Vyvanse Addiction And Abuse: The Dangers And Risks
Vyvanse is a central nervous system stimulant and Schedule II controlled substance. It increases dopamine and norepinephrine in the brain to improve focus and impulse control.
As Vyvanse enhances dopamine, it can produce effects that lead to tolerance, dependence, and addiction, particularly when misused.

Key Takeaways
-
Vyvanse (lisdexamfetamine) is a prescription stimulant used for ADHD and binge eating disorder. Unlike antidepressants, stimulant medications do carry a real risk of abuse because of their dopamine-enhancing effects.
-
While Vyvanse is designed as a prodrug (becoming active only after digestion), misuse is still possible — especially through overuse, dose escalation, or combining it with other stimulants.
-
Stopping Vyvanse too quickly may trigger withdrawal symptoms, including fatigue, low mood, irritability, and sleep changes.
-
Misuse often begins when someone feels they “need” Vyvanse to stay productive, focused, or emotionally regulated. This psychological reinforcement increases risk.
-
With supervised care, structured tapering, and behavioral support, most people can safely discontinue Vyvanse and rebuild healthy functioning.
Many people start Vyvanse during periods of overwhelming workload, untreated ADHD symptoms, or when daily functioning feels out of control. Suddenly, they can concentrate again, tasks feel manageable, and life becomes more organized.
But months later, anxiety sometimes emerges:
“I don’t feel normal without my dose,” or “I’m scared I won’t be productive if I stop.”
These fears do not always reflect addiction—but they can fuel patterns of dependence, misuse, and escalating use.
This article explains what Vyvanse addiction really means, how misuse develops, warning signs, and the safest ways to stop.
What Is Vyvanse Addiction?
Vyvanse (lisdexamfetamine) is a central nervous system stimulant and Schedule II controlled substance. It increases dopamine and norepinephrine in the brain to improve focus and impulse control. [1] Because Vyvanse enhances dopamine — a key neurotransmitter in reward — it can produce effects that lead to tolerance, dependence, and addiction, particularly when misused.
Tolerance
Some people feel that their usual dose no longer provides the same level of focus or energy, leading them to think they “need more” to function.
Dependence
Over time, the brain adapts to daily stimulant exposure. Without Vyvanse, people may feel mentally “slowed,” fatigued, anxious, or unable to concentrate — classical dependence symptoms.
Addiction
Addiction involves:
-
Cravings
-
Loss of control
-
Continued use despite harm
-
Seeking Vyvanse for emotional or performance enhancement
Unlike antidepressants, addiction to Vyvanse is well-documented and is a primary reason it’s tightly regulated.
Signs & Symptoms of Vyvanse Misuse

Vyvanse misuse does not always look dramatic. It often starts subtly — taking an extra dose “just to get through the day.” Over time, signs become more noticeable.
Physical Signs
-
Increased heart rate and blood pressure — stimulants place stress on the cardiovascular system, which may cause palpitations or a racing heartbeat.
-
Insomnia or a reduced need for sleep — people may stay awake for long stretches and feel wired even at night.
-
Loss of appetite and noticeable weight loss — Vyvanse suppresses hunger, often leading to skipped meals and nutritional deficiencies.
-
Persistent dry mouth and frequent headaches — both are common side effects that become more intense with higher doses.
-
Jitteriness, tremors, or physical restlessness — overactivation of the nervous system can cause shaking or a sense of being unable to sit still.
-
Overheating or excessive sweating — stimulants can interfere with body temperature regulation.
-
Energy crashes or extreme fatigue when the drug wears off — often followed by irritability, lethargy, or the urge to redose.
Emotional & Psychological Signs
-
Irritability, mood swings, or emotional numbing — emotional instability may increase as the brain becomes dependent on stimulant effects.
-
Anxiety, panic, or agitation — especially during comedowns, dose delays, or skipped days.
-
Feeling unable to function or think clearly without Vyvanse — dependence may appear as fear of losing productivity or cognitive ability.
-
Using Vyvanse for motivation rather than medical necessity — taking it to feel energized, confident, or capable rather than for ADHD symptom relief.
-
Obsessive focus on productivity, grades, or performance — the medication becomes tied to self-worth or achievement. [2]
-
Cravings for the emotional “lift” or sense of control Vyvanse provides — a strong internal pull to take more even when aware of risks.
Behavioral Signs
-
Taking higher doses than prescribed — increasing the amount to maintain effects or avoid fatigue.
-
Grinding, snorting, or manipulating capsules — less common, but a clear indicator of unsafe use aimed at intensifying effects.
-
Doctor-shopping or seeking early refills — going to multiple providers or claiming lost pills to access more medication.
-
Mixing Vyvanse with caffeine, nicotine, alcohol, or other stimulants — done to enhance alertness or prolong wakefulness, often increases medical risks.
-
Staying awake for long periods to study, work, or focus intensely — using the drug to push through exhaustion or meet deadlines.
-
Hiding use from friends, family, or coworkers — concealing dosing habits, minimizing how much is taken, or using secretly.
-
Prioritizing getting or taking the medication over responsibilities — rearranging routines around the drug, or panicking when it’s unavailable.
How Common Is Problematic Vyvanse (lisdexamfetamine) Use?
General prevalence
Nonmedical use and problematic use of prescription stimulants (including amphetamine-type medicines such as lisdexamfetamine/Vyvanse) is less common than some media portrayals, but still important to monitor.
National surveys show that a small but meaningful percentage of people report past-year misuse of prescription stimulants; rates are higher in adolescents and young adults and among people who already receive stimulant prescriptions.
In a 2025 U.S. national survey of adults prescribed stimulants, 25.3% reported past-year misuse and 9.0% met criteria for prescription stimulant use disorder (PSUD), with amphetamines (including lisdexamfetamine) disproportionately represented. [3]
Clinical settings
Clinically, groups more likely to struggle with problematic Vyvanse use or stimulant misuse include:
-
Adolescents and young adults (college-age) — highest rates of nonmedical use.
-
People with a prior substance use disorder or other substance-use risk factors.
-
Patients who divert their prescription (sell/share) or obtain multiple prescriptions.
-
People who escalate dose, crush or inject oral formulations, or combine stimulants with alcohol/other drugs — behaviours that raise the risk of addiction and adverse events.
Misuse prevalence varied by age: approximately 3.1% of young adults (18–25) reported past-year prescription stimulant misuse, compared with about 1.2% of adults 26+, demonstrating higher risk in younger populations. [4]
Withdrawal Frequency
When people stop or sharply reduce prolonged stimulant use, many experience a recognizable withdrawal syndrome — though exact prevalence estimates vary by population (medical prescription users vs. people using amphetamines frequently/recreationally).
Clinical reviews and trial reports indicate that withdrawal symptoms after stopping amphetamine-type stimulants commonly occur and are clinically relevant for people who have used them regularly for weeks to months.
Among chronic and heavy amphetamine users, research suggests that 80–97% experience withdrawal symptoms after abrupt discontinuation, with symptoms like fatigue, dysphoria, and mood changes lasting days to weeks. [5]
Causes: Why Does Vyvanse Addiction Happen?
Neurobiology (How Vyvanse Affects the Brain)
Vyvanse (lisdexamfetamine) is a prodrug, meaning it becomes active only after the body converts it into dextroamphetamine. This slow conversion was designed to reduce misuse, but it still significantly increases dopamine and norepinephrine in key brain regions, especially those involved in:
-
reward
-
motivation
-
attention
-
emotional regulation
-
executive functioning
The result is a noticeable boost in:
-
Focus and sustained attention
-
Energy and alertness
-
Motivation and goal-directed behavior
-
Productivity, task initiation, and mental stamina
These effects make the brain quickly form a learned association:
Vyvanse = productivity, capability, control, and emotional stability.
Over time, this becomes a powerful reinforcement loop, especially in people who already struggle with motivation or attention. Once this loop forms, the brain begins to rely on the stimulant to function at its “new normal.”
When the medication wears off, or a dose is missed, the brain produces fewer neurotransmitters on its own, leading to:
-
exhaustion
-
irritability
-
poor focus
-
mental fog
-
emotional flattening
This rebound discomfort often triggers the urge to take more medication, strengthening the addiction cycle.
Genetic & Biological Factors
Some individuals are biologically predisposed to stimulants, having a stronger or more rewarding effect. Factors that heighten vulnerability include:
-
ADHD or dopamine-related neurobiology — the brain may naturally produce lower dopamine, making stimulant effects feel essential.
-
Family history of addiction — inherited traits can influence reward sensitivity and impulse regulation.
-
High dopamine sensitivity — some people experience more intense “reward” from stimulants, increasing reinforcement.
-
Thyroid issues or metabolic disorders — these can amplify stimulant effects, making the medication feel unusually energizing or regulating.
-
Underlying anxiety, depression, or mood instability — stimulants may temporarily improve mood, creating emotional dependence.
Biological stressors such as hormonal shifts, chronic stress, irregular meals, dehydration, and sleep deprivation can intensify both the high and the crash, increasing the likelihood of misuse.
Psychological & Emotional Triggers
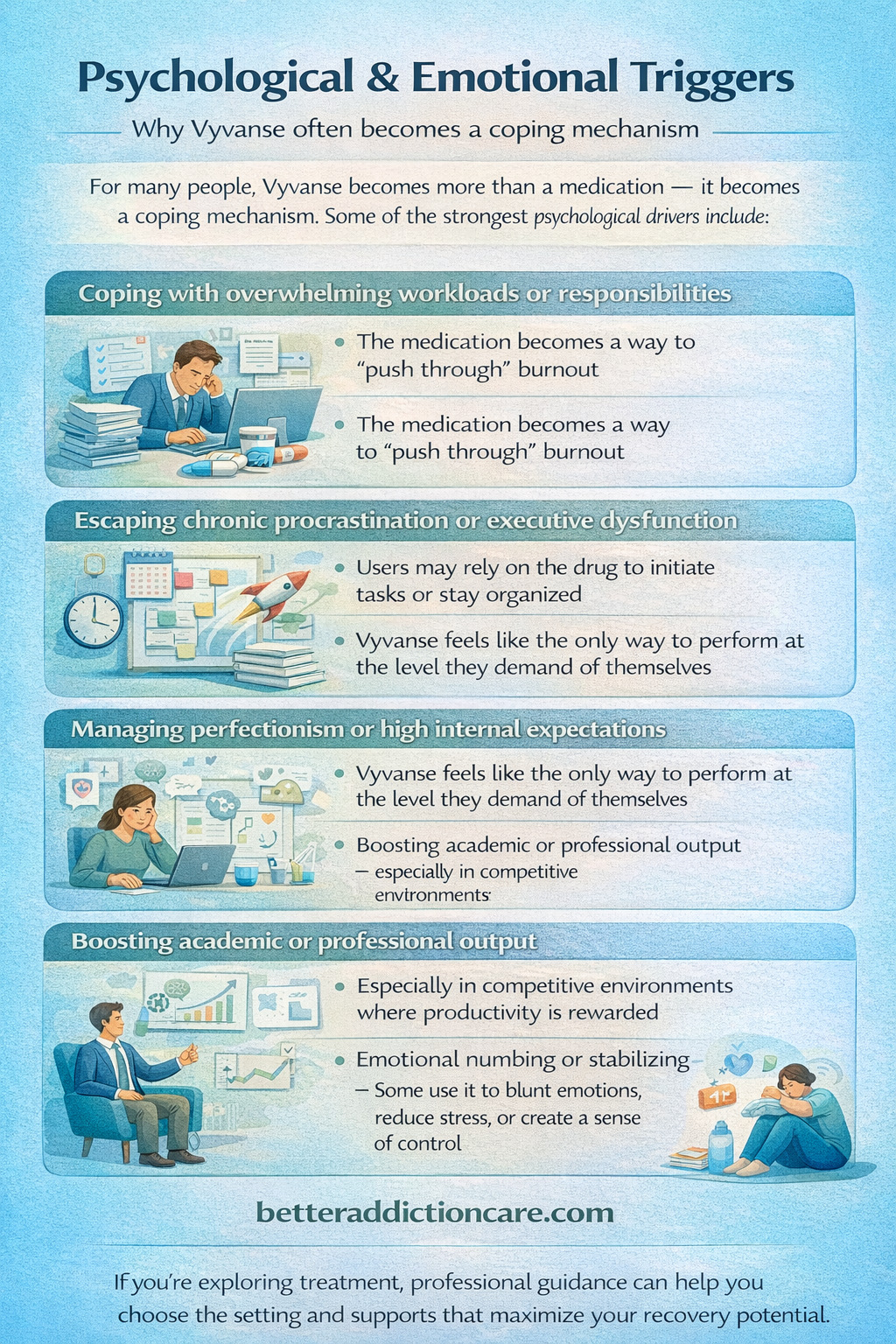
For many people, Vyvanse becomes more than a medication — it becomes a coping mechanism. Some of the strongest psychological drivers include:
-
Coping with overwhelming workloads or responsibilities — the medication becomes a way to “push through” burnout.
-
Escaping chronic procrastination or executive dysfunction — users may rely on the drug to initiate tasks or stay organized.
-
Managing perfectionism or high internal expectations — Vyvanse feels like the only way to perform at the level they demand of themselves.
-
Boosting academic or professional output — especially in competitive environments where productivity is rewarded.
-
Emotional numbing or stabilizing — some use it to blunt emotions, reduce stress, or create a sense of control.
Environmental & Social Factors
Context and environment play a major role in shaping misuse. Common contributors include:
-
Intense academic or workplace pressure — environments that reward output over wellbeing make stimulants appealing.
-
Cultural normalization of extreme productivity — “hustle culture” encourages pushing limits, often with chemical help.
-
Easy access through friends, classmates, coworkers, or online channels — increasing the chance of unprescribed use.
-
Social acceptance of “study drugs” — especially in campuses or in competitive fields where stimulant misuse is common.
-
Lack of education about the risks of dependence — people assume prescriptions are inherently safe, even though misuse can be dangerous.
From Treatment to Dependence
Vyvanse addiction rarely evolves overnight. It follows a gradual, predictable pattern in which a helpful medication slowly becomes something a person feels unable to function without. This progression can happen even when someone begins treatment with full medical supervision.
1. Diagnosis & Initial Benefit
At first, Vyvanse provides the intended effects: clearer focus, improved task initiation, better emotional regulation, and consistent productivity. Many people describe finally feeling “normal,” organized, or capable of meeting daily responsibilities.
2. Emotional Reliance on the Medication
As functioning improves, the person begins to psychologically anchor their stability and success to the medication. They may start believing:
-
“I can’t keep up without it.”
-
“This is the only way I perform well.”
This emotional connection deepens the internal pressure to maintain or increase use.
3. Tolerance Development
Over time, the brain adjusts to stimulant levels, and the original dose feels weaker. Tasks that once felt easy again become effortful, leading the person to think they “need” a slightly higher dose for the same level of clarity, drive, or mood stability.
4. Compensatory or Situational Overuse
As tolerance grows, the person may begin taking:
-
extra doses on stressful days
-
additional capsules to study longer
-
more medication to push through fatigue or deadlines
Vyvanse shifts from a scheduled treatment to a tool for managing life pressure.
5. Withdrawal Avoidance
Eventually, missing a dose triggers physical and emotional discomfort — exhaustion, irritability, mood crashes, anxiety, or mental fog. Instead of taking Vyvanse to improve ADHD symptoms, the person takes it to avoid crashing. This “avoidance loop” is a key turning point toward dependence.
6. Full Dependence
At this stage, Vyvanse is used to maintain basic functioning rather than treating symptoms. The person may feel:
-
unable to work, study, or socialize without it
-
emotionally flat or depressed off-medication
-
physically drained unless they redose
The drug becomes central to stability, productivity, and self-perception — marking the transition from therapeutic use to addiction. [1]
Who Is Most at Risk?
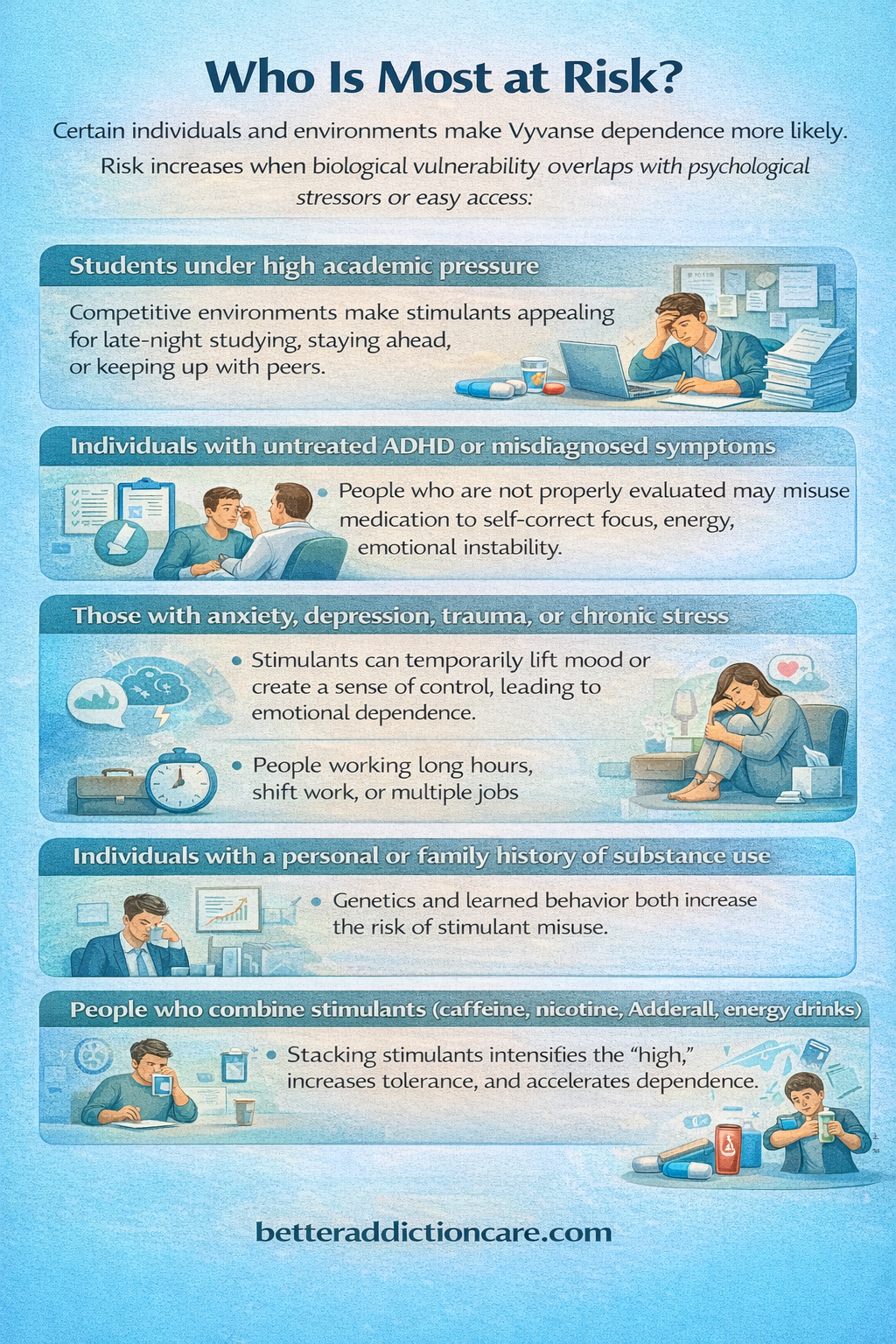
Certain individuals and environments make Vyvanse dependence more likely. Risk increases when biological vulnerability overlaps with psychological stressors or easy access.
-
Students under high academic pressure: Competitive environments make stimulants appealing for late-night studying, staying ahead, or keeping up with peers.
-
Individuals with untreated ADHD or misdiagnosed symptoms: People who are not properly evaluated may misuse medication to self-correct focus, energy, or emotional instability.
-
Those with anxiety, depression, trauma, or chronic stress: Stimulants can temporarily lift mood or create a sense of control, leading to emotional dependence.
-
People working long hours, shift work, or multiple jobs: Vyvanse becomes a way to stay awake, meet deadlines, or push through exhaustion.
-
Individuals with a personal or family history of substance use: Genetics and learned behavior both increase the risk of stimulant misuse.
-
People who combine stimulants (caffeine, nicotine, Adderall, energy drinks): Stacking stimulants intensifies the “high,” increases tolerance, and accelerates dependence.
Side Effects of Vyvanse Addiction
Short-Term Effects of Vyvanse Misuse
Misusing Vyvanse — taking higher doses, using it without a prescription, or combining it with other stimulants — overstimulates the central nervous system. Short-term effects can appear within hours and range from uncomfortable to dangerous. [1]
-
Anxiety, irritability, and agitation: Stimulant overactivation heightens the fight-or-flight response, leading to restlessness, emotional volatility, and difficulty calming down.
-
Insomnia and disrupted sleep patterns: Vyvanse’s long duration (10–14 hours) makes it easy to stay awake far beyond normal limits, which quickly destabilizes mood and energy cycles.
-
Heart palpitations or racing heartbeat: Increased catecholamines (dopamine/norepinephrine) speed up heart activity, making people feel on edge or physically overstimulated.
-
Loss of appetite and noticeable weight loss: Vyvanse suppresses hunger signals, often causing skipped meals, dehydration, and nutritional deficits.
-
Risk of dehydration: Increased energy output, reduced thirst cues, and prolonged wakefulness contribute to fluid loss and overheating.
-
Elevated blood pressure: Blood vessels constrict, and heart workload increases, especially when combined with caffeine or nicotine.
-
Intense “crash” when the medication wears off: This can include exhaustion, low mood, irritability, headaches, and mental fog — often driving the urge to redose.
Severe Short-Term Risks
-
Cardiac events (rare but possible): High doses can strain the heart, increasing the risk of arrhythmias, chest pain, or, in extreme cases, cardiac complications. [1]
-
Psychosis or stimulant-induced paranoia: Heavy misuse can trigger hallucinations, extreme suspiciousness, or delusional thinking, especially in individuals predisposed to mental health disorders.
-
Serotonin syndrome (when combined with SSRIs/SNRIs): Vyvanse affects monoamine levels, and mixing it with serotonergic medications can cause dangerous symptoms like confusion, fever, rapid heart rate, or muscle rigidity.
Long-Term Effects of Vyvanse Misuse
Chronic misuse changes the brain’s dopamine pathways and places ongoing stress on the body. Over time, these effects become more pronounced and harder to reverse.
-
Emotional blunting or reduced ability to feel pleasure: Constant dopamine stimulation can dull emotional responsiveness, causing detachment or apathy.
-
Chronic sleep disruption: Persistent insomnia leads to memory problems, irritability, poor judgment, and burnout.
-
Physical dependence and escalating tolerance: Higher doses become necessary for the same effect, and going without the medication causes withdrawal symptoms.
-
Malnutrition and sustained weight loss: Long-term appetite suppression may result in vitamin deficiencies, weakened immunity, and muscle loss.
-
Memory issues and cognitive fatigue: The overstimulation-crash–crash cycle impairs working memory, focus, and decision-making.
-
Cardiovascular strain: Prolonged stimulant exposure can elevate blood pressure, stress the heart, and contribute to long-term heart risks.
-
Increased depression and mood instability during withdrawal: Low dopamine levels during “off periods” can lead to sadness, emotional sensitivity, or hopelessness.
-
Binge–crash behavioral cycles: Periods of extreme productivity followed by emotional collapse can destabilize routines, reduce consistency, and increase dependence.
Impact on Daily Life
Vyvanse misuse doesn’t only affect the body — it disrupts daily functioning, relationships, and long-term stability.
-
Declining work or academic performance during crashes: People may be highly productive on medication but struggle with consistency, leading to missed deadlines or burnout.
-
Strained relationships due to irritability, mood swings, or withdrawal symptoms: Loved ones may notice aggression, emotional distance, or unpredictable behavior.
-
Difficulty functioning without Vyvanse: Normal tasks feel overwhelming, increasing panic or fear of going without medication.
-
Financial strain from overuse or doctor-shopping: People may spend significantly on extra prescriptions, travel, or online sources.
-
Social withdrawal: Fatigue, anxiety, or shame around misuse can lead to isolation and reduced engagement.
-
Increased risk-taking behaviors: Impulsivity, sleep deprivation, and overconfidence can contribute to unsafe driving, overspending, substance mixing, or dangerous decision-making.
Treatment Options for Vyvanse Misuse or Addiction

Effective treatment requires a personalized, multi-layered plan that addresses the biological, psychological, and social drivers of stimulant misuse. [6] Most people benefit from a combination of medical care, structured therapy, behavioral supports, and lifestyle stabilization. The goal is not just stopping the drug, but restoring healthy functioning, mood balance, and long-term recovery skills.
Detox / Withdrawal Management
Vyvanse withdrawal can be physically and emotionally challenging, especially for individuals taking high doses or using the drug daily. Because of this, detox should always be supervised rather than attempted abruptly.
Why “Cold Turkey” Is Discouraged?
Stopping Vyvanse suddenly may trigger:
-
extreme fatigue
-
depression or emotional crash
-
intense cravings
-
cognitive fog
-
sleep disturbances
-
return of untreated ADHD symptoms
A monitored detox prevents destabilization and reduces relapse risk during this vulnerable phase.
Supportive Medical Interventions
Clinicians may recommend:
-
Gradual tapering to reduce withdrawal intensity and allow the brain to rebalance dopamine/norepinephrine.
-
Adjunct medications (case-specific) to manage symptoms such as anxiety, insomnia, depression, or blood pressure changes.
-
Scheduled sleep and nutrition monitoring to support stabilization.
Medication-Assisted Treatment (MAT)
Note: These medications are not used to treat stimulant withdrawal directly but may be used when co-occurring opioid or alcohol use disorders are present, or when a patient needs relapse-prevention support.
-
Methadone: A long-acting opioid agonist that stabilizes cravings, reduces withdrawal, and prevents opioid misuse in individuals with co-occurring opioid addiction.
-
Buprenorphine: A partial opioid agonist that reduces cravings and withdrawal with a lower risk of respiratory depression; supports stability in dual-diagnosis cases.
-
Naltrexone: An opioid antagonist that blocks euphoric effects and reduces cravings for alcohol and opioids; may be used to support relapse-prevention in polydrug misuse.
-
Evidence: Medication-assisted treatment consistently reduces relapse rates and mortality in people with substance use disorders and is considered a gold-standard approach when applicable.
Levels of Care (Choosing the Right Treatment Setting)
Inpatient / Residential Treatment (30–90 days)
Best for individuals with severe dependence, repeated relapse, or unstable home environments. Benefits include:
-
24-hour support and monitoring
-
medical and psychiatric care
-
structured routine
-
separation from triggers
-
intensive therapy and skills development
Intensive Outpatient Programs (IOP) / Standard Outpatient
Intensive Outpatient Program is suitable for those with moderate addiction or strong social support. Includes:
-
therapy 3–5 days per week
-
regular medical check-ins
-
medication monitoring
-
relapse-prevention planning
-
continued work/school involvement
This level allows individuals to maintain daily responsibilities while receiving consistent treatment.
Therapies Used in Stimulant Addiction Treatment
A comprehensive therapy plan addresses the psychological drivers of misuse, emotional regulation, and behavior patterns.
-
Cognitive Behavioral Therapy (CBT): Helps identify distorted thinking patterns, manage cravings, build coping strategies, and change behaviors linked to stimulant use.
-
Motivational Interviewing (MI): Strengthens internal motivation for change, especially in people unsure about stopping use.
-
Family Therapy (Behavioral or Systems-Based Models): Addresses relationship strain, communication issues, and environmental triggers that influence misuse.
-
Skills-based training: Focus on emotional regulation, stress management, productivity without stimulants, and relapse-prevention strategies.
Peer Support & Recovery Capital
Long-term recovery improves when individuals build social and community resources that reinforce healthy habits.
-
NA and stimulant-specific recovery groups
-
SMART Recovery, Refuge Recovery, or other secular alternatives
-
Peer mentorship, sober communities, and accountability partners
-
Community health resources, vocational training, and academic support
Recovery capital strengthens stability and reduces isolation — a major relapse risk factor.
Holistic Supports (Adjunct Approaches)
Although not primary treatments, holistic supports play an important role in restoring balance and resilience:
-
Mindfulness and grounding practices — help reduce cravings and improve emotional regulation.
-
Regular exercise — stabilizes dopamine, mood, and sleep patterns.
-
Sleep hygiene — essential for recovery after stimulant-induced sleep disruption.
-
Balanced nutrition and hydration — rebuilds energy, reduces fatigue, and corrects malnutrition.
-
Stress-reduction practices: yoga, breathing exercises, nature exposure, journaling.
These supports help individuals feel better physically and mentally, improving treatment adherence.
Withdrawal Timeline (What to Expect)
Withdrawal varies based on dose, duration, age, health status, and co-occurring conditions. The timeline generally has two stages:
Acute Withdrawal (Days 1–7)
Common symptoms may include:
-
extreme fatigue
-
irritability
-
increased appetite
-
low mood or depressive crash
-
headaches
-
slowed thinking
-
anxiety or restlessness
-
sleep disturbances (insomnia or hypersomnia)
Protracted Withdrawal (Weeks to Months)
After acute symptoms fade, many individuals continue to experience:
-
persistent anxiety
-
Ongoing mood swings
-
strong cravings
-
memory lapses or difficulty focusing
-
low motivation and energy
-
disrupted sleep cycles
-
sensitivity to stress
Supportive therapy and medical monitoring are essential during this stage to prevent relapse and rebuild consistent functioning. [7]
When to Seek Immediate Help?
-
Chest pain, fainting, or severe heart symptoms
-
Agitation, paranoia, hallucinations
-
Suicidal thoughts during withdrawal
-
Severe dehydration or inability to eat
-
Overdose symptoms (extreme agitation, high fever, seizures)
Dosing, Safety & Overdose Risks
-
Typical doses: 30–70 mg daily, depending on clinical need
-
Never combine with other stimulants
-
Avoid mixing with alcohol, cocaine, or high caffeine intake
-
Overdose risk increases significantly when misused
Conclusion
Vyvanse can be life-changing for people with ADHD or binge eating disorder, restoring focus, stability, and emotional clarity. But because it affects the brain’s reward system, it carries a real risk of dependence, misuse, and addiction.
The good news is that recovery is entirely possible. With gradual tapering, proper psychiatric support, and therapy, most people regain healthy functioning and rebuild confidence without relying on stimulants.
Next Steps:
-
Reach out for a professional evaluation.
-
Choose the right level of care based on symptoms.
-
Build a supportive network of family, peers, and clinicians.
FAQs
Yes. Unlike antidepressants, Vyvanse has a real addiction risk due to dopamine elevation.
Fatigue, increased sleep, low mood, irritability, and cravings.
Depends on dose and duration. Tapers can range from several weeks to several months.
Yes, many patients do so under prescriber guidance.
Contact your clinician immediately or seek emergency care for heart symptoms or suicidal thoughts.







