Tizanidine (Zanaflex) Addiction Uses, Risks & Withdrawal
Tizanidine, sold under the brand name Zanaflex, is a centrally acting muscle relaxant approved for the treatment of spasticity, particularly in conditions such as multiple sclerosis, spinal cord injury, or other neurological disorders. [1]

Key Takeaways
-
Tizanidine misuse and dependence can develop quietly, especially when it’s used for sleep, anxiety relief, or pain beyond its intended purpose.
-
Tizanidine is not classically addictive, but abrupt discontinuation can cause rebound hypertension, tachycardia, and severe withdrawal symptoms, which may reinforce continued use.
-
Recovery and safe discontinuation are achievable with medical tapering, symptom management, and treatment of the underlying pain or muscle spasm that led to reliance.
Unlike benzodiazepines or opioids, tizanidine does not act on GABA or opioid receptors. Instead, it works as an alpha-2 adrenergic agonist, reducing excitatory nerve signals in the spinal cord. This decreases muscle tone and reflex activity but also produces sedation, blood pressure lowering, and calming effects.
Clinically, tizanidine is prescribed for:
-
Muscle spasticity related to neurological conditions
-
Painful muscle spasms and stiffness
-
Short-term musculoskeletal conditions (off-label)
Because of its sedating effects, tizanidine is frequently prescribed off-label for sleep, which increases the risk when long-term monitoring is limited.
Understanding how tizanidine fits into misuse and dependence requires clear definitions:
-
Tolerance — Some individuals require higher doses over time to achieve the same muscle relaxation or sedative effect.
-
Dependence — The body adapts to regular tizanidine exposure. Abrupt cessation can trigger clinically significant withdrawal, particularly cardiovascular symptoms.
-
Addiction — A behavioral syndrome involving compulsive use, craving, loss of control, and continued use despite harm.
Tizanidine does not reliably activate dopamine reward pathways, so classic addiction is uncommon — but behavioral dependence and misuse are well-documented.
Signs & Symptoms of Tizanidine Misuse
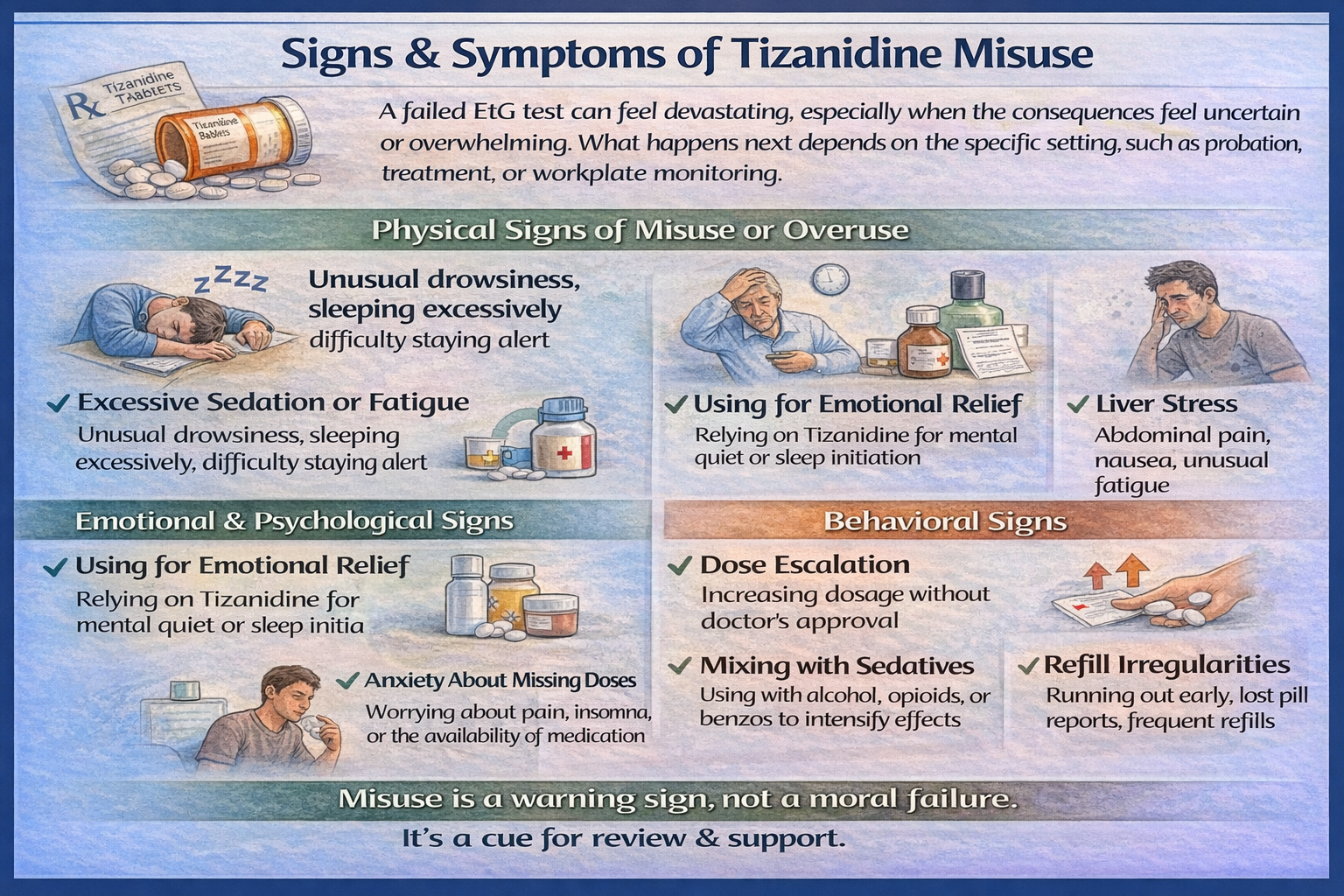
Physical Signs of Misuse or Overuse
-
Excessive Sedation or Fatigue: Using higher doses or taking tizanidine more frequently than prescribed can cause overwhelming drowsiness, prolonged periods of sleep, and difficulty staying alert during routine activities. Individuals may appear unusually slowed, struggle with concentration, or feel unable to function during the day, increasing the risk of accidents and impaired judgment.
-
Low Blood Pressure and Dizziness: Because tizanidine suppresses sympathetic nervous system activity, overuse can lead to significant drops in blood pressure, particularly when standing. [2] Symptoms may include lightheadedness, blurred vision, fainting, or falls—risks that are especially pronounced in older adults or those with cardiovascular conditions.
-
Slowed Heart Rate or Weakness: Excess dosing may result in bradycardia, generalized muscle weakness, and poor coordination. These effects can interfere with mobility, increase fall risk, and reduce the ability to perform tasks requiring balance or strength, even in otherwise healthy individuals.
-
Liver Stress: Tizanidine is metabolized by the liver, and elevated liver enzymes are a recognized risk with long-term or high-dose use. Without routine monitoring, liver stress may go unnoticed until symptoms such as fatigue, abdominal discomfort, or abnormal lab results emerge.
-
Withdrawal-Related Physical Symptoms: Missing doses or stopping suddenly can trigger rebound sympathetic activity, leading to high blood pressure, rapid heart rate, tremors, sweating, nausea, and agitation. These symptoms are often misinterpreted as worsening anxiety or medical relapse, when they actually reflect withdrawal physiology.
Emotional & Psychological Signs
-
Using Tizanidine for Emotional Relief: Some individuals gradually shift from using tizanidine for muscle symptoms to relying on it for emotional calming, mental quiet, or sleep initiation. This change often happens unintentionally and reflects relief-seeking behavior rather than recreational misuse.
-
Anxiety About Missing Doses: Fear of pain flares, blood pressure spikes, or insomnia can lead to rigid dosing schedules and preoccupation with medication availability. This anxiety is a common marker of physiologic dependence and nervous system adaptation.
-
Irritability or Restlessness Between Doses: Mood changes, agitation, or internal restlessness between doses often reflect withdrawal onset rather than addiction. However, these uncomfortable sensations can reinforce continued use and make tapering feel emotionally difficult without proper support.
Behavioral Signs
-
Dose Escalation Without Medical Approval: Taking additional tablets, shortening dosing intervals, or exceeding prescribed limits—often during stress or poor sleep—signals a shift away from therapeutic use and increases medical risk.
-
Mixing With Alcohol or Other Sedatives: Combining tizanidine with alcohol, opioids, or benzodiazepines greatly increases the risk of excessive sedation, respiratory depression, falls, and overdose. Many serious adverse events occur through these unrecognized interactions.
-
Refill Irregularities: Early refill requests, reports of lost medication, or running out sooner than expected may indicate non-therapeutic use patterns and warrant careful, non-punitive clinical review.
How Common Is Tizanidine Misuse?
General prevalence:
In 2023, tizanidine was the 81st most commonly prescribed medication in the United States, with more than 8.29 million prescriptions and about 2.5 million patients receiving the drug. [3]
Clinical settings:
Tizanidine is widely used in clinical settings for the management of spasticity in patients with multiple sclerosis, spinal cord injury, stroke, and related neurological conditions, with its utilization reflected in large outpatient prescription data. [1]
Withdrawal frequency:
Although potential withdrawal symptoms (e.g., rebound hypertension, tachycardia, anxiety) have been described, documented tizanidine withdrawal cases are few and uncommon in the medical literature. [4]
Causes: Why Does Tizanidine Get Misused?
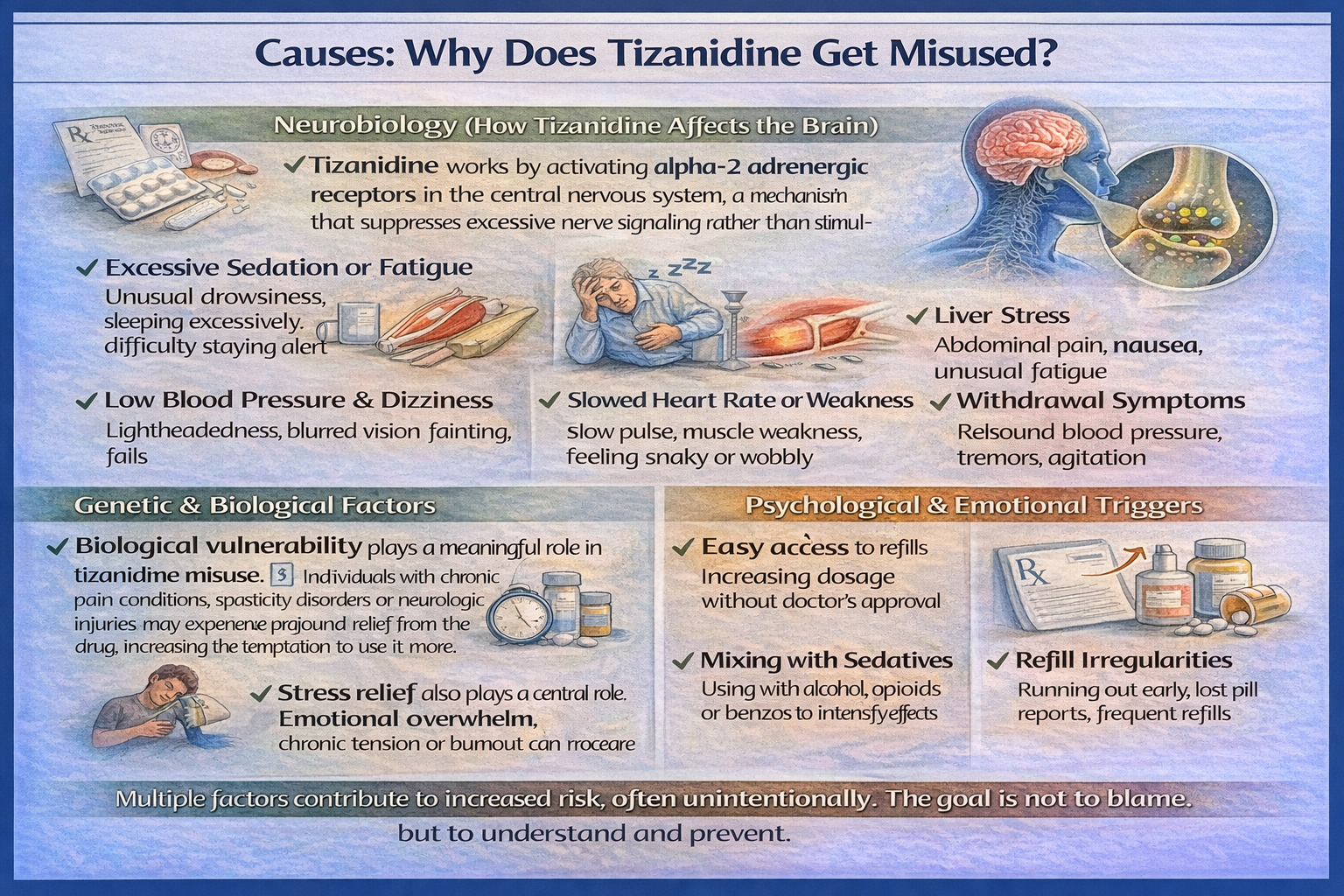
Neurobiology (How Tizanidine Affects the Brain?)
Tizanidine works by activating alpha-2 adrenergic receptors in the central nervous system, a mechanism that suppresses excessive nerve signaling rather than stimulating it.
By dampening sympathetic nervous system activity, the drug reduces muscle tone, decreases reflexive spasms, and produces a generalized calming effect throughout the body. This neurochemical action also lowers heart rate and blood pressure, contributing to the sensation of physical quiet and mental slowing.
Unlike classic addictive substances, tizanidine does not directly stimulate dopamine-driven reward pathways associated with craving or euphoria.
However, the rapid onset of sedation, relief from tension, and emotional quieting can feel psychologically reinforcing—especially during periods of stress, insomnia, or pain flares.
Over time, the brain may begin to associate the medication with safety, rest, or emotional control, increasing reliance even in the absence of physical addiction.
Genetic & Biological Factors
Biological vulnerability plays a meaningful role in tizanidine misuse. [5] Individuals with chronic pain conditions, spasticity disorders, or neurologic injuries may experience profound relief from the drug, increasing the temptation to use it more frequently or at higher doses.
Those with autonomic nervous system sensitivity—such as fluctuating blood pressure or heightened stress responses—may also be more sensitive to its calming effects.
Additionally, people who metabolize medications more slowly may experience prolonged sedation, increasing both perceived benefit and risk of accumulation. Co-existing sleep disorders can further reinforce nighttime use, while a personal or family history of medication dependence may predispose individuals to behavioral reliance, even when the drug itself is not classically addictive.
Psychological & Emotional Triggers
Psychological factors often drive the earliest stages of misuse. Many individuals begin relying on tizanidine to manage fear of pain recurrence, muscle tightening, or nighttime spasms, particularly after experiencing relief from initial doses.
Sleep anxiety is a common trigger, especially when sedation becomes associated with “finally being able to rest.”
Stress relief also plays a central role. Emotional overwhelm, chronic tension, or burnout can make the drug’s sedating effects feel like a temporary escape from mental pressure.
Over time, a subtle cognitive shift may develop—the belief that higher or more frequent dosing equals better control, reinforcing a cycle of use that becomes emotionally driven rather than symptom-based.
Environmental & Social Factors
Environmental conditions can unintentionally facilitate misuse. Easy access to refills, especially without structured follow-up, reduces opportunities for reassessment or dose adjustment. In settings where non-drug pain management options—such as physical therapy, stress regulation, or behavioral interventions—are limited, medication may become the primary coping tool.
High-stress or physically demanding work environments increase muscle tension and fatigue, leading to more frequent dosing “just to get through the day.”
Poor communication about tapering, inconsistent provider oversight, or unclear duration-of-use guidance further increase the risk that short-term therapy gradually turns into long-term dependence.
From Medical Use to Misuse (Progression)
The progression from appropriate use to misuse with tizanidine is typically physiologic and behavioral rather than addictive in the traditional sense.
It often begins with a legitimate prescription for muscle spasm, injury, or neurologic symptoms. As sedation improves sleep or temporarily eases emotional distress, the medication may be used beyond its original purpose.
During periods of stress, illness, or poor sleep, doses may be taken more frequently for relief.
Over time, the body adapts, and dependence develops, meaning abrupt dose reductions trigger withdrawal symptoms such as anxiety, rebound hypertension, or muscle tightness. Continued use then becomes avoidance-driven—not to feel “high,” but to prevent discomfort, instability, or emotional unease.
Who Is Most at Risk?
Certain populations face a higher risk of problematic use. Long-term users without a taper plan are especially vulnerable, as physiologic dependence can develop quietly. Patients who primarily use tizanidine as a sleep aid rather than for muscle symptoms may increase dosing over time as tolerance develops.
Individuals with cardiovascular conditions are at greater risk due to the drug’s blood pressure–lowering effects, while older adults may experience stronger sedation, dizziness, and cognitive slowing.
Combining tizanidine with other central nervous system depressants, such as benzodiazepines, opioids, or alcohol, significantly increases both misuse risk and medical danger.
Side Effects of Tizanidine Misuse or Dependence
Short-Term Side Effects
-
Sedation and Fatigue: Overuse or higher-than-prescribed doses can cause profound drowsiness, prolonged sleep, and difficulty maintaining alertness, increasing risk for accidents or impaired daily functioning.
-
Dizziness and Low Blood Pressure: Orthostatic hypotension is common, which may lead to lightheadedness, fainting, or falls, particularly in older adults or those with pre-existing cardiovascular conditions.
-
Nausea or Gastrointestinal Discomfort: Some users experience mild GI upset, including nausea, stomach cramping, or decreased appetite.
-
Muscle Weakness and Coordination Changes: Excess dosing can result in reduced muscle strength and slowed reflexes, making physical tasks more difficult and increasing injury risk.
-
Emotional or Cognitive Effects: Short-term use beyond therapeutic doses may produce mood changes, irritability, or temporary cognitive slowing, affecting attention and reaction time.
-
Rebound Symptoms if a Dose Is Missed: Suddenly skipping or stopping doses can lead to rebound effects such as rapid heart rate, tremors, sweating, and increased anxiety. These reactions may feel intense or alarming, but they reflect the body’s physiologic withdrawal response—not addiction itself.
Long-Term Side Effects
-
Chronic Hypotension and Cardiovascular Strain: Prolonged overuse can lead to persistent low blood pressure, fainting episodes, and increased cardiovascular risk.
-
Liver Stress: While tizanidine alone rarely causes liver damage, long-term or high-dose use may elevate liver enzymes, especially if combined with other hepatically metabolized drugs.
-
Cognitive and Mood Changes: Extended misuse may cause slower processing, reduced concentration, or depressive/anxious symptoms, often related to chronic sedation and disrupted sleep patterns.
-
Medication-Dependent Sleep: Reliance on tizanidine for sleep can make falling asleep or staying asleep difficult without the medication.
-
Hyperalgesia or Muscle Discomfort: Rarely, prolonged use may paradoxically increase sensitivity to pain or muscle tension, reinforcing continued dosing.
-
Overdose Risk: Combining tizanidine with alcohol, opioids, or benzodiazepines can lead to severe hypotension, excessive sedation, respiratory depression, or life-threatening events.
Impact on Daily Life
Chronic misuse or dependence can affect multiple aspects of functioning:
-
Work/School Decline: Fatigue, sedation, or cognitive slowing can reduce productivity, attendance, and task performance.
-
Relationship Strain: Irritability, mood fluctuations, and rigid medication routines may create tension in family and social relationships.
-
Financial or Legal Issues: Frequent early refills, doctor-shopping, or unintentional misuse can create economic strain or medical complications requiring urgent care.
Treatment Options
Recovery from tizanidine dependence or misuse requires a comprehensive, individualized plan that integrates medical management, psychological support, behavioral interventions, and social resources.
Because tizanidine affects the central nervous system and autonomic nervous system, withdrawal can produce significant physiologic stress, including blood pressure spikes, rapid heart rate, tremors, and anxiety, which can be dangerous if unmanaged.
Treatment should therefore be structured, patient-centered, and medically supervised, rather than relying on abrupt cessation.
Detox / Withdrawal Management
Detoxification begins with a gradual, medically supervised taper, tailored to the patient’s dose, duration of use, age, cardiovascular health, and co-existing conditions.
Abrupt discontinuation, or “cold turkey,” is unsafe and can lead to autonomic instability, rebound hypertension, tremors, excessive anxiety, insomnia, or even fainting.
Key components of detox include:
-
Gradual Dose Reduction: Doses are decreased in small increments over days to weeks, depending on individual tolerance and physiologic response.
-
Symptom Management: Supportive medications may be used selectively to manage withdrawal symptoms. For example, beta-blockers can help control heart rate and blood pressure spikes, while short-term non-sedating anxiolytics may ease acute anxiety or agitation.
-
Vital Sign Monitoring: Blood pressure, heart rate, and other indicators are closely tracked to prevent complications.
-
Education and Expectation Management: Patients and families are taught what to expect during withdrawal—such as rebound nervous system activity and temporary emotional lability—to reduce anxiety and increase adherence.
Clinical evidence and case reports show that structured tapering dramatically reduces the risk of severe withdrawal events and supports long-term stability. [6]
Levels of Care
Inpatient / Residential (30–90 days):
Best suited for patients at high risk of severe withdrawal or autonomic instability, or those lacking home support. Inpatient care provides:
-
24/7 monitoring of vital signs
-
Structured daily routines to minimize stress and ensure adherence to the taper
-
Immediate access to medical interventions for complications
-
Intensive psychological and behavioral support alongside medical management
Intensive Outpatient Programs (IOP):
IOPs are ideal for patients who are medically stable but require frequent therapy and ongoing supervision. Programs typically involve:
-
Multiple therapy sessions per week, including individual and group counseling
-
Ongoing medical oversight of tapering schedules
-
Skills training for stress management, sleep improvement, and avoidance of misuse triggers
-
Peer support integration to strengthen recovery networks
Standard Outpatient Care:
For patients with mild dependence or early-stage physiologic adaptation, standard outpatient care focuses on:
-
Slow, stepwise tapering with medical supervision
-
Monitoring of withdrawal symptoms and vital signs
-
Education on safe use, alternative coping strategies, and risk mitigation
-
Referral to therapy, peer support, or holistic programs as needed
Therapies
-
Cognitive Behavioral Therapy (CBT): Helps patients identify and modify thoughts and behaviors that reinforce tizanidine reliance. Focus areas include pain perception, sleep patterns, stress triggers, and emotional regulation.
-
Motivational Interviewing (MI): Enhances motivation, engagement, and adherence to tapering and recovery plans. MI is particularly effective when ambivalence or fear of withdrawal is a barrier.
-
Family Therapy: Involves family members to educate, support, and reinforce healthy coping strategies, reducing misunderstandings and relapse triggers.
-
Skills Training: Practical skills focus on managing triggers, coping with cravings, and preventing dose escalation. Skills may include pacing physical activity, relaxation techniques, sleep hygiene, and mindfulness strategies.
Peer Support & Recovery Capital
Recovery benefits from social and community support, often referred to as recovery capital. This includes:
-
Participation in peer support groups, such as NA alternatives or local recovery networks
-
Mentorship and shared experiences to normalize challenges and reinforce coping strategies
-
Building social, emotional, and community resources to replace reliance on medication as the primary stress management tool
Peer support helps reduce isolation, improve accountability, and provides practical tips for managing daily triggers, creating a sustainable foundation for long-term recovery.
Holistic Supports (Adjunct)
Adjunctive, non-pharmacologic strategies support emotional, cognitive, and physiologic stability:
-
Mindfulness, meditation, and relaxation techniques to reduce sympathetic nervous system hyperactivity
-
Regular exercise and physical therapy to maintain muscle tone, reduce spasticity, and improve cardiovascular health
-
Sleep hygiene practices such as consistent sleep schedules, limiting caffeine, and pre-bedtime routines to improve natural sleep regulation
-
Nutrition and liver support to optimize energy, metabolic health, and resilience during tapering
Holistic approaches enhance mood, stress tolerance, and physiologic recovery, complementing medical tapering and behavioral therapies.
Withdrawal Timeline — What to Expect?
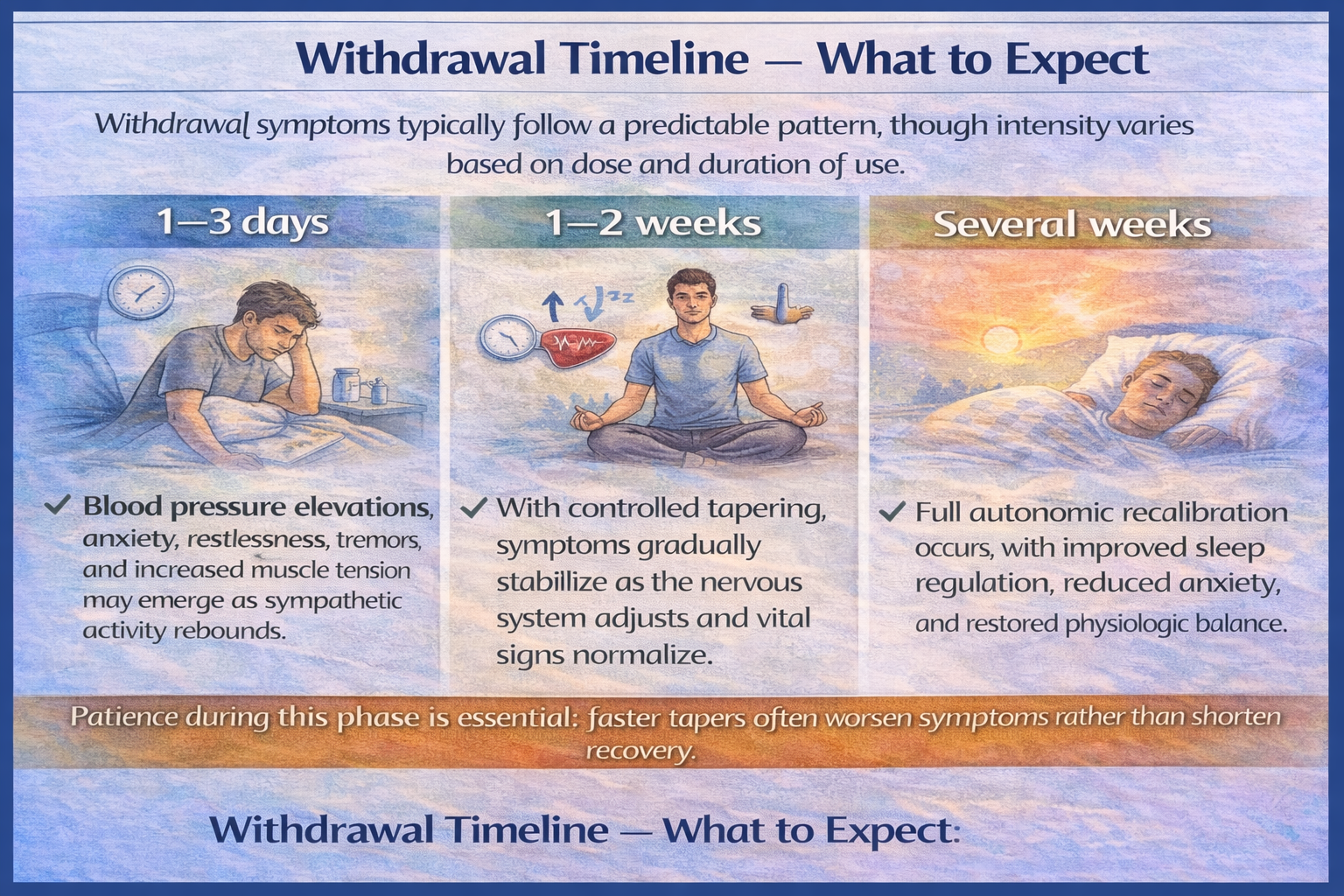
Withdrawal symptoms typically follow a predictable pattern, though intensity varies based on dose and duration of use.
-
1–3 days: Blood pressure elevations, anxiety, restlessness, tremors, and increased muscle tension may emerge as sympathetic activity rebounds.
-
1–2 weeks: With controlled tapering, symptoms gradually stabilize as the nervous system adjusts and vital signs normalize.
-
Several weeks: Full autonomic recalibration occurs, with improved sleep regulation, reduced anxiety, and restored physiologic balance.
Patience during this phase is essential; faster tapers often worsen symptoms rather than shorten recovery.
When to Seek Immediate Help
Urgent medical evaluation is necessary if withdrawal or misuse leads to severe hypertension, chest pain, fainting episodes, confusion, or collapse. These symptoms may signal dangerous autonomic instability or cardiovascular strain and should never be managed at home without medical supervision.
Dosing & Safety / Overdose Risks (For Legitimate Prescribing)
Typical Therapeutic Ranges & Formulations
Tizanidine is typically prescribed in low, divided doses due to its potent effects on the central and autonomic nervous systems. Treatment usually begins at 2 mg, taken up to every 6–8 hours as needed, with slow titration based on response and tolerability. Most patients achieve benefit within a total daily dose range of 8–24 mg, while the maximum recommended daily dose is 36 mg.
Tizanidine is available in immediate-release tablets and capsules, which are not interchangeable on a milligram-for-milligram basis due to differences in absorption. Consistency in formulation and timing with food is essential, as changes can significantly alter blood levels and side effect risk.
High-Risk Combinations
Tizanidine’s sedating and blood pressure–lowering effects are additive with other central nervous system depressants, making certain combinations particularly dangerous. High-risk interactions include:
-
Alcohol, which markedly increases sedation, hypotension, and accident risk
-
Benzodiazepines, which amplify CNS depression and impair respiratory drive
-
Other sedatives or sleep medications increase the risk of excessive drowsiness, falls, and loss of consciousness
These combinations are a leading cause of serious adverse events and should be avoided unless carefully evaluated and monitored.
Overdose Mechanism & Emergency Response
Tizanidine overdose primarily causes profound hypotension, bradycardia, and central nervous system depression, leading to extreme sedation, confusion, or collapse.
Respiratory depression is uncommon with tizanidine alone, but the risk rises significantly when combined with opioids, alcohol, or benzodiazepines.
Naloxone does not reverse tizanidine itself, but it can be life-saving if opioids are involved in a mixed overdose. For this reason, emergency services should always be contacted if an overdose is suspected, even if naloxone has been administered.
Safe Use Practices
Safe prescribing and use rely on clear education and risk prevention:
-
Store medication securely, away from children, pets, and others
-
Never share tizanidine, even with someone who has similar symptoms
-
Follow prescribed dosing exactly and avoid unsupervised dose changes
-
Dispose of unused medication properly, using pharmacy take-back programs or approved disposal methods
When used thoughtfully and monitored appropriately, tizanidine can be effective and safe. Problems most often arise from dose escalation, drug interactions, or abrupt discontinuation, all of which are preventable with education and follow-up.
FAQs
Yes. While tizanidine is not considered addictive, physical dependence can develop with regular or long-term use. This occurs because the nervous system adapts to the medication’s suppression of sympathetic activity, not because of reward-driven drug seeking.
The most serious risks involve cardiovascular instability and drug interactions. Abrupt discontinuation can cause rebound hypertension and rapid heart rate, while combining tizanidine with alcohol, opioids, or benzodiazepines increases the risk of profound sedation, hypotension, and respiratory depression.
Temporary return to use is relatively common and usually reflects symptom flare-ups, stress, or overly rapid dose reduction, not addiction. Clinically, it signals the need to slow the taper or better address pain, sleep, or anxiety drivers.
No. Unsupervised discontinuation is unsafe due to the risk of autonomic rebound, including blood pressure spikes and severe anxiety. Medical tapering allows for controlled dose reduction and monitoring of vital signs.
Family members can help by understanding that dependence is not addiction, avoiding judgment, and supporting adherence to taper plans. Encouraging medical follow-up, therapy participation, and stress-reduction strategies improves outcomes.
Yes. Withdrawal is usually manageable but can become dangerous without monitoring, especially in individuals with cardiovascular conditions or high-dose use. Medical supervision reduces risk and ensures early intervention if complications arise.
Resources
Related Articles
Treatment Centers in Texas









