What Is Venlafaxine? Effexor Withdrawal and Addiction
Venlafaxine, commonly known by the brand name Effexor, is a prescription antidepressant belonging to a class called serotonin–norepinephrine reuptake inhibitors (SNRIs).
Key Takeaways
-
Venlafaxine (Effexor) is an antidepressant that can cause physical dependence, meaning the brain adapts to its presence over time.
-
When the medication is reduced too quickly or stopped suddenly, withdrawal symptoms may occur.
-
This is not a sign of weakness or addiction. Withdrawal happens because of neurobiology, not behavior or intent.
-
With proper medical guidance, gradual tapering, emotional support, and patience, Effexor withdrawal is manageable, and recovery—whether that means stopping the medication or continuing it safely—is absolutely possible.
It is approved to treat:
-
Major depressive disorder
-
Generalized anxiety disorder
-
Social anxiety disorder
-
Panic disorder
Venlafaxine works by increasing the availability of two key brain chemicals:
-
Serotonin, involved in mood, sleep, and emotional regulation
-
Norepinephrine, involved in energy, focus, and stress response
For many people, this combination is effective. However, the same mechanism that helps regulate mood can also make the brain highly sensitive to dose changes.
Families often use the word addiction because what they see looks frightening. But medically, dependence and addiction are not the same thing.
-
Tolerance: Over time, the brain adjusts to venlafaxine. The same dose may feel less effective, which is a normal biological response.
-
Physical Dependence: The nervous system becomes accustomed to the medication’s presence. When it is reduced too quickly, the brain struggles to maintain balance, leading to withdrawal symptoms.
-
Addiction: Addiction involves compulsive drug-seeking behavior, cravings for intoxication, loss of control, and continued use despite harm.
Venlafaxine does not produce euphoria, cravings, or compulsive misuse. What people experience is withdrawal, not addiction.
Signs and Symptoms of Effexor Addiction

Physical Symptoms
-
Dizziness or vertigo: Sudden lightheadedness, spinning sensations, or balance problems, especially when standing or turning the head. These symptoms can make routine activities feel unsafe and often worsen after missed or delayed doses.
-
“Brain zaps” or electric shock sensations: Brief jolting, buzzing, or shock-like sensations in the head, often triggered by eye movement or posture changes. These sensations may occur repeatedly throughout the day and are a common reason individuals fear stopping Effexor.
-
Headaches: Persistent or throbbing head pain ranging from mild pressure to migraine-like discomfort. Headaches often intensify during tapering attempts and may ease quickly when the medication is resumed.
-
Nausea, vomiting, or diarrhea: Gastrointestinal distress caused by sudden changes in serotonin and norepinephrine levels. Symptoms may include loss of appetite, stomach pain, or unpredictable digestive upset that interferes with daily functioning.
-
Fatigue or weakness: Ongoing physical exhaustion, muscle heaviness, or low energy even after rest. This fatigue can reduce motivation, concentration, and the ability to complete routine tasks.
-
Flu-like symptoms: Body aches, chills, sweating, or a general feeling of illness that can be mistaken for an infection rather than medication-related effects.
-
Sleep disturbances: Difficulty falling or staying asleep, vivid or disturbing dreams, frequent awakenings, or excessive daytime sleepiness, which can worsen emotional and cognitive symptoms.
Emotional and Psychological Symptoms
-
Anxiety or panic attacks: Heightened nervousness, restlessness, racing thoughts, or sudden panic episodes, particularly when doses are missed or reduced. These symptoms may appear even in individuals without a prior history of anxiety.
-
Irritability or agitation: Increased sensitivity to stress, impatience, or sudden anger that feels disproportionate to the situation. Family members may notice mood swings or emotional volatility that seem out of character.
-
Depressed mood: Persistent sadness, hopelessness, or emotional heaviness that can emerge rapidly during withdrawal. Mood symptoms may feel more intense than those experienced before starting Effexor.
-
Emotional numbness: A blunted emotional state marked by feeling disconnected or “flat,” with reduced ability to experience pleasure, motivation, or emotional closeness.
-
Crying spells: Sudden, uncontrollable episodes of tearfulness without a clear trigger. These episodes can be distressing and confusing for both the individual and loved ones.
-
Difficulty concentrating: Brain fog, slowed thinking, memory lapses, or reduced focus that interfere with work, school, and everyday decision-making.
Behavioral Symptoms
-
Fear of missing doses: Heightened anxiety around taking Effexor at the same time every day, with distress or panic if a dose is delayed or forgotten.
-
Reluctance to taper: Resistance to reducing the dose despite side effects or medical recommendations, driven by fear of withdrawal symptoms or emotional instability.
-
Restarting medication to stop symptoms: Resuming a previous dose after attempting to taper to relieve physical or emotional discomfort, reinforcing reliance on the medication.
-
Withdrawal from social interaction: Pulling away from family, friends, or activities once enjoyed due to fatigue, mood changes, or fear of symptoms worsening.
-
Increased healthcare visits: Frequent appointments, urgent refill requests, or repeated medical consultations focused on managing symptoms rather than addressing long-term dependence.
How Common Is It? (Prevalence & Epidemiology)
General prevalence
Recent systematic evidence indicates that about 15% (approximately one in six to seven patients) who discontinue antidepressants experience withdrawal symptoms directly attributable to stopping the medication, after accounting for non-specific effects seen in placebo groups. This finding comes from a large meta-analysis of 79 studies with over 21,000 participants.[2]
Clinical settings
Among different antidepressants, venlafaxine (Effexor) and other SNRIs tend to show a relatively higher rate of discontinuation symptoms compared with some other agents.
In pooled clinical trials and open-label data, reported rates of withdrawal symptoms after stopping venlafaxine ranged from about 23% to 78%, though individual study designs varied. [3]
Withdrawal frequency
In the same systematic reviews, severe discontinuation symptoms were estimated to occur in roughly 2–3% of patients who stop antidepressants, including venlafaxine, and these severe reactions more frequently occurred with desvenlafaxine, venlafaxine, paroxetine, and some tricyclics than with other antidepressants. [4]
Causes: Why Does Effexor “Addiction” Get Misunderstood?
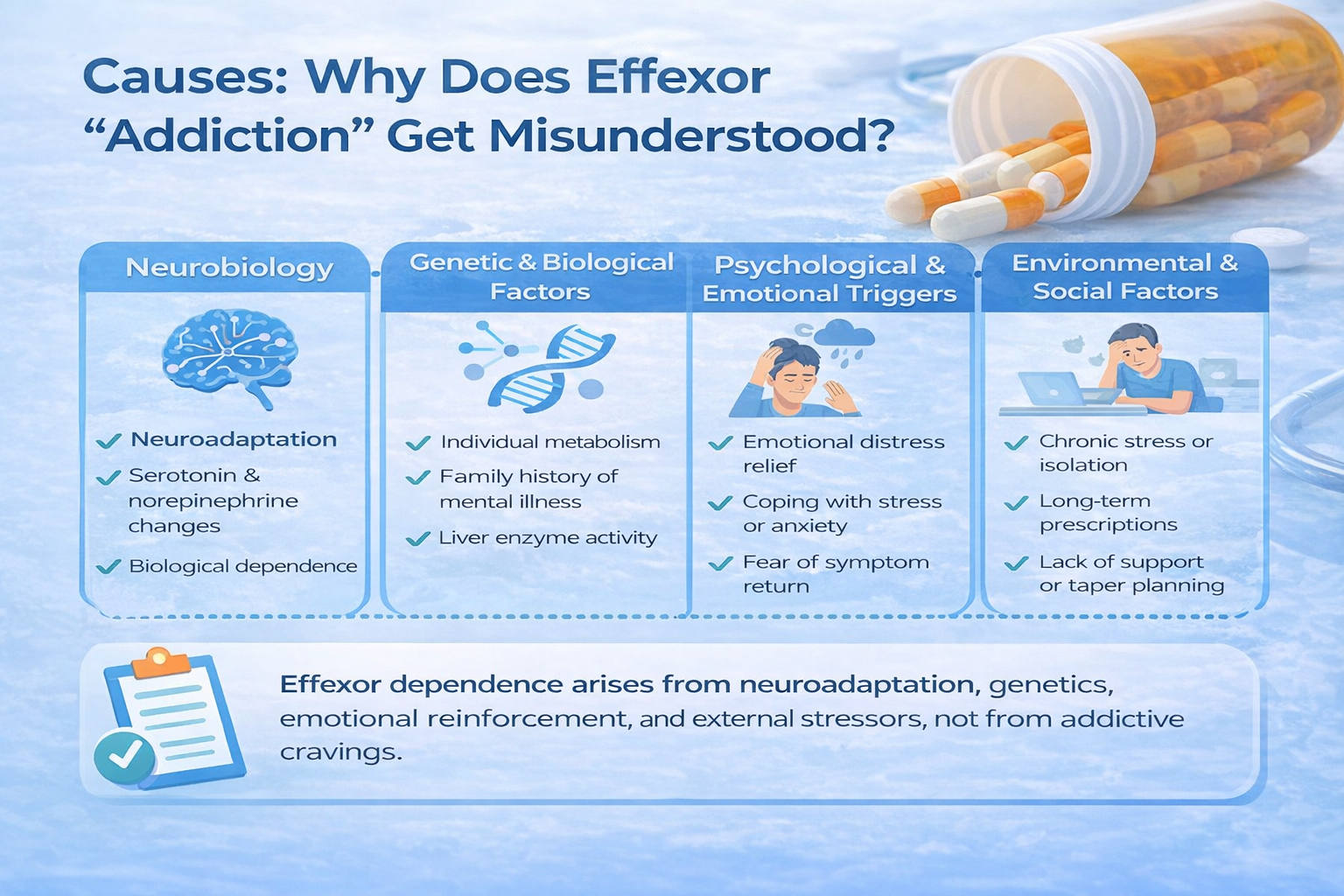
Neurobiology
Effexor works by inhibiting the reuptake of serotonin and norepinephrine, increasing their availability in the brain. Unlike addictive substances, it does not bind to dopamine reward receptors or directly stimulate the brain’s reward circuitry.
With repeated exposure:
-
The brain adapts to sustained serotonin and norepinephrine levels
-
Receptor sensitivity and neurotransmitter regulation adjust over time
-
Neural signaling becomes dependent on the presence of the medication for balance
When Effexor is reduced or stopped, this adapted system temporarily struggles to regulate mood, sleep, and sensory processing, leading to withdrawal symptoms. These changes are reversible but can feel intense during the adjustment period.
Clinical evidence shows that longer duration of use, higher doses, and rapid tapering increase the likelihood and severity of withdrawal symptoms. [5]
Importantly, this response reflects physiological dependence, not psychological addiction, and does not involve cravings driven by reward-seeking behavior.
Effexor withdrawal is best understood as a neuroadaptation reversal process, where the brain gradually relearns to regulate neurotransmitters independently.
Genetic & Biological Factors
Individual biology plays a significant role in vulnerability to Effexor dependence.
-
Genetic factors influence how quickly Effexor is metabolized and how sensitive neurotransmitter systems are to change.
-
A family history of mood disorders, anxiety disorders, or substance use disorders may increase susceptibility to dependence patterns.
-
Differences in liver enzyme activity can cause some individuals to experience stronger withdrawal effects, reinforcing continued use.
Co-occurring mental health conditions—such as major depression, generalized anxiety disorder, panic disorder, or PTSD—can further increase risk, as symptom rebound during withdrawal may feel intolerable.
Psychological & Emotional Triggers
Psychological reinforcement is a major driver of Effexor dependence.
-
Effexor often provides relief from emotional pain, anxiety, or overwhelming stress.
-
When emotional distress returns during dose changes, resuming the medication becomes a learned coping strategy.
-
Over time, individuals may come to believe they cannot function, cope, or remain emotionally stable without Effexor.
This cycle of distress → relief → reinforcement strengthens emotional reliance, even when the medication is taken exactly as prescribed.
Environmental & Social Factors
External circumstances can intensify reliance on Effexor.
-
Long-term prescribing without structured taper planning
-
Limited access to psychotherapy or non-medication coping supports
-
Social isolation or lack of emotional support
-
Chronic stress related to work, finances, caregiving, or health
-
Fear-based messaging about relapse or symptom return
When medication becomes the primary—or only—tool for managing emotional health, dependence risk increases.
From Symptom Relief to Dependence: How Progression Occurs?
Effexor dependence often develops gradually and unintentionally:
-
Initial treatment for depression, anxiety, or panic symptoms
-
Continued use leads to neurochemical adaptation and tolerance
-
Missed doses or taper attempts trigger withdrawal symptoms
-
Medication is resumed to stop discomfort and restore stability
-
Fear of withdrawal reinforces ongoing use
-
Attempts to stop become increasingly difficult without support
This progression does not reflect weakness or misuse intent, but rather a predictable response of the brain and nervous system to long-term SNRI exposure.
Who Is Most at Risk for Difficult Withdrawal?

While anyone can experience withdrawal symptoms when stopping Effexor, certain individuals tend to be more vulnerable due to how long they’ve used the medication, dosage levels, or underlying mental health factors.
Understanding these risk groups helps emphasize why a careful, personalized tapering plan is so important.
-
Those who have taken Effexor for years: Long-term use allows the brain to adapt closely to the presence of the medication. Over time, neurotransmitter balance becomes dependent on consistent dosing, making sudden reductions more challenging for the nervous system to adjust to smoothly.
-
Individuals on higher doses: Higher doses generally create a stronger neurochemical adjustment. When the dose is reduced too quickly, the brain may struggle to recalibrate, increasing the likelihood of more noticeable physical and emotional withdrawal symptoms.
-
People who taper too quickly: Rapid dose reductions are one of the most common causes of difficult withdrawal. Effexor leaves the body relatively fast, so lowering the dose without adequate time between steps can trigger intense symptoms that feel abrupt and overwhelming.
-
Those with anxiety or panic disorders: People with pre-existing anxiety or panic symptoms may be more sensitive to the physical sensations of withdrawal, such as dizziness, restlessness, or heart palpitations. These sensations can amplify fear and make symptoms feel more severe than they are.
-
People who previously struggled with antidepressant withdrawal: A history of withdrawal difficulties often signals increased sensitivity to medication changes. Past experiences can also increase anticipatory anxiety, which may intensify symptoms during future tapering attempts.
Being “at risk” does not mean withdrawal will be severe or unmanageable—it simply highlights the importance of slow tapering, medical guidance, and realistic expectations. With the right plan and support, most people are able to reduce Effexor safely and successfully.
Side Effects of Effexor Misuse or Dependence
Short-Term Effects
Short-term side effects are more likely during dose increases, missed doses, misuse, or early withdrawal and may include:
-
Nausea, vomiting, or stomach discomfort
-
Dizziness or lightheadedness
-
Headache or pressure sensations
-
Increased sweating or flushing
-
Insomnia or excessive sleepiness
-
Restlessness, agitation, or anxiety
-
Elevated heart rate or blood pressure
-
Appetite changes
-
Emotional blunting or feeling numb
-
Brain zaps or electric-shock sensations (especially if doses are missed)
Long-Term Effects
With prolonged use, high doses, or improper discontinuation, some individuals may experience:
-
Physical dependence makes it difficult to stop without withdrawal symptoms
-
Persistent gastrointestinal issues (nausea, constipation, diarrhea)
-
Blood pressure elevation over time
-
Sleep disruption or chronic fatigue
-
Emotional flattening or reduced emotional responsiveness
-
Cognitive effects such as brain fog, concentration difficulties, or memory issues
-
Worsening anxiety or depressive symptoms during tolerance or withdrawal
-
Increased sensitivity to pain or bodily sensations
-
Sexual dysfunction (reduced libido, delayed orgasm)
-
Higher risk of severe withdrawal symptoms if stopped abruptly
Impact on Daily Life

When Effexor dependence or withdrawal is poorly managed, it can significantly affect daily functioning:
-
Decline in work or school performance due to fatigue, brain fog, or mood instability
-
Difficulty maintaining routines or meeting responsibilities
-
Strain on relationships caused by irritability, emotional withdrawal, or mood swings
-
Increased health-related anxiety and fear of missed doses
-
Frequent medical visits or medication adjustments
-
Reduced overall quality of life during unmanaged tapering or withdrawal periods
Treatment Options
Effective management of Effexor withdrawal relies on an individualized treatment plan rather than a one-size-fits-all approach. Care is most successful when it combines medical guidance, psychological support, and social stability.
The goal is not just symptom reduction, but helping the nervous system recalibrate safely while maintaining emotional well-being and daily functioning.
Treatment plans should be flexible and responsive, adjusting based on symptom severity, duration of Effexor use, dose history, and personal vulnerability to medication changes.
Detox / Withdrawal Management
Setting:
Effexor withdrawal is most often managed in an outpatient setting, under the supervision of a prescribing clinician. Inpatient care is rarely required and is typically reserved for situations involving severe psychiatric instability or safety concerns.
Abrupt discontinuation (“cold turkey”) is strongly discouraged, as it significantly increases the risk of intense neurological and emotional symptoms.
Supports:
-
Gradual tapering is the cornerstone of withdrawal management, allowing the brain time to adjust to reduced serotonin and norepinephrine activity.
-
Adjunct medications may be prescribed short-term to relieve specific symptoms such as insomnia, nausea, dizziness, headaches, or acute anxiety.
-
Regular monitoring helps distinguish expected withdrawal effects from relapse or unrelated medical issues.
Withdrawal management is not about speeding the process—it is about minimizing distress and preventing complications.
Medication-Assisted Treatment (MAT)
Unlike opioid or alcohol use disorders, Medication-Assisted Treatment (MAT) is not typically indicated for Effexor withdrawal. There are no substitute medications equivalent to methadone or buprenorphine for antidepressants.
However, medication support may still include:
-
Symptom-targeted medications (e.g., sleep aids, anti-nausea agents)
-
Temporary stabilization strategies if mood or anxiety symptoms spike
-
Dose-formulation adjustments (such as smaller dose reductions) to ease tapering
Clinical experience and observational evidence show that slow tapering combined with medical oversight significantly reduces withdrawal severity and discontinuation failure, while abrupt cessation increases relapse risk and functional impairment. [6]
Levels of Care
Inpatient / Residential Care (short-term, safety-focused):
Used only when withdrawal coincides with:
-
Severe depression or suicidal ideation
-
Inability to function or care for oneself
-
Significant psychiatric destabilization
The focus is stabilization, monitoring, and symptom relief—not long-term confinement.
Outpatient / Intensive Outpatient Programs (IOP):
Most individuals benefit from outpatient care or IOPs, which provide:
-
Therapy several times per week
-
Ongoing medication oversight
-
Emotional support while maintaining daily routines
These settings offer structure without unnecessary disruption to work or family life.
Therapies
Psychotherapy plays a critical role during Effexor withdrawal, particularly for managing emotional and cognitive symptoms.
Common approaches include:
-
Cognitive Behavioral Therapy (CBT): Helps reduce catastrophic thinking, health anxiety, and fear-driven symptom amplification.
-
Motivational Interviewing (MI): Supports confidence and commitment during a challenging tapering process.
-
Family Therapy: Improves communication, reduces misunderstanding, and strengthens external support.
Therapy also equips individuals with relapse-prevention skills, emotional regulation tools, and strategies for handling stress during neurochemical adjustment.
Peer Support & Recovery Capital
Social connection reduces isolation and normalizes the withdrawal experience. While Effexor withdrawal is not an addiction, peer support can still be valuable.
Options include:
-
Mental health support groups
-
Peer-led recovery or wellness communities
-
Online forums moderated by clinicians or mental health organizations
Building recovery capital—supportive relationships, stable routines, and access to care—improves resilience throughout withdrawal and beyond.
Holistic Supports (Adjunct)
Lifestyle-based supports do not replace medical care, but they meaningfully buffer withdrawal stress and support nervous system recovery.
Helpful adjuncts include:
-
Mindfulness and relaxation practices to calm autonomic nervous system activation
-
Gentle exercise, which supports mood regulation and sleep quality
-
Sleep hygiene strategies to stabilize circadian rhythms disrupted during tapering
-
Balanced nutrition and hydration, which support energy levels and brain health
These practices promote emotional steadiness and improve overall tolerance of the withdrawal process.
Withdrawal Timeline (What to Expect)
Effexor withdrawal does not follow a rigid schedule. Symptoms vary based on dose, duration of use, taper speed, and individual nervous system sensitivity. However, many people experience symptoms in phases.
Acute Phase (Days 1–7)
Symptoms often begin within 24–72 hours after a dose reduction or missed doses, because Effexor has a relatively short half-life.
Common physical symptoms include:
-
Dizziness or “brain zaps” (electric shock sensations)
-
Nausea, vomiting, or gastrointestinal upset
-
Headaches and flu-like aches
-
Fatigue or weakness
-
Sweating and temperature sensitivity
-
Balance issues or lightheadedness
-
Visual disturbances or sensitivity to light
These symptoms reflect sudden changes in serotonin and norepinephrine signaling and can feel alarming, but are usually temporary.
Protracted Phase (Weeks–Months)
Some individuals experience lingering or delayed symptoms, especially after long-term use or rapid tapering.
Common features include:
-
Persistent anxiety or inner restlessness
-
Mood swings or emotional sensitivity
-
Sleep disturbances or vivid dreams
-
Irritability or difficulty concentrating
-
Fear of relapse or health-related anxiety
Protracted symptoms do not mean permanent damage. They reflect slower neurochemical recalibration and typically improve with time and supportive care.
When to Seek Immediate Help?
While Effexor withdrawal is usually not dangerous, urgent medical evaluation is necessary if severe symptoms develop.
Seek immediate help if any of the following occur:
-
Severe or uncontrolled vomiting, inability to keep fluids down, or signs of dehydration
-
Hallucinations, confusion, or disorientation
-
Suicidal thoughts, self-harm urges, or sudden behavioral changes
-
Seizures or loss of consciousness
Emergency actions:
If symptoms are severe or life-threatening, contact local emergency services immediately or go to the nearest emergency department. Effexor is not an opioid, so naloxone is not effective for venlafaxine-related emergencies.
Dosing & Safety / Overdose Risks (For Legit Prescribing)
Typical Therapeutic Ranges & Formulations
-
Immediate-release venlafaxine: commonly prescribed in divided doses
-
Extended-release (XR): typically, 37.5 mg to 225 mg per day, depending on diagnosis and response
(Some patients may be prescribed higher doses under specialist care.)
Dosing should always be individualized and adjusted gradually.
High-Risk Combinations
Certain combinations increase the risk of adverse effects or overdose:
-
Alcohol, which can worsen sedation, dizziness, and mood instability
-
Benzodiazepines or other sedatives increasing cognitive impairment
-
Other serotonergic medications raising the risk of serotonin syndrome
Patients should always disclose all medications and supplements to their prescriber.
Overdose Mechanism
Effexor overdose does not cause respiratory depression like opioids. Instead, risks include:
-
Seizures
-
Heart rhythm disturbances
-
Serotonin syndrome
-
Severe agitation or altered mental status
Prompt medical treatment significantly improves outcomes.
Safe Use Guidelines
-
Take Effexor only as prescribed
-
Do not double doses if one is missed
-
Store medication securely, away from children
-
Never share prescriptions
-
Dispose of unused medication through approved take-back programs
Conclusion
Effexor withdrawal can be frightening—but it is understandable, manageable, and temporary.
With:
-
Informed medical care
-
Gradual tapering
-
Emotional support
-
Patience and compassion
People can regain stability, confidence, and quality of life.
Recovery is not about rushing. It is about listening to the nervous system and responding with care.
FAQs
No. Effexor is not addictive and does not produce cravings, euphoria, or compulsive drug-seeking behavior. However, physical dependence can occur, meaning the body adapts to the medication and may react when it is reduced or stopped.
The most significant risks involve abrupt discontinuation, which can lead to severe withdrawal symptoms, emotional instability, and functional impairment. In overdose situations, seizures and cardiac effects are the primary concerns.
Symptom flare-ups during tapering are often withdrawal-related, not a true relapse of depression or anxiety. This distinction matters. Relapse does not mean failure—it signals the need to slow the taper or adjust support.
Self-directed discontinuation is not recommended. Medical supervision allows for dose adjustments, symptom monitoring, and early intervention if complications arise. A supported taper is safer and more sustainable.
Families can help by:
- Learning about antidepressant withdrawal
- Avoiding pressure to “push through” symptoms
- Encouraging medical and therapeutic support
- Offering patience, reassurance, and emotional validation
Supportive environments reduce distress and improve outcomes.
Effexor withdrawal is usually not life-threatening, but it can be severely distressing and occasionally risky without supervision. Medical guidance ensures safety and prevents unnecessary suffering.







