoms, according to a study titled "Antidepressant Discontinuation Syndrome” published in NIH.
The common Remeron withdrawal symptoms are listed below:
-
Insomnia: Insomnia is a common withdrawal symptom of remeron addiction that results from changes in serotonin and norepinephrine levels. Sleep hygiene, cognitive behavioral therapy for insomnia (CBT-I), and short-term use of sleep aids help manage insomnia for patients, according to the research on "Managing Insomnia in Patients with Antidepressant Withdrawal". Consistent sleep routines and stress reduction techniques are essential. The symptom typically lasts 1-2 weeks.
-
Nausea: Nausea is a common remeron withdrawal symptom that arises as the body's serotonin levels drop. Anti-nausea medications, hydration, and ginger tea ease this symptom of withdrawal according to the study, "Gastrointestinal Symptoms in Antidepressant Withdrawal" (NIH). Nausea subsides within a week but medical attention is required in severe cases.
-
Anxiety: Anxiety during remeron withdrawal is due to altered neurotransmitter activity, especially due to reduced serotonin levels. Anxiety causes restlessness, increased heart rate, or panic attacks. Relaxation techniques, breathing exercises, and short-term use of anxiolytics reduce the symptoms of anxiety, according to "Psychological Symptoms During Antidepressant Discontinuation." This symptom lasts from a few days to several weeks.
-
Headaches: Headaches are often reported during remeron withdrawal in patients with severe addiction. Headaches result from sudden shifts in brain chemistry. Over-the-counter pain relievers and rest are recommended to decrease headaches. Symptoms typically lessen within a few days but severe headaches may require medical advice from a doctor.
What are the risks of an overdose of Mirtazapine?
The risks of an overdose of Mirtazapine include serotonin syndrome, worsening of depression, suicidal thoughts, and impaired cognitive function. Serotonin syndrome occurs due to excessive serotonin in the brain, confusion, rapid heart rate, and severe agitation.
Serotonin syndrome is a critical risk in overdoses of mirtazapine, according to a study titled "Mirtazapine Overdose and Serotonin Syndrome published in NIH. Worsening of depression and suicidal thoughts are also possible as quick neurotransmitter changes intensify the symptoms of depression.
Cognitive impairment occurs, affecting memory, judgment, and motor coordination. Cognitive issues often arise when mirtazapine doses exceed recommended levels, according to a study titled "Mirtazapine overdose is unlikely to cause major toxicity” published in NIH. Patients may experience confusion, disorientation, or difficulty concentrating.
8.7% of mirtazapine overdoses in 2020 resulted in severe complications, with 45% of cases reported among individuals aged 18-34, according to the study “Mirtazapine overdose is unlikely to cause major toxicity” by NIH. Cases due to serotonin syndrome were found in 20% of cases, showing risk factors in younger populations as well.
How does Remeron Addiction Relate to Other Substance Addictions?
Remeron addiction relates to other substance addictions like opioids, alcohol, and stimulants, by sharing common features like dependence, withdrawal symptoms, and negative impacts on mental and physical well-being.
Do Remeron and Crystal meth affect neurotransmitters in the brain?
Yes, Remeron and Crystal meth both affect neurotransmitters in the brain. Remeron blocks specific receptors and regulates serotonin and norepinephrine, while crystal meth increases dopamine, serotonin, and norepinephrine levels. Remeron acts by blocking certain serotonin and alpha-2 receptors, which allows chemicals to stay longer in the brain which helps improve mood and reduce anxiety. On the other hand, meth suddenly increases the neurotransmitters and makes individuals feel alert, extremely energetic, and euphoric. This quick boost overwhelms the brain and leads to crystal meth addiction, emotional instability, disruption, and damage to brain cells.
Is Remeron considered to have a low potential for addiction compared to Xanax?
Yes, Remeron has a low potential for addiction compared to Xanax because it acts slowly regulating serotonin and norepinephrine levels. Remeron gradually increases neurotransmitters by blocking certain serotonin and alpha-2 adrenergic receptors. Remeron focuses on improving sleep, and mood, and reducing anxiety without producing immediate rewards and extreme euphoria. Whereas, Xanax works rapidly on Gamma-Aminobutyric Acid (GABA) receptors and focuses on a quick calming effect. This sudden relief leads to misuse of the drug, development of tolerance, and Xanax addiction.
Do Remeron and Benadryl serve as sedative medications?
Yes, Remeron and Benadryl both serve as sedative medications, but they provide different actions and uses. Remeron is an antidepressant that acts by gradually increasing serotonin and norepinephrine in the brain, treats anxiety and depression, and has sedative properties. Remeron directly blocks 5-HT2 and 5-HT3 receptors and stimulates 5HT1 receptors, which help improve sleep. On the other hand, Benadryl is an antihistamine used to relieve allergy reactions, such as sneezing, runny nose, itchy or watery eyes, and itching of the throat or nose. Benadryl induces sedation by blocking histamine receptors, which increases the feeling of drowsiness. The rate of Benadryl addiction is the same as Remeron.







