Mirtazapine Withdrawal: Symptoms, Timeline and Tips for Quitting
Deciding to stop Mirtazapine, also known by its brand name Remeron, often brings more questions than answers. What will the first days feel like? Will the symptoms drag on for weeks? What if my depression or anxiety comes back? These are the kinds of worries that make withdrawal feel so daunting.

When someone stops Mirtazapine, the brain has to adjust to functioning without the extra support it was getting to regulate mood and rest. This adjustment period is what causes withdrawal.
People often report dizziness, insomnia, irritability, vivid dreams, or a sudden spike in anxiety during this time. These symptoms are collectively known as antidepressant discontinuation syndrome, and while unpleasant, they are not considered medically dangerous for most people.
Key Takeaways
-
MIrtazapine withdrawal is real but temporary. Symptoms like nausea, dizziness, anxiety, and sleep changes are common when tapering off the medication. They usually begin within a few days, peak in the first two weeks, and improve steadily with time. Knowing this timeline helps reduce fear and uncertainty.
-
A gradual taper with medical support is the safest path forward. Stopping suddenly makes withdrawal harder and riskier. Working with a doctor ensures dose reductions are done carefully, while also monitoring for the return of depression or anxiety. This approach minimizes discomfort and protects long-term mental health.
-
Recovery is about more than stopping the medication—it’s about building stability. Coping strategies like sleep hygiene, exercise, balanced nutrition, therapy, and family support all play an important role. With planning, persistence, and the right guidance, withdrawal can be managed safely, and a healthier future is possible.
Mirtazapine Withdrawal: An Overview
Mirtazapine, sold under the brand name Remeron, is an antidepressant commonly prescribed for major depressive disorder, anxiety, and insomnia. It works by altering levels of brain chemicals such as serotonin and norepinephrine, helping regulate mood and sleep [1].
Because it directly influences brain chemistry, stopping Mirtazapine too quickly can trigger a set of physical and psychological reactions known as withdrawal or “antidepressant discontinuation syndrome.” These reactions happen because the brain needs time to adapt once the drug is removed [2].
Recognizing these as withdrawal—not a sudden relapse of depression—is important. It helps individuals and their families understand that symptoms are temporary and usually resolve with proper tapering [3].
The critical point is that withdrawal is not the same as addiction. Mirtazapine is not addictive in the sense of causing cravings, but the body does adapt to its presence. That adaptation is why tapering under medical supervision is recommended for anyone planning to stop the medication [4].
Common Symptoms of Mirtazapine Withdrawal
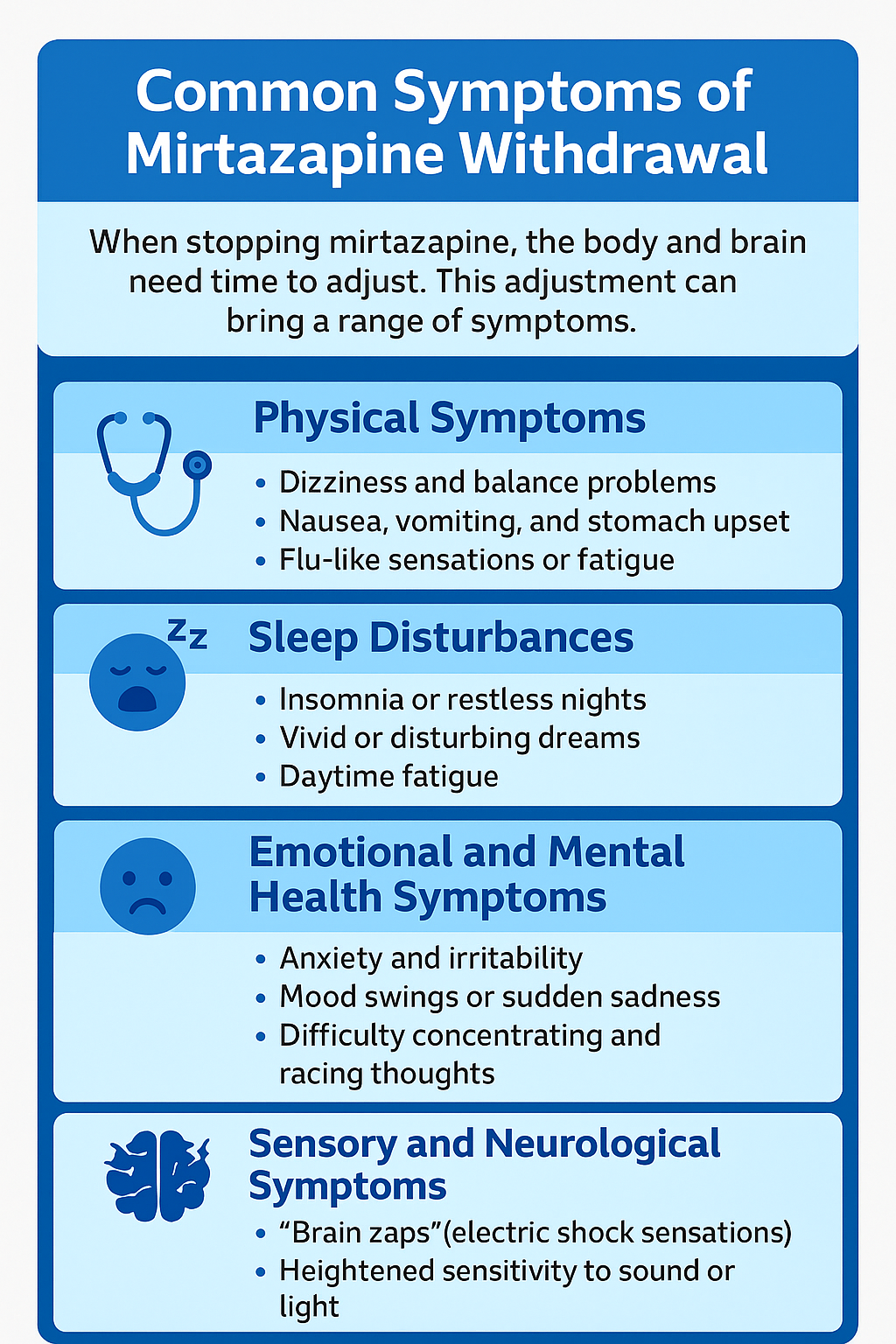
When stopping Mirtazapine, the body and brain need time to adjust. This adjustment can bring a range of symptoms that affect both physical health and emotional well-being. While not everyone will experience all of them, knowing what to expect reduces fear and helps you prepare [1][2].
Physical Symptoms
-
Dizziness and balance problems are often reported in the first few days of withdrawal.
-
Nausea, vomiting, and stomach upset may occur as the digestive system adjusts.
-
Flu-like sensations, headaches, or fatigue can leave the body feeling weak and run-down.
Physical symptoms are usually the first to appear and can make even simple tasks difficult. They are temporary but can be distressing if someone is unprepared for them. Staying hydrated, resting, and seeking medical advice when needed can make these more manageable.
Sleep Disturbances
-
Insomnia or restless nights are very common during the early weeks.
-
Vivid or disturbing dreams may replace the deeper, sedative sleep Mirtazapine once provided.
-
Daytime fatigue often follows poor sleep, making recovery feel harder.
Because Mirtazapine strongly affects sleep, stopping it often disrupts the body’s natural rhythms. Sleep issues usually peak in the first two weeks but gradually improve as the brain reestablishes balance (3).
Emotional and Mental Health Symptoms
-
Anxiety and irritability can rise sharply during withdrawal.
-
Mood swings or sudden sadness may resemble a return of depression.
-
Difficulty concentrating and racing thoughts are also reported by many.
These emotional changes can feel overwhelming, but they do not mean recovery is impossible. Distinguishing between withdrawal effects and a true relapse of depression is important—this is where medical guidance is essential.
Sensory and Neurological Symptoms
-
“Brain zaps” or electric-shock-like sensations are described by some people.
-
Heightened sensitivity to sound or light can make daily life uncomfortable.
-
Restlessness or shaking may also occur in more severe cases.
Though unusual, neurological symptoms highlight the brain’s effort to rebalance after relying on Mirtazapine for chemical regulation. They typically lessen as the nervous system adjusts.
Mirtazapine Withdrawal Timeline: What to Expect?
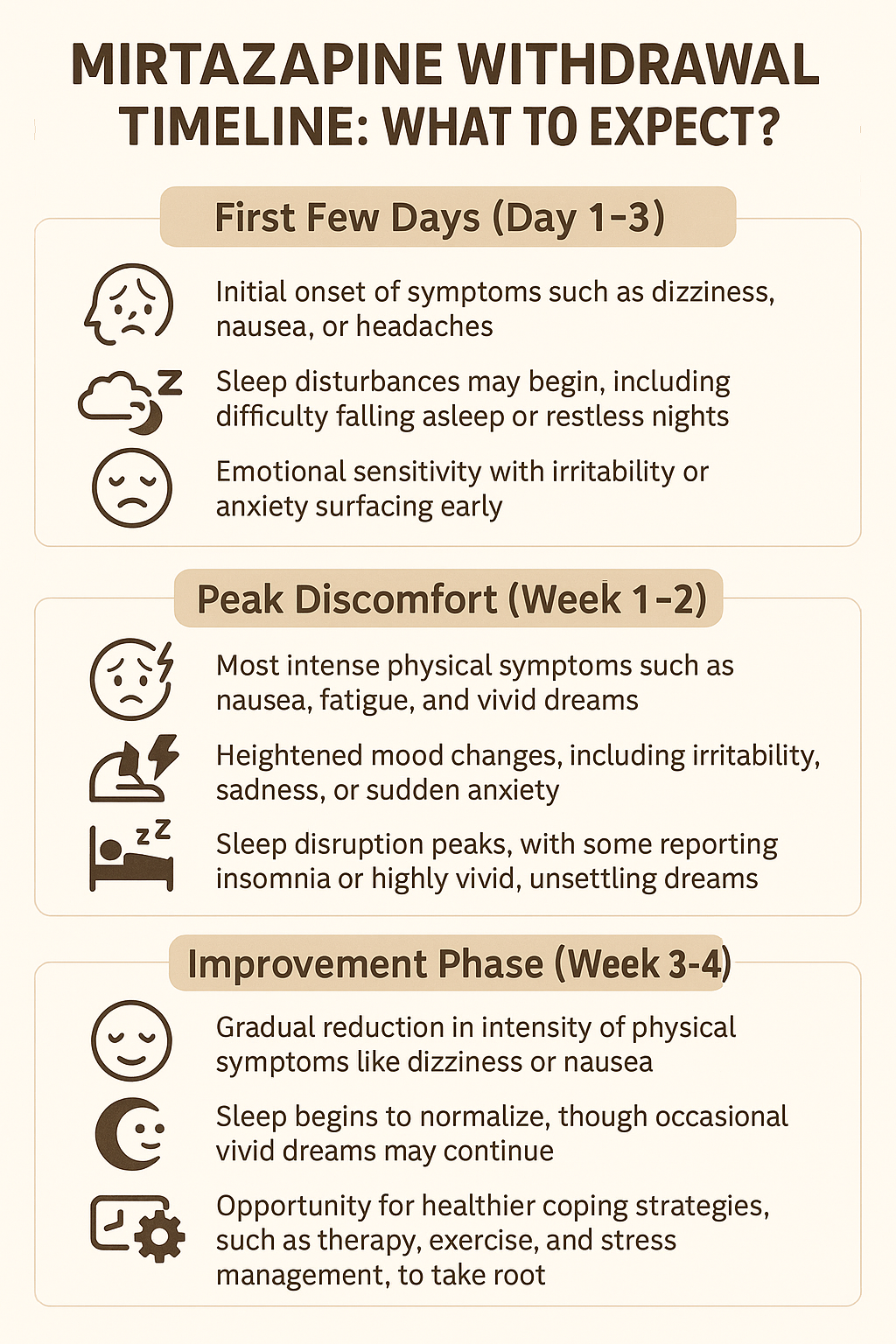
Mirtazapine withdrawal often follows a predictable course. While each person’s experience is unique, most report symptoms beginning within days, peaking in the first weeks, and then tapering over time [1][2].
First Few Days (Day 1–3)
-
Initial onset of symptoms such as dizziness, nausea, or headaches.
-
Sleep disturbances may begin, including difficulty falling asleep or restless nights.
-
Emotional sensitivity with irritability or anxiety surfacing early.
During the first few days, withdrawal can start quickly, especially if the medication is stopped suddenly. The brain, having relied on Mirtazapine to regulate serotonin and norepinephrine, begins adjusting to the absence. Symptoms at this stage are often mild but noticeable enough to cause concern.
Peak Discomfort (Week 1–2)
-
Most intense physical symptoms such as nausea, fatigue, and vivid dreams.
-
Heightened mood changes, including irritability, sadness, or sudden anxiety.
-
Sleep disruption peaks, with some reporting insomnia or highly vivid, unsettling dreams.
This is often the hardest phase for many people. The body is in active readjustment mode, and both physical and emotional symptoms feel strongest. Knowing this is a predictable stage helps reduce fear and encourages patients to push through rather than give up.
Improvement Phase (Week 3–4)
-
Gradual reduction in intensity of physical symptoms like dizziness or nausea.
-
Sleep begins to normalize, though occasional vivid dreams may continue.
-
Mood steadies, with anxiety and irritability beginning to ease.
By the third or fourth week, many people start noticing their symptoms lifting. Although progress is not always linear—good days may be followed by harder ones—the overall trend is improvement. Patience is critical, as the brain’s chemistry continues to stabilize.
Adjustment (Beyond 1 Month)
-
Lingering but less severe symptoms such as mild fatigue or occasional mood swings.
-
Return of baseline mental health symptoms like depression or anxiety in some individuals.
-
Opportunity for healthier coping strategies, such as therapy, exercise, and stress management, to take root.
For some, withdrawal symptoms fade completely after a few weeks. Others may notice lingering effects for a month or more, especially if they were on a high dose or used the medication long-term.
At this stage, ongoing self-care and professional guidance are key to maintaining recovery and preventing relapse.
Safe Approaches to Quitting Mirtazapine
Quitting Mirtazapine safely requires planning. Stopping suddenly—also called “going cold turkey”—can make withdrawal symptoms worse and increase the risk of relapse. The safest path is gradual tapering under medical supervision [2][3].
Why Tapering Is Safer Than Cold Turkey?
-
Cold turkey risks: Abruptly stopping Mirtazapine often leads to intense dizziness, nausea, anxiety, or severe insomnia. Some may also experience a sharp return of depression or anxiety symptoms.
-
Tapering benefits: A gradual dose reduction allows the brain more time to adjust. This significantly lowers withdrawal intensity and helps prevent emotional setbacks (3,4).
How Tapering Usually Works?
There’s no one-size-fits-all plan, but common tapering strategies include:
-
Small dose reductions: Doctors may lower the dose slowly over several weeks.
-
Longer taper schedules: For long-term users, tapering can take months to keep symptoms manageable.
-
Flexible adjustments: Tapering speed is adjusted based on how your body responds, not a fixed calendar (1,3).
The Role of Medical Supervision
A doctor’s guidance is crucial for:
-
Monitoring withdrawal symptoms as they appear.
-
Adjusting taper speed if side effects become difficult.
-
Watching for signs of relapse in depression or anxiety.
-
Providing reassurance and support throughout the process [2][6].
Coping Strategies for Managing Withdrawal
Even when tapering is done correctly, Mirtazapine withdrawal can bring difficult days. Using effective coping strategies can ease symptoms, improve daily functioning, and give you more control during the transition [2][4].
Focus on Sleep Hygiene
Insomnia and vivid dreams are among the most disruptive withdrawal symptoms. To support healthier sleep:
-
Stick to a consistent bedtime and wake-up routine so your body relearns a natural rhythm.
-
Reduce screen exposure and bright lights before bed, as these overstimulate the brain and delay rest.
-
Create a calming pre-sleep ritual such as reading, light stretching, or guided meditation to signal to your body that it’s time to wind down [2].
Support Your Body with Nutrition and Hydration
Your physical health directly influences how you feel during withdrawal. Practical steps include:
-
Eating balanced meals with proteins, complex carbs, and healthy fats to keep blood sugar steady and prevent mood swings.
-
Staying hydrated throughout the day to reduce fatigue, headaches, and digestive discomfort.
-
Limiting caffeine and alcohol, as these substances can intensify anxiety, worsen sleep issues, and prolong withdrawal discomfort [4].
Stay Physically Active
Exercise helps regulate mood and reduce withdrawal-related stress:
-
Light daily movement, such as walking or stretching, can improve circulation and ease tension in the body.
-
Moderate exercise like cycling, jogging, or swimming releases endorphins that stabilize mood and combat irritability.
-
Consistency is more important than intensity, so aim for manageable activities rather than pushing yourself too hard (5).
Practice Stress and Anxiety Management
Withdrawal often magnifies emotional stress, so proactive management is essential:
-
Mindfulness practices such as deep breathing or body scans help ground you when anxiety spikes.
-
Journaling about daily experiences and symptoms can make triggers easier to spot and reduce emotional overload.
-
Therapy or structured counseling support provides coping tools, reassurance, and an outlet for discussing setbacks [3][6].
Build a Support Network
Isolation can make withdrawal feel unbearable. Strong support improves resilience:
-
Share your goals with a trusted friend or family member, so they can check in and encourage you.
-
Join peer groups or online communities where others going through withdrawal share strategies and encouragement.
-
Avoid secrecy and self-isolation, which often make symptoms feel more overwhelming and recovery harder to sustain [6].
Maintain a Structured Daily Routine
-
Keep consistent meal and activity times, which stabilize energy levels and reduce withdrawal-related anxiety.
-
Plan tasks or activities ahead of time to avoid long stretches of unstructured downtime that may worsen restlessness or negative thoughts.
-
Balance productivity with rest, making sure recovery is sustainable and not exhausting.
Consider Professional Support Options
-
Cognitive Behavioral Therapy (CBT) or other short-term counseling can provide practical tools for handling mood swings and anxiety.
-
Check-ins with a primary care provider ensure that symptoms are being monitored and tapering remains safe.
-
Medication adjustments may be recommended if withdrawal becomes too severe or if mental health relapse risks increase [3].
When to Seek Medical Help?
Most people experience Mirtazapine withdrawal as uncomfortable but temporary. Still, there are times when symptoms signal something more serious. Knowing these red flags ensures withdrawal remains safe and manageable.
Severe Emotional or Mental Health Symptoms
If withdrawal triggers overwhelming depression, panic, or thoughts of self-harm, medical help is urgent. These signs may overlap with withdrawal but can also indicate a relapse of the original condition. Immediate support from a doctor or mental health provider keeps you safe and ensures your treatment plan is adjusted appropriately [3].
Disturbing Reactions and Intense Agitation
Hallucinations, paranoia, or extreme agitation are not typical withdrawal effects. If these symptoms appear, they should never be ignored. A healthcare professional can evaluate whether they are caused by withdrawal, another medical issue, or an underlying mental health concern that needs attention [2].
Struggling With Daily Functioning
Mild discomfort is common, but withdrawal should not prevent you from handling daily life. If symptoms make it impossible to attend school or work, manage responsibilities, or care for yourself, it is time to reach out. Doctors can provide tools to ease symptoms and help you regain stability [4].
Prolonged or Worsening Symptoms
Most withdrawal symptoms ease within a few weeks. If your discomfort continues beyond a month, or if symptoms become more intense instead of fading, professional support is necessary. Your doctor may slow the taper, adjust your dosage, or explore supportive therapies to improve comfort and safety [5].
Physical Red Flags
Though less common, some people may experience severe dizziness, rapid heart rate, or extreme nausea and vomiting. These symptoms can lead to dehydration or other complications and should be checked promptly by a healthcare provider.
Long-Term Recovery and Next Steps
Once withdrawal eases, the next stage is adjusting to daily life without Mirtazapine. This means learning how your body and mind function naturally and building confidence in handling sleep and mood without medication.
Ongoing monitoring is important. Some people remain stable, while others notice the return of depression or anxiety. Regular check-ins with a doctor or therapist provide reassurance and allow quick adjustments if needed.
Support makes recovery more sustainable. Family encouragement, peer groups, or counseling help reduce isolation and provide tools to manage setbacks. With steady support, recovery becomes less about withdrawal and more about creating a healthy, balanced future.
Conclusion
Quitting Mirtazapine is a process, not a single decision. Withdrawal symptoms can be uncomfortable, but they are temporary and manageable when you approach them with preparation and support.
The most important step is to work with your doctor on a safe tapering plan. Reducing the dose gradually allows your brain and body to adjust without overwhelming side effects. Never feel you have to handle this process on your own.
While symptoms like dizziness, nausea, or mood swings may appear, they usually improve within weeks. Healthy routines—consistent sleep, balanced nutrition, exercise, and stress management—help reduce discomfort and speed recovery.
For some, therapy or counseling provides added tools to cope with emotional changes. Family and friends can also play a vital role, offering encouragement and stability during difficult days.
If at any point symptoms become severe or if depression and anxiety return in full force, reach out for medical support immediately. Safety and stability are always the priority.
Commonly Asked Questions About Remeron Withdrawal
Stopping suddenly is not recommended. Going cold turkey increases the risk of severe withdrawal symptoms like insomnia, nausea, or anxiety. A slow, doctor-guided taper is the safest approach to minimize discomfort and keep your recovery on track.
For most people, symptoms appear within a few days, peak during the first two weeks, and fade over several weeks. Some may notice lingering effects for a month or longer, depending on dosage, duration of use, and overall health.
Underlying conditions can return once Mirtazapine is out of your system. This is why ongoing mental health support—through therapy, lifestyle changes, or alternative treatments—is so important during and after withdrawal.
Yes. Doctors may suggest supportive therapies like sleep hygiene routines, counseling, or, in some cases, short-term medications to manage severe discomfort. Non-medication approaches such as mindfulness, exercise, and balanced nutrition also make withdrawal easier to handle.
Family or friends can help by being patient, checking in regularly, and encouraging healthy routines. Just knowing someone is there to listen and support can make the process feel less isolating.
If symptoms interfere with daily functioning or cause emotional distress, reach out to your doctor immediately. Medical support can adjust the taper, provide symptom relief, and ensure your safety throughout the process.







