Wellbutrin Withdrawal: Symptoms, Causes, and Coping Strategies
Wellbutrin (bupropion) is an antidepressant that increases dopamine and norepinephrine, two neurotransmitters that play major roles in mood stability, focus, energy, and emotional regulation.
When Wellbutrin is stopped abruptly, the brain suddenly loses a consistent level of these chemicals. This rapid shift forces the nervous system into “catch-up mode,” where it struggles to regain equilibrium. That temporary imbalance is what creates withdrawal symptoms.
Key Takeaways
-
Is withdrawal real? Yes. Stopping Wellbutrin (bupropion) too quickly can lead to predictable discomfort as the brain recalibrates dopamine and norepinephrine levels after long-term use. These symptoms are temporary and improve gradually with a slowed tapering schedule.
-
How should I stop safely? The safest method is a medically supervised, stepwise taper that allows the nervous system to adjust in small increments. This significantly reduces the intensity of emotional, physical, and neurological symptoms.
-
What helps recovery? Structured routines, family involvement, steady sleep habits, therapeutic support, and gradual lifestyle adjustments help stabilize mood and ease the transition during the first 2–6 weeks of withdrawal.
Why does stopping suddenly cause withdrawal?
The brain adapts to the predictable presence of Wellbutrin. A sudden drop disrupts communication between mood-regulating circuits, similar to how abruptly turning off a loud fan leaves your ears adjusting to the sudden quiet. This neurological readjustment period can create dizziness, sleep disruption, irritability, or fatigue.
Withdrawal vs. relapse
Families often worry that withdrawal means a relapse into depression. The timing helps distinguish them:
-
Withdrawal begins within 24–72 hours of a dose reduction and often improves after 2–4 weeks.
-
Relapse builds more gradually and may worsen over weeks without improvement.
A healthcare provider helps ensure the right interpretation so your loved one gets the appropriate support.
Withdrawal does not mean addiction.
There are no cravings, compulsive use patterns, or reward-driven behaviors associated with antidepressants. Withdrawal reflects physiological readjustment, not addiction.
What Are the Common Symptoms of Wellbutrin Withdrawal?
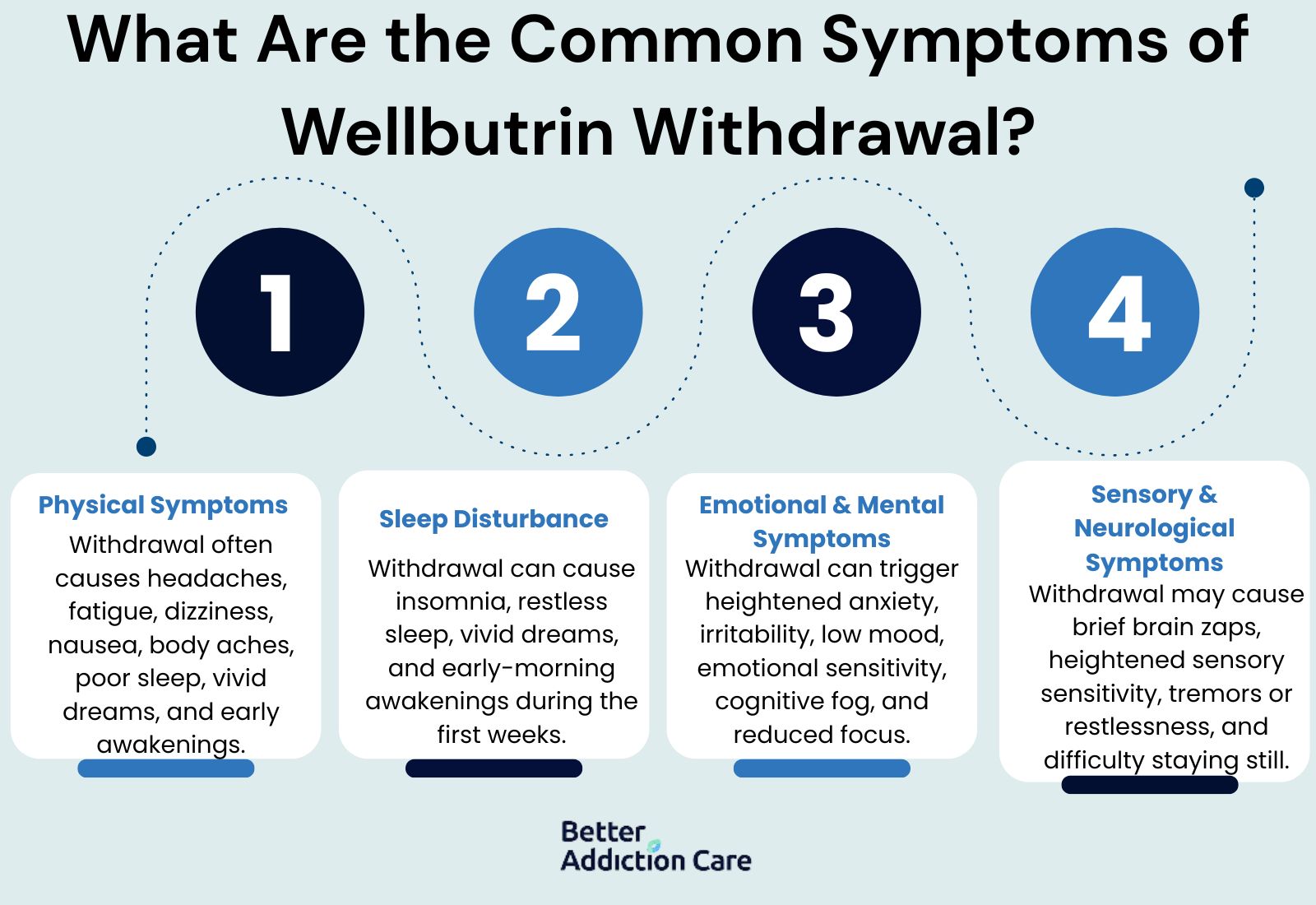
Withdrawal symptoms appear because the brain and nervous system need time to stabilize after dosage reductions. They vary widely depending on how long someone has taken Wellbutrin, their dose, and how quickly changes occur.
Physical Symptoms
Physical discomfort often appears early as the body adjusts to shifting norepinephrine levels. Many people describe experiences such as:
-
Head pressure, throbbing headaches, or a sensation of “tightness” around the temples that fluctuates throughout the day
-
General fatigue that makes simple tasks feel harder, especially during the first week of tapering
-
Dizziness, unsteadiness, or “floating” sensations that intensify when standing quickly or moving suddenly
-
Nausea or digestive upset, particularly if tapering occurred during a period of high stress
-
Body aches, chills, or sensations similar to mild flu that resolve as neurotransmitters rebalance
These symptoms typically ease as the nervous system adapts to each dose reduction. Many people report noticeable improvement by Week 3.
Sleep Disturbances
Sleep difficulties are common because dopamine helps regulate circadian rhythms. People often report:
-
Trouble falling asleep or waking up multiple times during the night
-
Restless or light sleep that feels unrefreshing
-
Vivid or unsettling dreams as the brain recalibrates its sleep architecture
-
Early-morning awakenings during the first 1–2 weeks of withdrawal
These sleep changes usually settle as the taper slows and neurotransmitter activity becomes more predictable.
Emotional and Mental Health Symptoms
Because Wellbutrin influences mood pathways, emotional symptoms can emerge during withdrawal. These may include:
-
Heightened anxiety, restlessness, or a sense of emotional “tension” that feels disproportionate to the situation
-
Irritability or quick frustration, which families often notice before the individual does
-
Temporary dips in mood, tearfulness, or emotional sensitivity that improve with routine, reassurance, and a slower taper
-
Cognitive fog, difficulty staying focused, or slowed processing speed during the peak adjustment period
These emotional fluctuations are expected and often brief when tapering is done gradually.
Sensory or Neurological Symptoms
Some individuals experience unusual sensations as the nervous system rebalances:
-
Brief electrical “brain zaps” or jolts that occur when shifting gaze, turning the head, or moving from resting to active
-
Increased sensitivity to bright lights or loud sounds
-
Moments of tremors, jitteriness, or inner restlessness
-
Short periods of pacing or difficulty sitting still
These neurological symptoms are uncomfortable but temporary and typically improve once tapering slows.
What Is the Typical Wellbutrin Withdrawal Timeline?
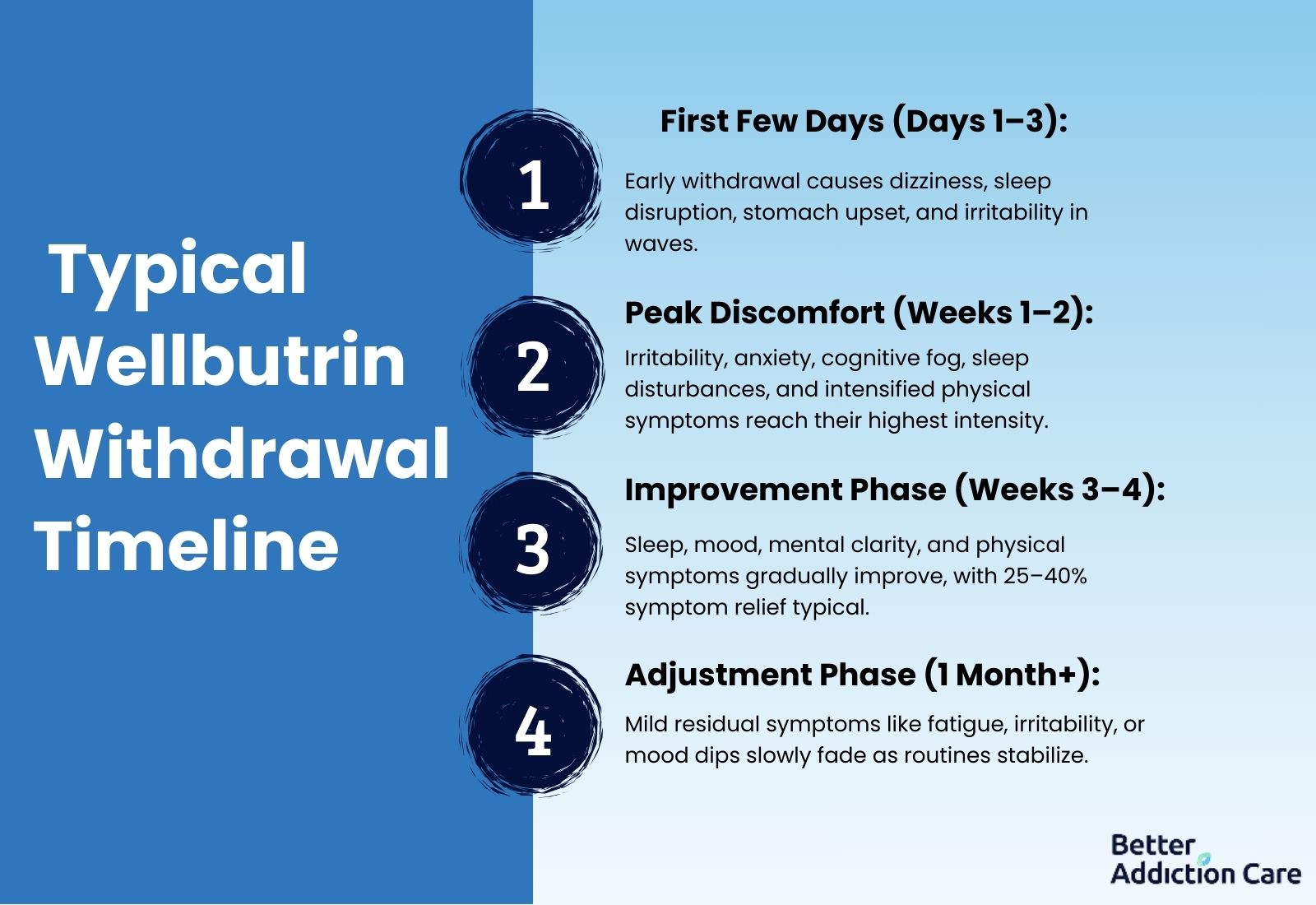
Every nervous system adapts at its own pace. However, the pattern below reflects what many families report through tapering monitored by a healthcare provider.
Withdrawal Timeline
First Few Days (Days 1–3): Early Adjustment
Withdrawal begins subtly. People often notice soft dizziness, disrupted sleep, stomach discomfort, or irritability. Symptoms may appear in waves rather than consistently.
Peak Discomfort (Weeks 1–2): Strongest Symptoms
This phase brings the most noticeable changes:
-
Increased irritability or emotional sensitivity
-
Difficulty concentrating or feeling mentally “foggy”
-
Heightened anxiety or internal restlessness
-
Nighttime awakenings or inconsistent sleep
-
Intensified physical symptoms such as dizziness or nausea
If symptoms are significant at this stage, tapering may need to slow down.
Improvement Phase (Weeks 3–4): Gradual Stabilization
Most people experience steady improvement:
-
Sleep begins normalizing
-
Mood fluctuations become milder
-
Mental clarity improves
-
Physical discomfort decreases
On average, many individuals notice 25–40% symptom improvement by the end of Week 4 after an appropriately paced taper (1,2).
Adjustment Phase (1 Month+): Residual Symptoms Fade
Some mild symptoms—such as occasional irritability, short bursts of fatigue, or brief mood dips—may continue. These typically lessen as healthy habits, routines, and sleep stabilize.
Why Should Wellbutrin Be Tapered Slowly?
Stopping Wellbutrin abruptly can cause severe mood destabilization, pronounced neurological symptoms, and insomnia. A slow taper is safer because it protects the nervous system from dramatic changes.
Cold-turkey risks
Abrupt discontinuation increases the likelihood of:
-
Heightened anxiety or panic
-
Severe sleep disturbances
-
Emotional crashes or difficulty regulating mood
-
Physical symptoms that interfere with daily functioning
-
Misinterpreted relapse signals
Benefits of a slow taper
A gradual taper:
-
Allows dopamine and norepinephrine circuits to adjust in manageable steps
-
Reduces symptom intensity
-
Stabilizes mood more reliably
-
Makes relapse far less likely
-
Helps families identify true mental health needs once the medication is removed
Medical supervision ensures the taper is customized to the person—not rushed by a fixed timeline.
What Helps Manage Wellbutrin Withdrawal Symptoms?
Support from mental health professionals is essential. Providers track symptom patterns, guide tapering, and offer tools to reduce discomfort.
How do healthcare providers help?
-
Adjusting taper steps: Providers may slow tapering if symptoms intensify or life stress becomes overwhelming.
-
Distinguishing relapse from withdrawal: Clinicians track timing, intensity, and symptom patterns to identify when a relapse may be starting—allowing intervention before symptoms become severe.
-
Offering short-term relief options: In some cases, providers may recommend non-addictive medications or behavioral interventions to stabilize sleep, anxiety, or concentration.
-
Monitoring for safety concerns: Regular appointments ensure emotional stability and provide families with a clear support structure.
What Coping Strategies Help Manage Withdrawal Symptoms?
These strategies help the nervous system regulate itself during tapering. They are most effective when consistently practiced and supported by family routines.
1. How Can I Improve My Sleep?
Prioritizing sleep is essential during withdrawal.
Establish a predictable bedtime and wake time every day, even on weekends, to reinforce the brain’s circadian rhythm.
Reduce exposure to screens and bright lights in the final hour before sleep and replace that stimulation with calming activities such as reading, gentle stretching, or a warm shower.
If nighttime anxiety interferes with falling asleep, grounding techniques—like slow breathing, weighted blankets, or a cool, dark sleep environment—may help the nervous system transition into rest.
Families can support this by keeping evenings calm and predictable.
2. What Should I Eat and Drink During Withdrawal?
Hydration and balanced nutrition support neurotransmitter recovery.
Aim for 6–8 glasses of water per day and include meals with steady protein sources that stabilize blood sugar.
Foods rich in omega-3 fatty acids, B vitamins, and complex carbohydrates provide nutritional building blocks that support neurological function.
Limiting caffeine during the first 2–3 weeks may reduce jitteriness and help regulate sleep.
3. Should I Exercise?
Gentle physical activity helps regulate dopamine pathways.
Instead of intense workouts, begin with 20–30 minutes of walking, stretching, or low-impact movement.
Exercise increases blood flow to the prefrontal cortex—an area involved in mood regulation—and can lessen emotional intensity.
The goal is consistency, not performance, and families can help by joining or encouraging movement without pressuring.
4. How Can I Reduce Stress and Anxiety?
Withdrawal can heighten the stress response.
Breathing exercises with extended exhalations (e.g., inhale for 4 seconds, exhale for 6 seconds) activate the parasympathetic nervous system.
Journaling first thing in the morning helps externalize anxiety that builds overnight. Sensory grounding—soft lighting, warm drinks, quiet spaces—calms overstimulated neural pathways.
Mindfulness practices, even just 5 minutes per day, also help retrain attention circuits.
5. How Can I Stay Connected and Supported?
Social support is one of the strongest predictors of smoother withdrawal.
Daily check-ins with loved ones build emotional stability, especially when symptoms fluctuate.
Structured family routines—shared meals, walks, or brief conversations—reduce feelings of isolation.
Peer support groups (virtual or in person) provide reassurance that symptoms are temporary and manageable.
6. Does Routine Matter?
Routine offers stability during neurochemical change.
Regular waking times, meal schedules, light exercise, and planned activities help regulate the brain’s internal clock.
Predictability reduces anxiety, strengthens emotional consistency, and prevents the “drift” that can occur when withdrawal disrupts motivation.
When Should I Seek Medical Help During Withdrawal?
Families and individuals should contact a provider immediately if withdrawal symptoms escalate beyond manageable discomfort. Urgent concerns include:
-
Suicidal thoughts, feelings of hopelessness, or dramatic mood changes
-
Severe insomnia lasting more than 5–7 nights without relief
-
Panic attacks or emotional overwhelm
-
Inability to maintain daily responsibilities at work, school, or home
-
Significant physical symptoms such as intense dizziness, chest discomfort, or shaking
-
Signs of depression returning rather than improving
Prompt medical oversight can prevent symptom progression and support emotional safety.
What Comes After Withdrawal? (Long-Term Recovery)
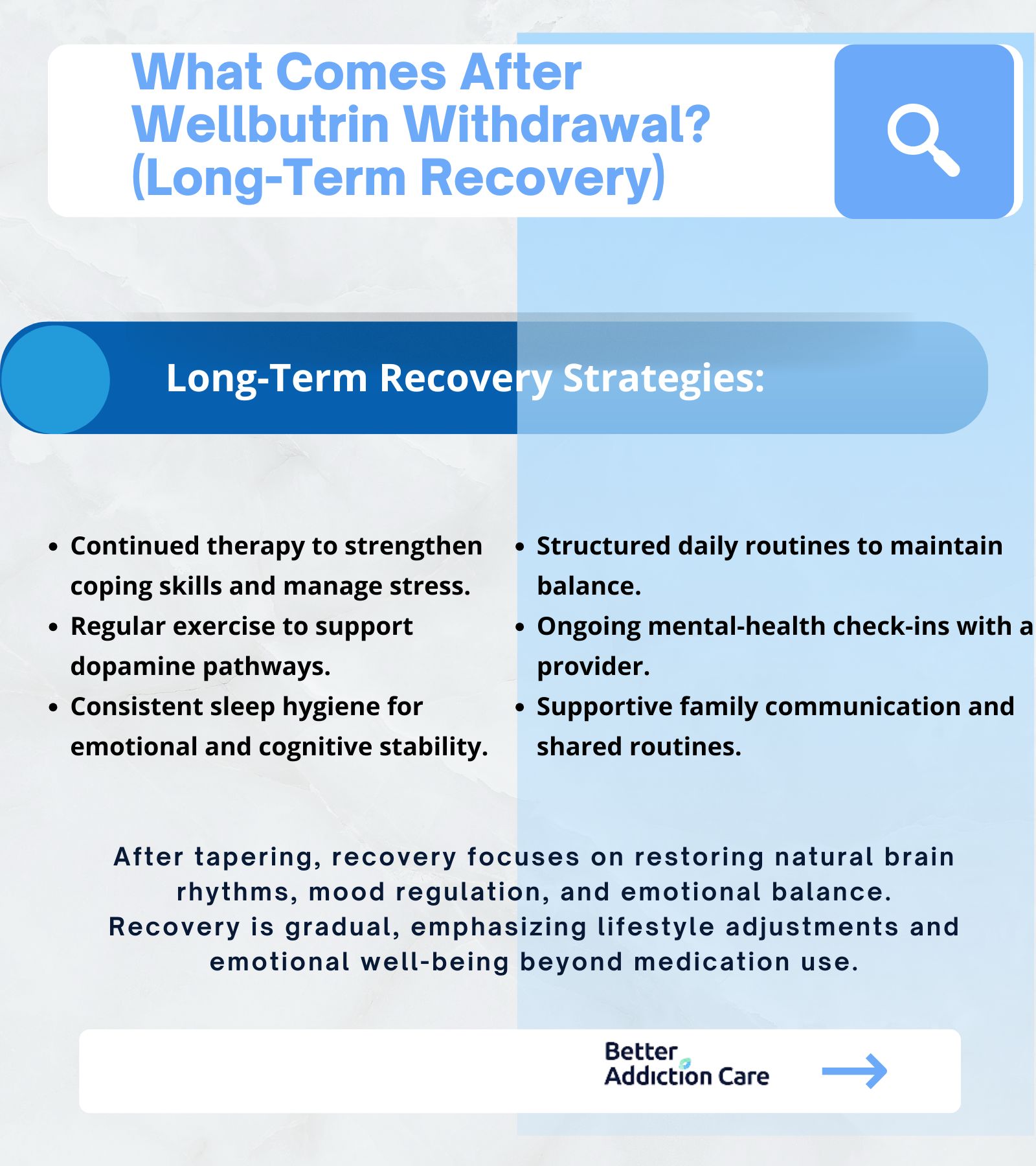
Completing the taper is only one step. Over the next 1–3 months, the brain continues re-establishing natural rhythms and strengthening mood regulation systems.
This is often when individuals begin recognizing their baseline emotional patterns without medication.
Long-term strategies supporting recovery:
-
Continued therapy to build coping skills and manage stress
-
Regular physical activity that supports dopamine pathways
-
Consistent sleep hygiene practices
-
Structured daily routines that reinforce emotional stability
-
Ongoing mental-health check-ins with a provider
-
Supportive family communication and shared routines
-
Long-term recovery is about rediscovering balance and making gradual adjustments to protect emotional well-being.
Conclusion
Wellbutrin withdrawal is temporary, manageable, and a sign that the brain is adjusting—not failing. When tapering is slow and supported, symptoms follow a predictable arc of discomfort followed by steady improvement. Families can provide stability and reassurance through routine, calm environments, and emotional presence.
With patience, structured habits, and medical supervision, most people regain emotional balance and move forward confidently into long-term recovery.
Abruptly stopping the medication is never recommended—gradual change consistently leads to better outcomes.
FAQs
Quitting suddenly significantly increases withdrawal symptoms and can destabilize mood regulation. A cold-turkey stop often leads to severe irritability, sleep disruption, and physical discomfort. Additionally, symptoms may be mistaken for relapse. A slow, medically supervised taper is the safest and most effective way to discontinue Wellbutrin.
For many people, the most intense symptoms occur during the first 1–2 weeks, with gradual improvement beginning soon after. By Weeks 3–4, most individuals notice substantial relief, though some may experience lingering fatigue or occasional mood dips for a month or more. Taper speed and consistency have a major impact on the timeline.
It’s possible—but not inevitable. Withdrawal symptoms can mimic relapse, which is why timing and symptom pattern matter. Withdrawal begins quickly after dose changes, while relapse develops slowly. Staying connected with a provider helps determine if therapy, lifestyle adjustments, or further taper modifications are needed.
Sleep routines, hydration, steady nutrition, light exercise, mindfulness practices, and predictable daily structure all support the nervous system. Family involvement—such as shared walks, quiet evenings, and gentle communication—also helps regulate emotions during the adjustment period.
Loved ones can help by maintaining calm routines, offering patient emotional support, reducing daily stressors, and validating the difficulty of withdrawal. Encouraging healthy habits—without pressuring—builds trust and makes the process smoother. Observing for mood changes and offering to join appointments can help ensure safety.
Contact a provider immediately. The taper may be too fast or require adjustment. No one should endure severe withdrawal; medical guidance ensures safety and prevents prolonged distress. In some cases, stabilizing at a previous dose or adjusting the taper schedule makes symptoms far more manageable.







