Inpatient Mental Health Program: Definition, Programs, Process, Cost
Inpatient mental health programs provide a structured and supportive environment for individuals struggling with severe mental health conditions. These programs offer round-the-clock medical and therapeutic care, ensuring that patients receive intensive support tailored to their needs. Designed for those requiring stabilization and long-term treatment, inpatient care helps individuals regain mental wellness through comprehensive interventions.

Inpatient mental health programs provide a structured and supportive environment for individuals struggling with severe mental health conditions. These programs offer round-the-clock medical and therapeutic care, ensuring that patients receive intensive support tailored to their needs. Designed for those requiring stabilization and long-term treatment, inpatient care helps individuals regain mental wellness through comprehensive interventions.
In 2023, the U.S. had 1,184 inpatient mental health facilities out of 12,012 total mental health treatment centers, highlighting the limited availability of intensive care options, according to a report by Statista. With 15.4 million U.S. adults experiencing serious mental illness (SMI) in 2022, only 66.7% received treatment, as reported by NIMH, underscoring the important role of inpatient programs in providing structured, 24/7 care for those in need.
Various evidence-based treatment approaches are utilized in inpatient mental health programs, including Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), medication management, and trauma-focused therapies. These treatments help individuals develop coping skills, regulate emotions, and address underlying psychological conditions. Group therapy, family therapy, and holistic interventions like mindfulness and stress reduction are also integral to recovery.
Inpatient mental health programs work as a structured process that begins with a thorough assessment and evaluation to create a personalized treatment plan. Patients participate in individual and group therapy, medication management, psychoeducation, and skill-building sessions under the guidance of mental health professionals. Continuous monitoring, crisis intervention, and discharge planning ensure a seamless transition to outpatient care and long-term recovery.
The cost of inpatient mental health programs varies widely, ranging from $5,000 to over $30,000 per month, depending on the facility, length of stay, and level of care provided. Factors influencing cost include staff qualifications, specialized treatments, and insurance coverage. While some programs accept insurance, others require out-of-pocket expenses or financial assistance options.
What is an Inpatient Mental Health Program?
An Inpatient Mental Health Program is a residential treatment option where individuals stay at a specialized facility 24/7 to receive intensive care for severe mental health conditions. This structured approach provides a highly supervised environment where patients have access to round-the-clock medical support, individual and group therapy, medication management, and crisis intervention. Inpatient treatment is designed for those experiencing acute psychiatric symptoms, such as severe depression, suicidal thoughts, psychosis, or self-harming behaviors, who require constant monitoring to ensure safety and stability.
These programs are an important step in stabilizing individuals before they transition to outpatient or partial hospitalization programs (PHPs) for continued care. Treatment duration varies based on individual needs, ranging from a few days to several weeks. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), in 2021, approximately 14.1 million adults in the U.S. had a serious mental illness (SMI), many of whom required intensive inpatient treatment to manage their condition effectively. By providing structured therapy, medication adjustments, and a supportive environment, inpatient programs help patients regain stability and develop coping skills for long-term recovery.
What is the purpose of the Inpatient Mental Health Program?
The purpose of an inpatient mental health program is to provide intensive, 24/7 care for individuals struggling with severe mental health conditions or co-occurring substance use disorders, ensuring their safety, stabilization, and long-term recovery. These programs offer a structured environment where patients receive medical supervision, therapy, and support to address their mental health challenges effectively.
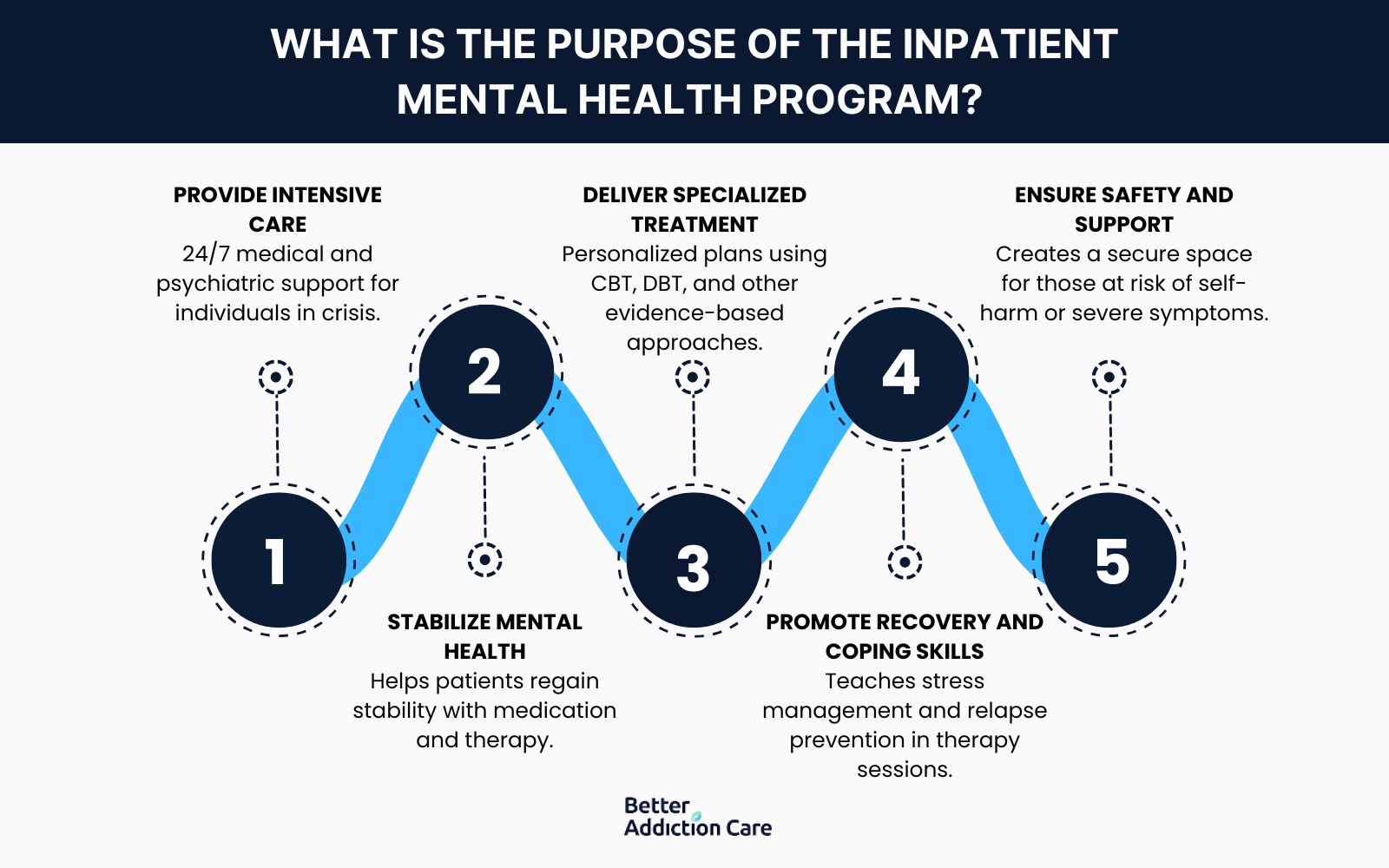
The purpose of an inpatient program is as follows:
-
Provide Intensive Care: Inpatient programs offer round-the-clock medical and psychiatric supervision to individuals experiencing acute mental health crises. This high level of care is important for those dealing with severe depression, anxiety disorders, schizophrenia, or substance withdrawal that require constant monitoring and immediate intervention.
-
Stabilize Mental Health: A key goal is to stabilize patients in crisis, ensuring they receive proper medication management, structured therapy sessions, and crisis intervention. According to the National Institute of Mental Health (NIMH), approximately 5.5% of U.S. adults experience a severe mental illness (SMI) annually, many of whom require inpatient care to regain stability.
-
Deliver Specialized Treatment: Inpatient programs provide personalized treatment plans, incorporating cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT), and medication-assisted treatment (MAT). These evidence-based approaches help address both mental health disorders and co-occurring substance use issues for comprehensive recovery.
-
Promote Recovery and Coping Skills: Patients participate in individual and group therapy, where they learn effective coping mechanisms, stress management techniques, and relapse prevention strategies. A study by Balachander S,et al. 2020, titled “Long-term Outcomes of Intensive Inpatient Care for Severe, Resistant Obsessive-Compulsive Disorder,” shows that structured inpatient care significantly improves long-term treatment outcomes, particularly for individuals at high risk of relapse. Intensive inpatient care for severe OCD showed significant improvement, with 50% of patients responding and 21% partially responding, while long-term follow-up identified 14.5% as remitters, 36.5% as responders, 34.7% as minimal responders, and 14.6% as nonresponders.
-
Ensure Safety and Support: Many individuals admitted to inpatient programs face suicidal thoughts, self-harm risks, or severe psychiatric symptoms that require a secure and supportive environment. By removing external stressors and providing constant professional care, inpatient programs create a safe space for recovery, reducing the risk of harm or hospitalization recurrence.
What are the Common Disorders Treated in an Inpatient Mental Health Program?
The common disorders treated in an inpatient mental health program are depression, anxiety disorders, bipolar disorder, schizophrenia, PTSD, OCD, eating disorders, borderline personality disorder, substance use disorders, and panic disorder. These conditions require intensive, structured care with 24/7 supervision to stabilize symptoms and promote recovery.
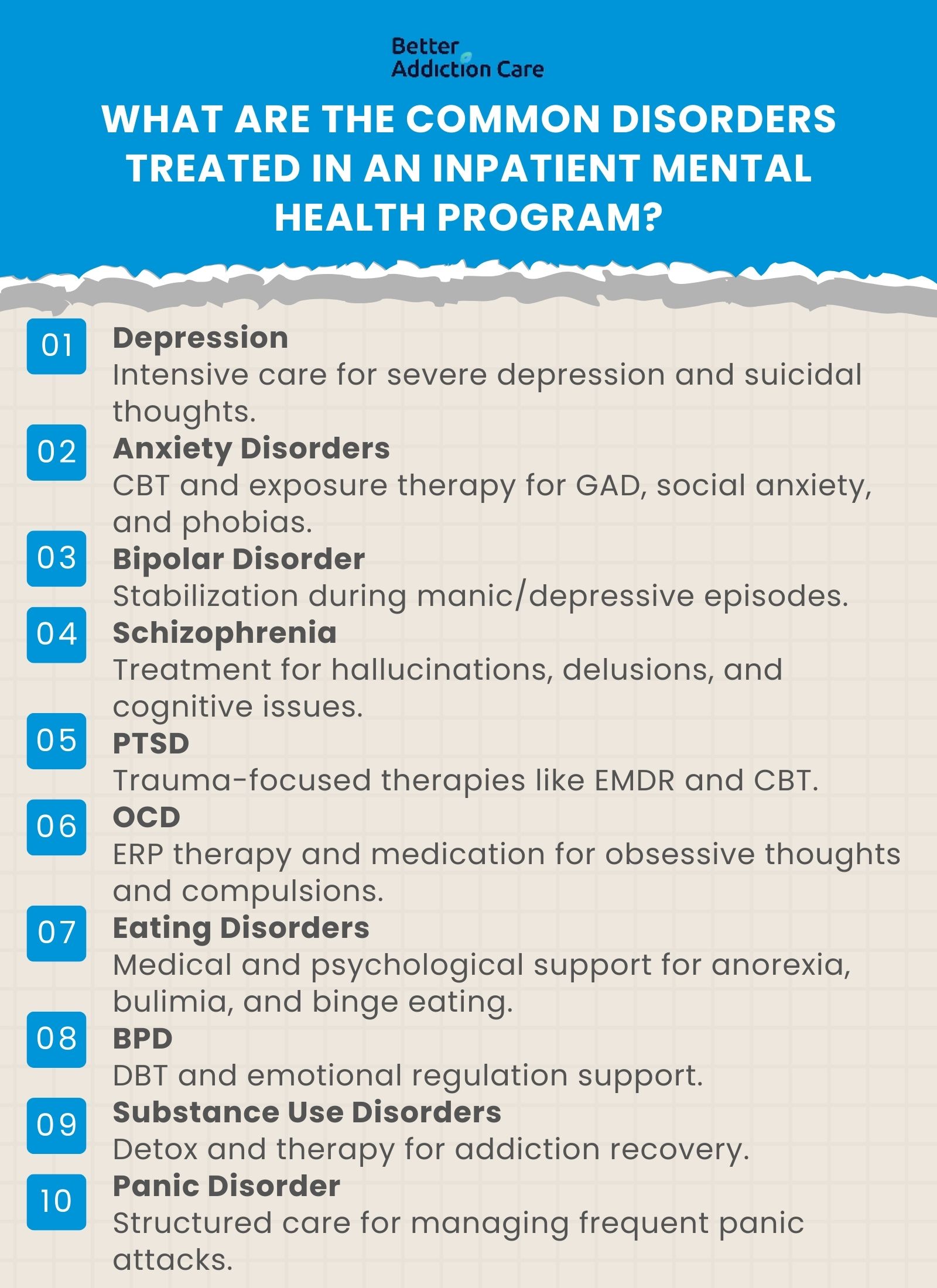
The common disorders treated in an inpatient mental health program are as follows:
-
Depression: Inpatient treatment helps individuals with severe depression who experience suicidal thoughts or an inability to function in daily life. Therapy, medication, and structured support work to improve mood and coping mechanisms. According to the National Institute of Mental Health (NIMH), in 2021, an estimated 21 million American adults experienced at least one major depressive episode, representing 8.3% of the total adult population, with women experiencing a higher prevalence than men.
-
Anxiety Disorders: Generalized anxiety disorder (GAD), social anxiety, and phobias are debilitating. Inpatient programs offer cognitive-behavioral therapy (CBT) and exposure therapy to help patients manage their symptoms effectively. According to the Anxiety and Depression Association of America (ADAAA), Generalized Anxiety Disorder (GAD) affects 6.8 million adults or 3.1% of the US population, yet only 43.2% are receiving treatment.
-
Bipolar Disorder: Patients with extreme mood swings benefit from medication stabilization, structured routines, and therapy to manage manic and depressive episodes. Inpatient care ensures a safe environment during severe episodes. According to the National Institute of Mental Health (NIMH) in the United States, an estimated 2.8% of adults experienced bipolar disorder in the past year, and 4.4% experience it at some point in their lives.
-
Schizophrenia: This condition requires intensive treatment, as it involves hallucinations, delusions, and cognitive impairment. Antipsychotic medications, therapy, and life skills training are key components of inpatient care. According to NAMI, in the U.S., the lifetime prevalence of schizophrenia is estimated to be around 0.3% to 0.7% of the population, with the disorder emerging between the mid-teens and mid-30s.
-
Post-Traumatic Stress Disorder (PTSD): Individuals with PTSD, particularly those with severe trauma, receive specialized therapy such as EMDR and trauma-focused CBT in inpatient settings to help them process and manage distressing memories. According to the National Institute of Mental Health (NIMH) in the U.S., an estimated 3.6% of adults have experienced PTSD in the past year, with a lifetime prevalence of 6.8%. Women are more likely to develop PTSD than men.
-
Obsessive-Compulsive Disorder (OCD): Patients with severe OCD who struggle with intrusive thoughts and compulsive behaviors benefit from inpatient care, which includes Exposure and Response Prevention (ERP) therapy and medication. According to the National Institute of Mental Health (NIMH) in the US, an estimated 1.2% of adults have had obsessive-compulsive disorder (OCD) in the past year, and 2.3% experience it at some point in their lifetime, with women having a slightly higher past-year prevalence than men.
-
Eating Disorders: Anorexia, bulimia, and binge-eating disorder require medical monitoring, nutritional counseling, and psychotherapy in inpatient settings to address both the psychological and physical health aspects of the disorder. According to the National Eating Disorder Association, 9% of the US population, or 28.8 million Americans, will have an eating disorder in their lifetime.
-
Borderline Personality Disorder (BPD): Individuals with BPD experience emotional dysregulation and impulsive behavior. Inpatient treatment provides dialectical behavior therapy (DBT) and emotional stabilization techniques. In the U.S., the lifetime prevalence of Borderline Personality Disorder (BPD) is estimated to be between 0.7% and 2.7% in the general adult population, with higher rates (around 20%) observed in psychiatric inpatients, according to a study by Chapman J, Jamil RT, Fleisher C, et al. 2024, titled “Borderline Personality Disorder.”
-
Substance Use Disorders: Inpatient rehab programs provide detox, medical supervision, and therapy to help patients recover from drug and alcohol addiction, reducing the risk of relapse.
-
Panic Disorder: Those with severe panic disorder, experiencing frequent and debilitating panic attacks, receive structured therapy and medication management to reduce episodes and regain control over daily life.
What are the Treatment Approaches during Inpatient Mental Health Programs?
The treatment approaches during an Inpatient Mental Health Program are Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), Psychodynamic Therapy Program, and Trauma-Focused Therapy Program. These treatment approaches are structured, evidence-based interventions designed to address a wide range of mental health conditions. These therapies are conducted in a controlled setting where patients receive intensive support and monitoring. The goal is to help individuals develop effective coping mechanisms, reduce symptoms, and improve overall well-being.
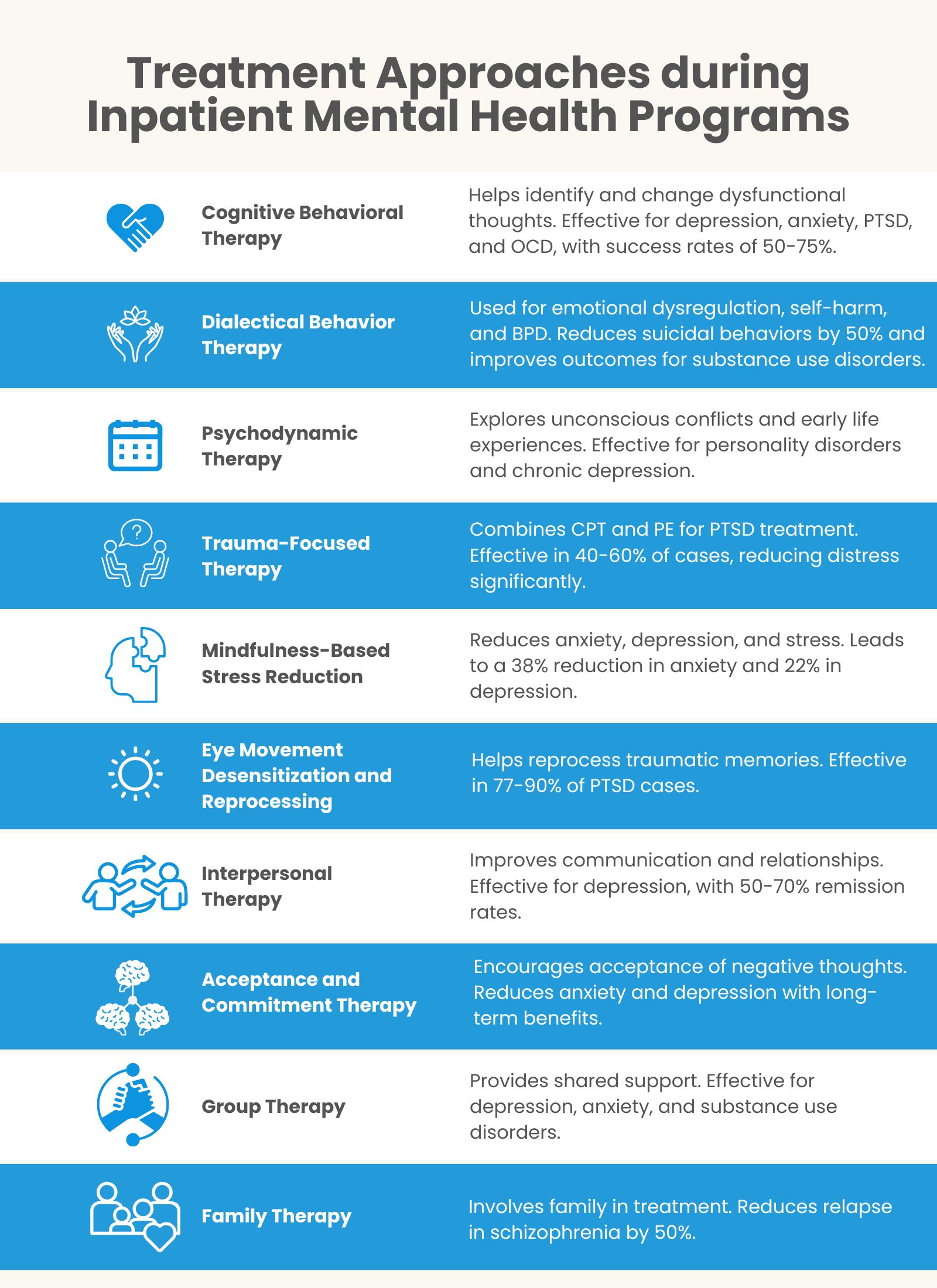
The treatment approaches during an Inpatient Mental Health Program are as follows:
Cognitive Behavioral Therapy (CBT) Program
Cognitive Behavioral Therapy (CBT) is a highly structured, evidence-based psychotherapy that helps patients identify and change dysfunctional thought patterns and behaviors. It operates on the principle that maladaptive thoughts contribute to emotional distress and behavioral issues. Cognitive behavioral therapy is widely used for depression, anxiety, PTSD, and obsessive-compulsive disorder (OCD). According to a meta-analysis by Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, Fang A. et al. 2012, titled “The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses,” of over 269 studies, CBT has a success rate of 50 to 75% in reducing symptoms of depression and anxiety. For OCD treatment, CBT combined with Exposure and Response Prevention (ERP) has shown response rates of 60 to 80%, as studied by Whittal ML et al. 2006, titled “Treatment of obsessive-compulsive disorder: Cognitive behavior therapy vs. exposure and response prevention.”
Dialectical Behavior Therapy (DBT) Program
Dialectical Behavior Therapy (DBT) is a comprehensive treatment originally designed for borderline personality disorder (BPD) but now widely used for emotional dysregulation, self-harm, and suicidal behaviors. DBT incorporates four key modules: mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness. Clinical trials by Linehan MM et al. 2006, titled “Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder,” show that Dilectical Behavior Therapy reduces suicidal behaviors by 50% compared to standard treatment. It has also been effective in treating substance use disorders, with one study by Linehan MM, et al. 2002, titled “Dialectical behavior therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder,” indicating a 64% reduction in drug use among DBT participants.
Psychodynamic Therapy Program
Psychodynamic therapy focuses on exploring unconscious conflicts, early life experiences, and unresolved emotions that influence present behavior. Unlike short-term therapies, it aims to provide long-lasting relief by addressing deep-seated emotional distress. Research by the American Psychological Association, “The Efficacy of Psychodynamic Psychotherapy,” indicates that patients undergoing psychodynamic therapy experience symptom reduction comparable to CBT, with long-term benefits continuing even after treatment ends. This approach is particularly beneficial for personality disorders, chronic depression, and trauma-related conditions.
Trauma-Focused Therapy Program
Trauma-focused therapy is designed for individuals struggling with post-traumatic stress disorder (PTSD) and trauma-related mental health issues. It integrates approaches such as Cognitive Processing Therapy (CPT) and Prolonged Exposure Therapy (PE), which help patients process and reframe traumatic experiences. Clinical trials by the National Center for PTSD indicate that CPT is effective in 40% to 60% of PTSD cases, significantly reducing distress and improving daily functioning.
Mindfulness-Based Stress Reduction (MBSR) Program
Mindfulness-Based Stress Reduction (MBSR) is a meditation-based intervention that enhances emotional regulation and reduces symptoms of anxiety, depression, and chronic stress. It involves mindfulness meditation, body awareness, and yoga techniques. A meta-analysis of 209 studies by Khoury B, Sharma M, Rush SE, Fournier C. et al. 2015, titled “Mindfulness-based stress reduction for healthy individuals: A meta-analysis” found that MBSR leads to a 38% reduction in anxiety symptoms and a 22% decrease in depression severity.
Eye Movement Desensitization and Reprocessing (EMDR) Program
EMDR is a specialized therapy for PTSD that involves guided eye movements to help reprocess traumatic memories. It is based on the Adaptive Information Processing (AIP) model, which posits that trauma is improperly stored in the brain. Research by Shapiro F. et al. 2014, titled “The role of eye movement desensitization and reprocessing (EMDR) therapy in medicine: addressing the psychological and physical symptoms stemming from adverse life experiences,” has found that 77-90% of individuals with single-event PTSD experience significant symptom reduction after three to six EMDR sessions.
Interpersonal Therapy (IPT) Program
Interpersonal Therapy (IPT) is a short-term, structured approach focusing on improving communication and relationships. It is particularly effective for depression, grief, and social anxiety. A study by Srivastava K, et al. 2024, titled “Comparative efficacy of cognitive behavior therapy and interpersonal therapy in the treatment of depression: A randomized controlled study,” shows that IPT is as effective as CBT for major depressive disorder, with remission rates ranging from 50% to 70%.
Acceptance and Commitment Therapy (ACT) Program
ACT is a third-wave behavioral therapy that encourages individuals to accept negative thoughts instead of avoiding them while committing to positive life changes. It is beneficial for chronic pain, depression, anxiety, and OCD. A systematic review by Beygi Z. et al. 2023, titled “An Overview of Reviews on the Effects of Acceptance and Commitment Therapy (ACT) on Depression and Anxiety,” found that ACT improves psychological flexibility and is effective in reducing anxiety and depression symptoms, with long-term benefits.
Group Therapy Program
Group therapy provides a structured environment where individuals share experiences and support each other. It is widely used for substance use disorders, depression, and social anxiety. Research by McDermut W, Miller IW, Brown RA. et al. 2001, titled “The efficacy of group psychotherapy for depression: a meta-analysis and review of the empirical research” suggests that group therapy is as effective as individual therapy for depression and anxiety, with significant symptom reductions in participants.
Family Therapy Program
Family therapy involves educating and involving family members in the treatment process to improve communication and support within the household. It is particularly useful for treating schizophrenia, addiction, and mood disorders. A study by Pharoah F, Mari J, Rathbone J, Wong W. et al. 2010, titled “Family intervention for schizophrenia,” indicates that family therapy reduces relapse rates in schizophrenia by 50% and improves overall treatment adherence.
What is the Process During Inpatient Mental Health Programs?
The process during Inpatient Mental Health Programs involves a structured, multi-phase approach to ensure comprehensive care for individuals facing mental health challenges. This process begins with a thorough assessment, followed by a personalized treatment plan that integrates therapy, medication, and skill-building. Continuous monitoring and support help individuals progress toward stability, while discharge planning and aftercare ensure long-term success.
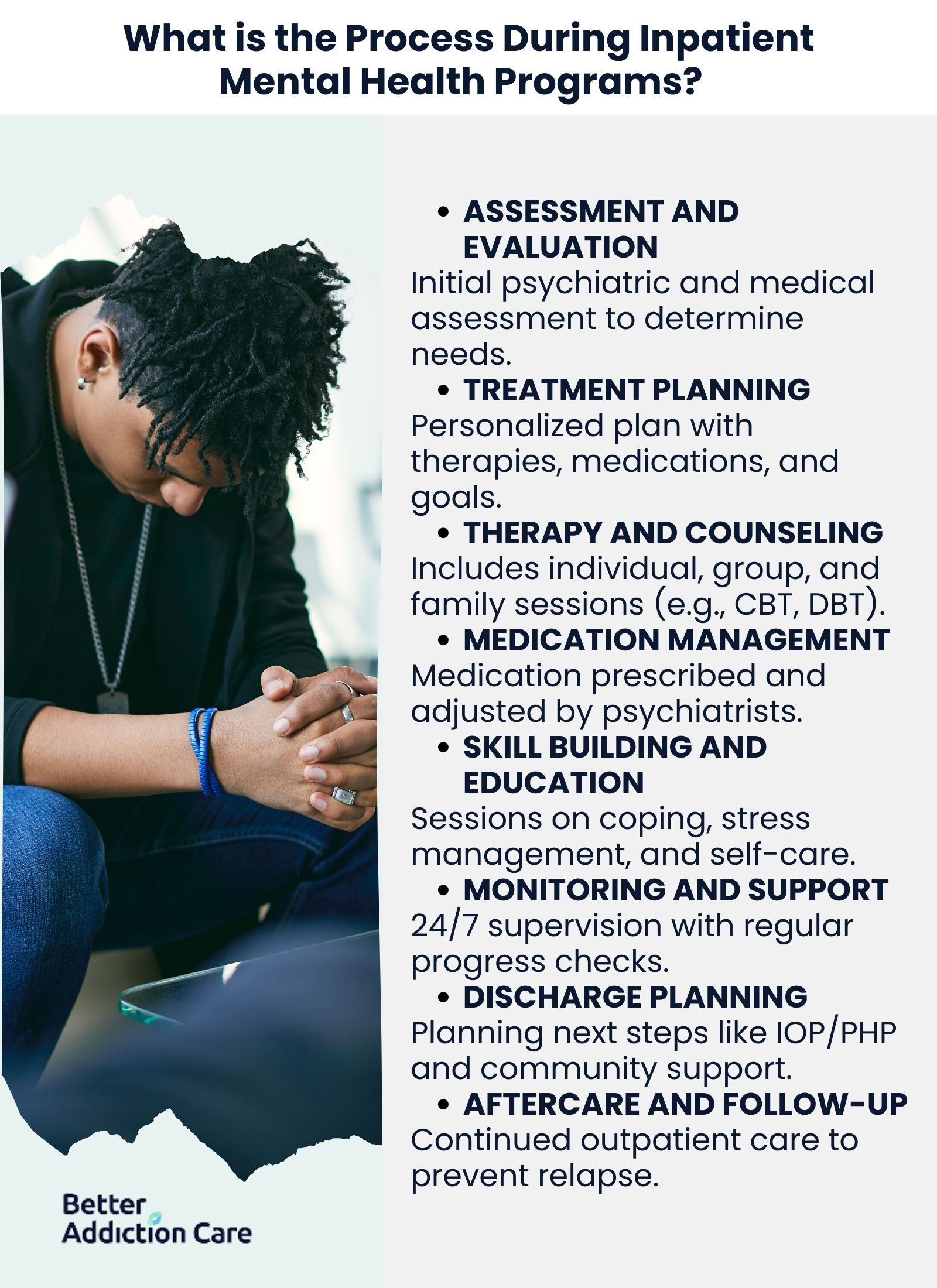
The process during Inpatient Mental Health Programs is detailed as follows:
-
Assessment and Evaluation: Upon admission, patients undergo a comprehensive psychiatric and medical evaluation to assess their mental health status, medical history, substance use, and risk factors. Standardized tools such as the DSM-5 criteria and structured interviews help clinicians determine diagnosis and severity. Research by Rush AJ et al. 2018, titled “Improving Depression Outcome by Patient-Centered Medical Management,” indicates that thorough initial assessments improve treatment outcomes by ensuring that interventions are tailored to the patient’s specific needs.
-
Treatment Planning: After evaluation, a personalized treatment plan is developed based on the individual's diagnosis, symptoms, and therapeutic needs. This plan outlines the specific therapies, medications, and interventions that will be used, ensuring a multidisciplinary approach. A study by Dixon LB, Holoshitz Y, Nossel I. et al. 2016, titled “Treatment engagement of individuals experiencing mental illness: review and update,” shows that customized treatment plans increase engagement and reduce relapse rates.
-
Therapy and Counseling: Patients participate in individual, group, and family therapy sessions to address emotional distress, behavioral patterns, and coping mechanisms. Evidence-based therapies like Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and trauma-focused approaches play a necessary role. Research by Nakao M, Shirotsuki K, Sugaya N. et al. 2021, titled “Cognitive-behavioral therapy for management of mental health and stress-related disorders: Recent advances in techniques and technologies,” indicates that structured therapy during inpatient care significantly reduces symptoms of major mental illnesses.
-
Medication Management: For patients requiring pharmacological intervention, psychiatrists prescribe and monitor medications to stabilize mood, reduce psychotic symptoms, or manage anxiety and depression. Medications such as antidepressants, antipsychotics, and mood stabilizers are frequently used. A study by the National Institute of Mental Health (NIMH) found that 70% of patients with schizophrenia experience symptom improvement with proper medication adherence.
-
Skill Building and Education: Inpatient programs incorporate psychoeducation and skill-building sessions to help patients develop emotional regulation, stress management, and social skills. These sessions focus on coping strategies, relapse prevention, and self-care techniques to support long-term recovery. Skill-building interventions improve self-efficacy and reduce the likelihood of rehospitalization.
-
Monitoring and Support: Patients receive 24/7 supervision and crisis intervention to ensure safety and stability. Regular check-ins with mental health professionals allow for progress tracking and immediate intervention in case of worsening symptoms. A study by Stewart, D., et al. 2009, titled “Manual restraint of adult psychiatric inpatients: A literature review,” shows that continuous support in inpatient settings reduces self-harm incidents and improves treatment adherence.
-
Discharge Planning: As patients approach recovery, clinicians develop a discharge plan that includes step-down care options like Intensive Outpatient Programs (IOP) or Partial Hospitalization Programs (PHP). A well-structured discharge plan ensures patients have continued access to therapy, medication management, and community resources. Research by Tyler N, Wright N, Waring J. et al. 2019, titled “Interventions to improve discharge from acute adult mental health inpatient care to the community: systematic review and narrative synthesis,” shows patients with structured discharge plans have 40% lower readmission rates.
-
Aftercare and Follow-Up: Long-term recovery is supported through outpatient therapy, support groups, and follow-up psychiatric care. Programs like 12-step groups, ongoing counseling, and medication management play a key role in preventing relapse. A study by Donovan DM, Ingalsbe MH, Benbow J, and Daley DC. et al. 2013, titled “12-step interventions and mutual support programs for substance use disorders: an overview,” indicates that patients who engage in aftercare services have a 60% higher chance of maintaining recovery.
Who Needs an Inpatient Mental Health Program?
The people who need an inpatient mental health program include individuals experiencing severe mental health symptoms that significantly impair daily functioning or pose a risk to themselves or others. This level of care provides 24/7 supervision, intensive therapy, and medical support to stabilize mental health conditions and ensure safety. Inpatient treatment is necessary for those who require immediate intervention, have not responded to outpatient care, or need a structured environment for recovery.
The following individuals need an Inpatient Mental Health Program:
-
Individuals Experiencing Severe Depression: Severe depression causes persistent sadness, loss of interest, extreme fatigue, and suicidal thoughts. When symptoms interfere with basic self-care and daily responsibilities, inpatient treatment provides a safe environment, intensive therapy, and medication management to help individuals regain stability. A study by Angst J et al. 1999, titled “Suicide Risk in Patients With Major Depressive Disorder,” shows that hospitalization reduces suicide risk in individuals with major depressive disorder.
-
People with Suicidal Thoughts or Behaviors: Those who experience suicidal ideation, self-harm, or suicide attempts require immediate intervention in a secure setting. Inpatient programs provide constant supervision, crisis management, and therapeutic interventions to prevent self-harm and address underlying mental health conditions. The National Institute of Mental Health (NIMH) reports that nearly 46,000 suicides occur annually in the U.S., emphasizing the need for intensive care.
-
Individuals with Severe Trauma: People suffering from post-traumatic stress disorder (PTSD) or complex trauma experience flashbacks, dissociation, emotional numbness, and extreme distress. Inpatient programs provide trauma-focused therapy, coping strategies, and a controlled environment to help individuals process their experiences safely. Research by Bradley R et al. 2005, titled “A Multidimensional Meta-Analysis of Psychotherapy for PTSD,” indicates that structured inpatient care improves PTSD symptoms in 60% to 80% of patients.
-
People with Psychotic Disorders: Conditions like schizophrenia, schizoaffective disorder, and severe bipolar disorder with psychotic features require hospitalization. Individuals experiencing hallucinations, delusions, or extreme paranoia benefit from round-the-clock monitoring, medication stabilization, and therapy in an inpatient setting. A systematic review by Marshall M et al., 2005, titled “Association Between Duration of Untreated Psychosis and Outcome in Cohorts of First-Episode Patients,” shows that early intervention in inpatient care improves long-term outcomes in psychotic disorders.
-
Individuals with Substance Use Disorders and Co-occurring Mental Health Issues: People with co-occurring substance use and mental health disorders (dual diagnosis) require inpatient care to detox safely, receive psychiatric treatment, and develop relapse prevention strategies. A study by the Substance Abuse and Mental Health Services Administration (SAMHSA) found that 45% of individuals with a substance use disorder also have a co-occurring mental health condition.
-
People Experiencing a Mental Health Crisis: A mental health crisis involves extreme agitation, violent outbursts, dissociation, or self-destructive behavior. Inpatient care ensures immediate stabilization through medication, structured therapy, and crisis intervention strategies. Crisis intervention services in inpatient settings have been shown by Wang D, Gupta V. et al. 2023, titled “Crisis Intervention” to reduce emergency room visits and prevent long-term psychiatric decline.
-
Individuals Who Have Not Responded to Outpatient Treatment: Some individuals do not achieve symptom relief with outpatient therapy, medication, or community-based interventions. Inpatient programs provide more intensive treatment, medication adjustments, and a controlled environment to help patients who need a higher level of care. A study by Voineskos D, Daskalakis ZJ, Blumberger DM. et al. 2020, titled “Management of Treatment-Resistant Depression: Challenges and Strategies,” indicates that treatment-resistant depression improves significantly with inpatient interventions.
-
Those Who Require 24/7 Supervision and Support: Individuals who cannot function independently or are at risk of harming themselves or others require continuous monitoring. Inpatient care provides structured support, crisis management, and a therapeutic environment to ensure safety and progress toward recovery. Research by Zambrowicz R. et al. 2019, titled “Inpatient Psychiatric Care Outcomes for Adolescents: A Test of Clinical and Psychosocial Moderators,” highlights that patients with severe psychiatric conditions experience better outcomes with inpatient stabilization.
-
People with Severe Mood Disorders: Conditions like bipolar disorder, major depressive disorder, and severe anxiety disorders lead to unpredictable mood swings, impulsive behaviors, and episodes of mania or deep depression. Inpatient treatment provides medication regulation, behavioral therapy, and coping strategies to help stabilize mood disorders. A study by Gignac A. et al. 2015, titled “Course and outcome following a first episode of mania: Four-year prospective data from the Systematic Treatment Optimization Program (STOP-EM),” shows that hospitalization reduces the severity of mood disorder symptoms and improves long-term management.
What Is the Cost of an Inpatient Mental Health Program?
The cost of an inpatient mental health program in the United States ranges from $5,000 to $60,000 or more for a 30-day stay. Several factors influence these costs, including the type of facility, location, duration of treatment, and level of care provided. Luxury treatment centers with upscale accommodations and specialized services are more expensive than standard facilities. Programs in urban areas or high-cost regions generally charge more than those in rural locations.
The scope of treatment also plays an integral role in determining cost. Programs offering intensive therapy, medication management, and round-the-clock medical supervision incur higher fees. Insurance coverage helps offset expenses, but out-of-pocket costs depend on the specific policy and provider network. Without adequate financial resources, many individuals face challenges in accessing necessary inpatient mental health care, which leads to untreated conditions and worsening symptoms. It is important to explore different payment options, including insurance benefits, sliding-scale fees, and financial assistance programs, to ensure affordability and accessibility.
Does Insurance Cover Inpatient Mental Health Programs?
Yes, insurance does cover inpatient mental health programs, but the extent of coverage depends on the specific insurance plan. Under the Affordable Care Act (ACA) and the Mental Health Parity and Addiction Equity Act (MHPAEA), insurance providers must cover mental health treatment at the same level as physical health care. Most private insurance plans, Medicaid, and Medicare provide some level of coverage for inpatient mental health services, including hospitalization, therapy, and medication management.
Coverage varies based on factors such as plan type, provider network, length of stay, and medical necessity requirements. Some policies require pre-authorization or impose limits on the number of covered days. Patients should check with their insurance provider to understand their benefits, co-pays, deductibles, and any out-of-pocket costs associated with inpatient mental health treatment.
How to Find Inpatient Mental Health Treatment Programs and Rehabs Near Me?
To find Inpatient Mental Health Treatment Programs near you, individuals explore online directories, contact mental health hotlines, or consult local hospitals and clinics. Seeking professional guidance from a primary care physician or therapist also helps identify the most suitable treatment programs based on specific needs.
Reliable resources include the Substance Abuse and Mental Health Services Administration (SAMHSA) treatment locator, National Alliance on Mental Illness (NAMI) helpline, and MentalHealth.gov, which offer nationwide directories of accredited inpatient facilities. Many hospitals have dedicated psychiatric units, and nonprofit organizations provide referrals to inpatient programs and rehabs specializing in various mental health conditions.
How Long Do Inpatient Mental Health Programs Last?
Inpatient Mental Health Programs last anywhere from a few days to several months, with the typical stay ranging between 30 to 90 days depending on the severity of the condition and individual treatment needs. Short-term stays (a few days to a couple of weeks) are focused on crisis stabilization, while long-term programs (several months) provide intensive treatment for chronic or severe mental health conditions.
Several factors influence the duration of inpatient treatment, including the type and severity of the mental health disorder, the individual's response to therapy and medication, insurance coverage, and the facility's treatment approach. Patients requiring detoxification, medication adjustments, or extensive behavioral therapy need longer stays, while those with strong outpatient support systems transition to lower levels of care sooner.
What Is the Difference Between Inpatient Treatment and Outpatient Treatment?
The main difference between inpatient treatment and outpatient treatment is that inpatient treatment requires individuals to stay at a facility for 24/7 care, while outpatient treatment allows individuals to live at home and attend scheduled therapy sessions. Inpatient treatment provides a structured environment with constant supervision, making it ideal for those with severe mental health or substance use disorders who need intensive care and medical support.
In contrast, outpatient treatment offers flexibility, allowing individuals to continue their daily responsibilities, such as work or school, while receiving treatment. Outpatient programs vary in intensity, from standard therapy sessions to more comprehensive options like Partial Hospitalization Programs (PHPs) and Intensive Outpatient Programs (IOPs). The choice between inpatient vs outpatient treatment depends on factors such as the severity of the condition, level of support at home, and medical necessity.
What Happens After Completing an Inpatient Mental Health Program?
After completing an inpatient mental health program, individuals transition to aftercare services to maintain stability and prevent relapse. This includes outpatient therapy, medication management, support groups, and follow-up care with mental health professionals. Some step down to Partial Hospitalization Programs (PHPs) or Intensive Outpatient Programs (IOPs) for continued support while gradually reintegrating into daily life. A well-structured discharge plan helps ensure that individuals stay connected with necessary resources, including therapy, case management, and community support networks, reducing the risk of setbacks.
Are Inpatient Mental Health Programs Confidential?
Yes, inpatient mental health programs are confidential. Federal laws such as the Health Insurance Portability and Accountability Act (HIPAA) protect patients' privacy, ensuring their medical records and treatment details remain private. Mental health facilities have strict confidentiality policies, and information is only disclosed with the patient’s written consent or in cases of legal or medical necessity, such as harm to self or others. This confidentiality helps individuals feel secure in seeking treatment without fear of stigma or repercussions.
How Are Medications Managed in Inpatient Mental Health Programs?
Medications are managed in inpatient mental health programs through a structured and supervised regimen to ensure adherence, effectiveness, and safety. Psychiatrists, nurses, and medical staff regularly assess patients to monitor medication responses, adjust dosages, and address side effects. Medications such as antidepressants, mood stabilizers, antipsychotics, or anti-anxiety drugs are prescribed based on individual needs. Patients also receive education on medication use, potential interactions, and long-term management strategies to support continued stability after discharge.
Can I Continue My Work or School While in an Inpatient Mental Health Program?
No, you cannot continue your work or school while in an inpatient mental health program because these programs require full-time residential care and focus entirely on treatment and recovery. Inpatient stays range from a few weeks to several months, depending on the severity of the condition. While patients participate in therapeutic activities and structured daily routines, they are not usually permitted to engage in external responsibilities like work or school. However, after discharge, they transition to outpatient care while resuming their regular activities.
Is an Inpatient Mental Health Program the Same as Inpatient Psychiatric Care?
No, an inpatient mental health program and inpatient psychiatric care are not exactly the same, though they share similarities. Inpatient psychiatric care is a more intensive form of treatment used for individuals experiencing severe mental health crises, suicidal thoughts, or psychosis requiring immediate stabilization in a hospital setting. In contrast, inpatient mental health programs are more structured for long-term recovery and rehabilitation, focusing on therapy, medication management, and skill-building. While both provide 24/7 care, inpatient psychiatric care is shorter-term and crisis-focused, whereas mental health programs involve extended treatment for ongoing conditions.