Valium Addiction: Signs, Withdrawal, and Treatment
Valium (diazepam) is often prescribed for anxiety, insomnia, and muscle spasms, but its calming effects make it highly addictive with long-term use. What starts as legitimate treatment can quickly lead to dependence marked by cravings, memory lapses, sedation, and withdrawal from daily life (1).

Stopping suddenly is unsafe—withdrawal may trigger anxiety, tremors, insomnia, and in severe cases, seizures or hallucinations (2). That’s why tapering under medical supervision is essential.
The good news: recovery is possible. With medical detox, therapy, and ongoing support, many people overcome Valium addiction and rebuild healthier, more stable lives(3).
Key Takeaways
-
Valium addiction is a medical condition, not a weakness. It develops through changes in brain chemistry, making medical supervision essential for safe withdrawal and long-term recovery.
-
Professional treatment is the safest and most effective option. Medical detox, inpatient or outpatient rehab, and evidence-based therapies like CBT give individuals the tools they need to manage cravings, address triggers, and rebuild their lives.
-
Long-term recovery requires ongoing support. Aftercare programs, family involvement, and relapse prevention strategies help sustain progress. With patience, persistence, and the right help, lasting recovery is within reach.
What Valium Is and How It’s Used?
Valium (diazepam) belongs to the benzodiazepine family, a group of medications known for their calming effects. Doctors often prescribe it for anxiety, muscle spasms, insomnia, or seizures.
When used short-term and as directed, it can bring real relief. The problem arises when Valium is taken for longer periods or at higher doses than prescribed (1).
Why Valium Can Become Addictive?
Valium works by enhancing the effect of GABA, a brain chemical that slows down activity in the nervous system. This produces relaxation and sedation.
Over time, the brain adapts and begins to depend on the drug to feel “normal.” As tolerance builds, people may take more than prescribed, increasing the risk of addiction[1].
The Shift From Use to Addiction
Dependence develops first: the body expects Valium and reacts with withdrawal when it’s absent. Addiction goes further. It’s marked by cravings, compulsive use, and continuing the drug despite harm.
At this point, Valium use is no longer about medical relief—it becomes a cycle that’s difficult to break without help[2].
Why Early Recognition Matters?
Valium addiction often develops gradually. Signs like sedation, memory lapses, or withdrawal from social activities may seem minor at first, but worsen over time. Recognizing these early changes allows families and individuals to seek treatment before health, relationships, and safety are severely impacted [4].
Dependence vs. Addiction: What’s the Difference?
Understanding Dependence
Dependence happens when the body adapts to regular Valium use. Over time, tolerance builds, meaning higher doses are needed to feel the same calming effects.
If the drug is reduced or stopped, withdrawal symptoms such as anxiety, irritability, or insomnia appear. Dependence does not always mean addiction, but it’s the first sign that the brain has come to rely on Valium to function normally (1).
What Makes It an Addiction?
Addiction goes beyond physical dependence. It is a behavioral health condition marked by cravings, loss of control, and continued use despite negative consequences.
Someone addicted to Valium may try to cut down but fail, spend large amounts of time obtaining or using the drug, or neglect responsibilities because of it[3].
This difference is more than just medical language. Dependence can occur even under a doctor’s care, but addiction reflects a harmful pattern that requires treatment.
Families often mistake dependence for “just needing the medication,” when in reality, compulsive use signals a deeper problem. Recognizing the shift early allows for safer intervention and prevents dangerous withdrawal or overdose risks[2][3].
Dependence shows the body is adjusting to Valium; addiction shows life is being taken over by it. Knowing the difference helps individuals and families act before the consequences grow more severe.
Recognizing the Signs of Valium Addiction
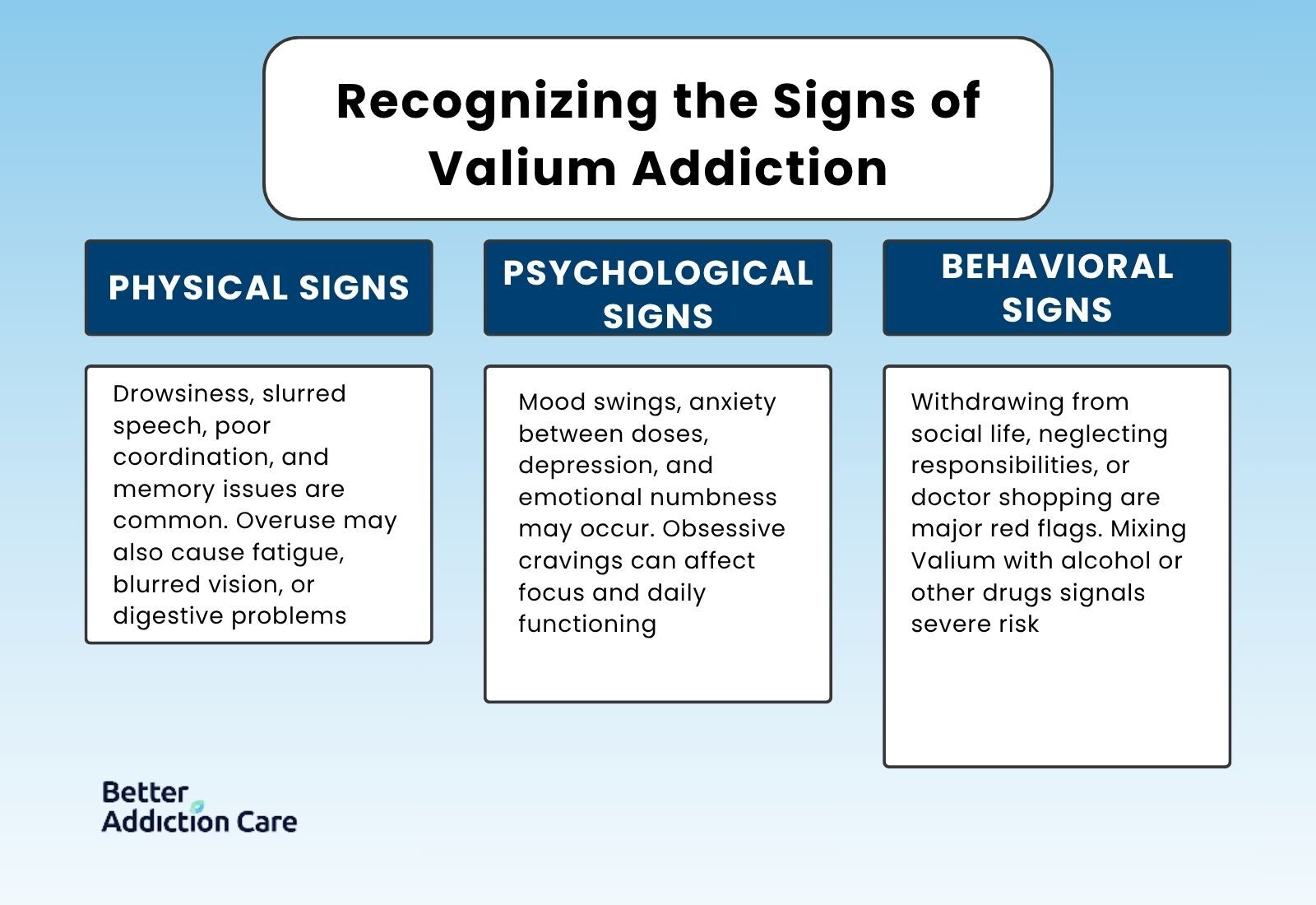
Valium addiction can be difficult to spot at first.
The drug’s calming effects may seem helpful, but over time, warning signs emerge in physical health, mental well-being, and everyday behavior. Recognizing these patterns early can make the difference between safe recovery and deeper harm.
Physical Signs
Valium acts on the central nervous system, so its effects show up physically. People may appear unusually drowsy or sedated even at inappropriate times of day.
Slurred speech, poor coordination, or balance problems can resemble intoxication.
Memory gaps and slowed reaction times are also common. Overuse may lead to fatigue, blurred vision, or digestive issues that interfere with normal routines (1).
Psychological Signs
Addiction also affects mood and mental health. Many report heightened anxiety or irritability between doses. Depression, mood swings, and emotional numbness may appear as the brain grows dependent on Valium.
Cravings for the drug can dominate thoughts, making it hard to focus on work, studies, or personal responsibilities.
These psychological signs can be mistaken for mental health conditions alone, but when paired with ongoing Valium use, they often reflect addiction[3].
Behavioral Signs
Behavioral changes are often the clearest warning signs for families. Someone addicted to Valium may withdraw from social life, lose interest in hobbies, or neglect work and school obligations.
Doctor shopping—seeking multiple prescriptions, or taking higher doses than prescribed, are red flags. In severe cases, individuals may combine Valium with alcohol or other drugs, greatly increasing the risk of overdose[2].
Why Families Should Pay Attention?
Addiction rarely announces itself openly. Loved ones are often the first to notice subtle but persistent changes. Spotting sedation, secrecy, or mood instability should not be dismissed as stress or normal behavior.
Addressing these signs early with compassion and professional guidance makes treatment safer and more effective.
Physical, psychological, and behavioral changes together point to Valium addiction. Recognizing the pattern early allows families and individuals to seek help before health and safety are seriously compromised.
Withdrawal from Valium: Symptoms and Timeline
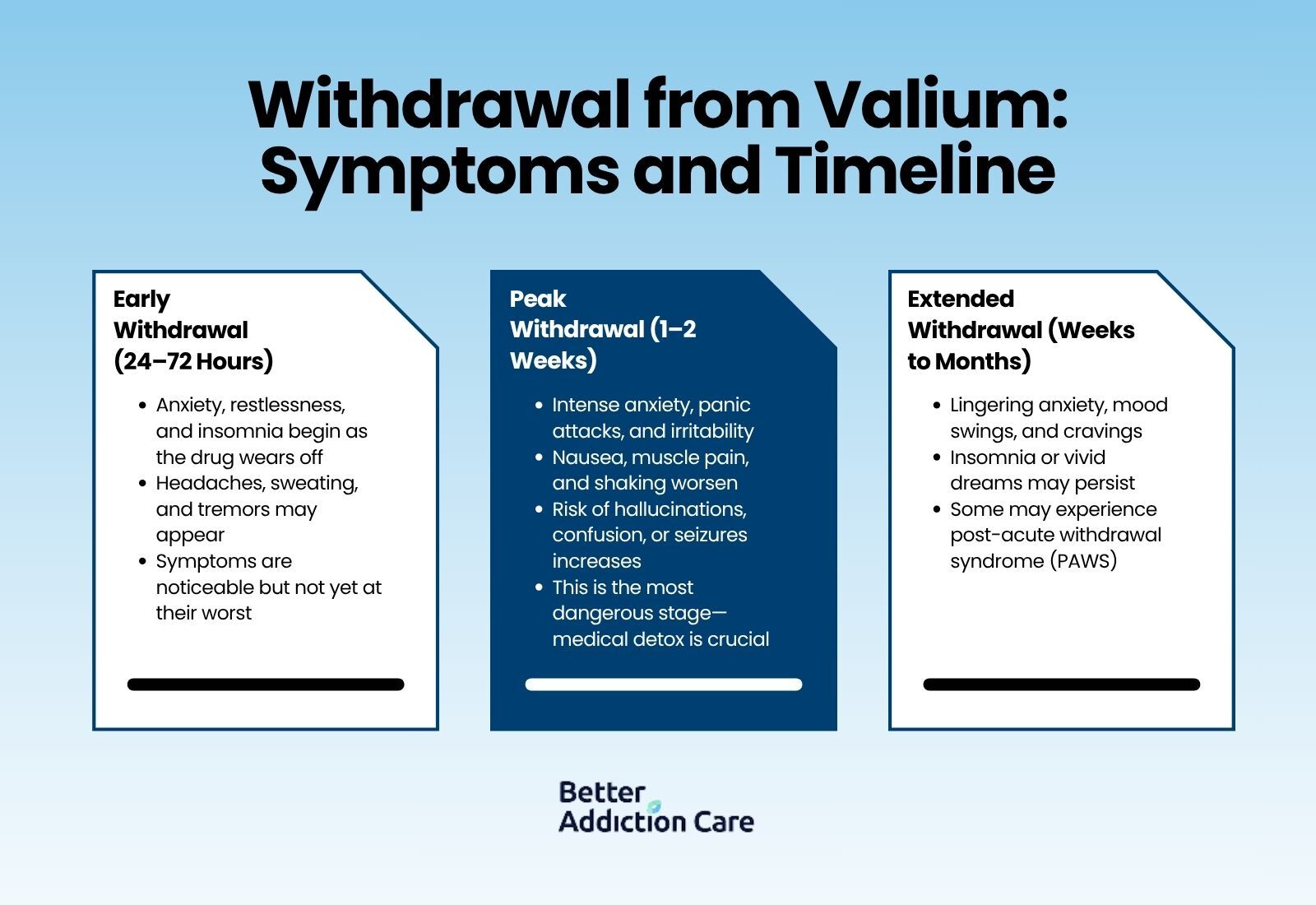
Stopping Valium is not like stopping most other prescription drugs. Because it directly alters brain chemistry, withdrawal can be uncomfortable and, in some cases, dangerous. Understanding the timeline helps individuals and families know what to expect and why medical supervision is so important.
Early Withdrawal (First 24–72 Hours)
-
Onset of anxiety and restlessness as the calming effects of Valium wear off.
-
Sleep disruption often begins with trouble falling asleep or staying asleep.
-
Physical changes such as headaches, sweating, or tremors may appear.
During this stage, symptoms can feel unsettling but are usually not at their peak. For many, the first few days are the signal that the body has grown dependent on the drug[1].
Peak Withdrawal (First 1–2 Weeks)
-
Severe anxiety, panic attacks, and irritability are common as the brain struggles to regain balance.
-
Nausea, muscle pain, and shaking may worsen.
-
Hallucinations, confusion, or seizures can develop in more severe cases.
This is the most dangerous phase. Quitting “cold turkey” greatly increases the risk of seizures, which is why medical detox and tapering are strongly recommended[5].
Extended Withdrawal (Weeks to Months)
-
Lingering anxiety and mood instability can continue for weeks.
-
Insomnia or vivid dreams may persist even after other symptoms fade.
-
Cravings for Valium often appear during stressful moments.
Some individuals experience protracted withdrawal, also known as post-acute withdrawal syndrome (PAWS). While symptoms are less intense than in the peak phase, they can interfere with recovery if left unaddressed. Ongoing medical and therapeutic support helps reduce the impact of this stage[6].
Unlike some substances, Valium withdrawal can become life-threatening. Supervised detox allows doctors to taper the dose gradually, monitor vital signs, and provide support for both physical and psychological symptoms[6]. This reduces the risk of seizures and improves long-term recovery outcomes.
Valium withdrawal typically begins within days, peaks in the first two weeks, and gradually lessens over time. With medical supervision, the process is safer, more manageable, and less frightening for both individuals and their families.
Risks of Polysubstance Use with Valium
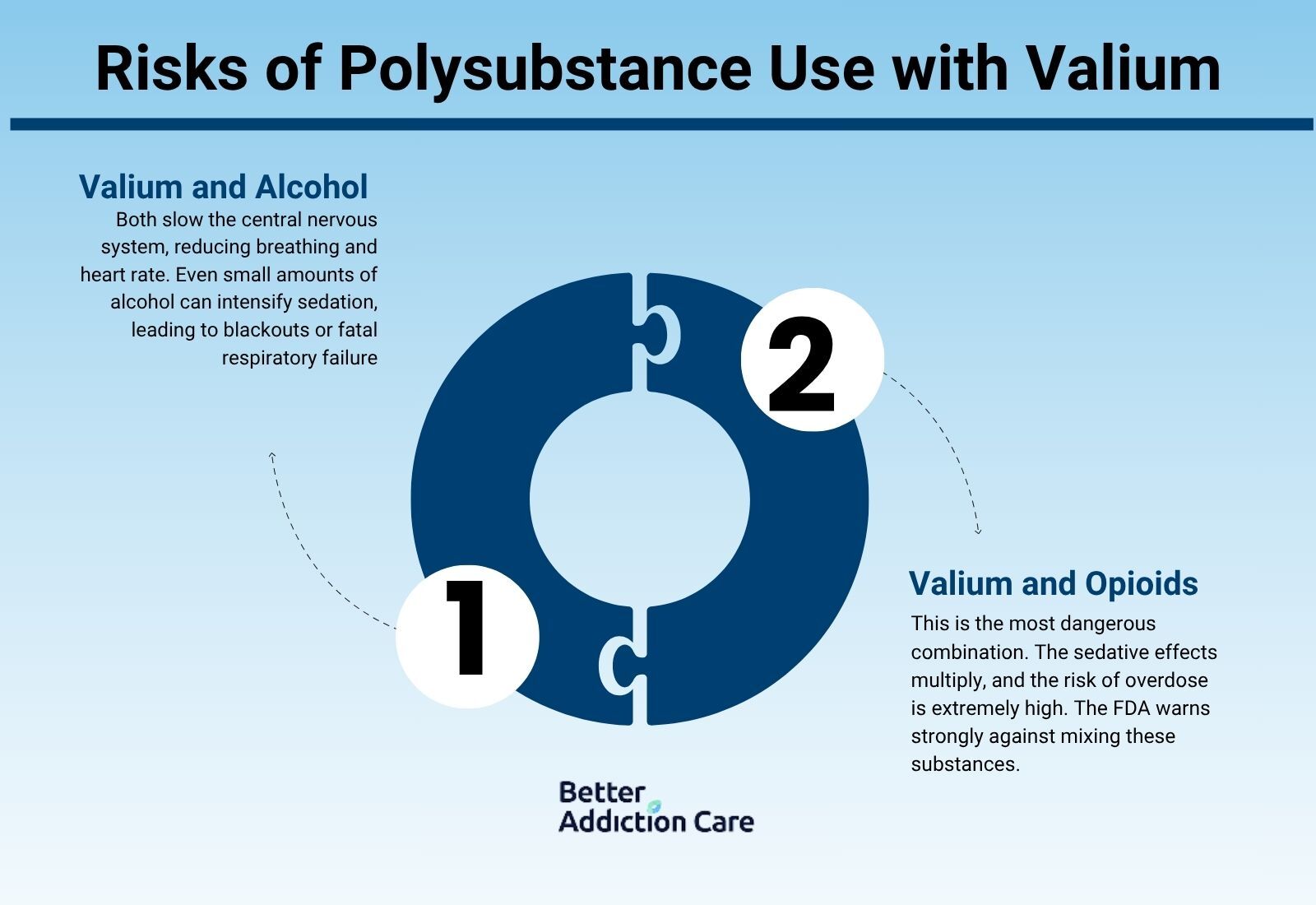
Valium misuse is risky on its own, but when combined with alcohol, opioids, or other sedatives, the danger escalates quickly. This type of pattern—called polysubstance use—accounts for many benzodiazepine-related overdose deaths in the United States[1].
Valium and Alcohol
Both Valium and alcohol depress the central nervous system. Together, they slow breathing and heart rate to unsafe levels.
Even small amounts of alcohol can intensify Valium’s sedative effects, leading to blackouts, accidents, or overdose. The combination is especially lethal because respiratory failure can occur without warning[2].
Valium and Opioids
The deadliest combination is Valium and opioids. Both act as sedatives, and when taken together, the effects multiply.
The FDA has issued strong warnings about this mix because of its high overdose potential[2].
Many overdose deaths involve exactly this combination—prescription medications misused in ways never intended.
Why People Mix Substances?
Some mix Valium with alcohol or opioids to heighten the high or escape emotional pain. Others may not realize that combining prescriptions increases risk. Regardless of intent, polysubstance use is one of the strongest signals that professional treatment is urgently needed.
Long-Term Risks
Beyond the immediate danger of overdose, long-term mixing damages health. Memory problems, poor coordination, and emotional instability worsen with time. Withdrawal also becomes more complicated, as multiple substances often require tapering under medical supervision.
Mixing Valium with alcohol, opioids, or other depressants isn’t just risky—it’s life-threatening. Recognizing this danger is often the wake-up call families and individuals need to seek treatment quickly.
Treatment for Valium Addiction
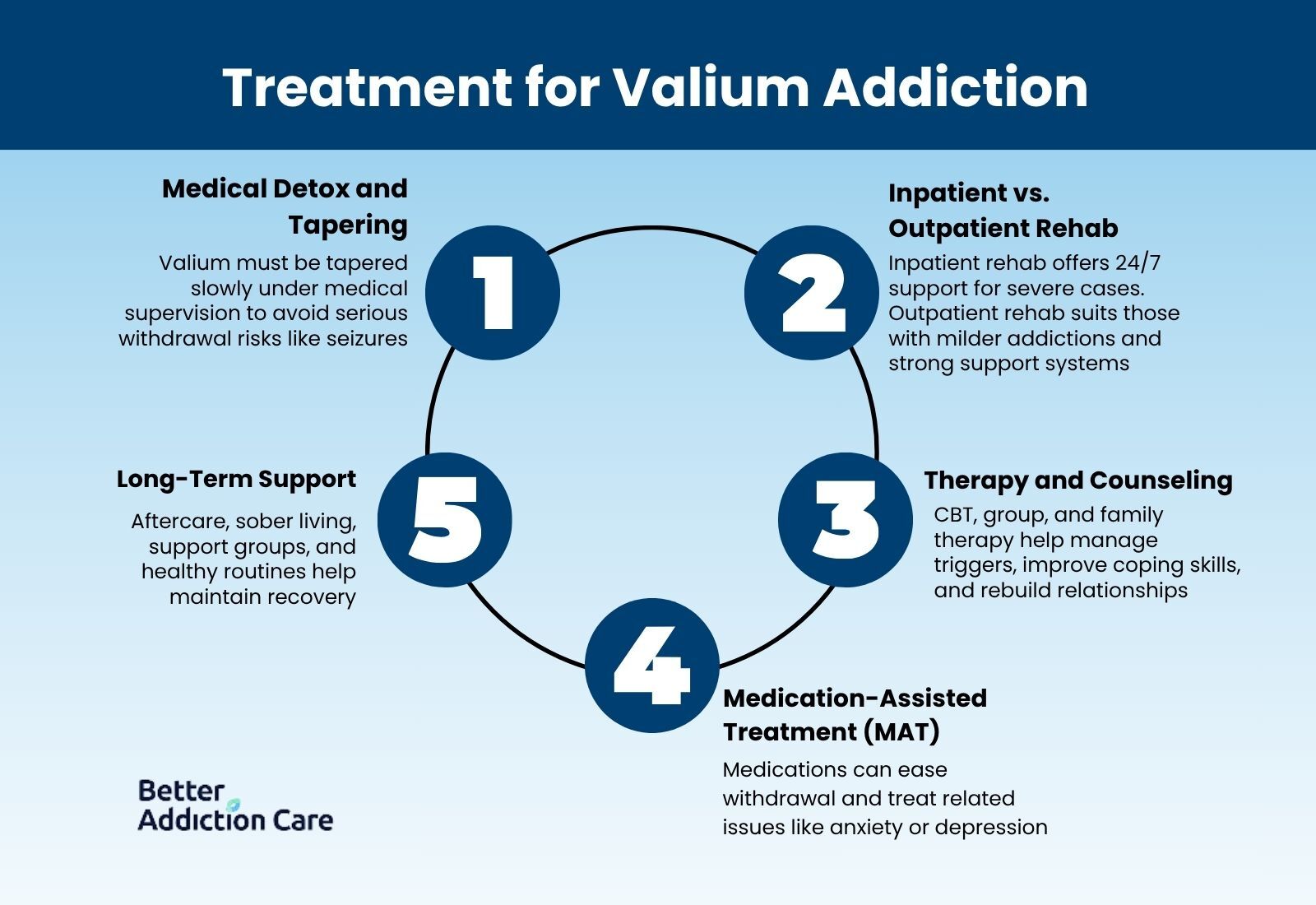
Treating Valium addiction requires more than willpower. Because the drug directly alters brain chemistry, safe recovery involves medical supervision, structured therapy, and ongoing support. With the right treatment, individuals can regain stability and build a healthier future.
Medical Detox and Tapering
The first step is usually detox. Unlike many drugs, Valium cannot be stopped suddenly without serious risks. Medical professionals use a tapering process, gradually lowering the dose to reduce withdrawal symptoms and prevent seizures[5].
In some cases, doctors may switch patients to a longer-acting benzodiazepine before tapering, making the transition smoother.
Detox often takes place in a hospital or specialized facility, where vital signs and symptoms are closely monitored. This setting provides safety and reassurance during the most difficult phase of withdrawal (6).
Inpatient vs. Outpatient Rehab
Once detox is complete, rehabilitation begins. Inpatient rehab offers 24/7 medical and emotional support, making it a strong option for those with severe addictions or polysubstance use[3].
Outpatient rehab allows individuals to live at home while attending scheduled treatment sessions, which may work better for those with strong family support or milder addictions.
Both settings provide therapy, education, and relapse prevention tools. The best choice depends on personal circumstances, health history, and the level of support available.
Therapy and Counseling Approaches
Therapy is central to long-term recovery. Cognitive Behavioral Therapy (CBT) helps individuals identify triggers, manage cravings, and change harmful thought patterns[6]. Group therapy provides peer support, reducing the isolation often felt during recovery.
Family therapy is also valuable. It helps loved ones understand addiction as a medical condition rather than a moral failing, while teaching healthier ways to support recovery[3].
Medication-Assisted Treatment (MAT)
While there is no specific “replacement drug” for Valium, medications may be used to ease withdrawal symptoms, stabilize mood, or address co-occurring disorders like depression or anxiety. This approach reduces the risk of relapse and makes therapy more effective [1][3].
Building Long-Term Support
Treatment does not end after rehab. Aftercare programs, sober living environments, and peer support groups such as 12-step or non-12-step programs provide accountability and encouragement[3].
Lifestyle changes—healthy routines, exercise, and stress management—help maintain balance long after treatment ends.
Conclusion: Finding a Path Forward
Valium addiction can feel overwhelming, but recovery is always possible. With medical detox, structured therapy, and strong support systems, individuals can safely withdraw from Valium and build new patterns of living.
Families play a powerful role by offering encouragement, setting boundaries, and staying involved throughout the journey.
If you or a loved one is struggling with Valium use, the first step is reaching out to a healthcare provider or treatment program. Professional guidance makes the process safer, reduces relapse risk, and helps create a long-term recovery plan. You don’t have to face this alone—help is available 24/7.
Common Questions About Valium Addiction: Signs, Withdrawal, and Treatment
Withdrawal symptoms often begin within 1–3 days after stopping Valium, peak around the first two weeks, and can last several weeks. For some, lingering anxiety or sleep issues may continue for months, which is why tapering under medical supervision is important.
Even short-term use can create dependence. Stopping suddenly without medical advice is risky and can cause severe symptoms, including seizures. It’s always safest to talk with a doctor before making changes.
Yes, relapse can happen, especially if stress or triggers aren’t managed. But relapse is not failure—it’s a signal that stronger strategies or additional support are needed. Many people achieve lasting recovery with persistence and the right treatment plan.
Combining Valium with alcohol, opioids, or other sedatives greatly increases the risk of overdose, slowed breathing, and even death. This combination should be avoided entirely.
Families can help by encouraging treatment, setting healthy boundaries, and offering emotional support. Joining family therapy or support groups also helps loved ones stay resilient while guiding recovery.
Some people may notice a return of underlying symptoms. However, therapy, lifestyle changes, and non-addictive treatments can effectively manage these issues without relying on Valium.
Recovery timelines vary. Detox and early stabilization may take weeks, while ongoing therapy and relapse prevention can extend for months or longer. Addiction is best viewed as a long-term process, not a quick fix.
Resources
Related Articles
Treatment Centers in New Jersey










