Mirtazapine and Weight Gain: Mechanisms, Prevalence, and Management
Mirtazapine is an atypical antidepressant commonly used to treat:
- major depressive disorder
- anxiety disorders
- trauma-related insomnia
- appetite loss associated with severe depression

Why Is It Associated With Weight Gain?
It works by blocking α2-adrenergic receptors, which increases serotonin and norepinephrine availability. Because these neurotransmitters regulate mood, sleep, appetite, stress response, and emotional regulation, many people feel calmer and sleep more deeply within the first week.
Key Takeaways
-
Weight gain with mirtazapine is common because it increases appetite-related signals in the hypothalamus, slows metabolic rate slightly, and improves sleep—factors that often increase calorie intake.
-
Not all weight gain is permanent. Many people plateau by month three, and gradual tapering (when medically appropriate) combined with structured lifestyle changes can reverse most gains.
-
Families can help by monitoring early appetite changes, supporting meal-planning, encouraging realistic activity routines, and staying involved in follow-up appointments—especially during the first 6–8 weeks when changes happen fastest.
How Common Is Weight Gain With Mirtazapine?
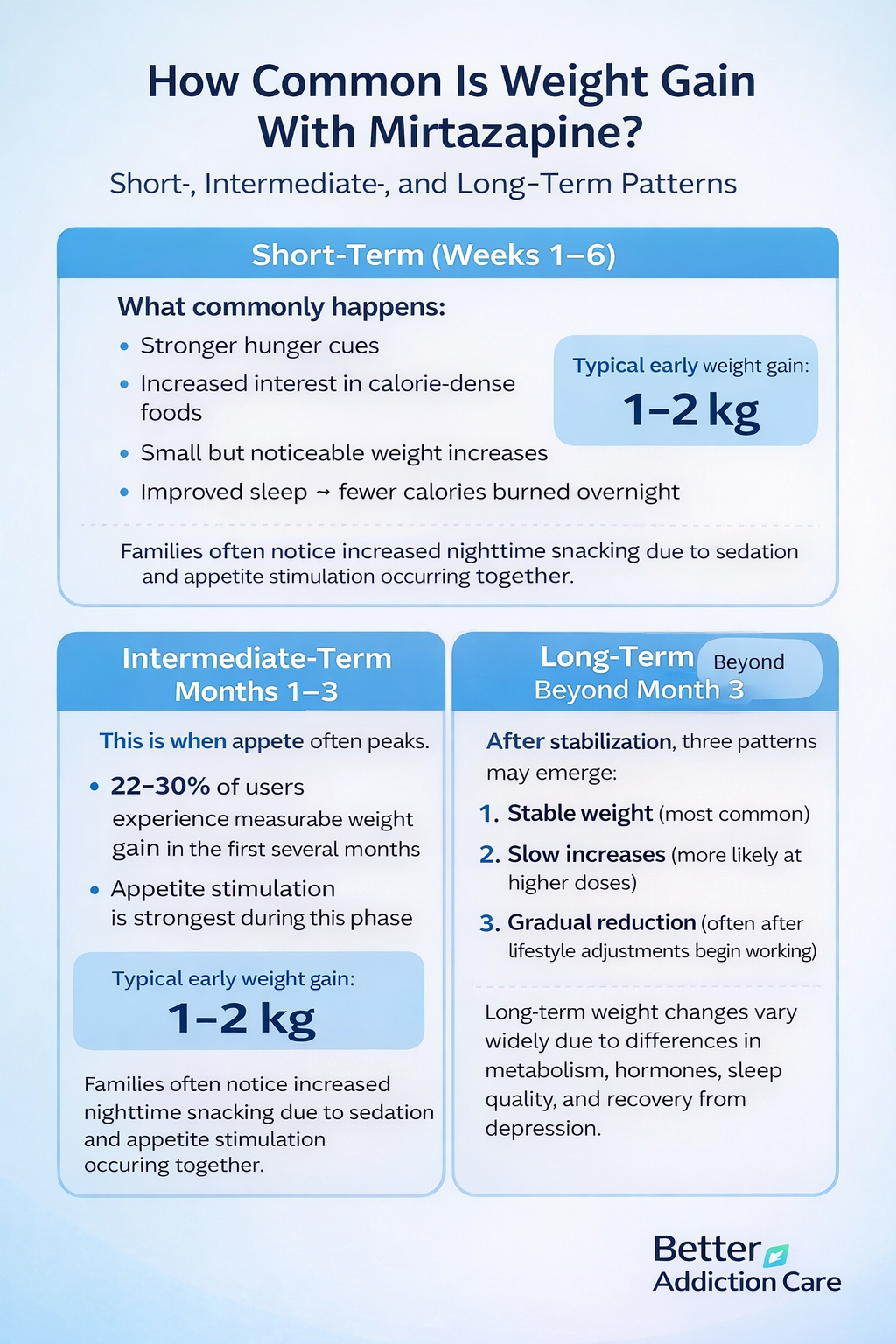
Short-Term (Weeks 1–6)
Most people experience:
-
stronger hunger cues
-
increased interest in calorie-dense foods
-
small but noticeable weight increases
-
improved sleep → fewer calories burned overnight
Typical early weight gain: 1–2 kg.
Families often notice increased nighttime snacking due to sedation and appetite stimulation occurring together.
Intermediate-Term (Months 1–3)
This is when appetite often peaks. Clinical studies report that 22–30% of mirtazapine users experience measurable weight gain during the first several months of treatment.” [1].
Average gain in this phase: 3–9 lbs.
However, many plateau naturally after the third month:
-
receptor sensitivity stabilizes
-
hunger hormones adjust
-
the body recalibrates from the initial appetite rebound
Long-Term (Beyond Month 3)
After stabilization, three patterns can emerge:
-
Stable weight (most common after month 3)
-
Slow increases (especially with higher doses)
-
Gradual reduction (often when lifestyle adjustments begin working)
Long-term weight gain varies widely because individual metabolism, hormone levels, sleep quality, and depression recovery differ dramatically.
Who Is Most at Risk?
-
Individuals recovering from appetite loss due to depression
-
Those with naturally slower metabolism
-
People with insulin resistance or pre-diabetic patterns
-
Individuals who experience emotional eating during stress
-
Young adults with strong dopamine-reward responses
-
People with irregular sleep schedules before treatment
Why do some people not Gain Weight?
A smaller group experiences little or no weight change.
This is often due to:
-
robust leptin sensitivity
-
regular pre-existing eating habits
-
high non-exercise activity (walking, fidgeting, pacing)
-
faster metabolic rate
-
structured meal patterns
-
supportive home environments
These individuals may not experience the same appetite rebound.
Why Does Mirtazapine Cause Weight Gain?
Weight gain from mirtazapine is not random. It comes from a combination of biological, hormonal, and behavioral mechanisms that build on one another over the first several weeks of treatment.
1. Appetite and Hunger Regulation
Histamine H1 Blockade: The “Hunger Switch”
The strongest appetite-stimulating effect of mirtazapine comes from histamine H1 receptor blockage, which directly influences how quickly hunger signals activate and how satisfied a person feels after eating.
Blocking these receptors:
-
increases hunger intensity throughout the day, making meals feel less filling and triggering earlier return of hunger between meals
-
reduces natural satiety signals, so the brain takes longer to register that the stomach is full, leading to larger portion sizes
-
enhances cravings for calorie-dense comfort foods, especially sugary or carb-heavy items that the body associates with quick energy and emotional relief
-
lowers internal “brakes” on appetite, making food cues (smells, visuals, memories of food) more powerful and harder to ignore
-
amplifies nighttime appetite, because the sedating effects of the medication overlap with hunger pathways that become more active in the evening
This mechanism is supported by clinical findings showing elevated appetite levels in the majority of new users[2].
Serotonin Receptors 5-HT2 and 5-HT3
Mirtazapine also blocks serotonin 5-HT2 and 5-HT3 receptors, which influence taste, digestion, reward processing, and fullness perception.
This leads to:
-
delayed feelings of fullness after meals, causing individuals to eat past their usual stopping point before recognizing they are satisfied
-
intensifying cravings during times of emotional stress, because serotonin influences how pleasurable food feels during recovery
-
increased preference for sweet, starchy, or high-carbohydrate foods, as these activate the brain’s quick reward pathways that become more reactive early in treatment
-
stronger interest in food even without emotional triggers, because serotonin shifts the balance between hunger and satisfaction
-
heightened response to the taste and smell of food, making certain foods feel unusually comforting or irresistible
2. Metabolic Rate Changes
Depression often elevates cortisol—the primary stress hormone—which accelerates muscle breakdown, disrupts sleep, and suppresses appetite.
When mirtazapine begins stabilizing the emotional system, several metabolic shifts occur.
When mirtazapine begins healing the emotional system:
-
cortisol levels start to normalize, reducing the body’s high-alert stress state and lowering the number of calories burned through tension and restlessness
-
sleep quality improves, which is good for emotional recovery, but slightly decreases overnight calorie burn because the brain and body move from hyperarousal to restorative patterns
-
the body shifts into a more energy-conserving mode, prioritizing repair, emotional regulation, and hormone stabilization over calorie expenditure
-
metabolism decreases slightly as the nervous system recovers, making the body more efficient at storing calories instead of burning them quickly
-
physical restlessness often decreases, leading to fewer unconscious movements (pacing, fidgeting), which normally burn more calories than people think
Even a 3–5% reduction in metabolic rate can contribute to gradual weight gain over several weeks, especially when depression recovery reduces stress-driven calorie burn. [3].
3. Hormonal Effects on Hunger and Fullness
Mirtazapine influences several appetite-related hormones. These hormonal shifts can be powerful enough to override logical eating patterns because they originate from biological signals—not emotional weakness.
Mirtazapine influences hormones such as:
-
Ghrelin — stimulates hunger, increasing the frequency and intensity of hunger waves, especially before bed or between meals
-
Leptin — signals fullness, but becomes temporarily less responsive, so it takes more food for the brain to register satisfaction
-
Neuropeptide Y — increases cravings for carbs, especially when the body is recovering from poor sleep, stress, or prior caloric restriction
-
Insulin — becomes more influential, especially in individuals with pre-existing insulin resistance, leading to stronger cravings for quick-energy foods
-
Cortisol — normalizes, which is beneficial for mental health, but can slow calorie burn and increase appetite during early recovery
This temporary hormonal mismatch makes hunger feel biological rather than emotional. Imagine the hunger dial being turned up to 8, while the fullness dial remains stuck at 4.
4. Behavioral and Lifestyle Factors
Depression disrupts routines—food patterns, sleep cycles, activity levels, and emotional coping behaviors shift dramatically during prolonged emotional distress.
Mirtazapine restores these systems, but recovery itself brings new exposures and behaviors that can influence weight.
Mirtazapine restores them, but recovery itself increases exposure to:
-
social meals that feel enjoyable again, often increasing calorie intake because shared eating feels comforting and reconnects individuals to daily life
-
comfort eating as emotional pain lessens, since food begins to taste more rewarding after months of numbness or appetite loss
-
late-night snacking triggered by medication timing, especially when mirtazapine is taken in the evening and overlaps with sedation-driven appetite
-
less stress-induced pacing or restlessness, which reduces unconscious calorie burn that was previously elevated during high-anxiety states
-
return of normal eating habits after long appetite suppression, which can feel like overeating but is often the body’s attempt to replenish nutritional deficits
Families often observe that their loved one begins:
-
finishing meals faster than before, because appetite signals feel stronger and more urgent
-
seeking snacks between meals or late in the evening, driven by a combination of biological signals and restored enjoyment of food
-
craving sweets or high-carbohydrate foods after dinner, which are more appealing when serotonin receptors shift and histamine pathways are blocked
-
eating larger portions or seconds, especially at night when the medication’s appetite-stimulating effects peak
-
showing enthusiasm for foods they previously avoided, because taste, texture, and reward processing become more satisfying during emotional recovery
These behaviors are common, predictable responses to biological changes—not failures of discipline, motivation, or self-control.
Is Weight Gain From Mirtazapine Permanent?
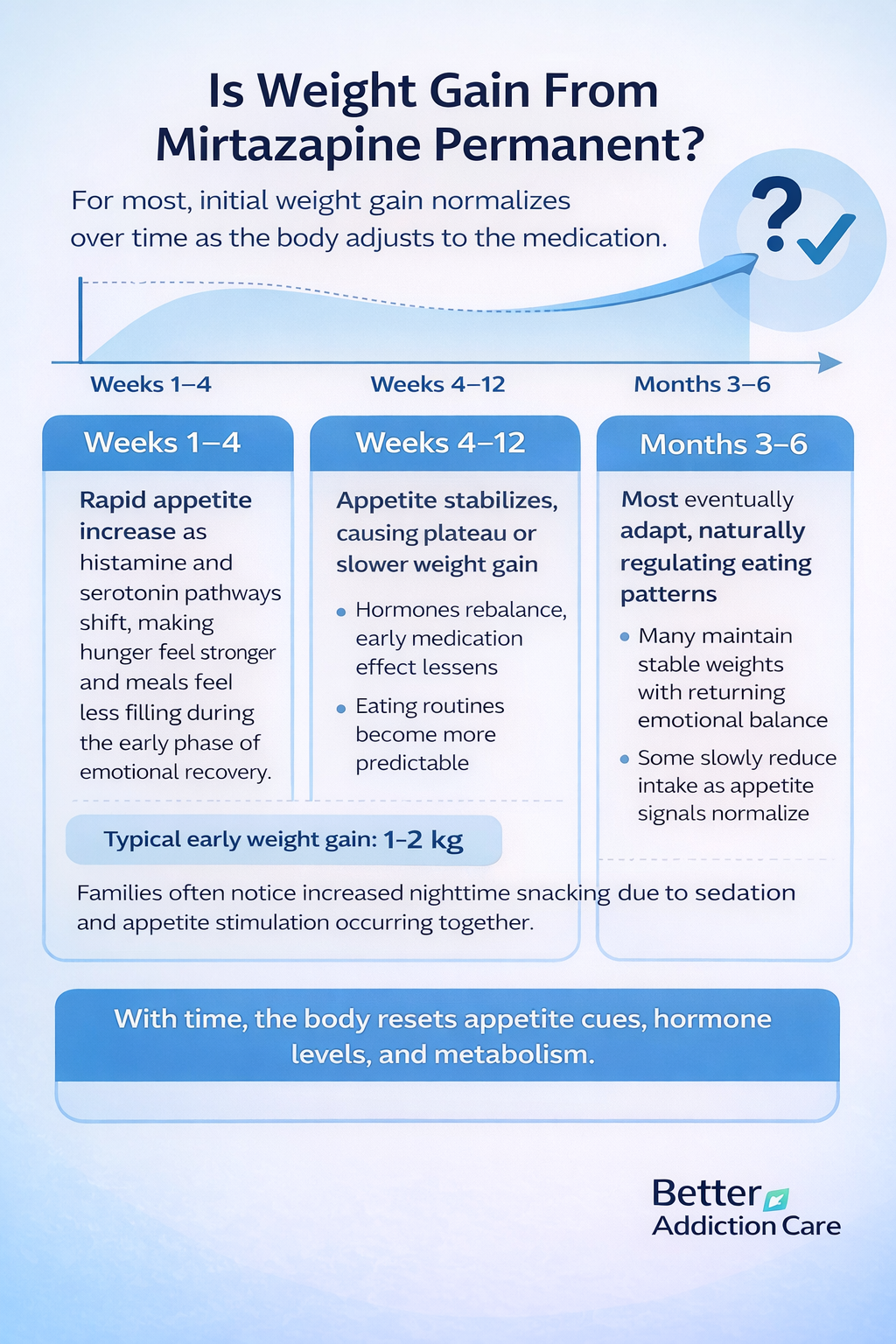
Not necessarily. The body adapts to receptor changes over time, and many of the appetite-driven shifts that appear early in treatment naturally settle as hormonal pathways stabilize and the nervous system adjusts to the medication.
Typical Pattern
Weeks 1–4
-
Rapid appetite increase as histamine and serotonin pathways shift, making hunger feel stronger and meals feel less filling during the early phase of emotional recovery.
-
Initial weight gain driven by stronger cravings, nighttime eating, and improved sleep, which together create a temporary imbalance in energy intake and expenditure.
Weeks 4–12
-
Appetite stabilizes as hunger hormones begin to rebalance, allowing individuals to regain a more predictable rhythm with meals and snacks.
-
Weight plateaus as the body adjusts to the medication, slowing down the early rapid changes once receptor sensitivity begins to normalize.
Months 3–6
-
Some individuals continue gradual increases, especially if appetite remains elevated or if lifestyle factors such as sleep and stress are still stabilizing.
-
Many stabilize naturally once emotional functioning improves, making it easier to maintain consistent eating habits and structured routines.
-
Some naturally reduce intake as appetite signals settle, leading to slow, steady normalization of eating patterns without intentional dieting.
Most people lose 50–80% of the weight gained on mirtazapine within 3–6 months after supervised tapering, as appetite and hormone sensitivity gradually normalize[4].
When Weight Does Not Decrease Easily?
A small percentage experience persistent changes due to:
-
long-term receptor adaptations
-
pre-existing metabolic vulnerability
-
chronic stress
-
irregular sleep cycles
-
emotional eating
-
sedentary routines
How Can Weight Gain Be Managed While Taking Mirtazapine?
Weight gain doesn’t mean treatment must stop. Combining medical guidance with realistic lifestyle strategies can help balance the benefits of Mirtazapine with healthy weight maintenance.
1. Monitor Weight and Appetite Early
Families can help by:
-
tracking weekly weight
-
noting sudden appetite spikes
-
watching for emotional hunger
-
using gentle, supportive language
-
observing nighttime snacking patterns
Early awareness prevents larger fluctuations.
2. Optimize Nutrition (Without Harsh Restriction)
Harsh dieting worsens depression and increases binge eating.
Structured but flexible eating promotes stability.
Core strategies:
-
include fiber at every meal
-
add proteins that slow digestion
-
maintain hydration (6–8 cups daily)
-
eat every 3–4 hours
-
balance meals with protein + fiber + complex carbs
Families can meal-prep or plan grocery lists together.
3. Increase Physical Activity (Realistic, Not Intensive)
The goal is consistency, not intensity.
Effective routine:
-
3 times per week structured exercise
-
daily movement such as walking or chores
-
stretching and light strengthening
-
10-minute “movement snacks” throughout the day
These routines help rebalance hunger hormones and reduce cravings.
4. Support Sleep and Stress Management
Improving sleep quality improves leptin and ghrelin sensitivity.
Strategies include:
-
consistent bedtime
-
low-light evenings
-
reduced screens
-
relaxation practices
-
calming pre-sleep environment
Families can support by maintaining quiet, predictable routines at home.
5. Discuss Medical Options
Weight gain alone is not a sign that the medication is harmful.
Doctors may:
-
lower the dose
-
switch dosing time
-
change medication
-
add supportive medications (rarely)
Never stop abruptly; withdrawal can destabilize mood.
When Should I Talk to My Doctor About Weight Gain?
Seek help if your loved one:
-
gains more than 5% body weight in 30 days
-
has constant hunger interfering with daily life
-
experiences sudden emotional eating
-
develops fatigue despite initial improvement
-
shows rapid changes in sleep cycles
Your doctor can assess:
-
metabolic changes
-
depression progress
-
medication adjustments
-
lab values
-
possible interactions
Can Weight Gain Be Prevented When Starting Mirtazapine?
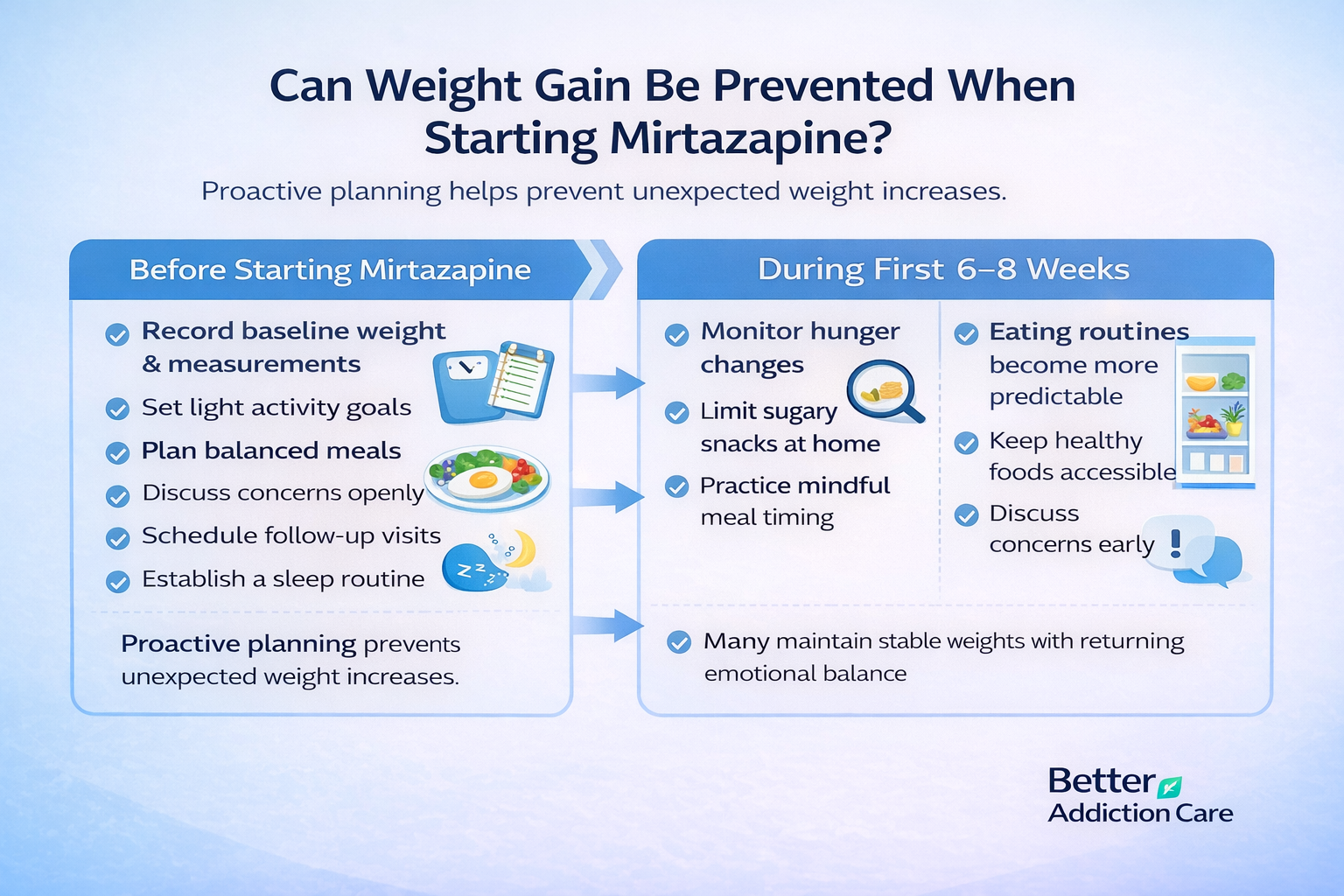
Before starting:
-
record baseline weight and measurements
-
set light activity goals
-
plan balanced meals
-
discuss concerns openly
-
schedule follow-up visits
-
establish a predictable sleep routine
During the first 6–8 weeks:
-
monitor hunger changes
-
avoid large stockpiles of sugary snacks
-
practice mindful meal timing
-
adjust environment (healthy foods accessible)
-
communicate changes early
Proactive planning prevents unexpected weight increases.
Conclusion
Weight gain from mirtazapine is understandable, manageable, and often reversible.
It reflects biological healing—not personal failure. With supportive structure, open communication, and early monitoring, individuals can maintain emotional stability while preventing major weight changes.
Families play a crucial role. Their involvement stabilizes routines, supports recovery, and ensures early symptom recognition. Most importantly, they help their loved one stay grounded in hope—even when the process feels overwhelming.
If weight gain becomes distressing or rapid, medical guidance can reshape treatment safely.
No one needs to choose between mental health and physical well-being; both can be protected with the right plan.
FAQs
Mirtazapine increases hunger because it blocks histamine H1 receptors and alters serotonin pathways that normally help regulate satiety and fullness signals. As these systems shift, appetite becomes stronger, cravings feel more urgent, and meals feel less filling. This hunger surge is temporary for most people and usually stabilizes as the body adapts.
Switching medications can help some people because not all antidepressants affect appetite and metabolism in the same way. However, appetite changes may take several weeks to settle, and switching too quickly can destabilize mood. Any change should be guided by a clinician who can assess risks, benefits, and safer long-term options for your loved one.
Most people notice appetite changes ease within 6–12 weeks as hunger hormones rebalance and receptor activity stabilizes. Some may need up to three months for cravings and portion sizes to feel normal again. Tracking early patterns with your family or provider helps distinguish between temporary side effects and changes needing adjustments.
Sometimes. Lower doses may reduce sedation and appetite stimulation, but dose-dependent effects vary widely from person to person. In some individuals, reducing the dose eases cravings; in others, it makes no noticeable difference. Because appetite changes are highly individualized, any dose adjustment should be discussed with your healthcare provider.
Yes, many people lose much of the weight they gained once their appetite stabilizes or the medication is gradually tapered under medical supervision. As receptor activity normalizes, hunger decreases, and metabolism improves. Consistent routines—nutritious meals, structured activity, sleep stability, and family support—help accelerate this natural rebalancing process.
Absolutely. Families play a crucial role by helping create structured mealtimes, encouraging gentle physical activity, establishing predictable sleep routines, and offering emotional support without shame. Observing appetite changes together and communicating them early to a provider can prevent rapid weight gain and help your loved one stay consistent with treatment.
Yes. Nighttime eating typically decreases as the sedation and appetite-stimulating effects of mirtazapine stabilize. Early in treatment, the medication peaks at night, increasing hunger signals, but this often improves within a few weeks. Structuring evening routines, planning balanced dinners, and avoiding highly processed snacks at home can make a noticeable difference.