Suboxone Addiction: Signs, Symptoms, Withdrawal, and Treatment
Suboxone addiction occurs when individuals misuse Suboxone seeking its effects on mood and physical sensations. Suboxone is intended for recovery and misuse leads to dependency, creating physical and psychological challenges that require focused treatment to address and overcome. Approximately 1.7 million individuals aged 12 or older in the United States reported misusing buprenorphine products, including Suboxone, according to the 2021 National Survey on Drug Use and Health (NSDUH) conducted by the Substance Abuse and Mental Health Services Administration (SAMHSA).
Suboxone addiction occurs when individuals misuse Suboxone seeking its effects on mood and physical sensations. Suboxone is intended for recovery and misuse leads to dependency, creating physical and psychological challenges that require focused treatment to address and overcome. Approximately 1.7 million individuals aged 12 or older in the United States reported misusing buprenorphine products, including Suboxone, according to the 2021 National Survey on Drug Use and Health (NSDUH) conducted by the Substance Abuse and Mental Health Services Administration (SAMHSA).
The signs of Suboxone addiction include behaviors such as doctor shopping to obtain additional prescriptions, hiding or lying about Suboxone use, and neglecting personal or professional responsibilities. These signs also involve isolating from loved ones, obsessing over obtaining the medication, and consistently taking doses larger than prescribed, disrupting daily routines and obligations. Many individuals believe buprenorphine is less addictive than other opioids, such as methadone. All controlled substances, including buprenorphine, carry risks of misuse, dependence, and addiction, according to “Drugs of Abuse: A DEA Resource Guide,” published by the Drug Enforcement Administration in 2020.
Symptoms of Suboxone addiction appear both physically and mentally, with individuals experiencing drowsiness, nausea, confusion, and shifts in mood, along with persistent cravings and anxiety. These symptoms progress over time, leading to significant lifestyle and health changes as dependency on Suboxone deepens.
Withdrawal from Suboxone brings physical symptoms such as sweating, muscle aches, nausea, and powerful cravings. Psychological effects like irritability, anxiety, and depression accompany these physical symptoms, making the withdrawal process challenging without structured support. Suboxone withdrawal symptoms typically begin 36 to 72 hours after the last dose and can last up to several weeks according to the U.S. Food and Drug Administration (FDA).
Treatment for Suboxone addiction includes medically supervised detox to manage withdrawal symptoms in a safe environment. After detox, individuals engage in behavioral therapies such as cognitive-behavioral therapy, counseling, and support groups, addressing underlying causes of addiction, strengthening coping skills, and establishing a lasting foundation for recovery.
What is Suboxone Addiction?
Suboxone addiction is a type of substance use disorder and drug addiction that involves the compulsive use of Suboxone, a medication prescribed to treat opioid dependence. Individuals develop an addiction to Suboxone when they use it beyond prescribed limits (max dose 24 mg per day) or seek its effects rather than its intended therapeutic purpose. Suboxone addiction is characterized by a physical and psychological dependence on the drug, where users experience cravings, heightened tolerance, and an inability to control their intake.
People most likely to develop Suboxone addiction include those with a history of opioid misuse or substance use disorders. Misuse of buprenorphine can lead to moderate to low physical dependence and high psychological dependence, particularly among individuals with a history of substance abuse or those who try to self medicate. Such misuse increases the risks of addiction, overdose, or even death, according to Drugs.com research titled “Buprenorphine,” last updated in August 2023.
What is Suboxone?
Suboxone is a medication primarily used to treat opioid use disorder by reducing withdrawal symptoms and cravings. It combines two active ingredients—buprenorphine and naloxone—that work together to support recovery. Buprenorphine is a partial opioid agonist, which means it activates opioid receptors in the brain to relieve withdrawal symptoms and reduce cravings without producing the same intense euphoria as full opioids. Naloxone, an opioid antagonist, blocks opioid receptors and is included to prevent misuse, as it triggers withdrawal symptoms if Suboxone is injected rather than taken as prescribed.
The overall national buprenorphine dispensing rate was 4.8 buprenorphine prescriptions dispensed per 100 persons. This amounted to a total of more than 16 million buprenorphine prescriptions dispensed across the United States in 2022 according to the Centers for Disease Control and Prevention (CDC), in 2022.
Here are the details about Suboxone:
|
Dosage Stage |
Dose |
Method of Ingestion |
Notes |
|
Induction (Day 1) |
2 mg/0.5 mg to 8 mg/2 mg |
Sublingual (under tongue) |
Placed under the tongue until dissolved. Maximum first day dose: 8 mg/2 mg |
|
Induction (Day 2) |
Up to 16 mg/4 mg |
Sublingual |
Single daily dose, based on withdrawal symptoms |
|
Maintenance |
4 mg/1 mg to 24 mg/6 mg daily |
Sublingual or Buccal |
Target dosage: 16 mg/4 mg as a single daily dose |
|
Maximum Daily Dose |
24 mg/6 mg |
Sublingual or Buccal |
Not to be exceeded |
What are the Signs, Symptoms and Side Effects of Suboxone?
The signs, symptoms, and side effects of Suboxone addiction are both physical and psychological. Suboxone addiction affects the body and mind, creating physical discomfort and interfering with mental well-being. Suboxone misuse leads to physical withdrawal symptoms as well as psychological dependence, making recovery challenging and increasing the likelihood of relapse.
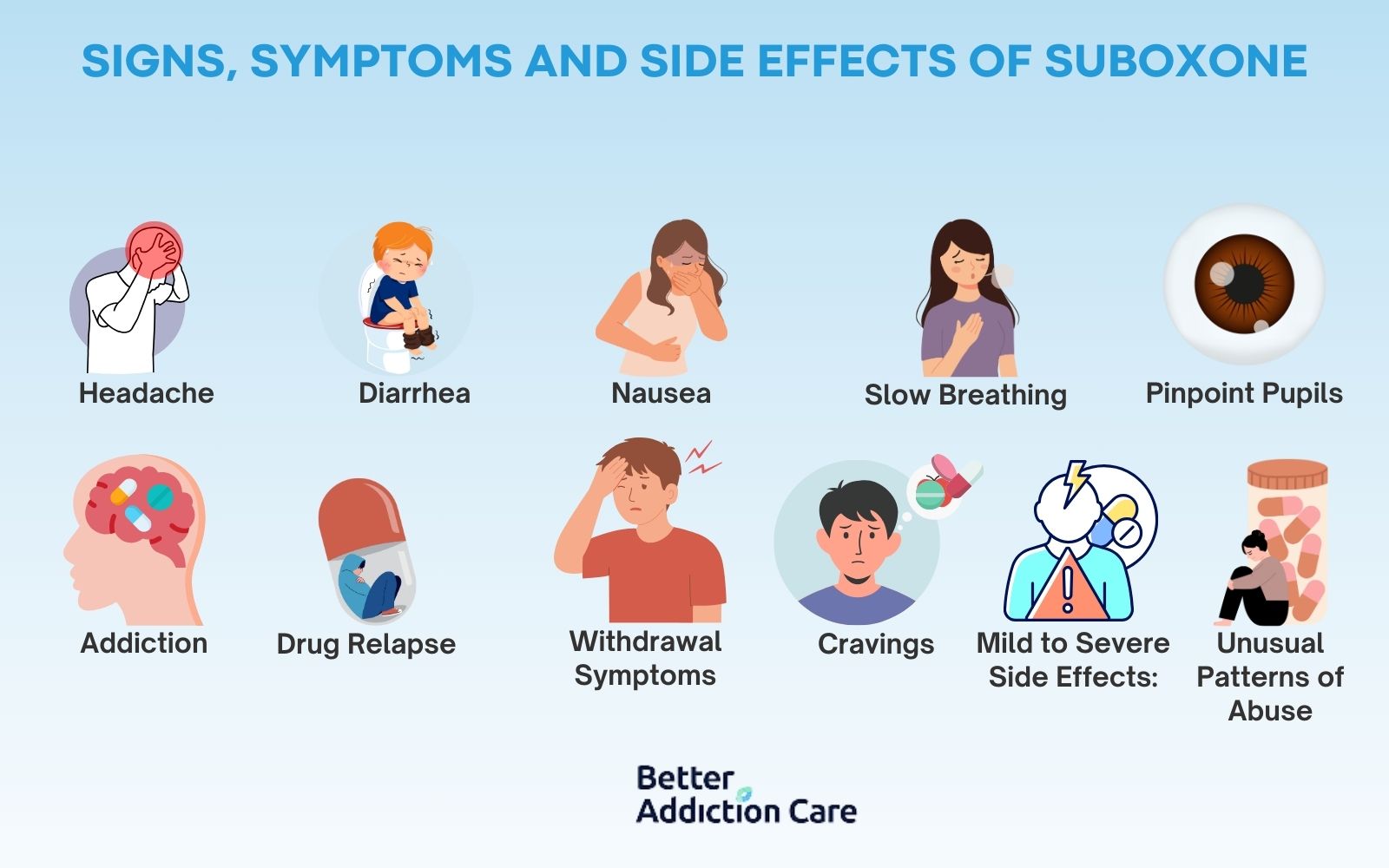
The signs, symptoms and side effects of Suboxone are detailed below:
-
Headache: Headaches are a common physical side effect of Suboxone addiction, resulting from the body’s response to the drug or withdrawal. This type of pain occurs as the drug disrupts normal neurological functions, leading to tension and discomfort. For many users, the headaches are persistent, impacting daily life and concentration, making it difficult to focus on tasks.
-
Diarrhea: Diarrhea is a physical symptom and occurs as the body struggles to adjust to Suboxone, especially during withdrawal. Diarrhea happens due to the effects of Suboxone on the gastrointestinal tract, which becomes sensitive or reactive during withdrawal. This symptom, while manageable, causes significant discomfort and dehydration if left untreated.
-
Nausea: Nausea is a physical side effect associated with Suboxone addiction and withdrawal. It often results from changes in the brain's response to the drug and disruptions in the digestive system. Nausea is typically experienced as the body adjusts to a reduction or absence of Suboxone, especially in the early stages of detox. 40% of people develop nausea due to opioids, and up to 25% vomit after opioid intake according to Manza, P. 2024 “Opioids and Nausea: Everything You Need to Know”.
-
Slow Breathing: Slow breathing, or hypoventilation, is a physical symptom of Suboxone addiction caused by the central nervous system depressant effects of buprenorphine. Slow breathing occurs when individuals misuse Suboxone, taking excessive doses or combining it with other depressants, which amplifies its impact on the respiratory system. Suboxone effects slow the signals controlling breathing, leading to a reduced breathing rate, which poses significant health risks if not managed.
-
Pinpoint Pupils: Pinpoint pupils, or miosis, are a physical symptom of Suboxone addiction, resulting from the body’s response to opioids. Opioids stimulate the parasympathetic nervous system, which is responsible for constricting the pupils. This activation causes the pupillary sphincter muscle to contract, resulting in smaller pupils according to Peckham, A. 2024 in “How do opioids affect the eyes?” published by Medical News Today. This response prevents the pupils from adjusting to changes in light, which make environments with varied lighting uncomfortable for the individual.
-
Addiction: Addiction to Suboxone is a psychological sign marked by an uncontrollable urge to continue using the drug despite negative consequences. Addiction manifests as an intense need to consume Suboxone, resulting in behavioral changes, neglect of responsibilities, and compulsive use patterns. The psychological aspect of addiction is driven by changes in the brain's reward system, making it difficult for individuals to quit on their own.
-
Drug Relapse: Drug relapse is a psychological symptom of Suboxone addiction, where individuals return to use after attempting to quit. Relapse results from psychological dependency and withdrawal symptoms, making recovery challenging. Relapse is dangerous, as returning to a previous dosage increases the risk of overdose due to reduced tolerance.
-
Withdrawal Symptoms: Withdrawal symptoms are both physical and psychological, indicating the body’s dependence on Suboxone. Withdrawal symptoms occur when the drug is discontinued or dosage is reduced, leading to discomfort and cravings. Symptoms like nausea, headaches, and anxiety are common during withdrawal, underscoring the physical and psychological impact of Suboxone dependency. Suboxone withdrawal symptoms resemble those experienced during withdrawal from other opioids, including anxiety, depression, gastrointestinal issues like diarrhea and abdominal pain, headaches, nausea, vomiting, and fatigue, as noted by Drugs.com in “How long does Suboxone withdrawal last?” updated in March 2023.
-
Cravings: Cravings are a psychological symptom of Suboxone addiction, marked by an intense desire to use the drug. Cravings arise from changes in the brain’s reward pathways, reinforcing the need for Suboxone to feel normal. Cravings often contribute to relapse and hinder recovery efforts.
-
Unusual Patterns of Abuse: Unusual patterns of abuse, such as doctor shopping or attempting to obtain Suboxone from multiple sources, are behavioral signs of addiction. These actions indicate a psychological dependence on the drug and a growing need to maintain access to it. Such patterns reflect the compulsive nature of addiction, where individuals prioritize drug-seeking behaviors over other responsibilities. Opioids, including buprenorphine, had the highest rates of doctor-shopping among medications, highlighting a significant problem with the non-medical use of these substances according to a 2023 study by Soeiro T. et al., titled “Systematic assessment of non-medical use of prescription drugs using doctor-shopping indicators: A nation-wide, repeated cross-sectional study,”.
-
Mild to Severe Side Effects: Suboxone addiction includes a range of side effects, from mild symptoms like drowsiness to more severe psychological symptoms such as depression. These effects stem from the drug’s influence on brain chemistry, which impacts mood, perception, and overall mental health. Severe side effects are particularly concerning, as they increase the need for comprehensive addiction treatment.
When Does Suboxone Consumption Cause Addiction?
Suboxone consumption causes addiction when it is taken in higher doses (more than 8 mg per day) or for longer durations than prescribed. A typical therapeutic dose of Suboxone for opioid dependence usually ranges from 2 mg to 8 mg of buprenorphine daily, with doses above 8 mg considered high and more likely to lead to dependence. For men, higher doses are occasionally adjusted based on body mass and metabolism; for women, sensitivity to the drug results in lower thresholds for tolerance. If Suboxone is taken by injection or in larger quantities than prescribed—such as consuming 12 mg to 16 mg daily instead of the recommended 8 mg—addiction risks significantly increase.
Duration is also a factor in Suboxone addiction. Prescribers (Doctors and Therapists) typically recommend a treatment duration of 6 to 12 months, depending on individual recovery needs, with gradual tapering towards the end. Exceeding this timeframe without professional oversight or increasing the dose without approval leads to dependency, as the body adjusts to regular, prolonged exposure. For instance, maintaining a high dose beyond the recommended period, or for men and women taking doses above their personal thresholds (like 8 mg for most and lower for those with higher sensitivity), increases addiction risk due to the prolonged interaction with the brain’s opioid receptors.
The effectiveness of naloxone in Suboxone during diversion has recently been debated, as stated in the 2022 Frontiers in Psychiatry issue titled “Suboxone: History, controversy, and open questions.” Naloxone has a half-life of 2 to 12 hours, while buprenorphine has a half life of 24 to 42 hours, according to Suboxone’s FDA label. This discrepancy suggests that naloxone’s blocking effects may wear off before buprenorphine's agonistic effects, potentially allowing users to experience some drug-associated rewards, which can lead to subconscious reinforcement and sensitization through repeated exposure.
What is the Withdrawal Timeline for Suboxone?
The withdrawal timeline for Suboxone includes three stages (early withdrawal, acute withdrawal, protracted withdrawal), each marked by distinct symptoms and durations. The duration and severity of withdrawal symptoms vary depending on factors like the duration of use, dosage, and individual biological differences, though it is generally similar across male and female adults. Lifestyle, metabolism, and the presence of other substances slightly alters this timeline.
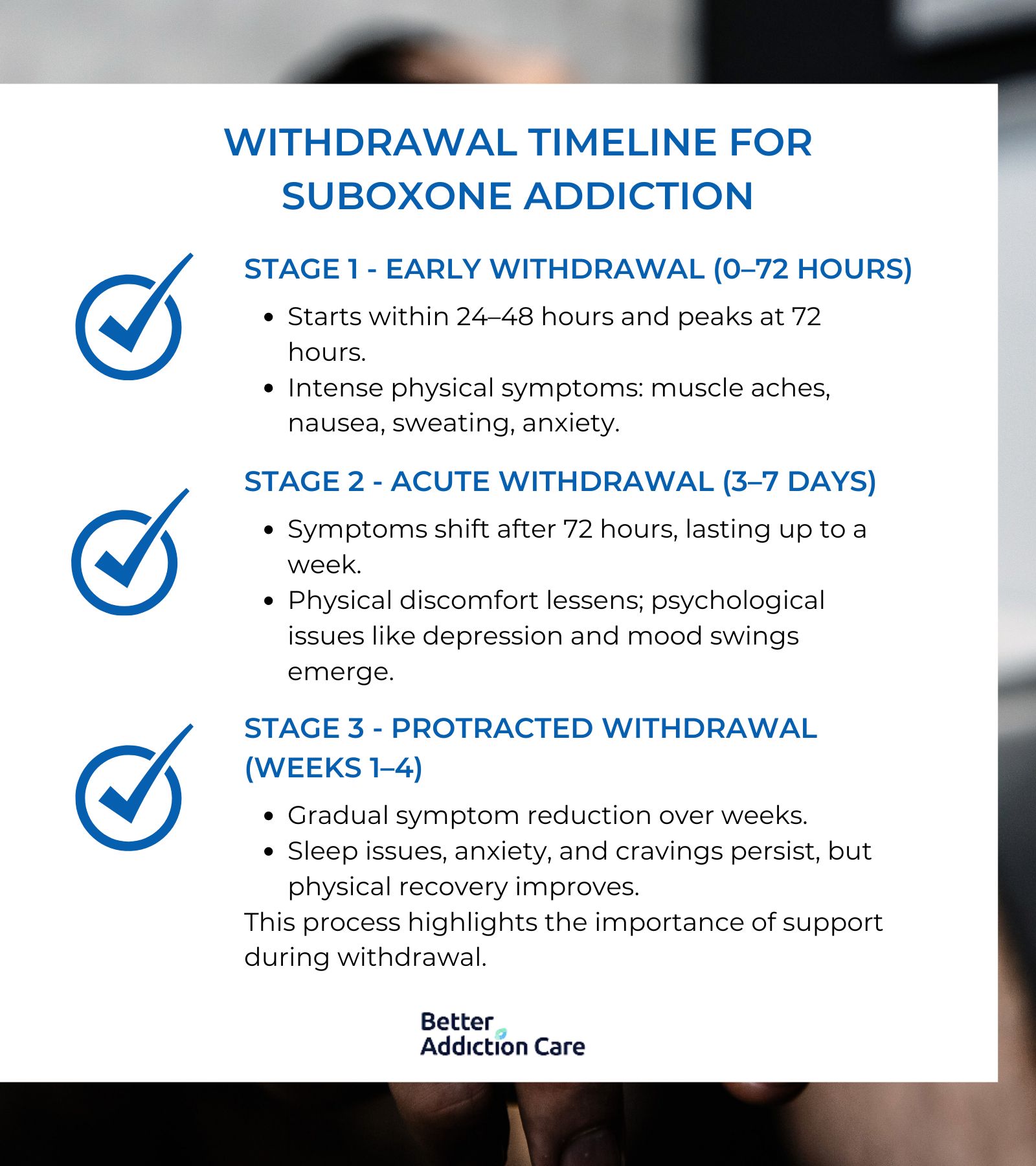
The withdrawal timeline for Suboxone addiction is written below:
-
Stage 1 - Early Withdrawal (0 to 72 Hours): The first stage of Suboxone withdrawal begins within 24 to 48 hours after the last dose and intensifies over the first three days. Symptoms during this period are primarily physical, including muscle aches, sweating, nausea, and anxiety. Some individuals also experience gastrointestinal distress and increased heart rate. This initial phase is often the most intense, peaking at around 72 hours before transitioning to the next stage.
-
Stage 2- Acute Withdrawal (3 to 7 Days): After 72 hours, the withdrawal symptoms shift into the acute stage, typically lasting from day three to around day seven. Physical symptoms tend to subside slightly, while psychological symptoms such as depression, irritability, and mood swings become more pronounced. Insomnia and fatigue also persist during this phase, making daily functioning challenging.
-
Stage 3- Protracted Withdrawal (Weeks 1 to 4); After the first week, symptoms begin to diminish in intensity, but lingering effects, like sleep disturbances, anxiety, and mood instability, continues for up to four weeks. This phase marks the body's gradual adjustment to the absence of Suboxone, with cravings and occasional bouts of restlessness persisting. By the end of the fourth week, most physical symptoms resolve, although psychological recovery continues beyond this period.
Medically supervised tapering, adequate hydration, a balanced diet, and mental health support are essential in managing and potentially reducing withdrawal duration. Supportive medications, such as clonidine or non-opioid pain relievers, also help alleviate symptoms, thus easing the process and potentially shortening the timeline for some individuals according to Kosten, T. R., & George, T. P. (2002). in "The Neurobiology of Opioid Dependence: Implications for Treatment." published by National Institutes of Health.
How to Treat Suboxone Addiction
To treat Suboxone addiction, requires a comprehensive approach that combines medical and psychological interventions to address both the physical dependency and underlying behavioral factors. Effective treatment involves medical supervision, gradual tapering, behavioral therapy, support groups, and co-occurring treatment for any related mental health disorders.
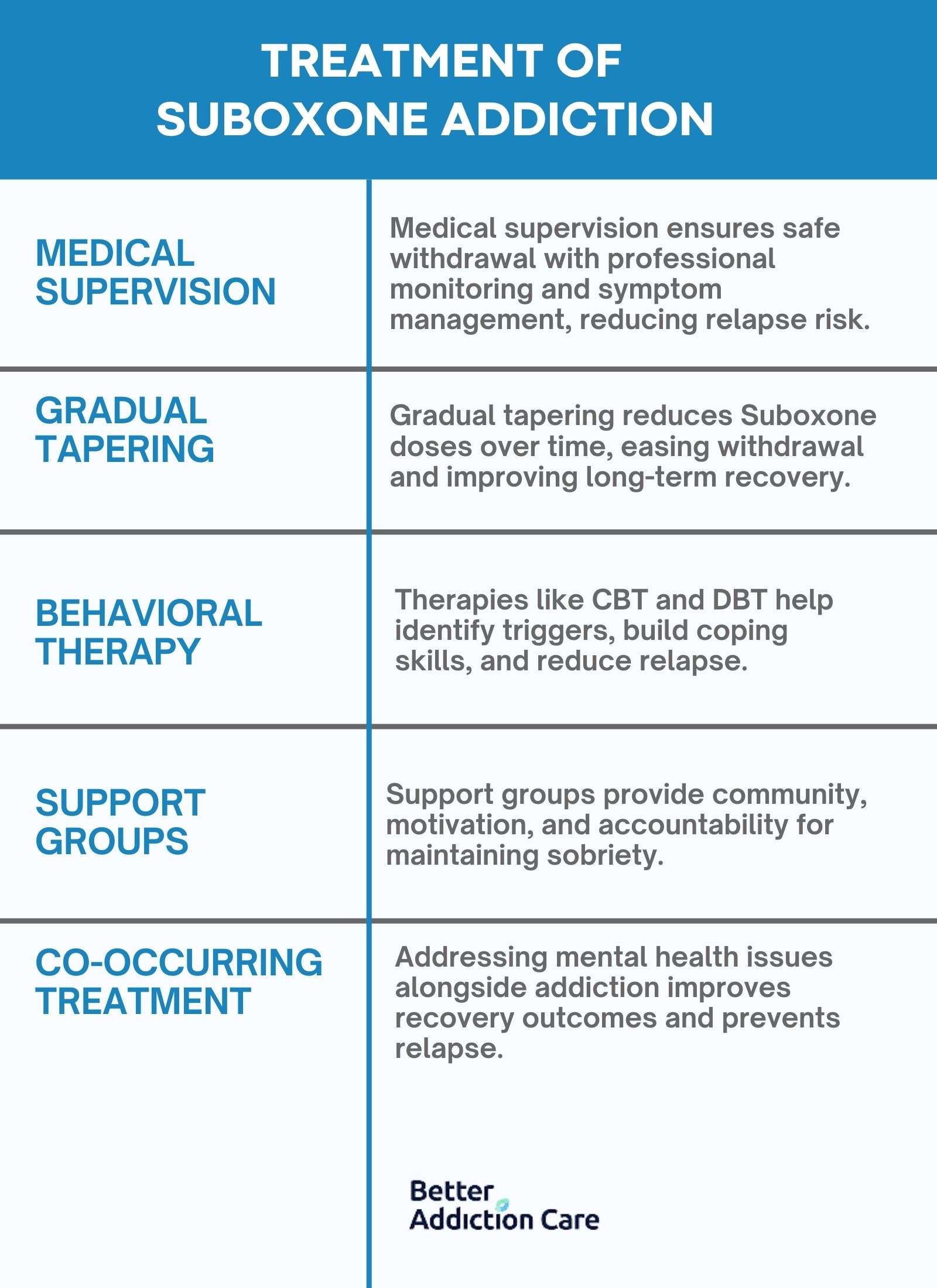
Here is a detailed list of treatments for Suboxone Addiction:
-
Medical Supervision: Medical supervision provides a safe and structured environment where healthcare professionals monitor withdrawal symptoms and manage potential complications. During medically supervised treatment, patients receive medications to alleviate withdrawal symptoms, reduce cravings, and stabilize their physical condition. This approach is highly effective in ensuring a safer withdrawal process, reducing the risk of relapse by offering continuous support and medical intervention as needed.
-
Gradual Tapering: Gradual tapering involves slowly reducing the dosage of Suboxone under medical guidance to minimize withdrawal symptoms and cravings. Tapering helps the body adjust gradually to lower levels of the drug, reducing the intensity of physical and psychological symptoms. This method is efficient in preventing abrupt withdrawal effects and is often customized based on the patient’s response, making it a preferred approach for long-term success in treating Suboxone addiction. A 2013 study examined the effectiveness of various buprenorphine taper durations among individuals primarily abusing prescription opioids. The findings revealed that a 4 week taper regimen produced significantly better outcomes than the shorter 1 and 2 week tapers. This extended duration also led to higher rates of treatment retention and increased adherence to naltrexone, both critical elements in achieving successful addiction recovery according to titled “A Randomized, Double-Blind Evaluation of Buprenorphine Taper Duration in Primary Prescription Opioid Abusers,” published by JAMA Psychiatry.
-
Behavioral Therapy: Behavioral therapy, such as Cognitive Behavioral Therapy (CBT) or Dialectical Behavior Therapy (DBT), addresses the psychological components of addiction. These therapies help individuals identify triggers, develop coping strategies, and modify harmful behaviors associated with drug use. Behavioral therapy is highly effective for sustaining recovery by providing patients with the tools to manage stress, avoid relapse, and improve overall mental health, making it a cornerstone of addiction treatment. Combining CBT with pharmacotherapy is more effective than either usual care or pharmacotherapy alone. Although CBT did not surpass other evidence-based approaches in isolation, it proved to be a vital element of an effective combined treatment strategy according to the 2020 study led by Ray L.A. et al. titled “Combined Pharmacotherapy and Cognitive Behavioral Therapy for Adults With Alcohol or Substance Use Disorders: A Systematic Review and Meta-analysis,” .
-
Support Groups: Support groups, such as Narcotics Anonymous (NA) or specialized Suboxone support meetings, offer a community environment where individuals share experiences, gain support, and stay accountable in their recovery journey. Support groups enhance motivation and provide a sense of belonging, which are crucial for maintaining sobriety. While support groups are not a replacement for professional treatment, they are highly efficient as an ongoing support mechanism, helping reduce feelings of isolation and building resilience.
-
Co-occurring Treatment: Many individuals with Suboxone addiction also face co-occurring mental health disorders, such as anxiety or depression. Co-occurring treatment addresses these mental health issues simultaneously with addiction treatment, improving overall outcomes. Treating both conditions concurrently is essential for sustainable recovery, as untreated mental health issues lead to relapse. This integrated approach is effective in providing a comprehensive solution for individuals struggling with both addiction and mental health challenges.
How Is Suboxone Regulated in the US?
Suboxone is regulated in the United States as a Schedule III controlled substance under the Controlled Substances Act. This classification indicates a moderate to low potential for physical and psychological dependence. The Drug Enforcement Administration (DEA) is primarily responsible for enforcing regulations surrounding Suboxone, particularly due to its active ingredient, buprenorphine, which requires careful oversight to prevent misuse and diversion.
The regulation of buprenorphine underwent a significant change with the passage of the Mainstreaming Addiction Treatment (MAT) Act of 2022 and Section 1262 of the Consolidated Appropriations Act, 2023. These legislative updates removed previous restrictions that required providers to obtain a special waiver to prescribe buprenorphine for opioid use disorder, aiming to expand access to treatment for individuals in need.
What Is Suboxone Used For?
Suboxone is used for treatment of opioid dependence by reducing withdrawal symptoms and cravings. Suboxone serves both as a long-term maintenance treatment and as a transitional support during detoxification. Suboxone is prescribed to individuals with hypersensitivity to opioids such as oxycodone, acetaminophen, or morphine, providing an effective alternative. Suboxone is a main component of medication-assisted treatment (MAT), proven to reduce relapse rates. In cases of misuse, some individuals with substance use disorder attempt to crush or dissolve Suboxone to bypass its effects; however, the naloxone component deters misuse.
What Is the Chemical Composition of Suboxone?
Suboxone’s chemical composition is a fixed-dose combination of buprenorphine and naloxone in a 4:1 ratio. Buprenorphine, with the molecular formula C19H21NO4, acts as a partial agonist at the μ-opioid receptor, relieving cravings and withdrawal symptoms without the intense euphoria associated with full opioid agonists. Naloxone hydrochloride dihydrate, with the molecular formula C19H21NO4 • HCl • 2H2O, functions as a non-selective competitive opioid receptor antagonist. This combination (Buprenorphine and Naloxone) provides therapeutic benefits for opioid addiction treatment while preventing misuse.
Can You Overdose on Suboxone?
Yes, you can overdose on Suboxone, especially when someone exceeds the recommended dosage. For adults, typical therapeutic doses range from 2 mg to 24 mg of buprenorphine per day, depending on the stage of treatment and individual needs. Exceeding 24 mg significantly raises the risk of overdose, though individual tolerance and body weight are factors. Dosage guidelines are generally the same for men and women, as both respond similarly to the effects of buprenorphine.
Buprenorphine in Suboxone, as a partial opioid agonist, has a "ceiling effect," meaning it produces a limited euphoria compared to full opioids. The ceiling effect reduces, but does not eliminate, the risk of respiratory depression at higher doses, which still leads to overdose, particularly when Suboxone is combined with other depressants. Buprenorphine, the active ingredient in Suboxone, was involved in only a small fraction of opioid overdose deaths. Between July 2019 and June 2021, buprenorphine was implicated in 1,955 overdose deaths, representing 2.6% of the 74,474 opioid-related deaths recorded according to a 2023 study published in JAMA Network Open.
What Happens If You Take Too Much Suboxone?
If you take too much Suboxone (more than 24 mg of buprenorphine in a single day) it will lead to overdose symptoms, including respiratory depression, confusion, and sedation. Combining Suboxone with other central nervous system (CNS) depressants like benzodiazepines, alcohol, or other opioids significantly increases the risk of severe respiratory depression, coma, or death. For instance, mixing 2 mg of Suboxone with 0.5 mg of Xanax, or 4 mg of Suboxone with just two standard alcoholic drinks, amplifies sedative effects. Even low-dose combinations, such as 2 mg of Suboxone with 5 mg of oxycodone, are dangerously potent, as these mixtures heighten respiratory and sedative risks, posing serious health threats.
How Long Does It Take to Get Addicted to Suboxone?
It takes 2 weeks of daily use to get addicted to Suboxone depending on dosage and individual factors. For instance, taking Suboxone at 8 mg or higher per day for more than two weeks increases the likelihood of dependency. Higher doses and extended use periods will accelerate the development of addiction, as the body builds a tolerance more quickly at these levels.
Can Suboxone Cause an Overdose?
Yes, Suboxone can cause an overdose because buprenorphine, its active ingredient, is a long-acting opioid agonist. Overdose leads to respiratory depression, extreme sedation, and loss of consciousness. Mixing Suboxone with other central nervous system depressants, such as benzodiazepines or alcohol, further increases the risk of overdose.
What Is the Dosage for Suboxone?
The dosage for Suboxone ranges from 2 mg to 24 mg daily. It is typically administered as a sublingual film or tablet once per day, although some treatment plans start with twice-daily dosing according to the 2024 “Suboxone Dosage Guide” published by Drugs.com. The maximum recommended dose should not exceed 24 mg per day. Dosage does not differ between male and female adults but is adjusted according to individual needs and treatment response.
Does Suboxone Treat Opiate Withdrawal?
Yes, Suboxone does treat opiate withdrawal because it contains buprenorphine, which binds to opioid receptors to reduce withdrawal symptoms without causing intense euphoria. Suboxone’s partial agonist effect at opioid receptors provides just enough stimulation to prevent cravings, making it easier to maintain sobriety. The long half-life of buprenorphine in Suboxone stabilizes withdrawal symptoms, allowing for once-daily dosing that provides consistent relief over 24 hours.
Does Suboxone Make You High?
No, Suboxone does not make you high because buprenorphine in Suboxone is a partial agonist, meaning it only partially activates opioid receptors, which limits euphoria. Suboxone has a "ceiling effect," where increasing the dose beyond a certain point does not intensify effects, reducing the risk of misuse. The addition of naloxone deters misuse by causing withdrawal symptoms if Suboxone is injected rather than taken as prescribed.
Is Suboxone a Narcotic?
Yes, Suboxone is classified as a narcotic under U.S. federal law by the Drug Enforcement Administration (DEA). Suboxone contains buprenorphine, a controlled opioid that interacts with the central nervous system to relieve withdrawal symptoms and manage cravings, similar to other narcotics.
Does Suboxone Interact with Other Medications?
Yes, Suboxone interacts with various medications like antibiotics, benzodiazepines, opioids and alcohol. It interacts with certain antibiotics, such as erythromycin, levofloxacin, and clarithromycin, which alter its effects. CYP3A4 inhibitors like erythromycin increase buprenorphine’s bioavailability, raising the risk of side effects like sedation and respiratory depression according to Goodman and Gilman’s Manual of Pharmacology and Therapeutics written by Brunton et al., 2021.
Suboxone also has dangerous interactions with benzodiazepines (e.g., Xanax, Valium, Klonopin) is especially risky, as both classes depress the central nervous system (CNS). This can lead to extreme sedation, respiratory depression, and increased overdose potential according to research by Lembke et al., 2018 and published in the Journal of Clinical Psychiatry.
Combining Suboxone with other opioids—like oxycodone, hydrocodone, and morphine—can lead to respiratory depression and increase the potential for overdose. Opioid combinations create competition for opioid receptors, which can block intended therapeutic effects and heighten overdose potential. This is particularly dangerous because the added respiratory depressant effect compounds with each drug, resulting in an amplified risk to patient safety as stated by The National Institute on Drug Abuse (NIDA).
Suboxone combined with alcohol is dangerous because both substances act as CNS depressants. The American Society of Addiction Medicine (ASAM) indicates that this interaction heightens the sedative effects, increasing the chances of respiratory depression and accidental injury.
What Is the Difference Between Suboxone and Methadone?
The difference between Suboxone and Methadone is that methadone is a full opioid agonist while Suboxone is a partial agonist. Suboxone contains buprenorphine (C19H21NO4) and naloxone (C19H21NO4 • HCl • 2H2O), while methadone is solely composed of methadone hydrochloride (C21H27NO • HCl). Methadone is generally more addictive because it fully activates opioid receptors and produces stronger euphoria than Suboxone. Both medications serve as treatments for opioid addiction and help reduce cravings, but each has a distinct risk profile. Both Suboxone and methadone work by interacting with opioid receptors to manage withdrawal symptoms and cravings, but methadone’s full agonist nature contributes to a higher potential for dependency. The risk of fatal overdose is about 6 times lower with buprenorphine (in Suboxone) compared to methadone according to DerSarkission, C. 2024 in “What's the Difference Between Methadone and Suboxone?” published by WebMD.
Related Articles
Treatment Centers in Virginia










