Does Effexor Cause Weight Gain? Is It a Common Side Effect?
Effexor functions by blocking the reabsorption (reuptake) of serotonin and norepinephrine in the brain.
This increases their availability in synaptic spaces, helping improve mood, reduce anxiety, and enhance overall emotional balance.
However, these same neurotransmitters are also involved in hunger signals, satiety, and energy expenditure.
Key Takeaways
-
Effexor (venlafaxine) can affect weight differently for each person. Some may experience mild weight loss initially, while others notice gradual weight gain over time. These changes are often linked to appetite, metabolism, and improvements in mood rather than the medication alone.
-
Weight changes usually develop slowly over weeks to months, which makes them easier to manage if monitored early. Keeping track of appetite, daily habits, and body weight can help address small changes before they become persistent.
-
Combining healthy lifestyle habits with guidance from a healthcare provider supports long-term success. With proper monitoring and adjustments, patients can continue benefiting from Effexor without major impacts on overall well-being.
What Is Effexor and Why Is It Associated with Weight Gain?
Effexor, also known by its generic name venlafaxine, is a prescription antidepressant classified as a serotonin-norepinephrine reuptake inhibitor (SNRI).
It is widely prescribed for major depressive disorder, generalized anxiety disorder, panic disorder, and social anxiety disorder.
Unlike antidepressants that primarily target serotonin, Effexor works on two major neurotransmitters—serotonin and norepinephrine. [1] These brain chemicals are essential for mood regulation, emotional stability, stress response, energy levels, and appetite control.
Effexor functions by blocking the reabsorption (reuptake) of serotonin and norepinephrine in the brain. This increases their availability in synaptic spaces, helping improve mood, reduce anxiety, and enhance overall emotional balance.
However, these same neurotransmitters are also involved in hunger signals, satiety, and energy expenditure.
Because of this connection, some individuals may notice changes in appetite or weight during treatment. Importantly, these effects are indirect, not a direct fat-promoting action of the medication.
Potential contributors to weight changes include:
-
Mood improvement: As depression or anxiety improves, appetite may return to normal
-
Reduced stress: Lower anxiety can decrease appetite suppression
-
Lifestyle changes: Improved motivation may alter eating or activity patterns
-
Individual metabolism: Age, genetics, baseline weight, and hormonal factors
Understanding these influences helps patients view weight changes as part of the recovery process rather than an unavoidable medication side effect.
How Common Is Weight Gain with Effexor?
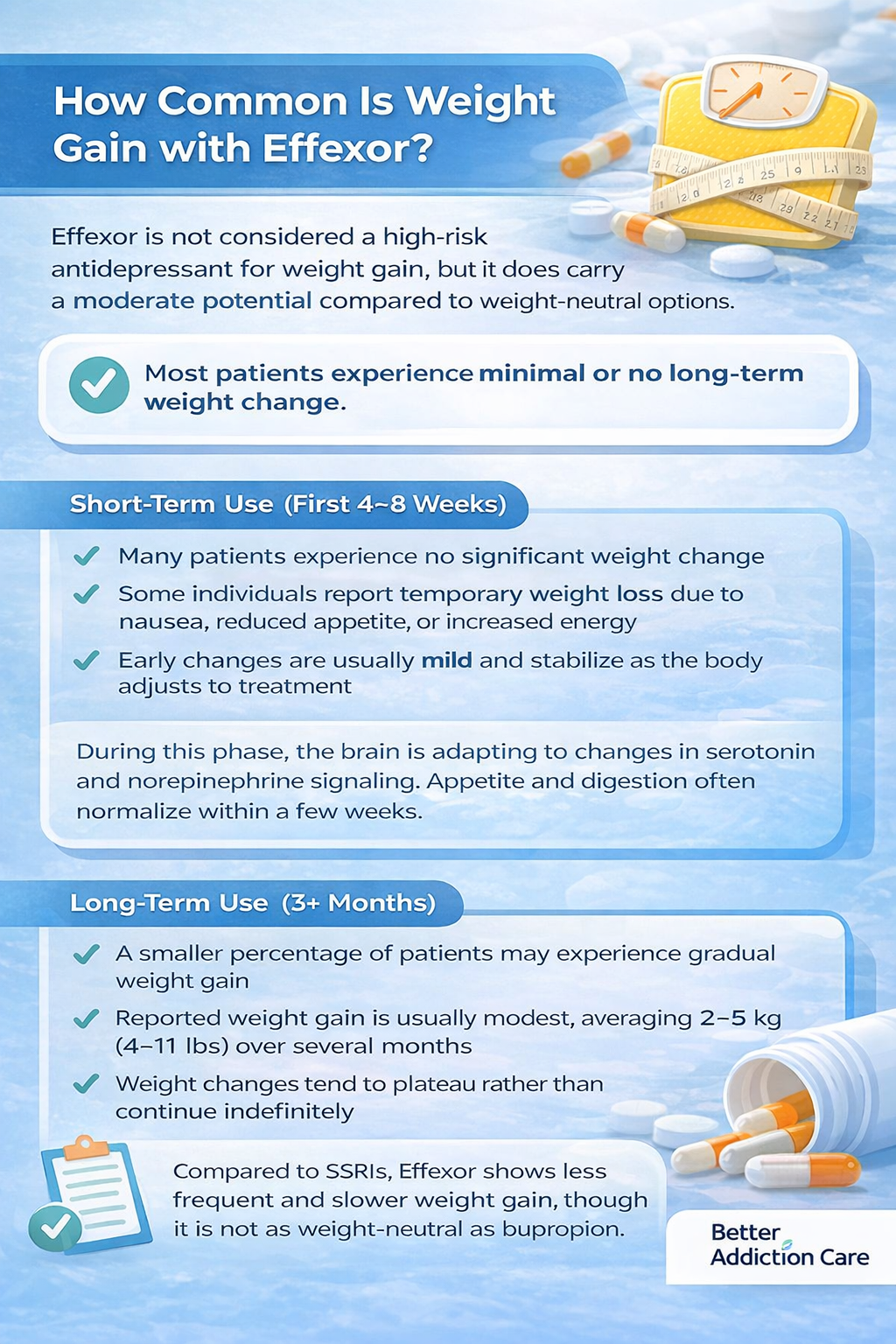
Effexor is not considered a high-risk antidepressant for weight gain, but it does carry a moderate potential compared to weight-neutral options.
Most patients experience minimal or no long-term weight change.
Short-Term Use (First 4–8 Weeks)
-
Many patients experience no significant weight change
-
Some individuals report temporary weight loss due to nausea, reduced appetite, or increased energy
-
Early changes are usually mild and stabilize as the body adjusts to treatment
During this phase, the brain is adapting to changes in serotonin and norepinephrine signaling. Appetite and digestion often normalize within a few weeks.
Long-Term Use (3+ Months)
-
A smaller percentage of patients may experience gradual weight gain
-
Reported weight gain is usually modest, averaging 2–5 kg (4–11 lbs) over several months
-
Weight changes tend to plateau rather than continue indefinitely
Compared to SSRIs, Effexor shows less frequent and slower weight gain, though it is not as weight-neutral as bupropion.
At-Risk Groups
Certain individuals may be more susceptible to weight changes:
-
Those with reduced physical activity
-
Patients whose depression previously suppressed their appetite
-
Individuals with metabolic conditions or insulin resistance
-
Long-term users without lifestyle adjustments
Family members may notice subtle increases in portion sizes, snacking frequency, or reduced movement before weight changes become visible. Early awareness allows for gentle, supportive guidance without creating stress.
Clinical Evidence
-
In clinical research, up to approximately 10–15% of patients on venlafaxine reported gaining at least 5% of their baseline body weight compared to a lower proportion in control groups, such as sertraline. [2]
-
Weight gain is more closely linked to treatment duration and behavioral factors than to dose alone.
Why Does Effexor Cause Weight Gain?
When weight changes occur with Effexor (venlafaxine), they are rarely caused by a single factor. Instead, weight gain usually develops through a combination of biological, hormonal, and behavioral changes that unfold gradually over time.
These effects can vary widely from person to person. Some individuals notice no change at all, while others experience slow but noticeable weight gain after several months of use.
Appetite and Hunger Regulation
Serotonin plays a major role in regulating appetite, satiety, and feelings of fullness after meals.
When serotonin levels stabilize with Effexor treatment, appetite may increase—especially in people who previously had a reduced appetite due to depression or anxiety.
In these cases, the return of hunger can feel sudden, leading to larger portion sizes or more frequent eating without conscious awareness.
Norepinephrine also affects appetite by influencing stress response and emotional eating patterns.
As anxiety decreases and emotional stability improves, appetite suppression caused by chronic stress may disappear.
This shift can lead to increased food intake, particularly comfort foods or carbohydrates that the body associates with emotional relief.
For many patients, this change reflects a return to “normal” eating rather than overeating. However, if calorie intake rises without adjustments in activity level, gradual weight gain can follow.
Metabolic Rate and Energy Balance
Effexor may subtly affect the body’s energy balance by influencing how calories are burned throughout the day. While it is not known to drastically slow metabolism, small changes in energy expenditure can still matter over time.
Some patients experience reduced restlessness, improved sleep, or relief from agitation.
While these improvements are beneficial for mental health, they may slightly lower daily calorie burn if physical activity levels remain the same.
Others may feel less driven to move or exercise as their nervous system becomes calmer.
In addition, improvements in fatigue may lead to more consistent eating patterns, which can increase total daily caloric intake.
These metabolic and energy-related changes are usually minor on their own, but when sustained over weeks or months, they can gradually contribute to weight gain.
Hormonal Influences
Antidepressants like Effexor may indirectly influence hormones that regulate hunger and fullness.
These hormones help signal when to eat and when to stop, and even small disruptions can affect appetite.
Key hormones involved include:
-
Leptin, which signals fullness and helps regulate long-term energy balance
-
Ghrelin, which stimulates hunger and increases food-seeking behavior [3]
In some individuals, changes in these hormonal signals may lead to eating before true physical hunger develops or feeling less satisfied after meals.
While these effects are generally mild and not experienced by everyone, hormonally sensitive people may notice increased cravings or difficulty recognizing satiety cues.
These hormonal shifts do not usually cause rapid weight gain, but they can reinforce gradual changes in eating behavior over time.
Behavioral and Lifestyle Factors
As mood improves with Effexor treatment, many patients naturally return to healthier daily routines. While this is a positive outcome, it can unintentionally increase calorie intake.
Common behavioral changes include:
-
Eating more regular meals after periods of appetite loss
-
Participating in social meals with family or friends
-
Snacking more frequently throughout the day
-
Relaxing strict food rules that were previously used during illness
These shifts often reflect emotional recovery rather than unhealthy habits. However, without mindful portion control or routine physical activity, total calorie intake may increase beyond the body’s needs.
Families and caregivers can play a supportive role by encouraging balanced meals, consistent eating schedules, and enjoyable physical activities rather than focusing on weight alone.
Creating a supportive environment helps maintain both mental well-being and long-term physical health.
Is Weight Gain from Effexor Permanent?
In most cases, weight gain associated with Effexor is not permanent and can be managed effectively.
Weight Gain Often Stabilizes
-
Research shows weight changes often plateau within 6–12 months
-
Appetite increases frequently represent a return to baseline eating patterns
-
Continued, unchecked gain is uncommon with early lifestyle adjustments
Reversibility with Medical Guidance
-
Gradual tapering or medication adjustments under medical supervision often lead to weight normalization
-
Dose optimization may reduce appetite effects
-
Weight changes usually reverse slowly rather than abruptly
In rare cases where weight gain persists, management strategies include:
-
Structured nutrition planning
-
Consistent physical activity routines
-
Mindful eating practices
-
Medical review of treatment options
Weight change should be framed as a manageable side effect—not a failure of treatment or self-control.
How Can Weight Gain Be Managed While Taking Effexor?
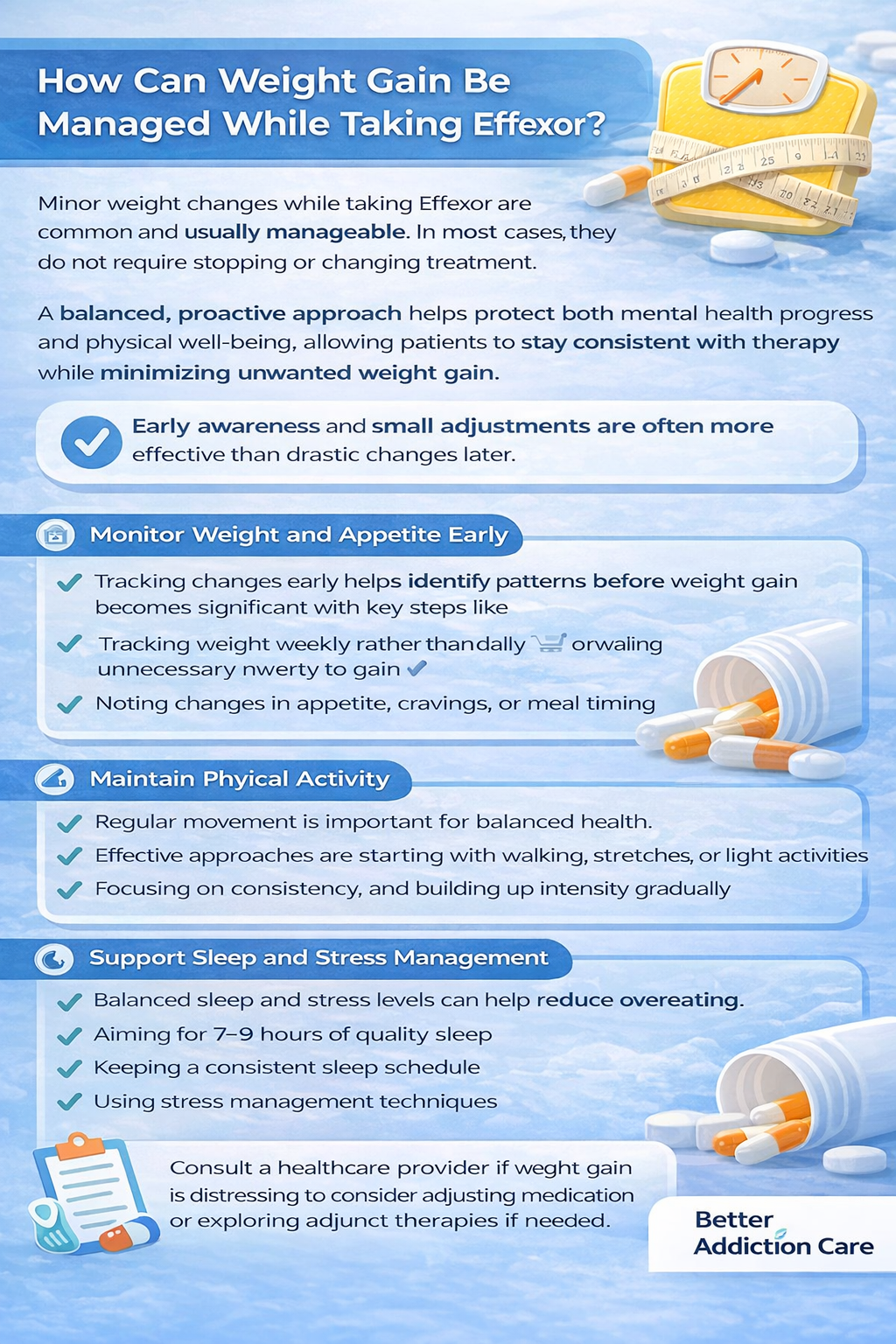
Minor weight changes while taking Effexor are common and usually manageable. In most cases, they do not require stopping or changing treatment.
A balanced, proactive approach helps protect both mental health progress and physical well-being, allowing patients to stay consistent with therapy while minimizing unwanted weight gain.
Early awareness and small adjustments are often more effective than drastic changes later.
1. Monitor Weight and Appetite Early
Tracking changes early helps identify patterns before weight gain becomes significant. Small increases are easier to manage when addressed promptly.
Key steps include:
-
Tracking weight weekly rather than daily to avoid unnecessary anxiety
-
Noting changes in appetite, cravings, or meal timing
-
Paying attention to emotional eating triggers
-
Setting realistic expectations for minor fluctuations during treatment initiation
Weight can naturally fluctuate due to water retention, improved appetite, or changes in routine. Recognizing what is temporary versus persistent helps guide appropriate responses without overreacting.
2. Optimize Nutrition
Nutrition plays a central role in managing weight while on antidepressants. The goal is not restriction, but balance and consistency.
Helpful strategies include:
-
Emphasizing lean proteins, vegetables, fruits, and whole grains to support satiety
-
Planning meals and snacks ahead of time to reduce impulsive eating
-
Choosing high-fiber foods that promote fullness and stabilize blood sugar
-
Staying well-hydrated, as thirst can mimic hunger
-
Practicing portion awareness rather than strict calorie counting
Structured eating patterns can help prevent overeating driven by restored appetite or improved mood. Consistent meals also support energy levels and emotional stability.
3. Maintain Physical Activity
Regular movement supports both mental health and metabolic balance. It does not need to be intense to be effective.
Recommended approaches include:
-
Starting with walking, stretching, or gentle yoga
-
Incorporating light resistance or bodyweight exercises as tolerated
-
Focusing on consistency rather than duration or intensity
-
Choosing activities that feel enjoyable and sustainable
Physical activity improves insulin sensitivity, supports energy expenditure, and enhances mood—often reinforcing the benefits of Effexor rather than competing with them.
4. Support Sleep and Stress Management
Sleep and stress have a direct impact on appetite-regulating hormones. Poor sleep increases hunger signals and reduces feelings of fullness.
Supportive strategies include:
-
Aiming for 7–9 hours of quality sleep per night
-
Keeping consistent sleep and wake times
-
Reducing screen exposure before bedtime
-
Using mindfulness, breathing exercises, or relaxation techniques to manage stress
Reducing emotional and stress-related eating is often easier when sleep quality improves and stress levels are better regulated.
5. Discuss Medical Options
If lifestyle strategies are not effective or weight gain becomes distressing, medical guidance is essential.
Possible discussions with a healthcare professional may include:
-
Reviewing medication dosage and timing
-
Assessing whether weight changes are medication-related or lifestyle-related
-
Exploring adjunct therapies that support metabolic balance
-
Considering alternative treatments if clinically appropriate
Medication should never be adjusted or discontinued without professional guidance. Mental health stability remains the top priority, and any changes should be made thoughtfully and safely.
When Should I Talk to My Doctor About Weight Gain?
Early consultation ensures peace of mind and prevents long-term issues.
Red Flags for Medical Review
-
Rapid gain of 2–3 kg (4–6 lbs) in a short period
-
Weight changes without a dietary or activity explanation
-
Metabolic concerns (blood sugar, cholesterol, blood pressure)
-
Emotional distress related to weight changes
How Your Doctor Can Help?
-
Review treatment plan
-
Assess metabolic and lifestyle factors
-
Recommend nutrition or activity support
-
Adjust medication if necessary
Seeking guidance is proactive—not a sign of failure.
Can Weight Gain Be Prevented When Starting Effexor?
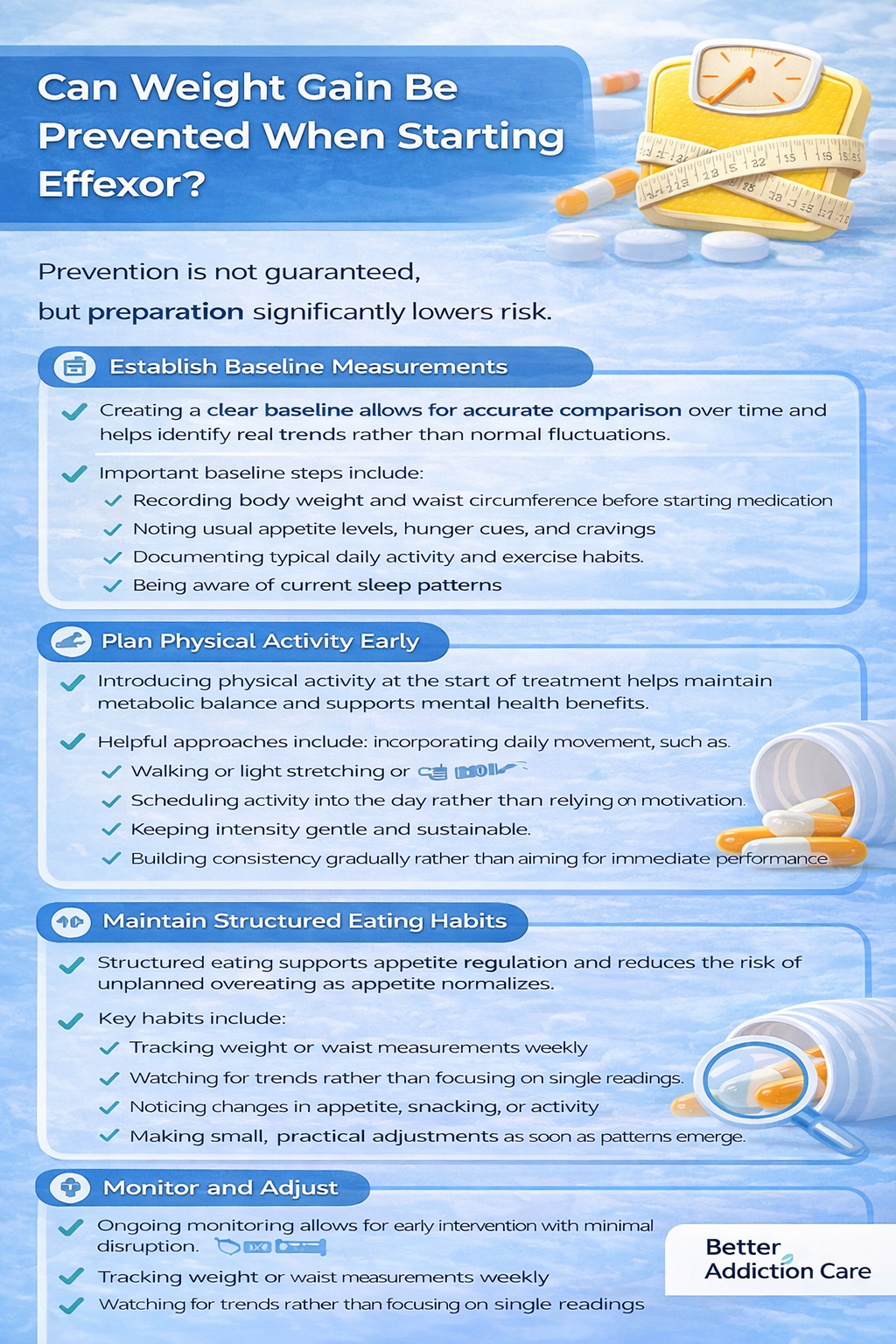
Prevention is not guaranteed, but preparation significantly lowers risk.
1. Establish Baseline Measurements
Creating a clear baseline allows for accurate comparison over time and helps identify real trends rather than normal fluctuations.
Important baseline steps include:
-
Recording body weight and waist circumference before starting medication
-
Noting usual appetite levels, hunger cues, and cravings
-
Documenting typical daily activity and exercise habits
-
Being aware of current sleep patterns
These measurements provide context and prevent unnecessary concern over short-term changes that may be unrelated to medication.
2. Plan Physical Activity Early
Introducing physical activity at the start of treatment helps maintain metabolic balance and supports mental health benefits.
Helpful approaches include:
-
Incorporating daily movement, such as walking or light stretching
-
Scheduling activity into the day rather than relying on motivation
-
Keeping intensity gentle and sustainable
-
Building consistency gradually rather than aiming for immediate performance
Early activity routines are easier to maintain long-term and reduce the likelihood of gradual weight accumulation.
3. Maintain Structured Eating Habits
Structured eating supports appetite regulation and reduces the risk of unplanned overeating as appetite normalizes.
Key habits include:
-
Eating regular meals at consistent times
-
Choosing nutrient-dense foods that promote fullness and stable energy
-
Including protein and fiber at each meal
-
Avoiding skipped meals, which can trigger rebound hunger later in the day
Predictable eating patterns help align hunger signals with true physical needs rather than emotional or stress-driven cues.
4. Monitor and Adjust
Ongoing monitoring allows for early intervention with minimal disruption.
Effective monitoring includes:
-
Tracking weight or waist measurements weekly
-
Watching for trends rather than focusing on single readings
-
Noticing changes in appetite, snacking, or activity
-
Making small, practical adjustments as soon as patterns emerge
Early changes are easier to manage and reduce the need for more intensive interventions later.
5. Communicate with Your Healthcare Provider
Open communication improves treatment outcomes and prevents unnecessary frustration.
Patients are encouraged to:
-
Share weight-related concerns proactively
-
Discuss appetite or energy changes during follow-ups
-
Ask questions about expected side effects
-
Review options early if changes become concerning
Early discussion allows adjustments that preserve both treatment effectiveness and quality of life, without compromising mental health progress.







