How to Get Insurance to Pay for Inpatient Drug Rehab
Inpatient rehab is an important step toward recovery, and insurance helps cover much of the cost. Many health plans include benefits for substance use treatment, including detox and residential care. If you're unsure about your coverage, it's best to contact your provider, who helps you review your policy and understand your options, so you take the next step with confidence.

According to the U.S. Department of Health and Human Services, in 2021, 91% of Americans with health insurance had coverage for substance use disorder treatment services. This is based on data from the National Survey on Drug Use and Health (NSDUH).
According to the U.S. Department of Health and Human Services, in 2021, 91% of Americans with health insurance had coverage for substance use disorder treatment services. This is based on data from the National Survey on Drug Use and Health (NSDUH).
What are the Steps to Get Inpatient Rehab Covered by Insurance?

To get inpatient rehab covered by insurance, follow these steps:
-
Verify Your Insurance Benefits: Contact your health insurance provider or use an online verification tool to find out what levels of rehab are covered, including detox, inpatient, and outpatient treatment.
-
Get a Clinical Assessment: Many insurance plans require a professional evaluation to determine medical necessity. This assessment helps justify the need for inpatient care.
-
Choose an In-Network Rehab Facility: Selecting a facility that is in-network with your insurance provider reduces out-of-pocket costs and simplifies the approval process.
-
Obtain Preauthorization if Required: Some insurers require preapproval before treatment begins. The rehab center assists you with this step.
-
Work with the Admissions Team: Most treatment centers have staff who help coordinate with your insurer to ensure coverage and streamline the intake process.
-
Keep Records: Maintain all documentation related to your insurance coverage and rehab stay, including approvals, assessments, and communication with your provider.
Does Health Insurance Pay for Drug Rehab?
Yes, health insurance does pay for drug rehab, either partially or in full. Under laws like the Affordable Care Act and the Mental Health Parity and Addiction Equity Act, insurance providers are required to offer some level of coverage for substance use treatment. However, coverage varies widely depending on the type of insurance you have. Private insurance plans, whether purchased individually or through an employer, include inpatient and outpatient rehab benefits.
The average cost of a 30-day inpatient rehab stay in the U.S. is about $18,000–$20,000. With insurance, patients pay only their deductible and copay, which is as low as 10–20% of the total cost, depending on the plan.
What Treatments Are Covered In Inpatient Drug Rehab?
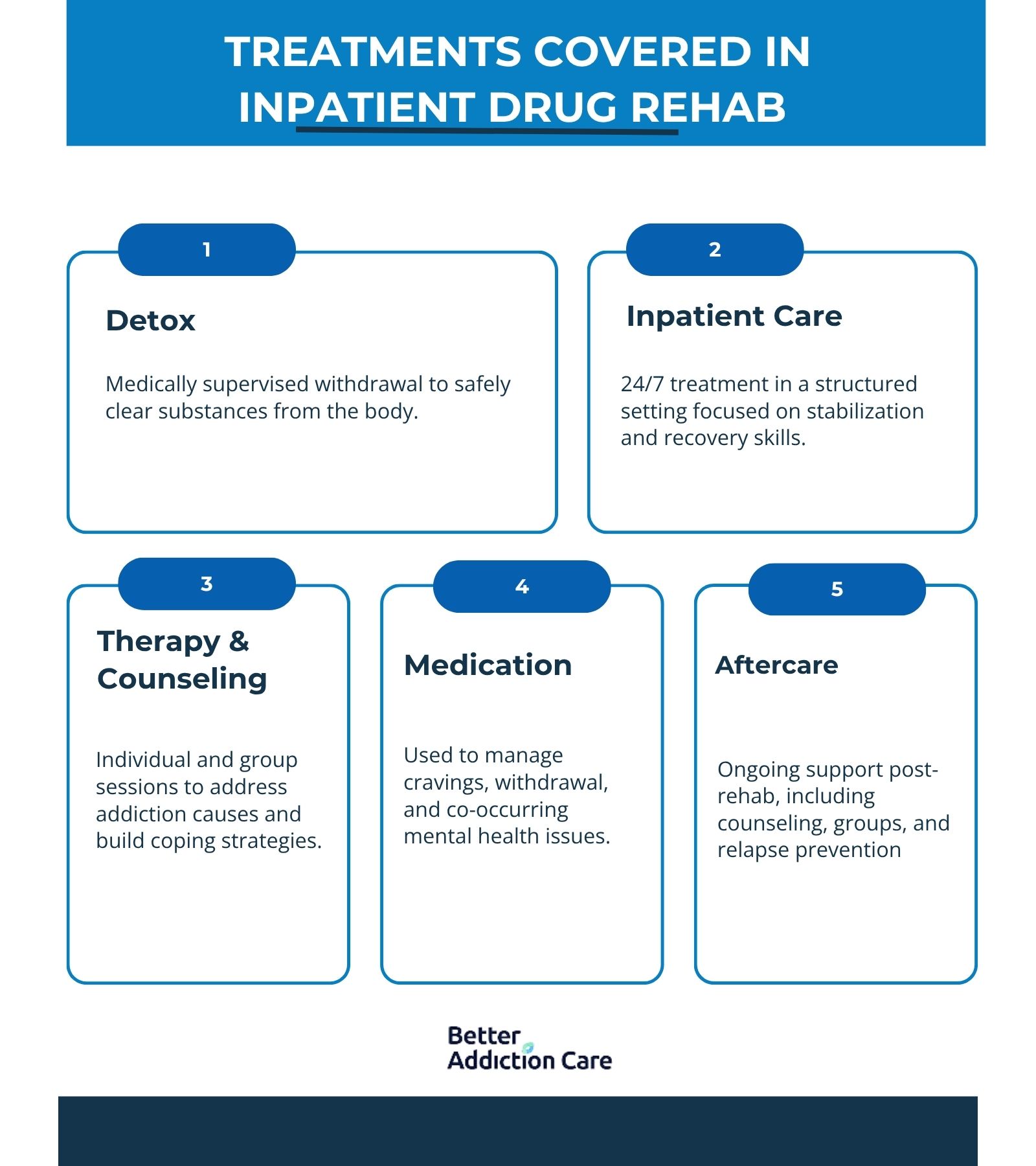
The treatments covered in inpatient drug rehab include detox, inpatient treatment, therapy and counseling, medication management, and aftercare with ongoing support. These services work together to provide a comprehensive approach to recovery, addressing both the physical and emotional aspects of addiction. With the right coverage, you focus on healing while your insurance helps manage the cost of drug rehab.
Here are the treatments covered in inpatient drug rehab:
Detox:
Detox is the first step where the body clears itself of addictive substances under medical supervision. This process helps manage withdrawal symptoms safely and prepares you for the next phase of treatment.
Inpatient Program:
Inpatient treatment provides 24/7 care in a structured, supportive environment. It focuses on stabilizing your condition, developing healthy habits, and building a strong foundation for long-term recovery.
Therapy and Counseling:
Individual and group therapy sessions help address the underlying causes of addiction, teach coping skills, and support emotional healing. Counseling also strengthens motivation and fosters accountability.
Medication:
Medications are prescribed to reduce cravings, ease withdrawal symptoms, or treat co-occurring mental health disorders. Medication Assisted Treatment is the key to helping improve treatment outcomes.
Aftercare and Ongoing Support:
Aftercare programs and ongoing support services provide continued guidance once inpatient treatment ends. This helps prevent relapse and encourages lasting sobriety through counseling, support groups, and follow-up care.
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), in 2011, approximately 59.6% of substance abuse treatment admissions aged 26 or older reported having no health insurance. Among those with insurance, 21.3% had Medicaid coverage, and 10.5% had private insurance.
How Can I Verify My Insurance Benefits?
You can verify your insurance benefits in many different ways, including contacting the rehab center yourself, contacting your insurance provider, or reaching out through online resources like Better Addiction Care. BAC helps connect you with different treatment centers in your area and has a form that you fill out to verify your benefits and see what treatment centers take your insurance.
What If Your Insurance Claim For Rehab Is Denied?
If your insurance claim for rehab is denied, don’t panic; you have the right to appeal. Denials are overturned by carefully following your insurer’s appeal process. Start by reviewing the denial letter to understand the reason, then gather supporting medical records or letters from your doctor to strengthen your case. Be sure to submit everything within the required timeframe. If needed, consider working with the rehab center’s billing team or a healthcare advocate to guide you through the appeal process and improve your chances of approval.
How Many Times Will Insurance Pay for Rehab?
The number of times insurance will pay for rehab depends on your specific policy limits and whether each treatment is considered medically necessary. Some plans cover multiple stays per year, while others have strict caps or require a certain amount of time between treatments. Pre-approval is especially important for repeat stays to avoid unexpected denials. If coverage is denied for a second or third stay, you still have the right to appeal with updated documentation showing the continued need for treatment.
What are Financial Alternatives if Insurance Does Not Cover the Cost of Inpatient Drug Rehab?

If your insurance doesn’t cover the full cost of inpatient rehab, there are other financial options to help manage expenses. Many rehab centers offer flexible payment plans, and loans or government programs also provide support.
-
Payment plans with monthly installments through rehab centers.
-
Medical or personal loans for upfront treatment costs.
-
State and federal assistance programs for addiction treatment.
Do I have to pay anything out-of-pocket?
Yes, you have to pay some out-of-pocket costs such as copays, deductibles, or fees for services not fully covered by your insurance. The exact amount depends on your specific plan and the rehab facility you choose.
Can I go to rehab without insurance?
Yes, you can go to rehab without insurance. Many treatment centers offer sliding scale fees, payment plans, or financial assistance programs to help make care affordable even if you don’t have insurance coverage.
What are the Steps to Get Inpatient Rehab Covered by Insurance?

To get inpatient rehab covered by insurance, follow these steps:
-
Verify Your Insurance Benefits: Contact your health insurance provider or use an online verification tool to find out what levels of rehab are covered, including detox, inpatient, and outpatient treatment.
-
Get a Clinical Assessment: Many insurance plans require a professional evaluation to determine medical necessity. This assessment helps justify the need for inpatient care.
-
Choose an In-Network Rehab Facility: Selecting a facility that is in-network with your insurance provider reduces out-of-pocket costs and simplifies the approval process.
-
Obtain Preauthorization if Required: Some insurers require preapproval before treatment begins. The rehab center assists you with this step.
-
Work with the Admissions Team: Most treatment centers have staff who help coordinate with your insurer to ensure coverage and streamline the intake process.
-
Keep Records: Maintain all documentation related to your insurance coverage and rehab stay, including approvals, assessments, and communication with your provider.
Does Health Insurance Pay for Drug Rehab?
Yes, health insurance does pay for drug rehab, either partially or in full. Under laws like the Affordable Care Act and the Mental Health Parity and Addiction Equity Act, insurance providers are required to offer some level of coverage for substance use treatment. However, coverage varies widely depending on the type of insurance you have. Private insurance plans, whether purchased individually or through an employer, include inpatient and outpatient rehab benefits.
The average cost of a 30-day inpatient rehab stay in the U.S. is about $18,000–$20,000. With insurance, patients pay only their deductible and copay, which is as low as 10–20% of the total cost, depending on the plan.
What Treatments Are Covered In Inpatient Drug Rehab?
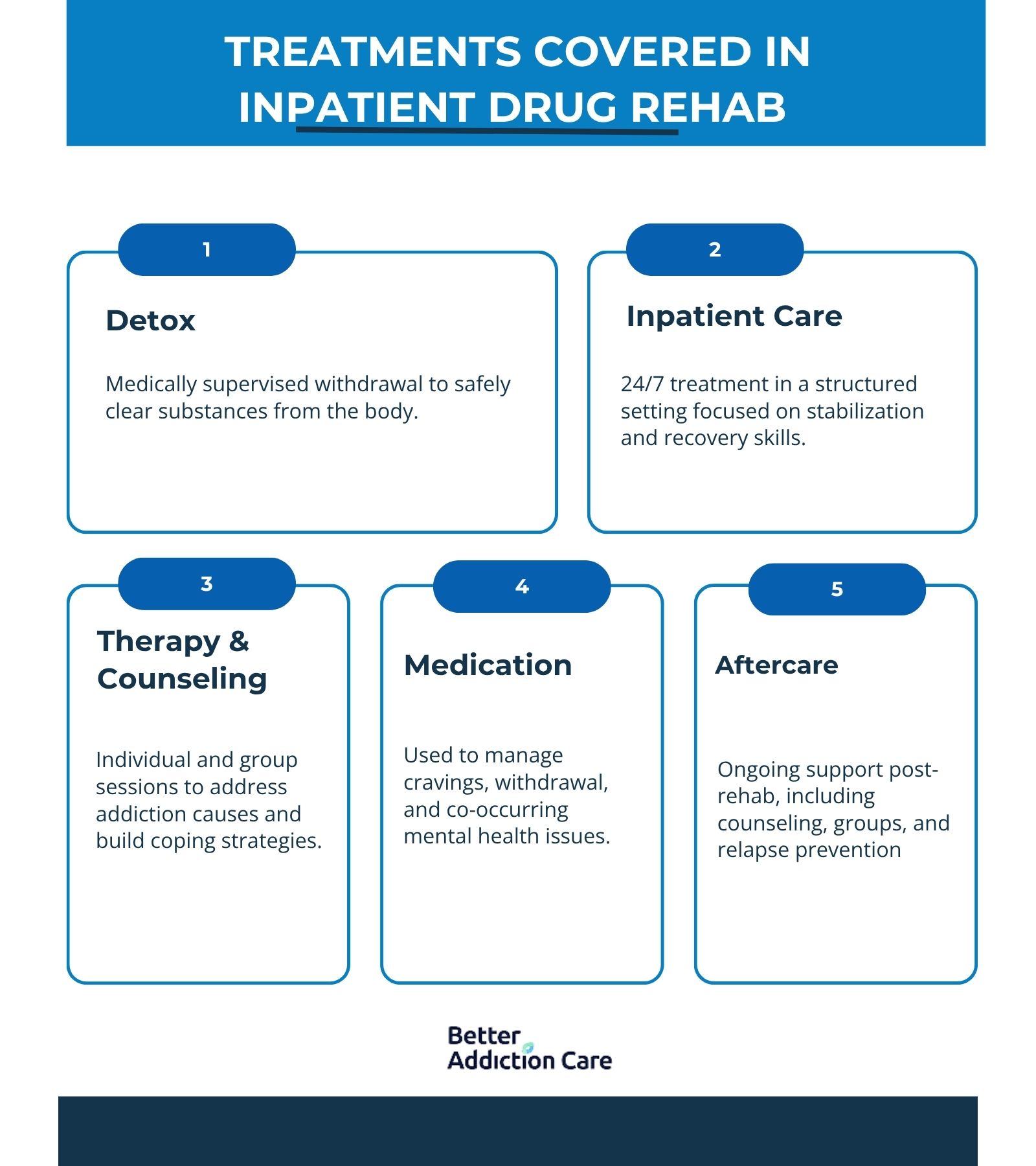
The treatments covered in inpatient drug rehab include detox, inpatient treatment, therapy and counseling, medication management, and aftercare with ongoing support. These services work together to provide a comprehensive approach to recovery, addressing both the physical and emotional aspects of addiction. With the right coverage, you focus on healing while your insurance helps manage the cost of drug rehab.
Here are the treatments covered in inpatient drug rehab:
Detox:
Detox is the first step where the body clears itself of addictive substances under medical supervision. This process helps manage withdrawal symptoms safely and prepares you for the next phase of treatment.
Inpatient Program:
Inpatient treatment provides 24/7 care in a structured, supportive environment. It focuses on stabilizing your condition, developing healthy habits, and building a strong foundation for long-term recovery.
Therapy and Counseling:
Individual and group therapy sessions help address the underlying causes of addiction, teach coping skills, and support emotional healing. Counseling also strengthens motivation and fosters accountability.
Medication:
Medications are prescribed to reduce cravings, ease withdrawal symptoms, or treat co-occurring mental health disorders. Medication Assisted Treatment is the key to helping improve treatment outcomes.
Aftercare and Ongoing Support:
Aftercare programs and ongoing support services provide continued guidance once inpatient treatment ends. This helps prevent relapse and encourages lasting sobriety through counseling, support groups, and follow-up care.
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), in 2011, approximately 59.6% of substance abuse treatment admissions aged 26 or older reported having no health insurance. Among those with insurance, 21.3% had Medicaid coverage, and 10.5% had private insurance.
How Can I Verify My Insurance Benefits?
You can verify your insurance benefits in many different ways, including contacting the rehab center yourself, contacting your insurance provider, or reaching out through online resources like Better Addiction Care. BAC helps connect you with different treatment centers in your area and has a form that you fill out to verify your benefits and see what treatment centers take your insurance.
What If Your Insurance Claim For Rehab Is Denied?
If your insurance claim for rehab is denied, don’t panic; you have the right to appeal. Denials are overturned by carefully following your insurer’s appeal process. Start by reviewing the denial letter to understand the reason, then gather supporting medical records or letters from your doctor to strengthen your case. Be sure to submit everything within the required timeframe. If needed, consider working with the rehab center’s billing team or a healthcare advocate to guide you through the appeal process and improve your chances of approval.
How Many Times Will Insurance Pay for Rehab?
The number of times insurance will pay for rehab depends on your specific policy limits and whether each treatment is considered medically necessary. Some plans cover multiple stays per year, while others have strict caps or require a certain amount of time between treatments. Pre-approval is especially important for repeat stays to avoid unexpected denials. If coverage is denied for a second or third stay, you still have the right to appeal with updated documentation showing the continued need for treatment.
What are Financial Alternatives if Insurance Does Not Cover the Cost of Inpatient Drug Rehab?

If your insurance doesn’t cover the full cost of inpatient rehab, there are other financial options to help manage expenses. Many rehab centers offer flexible payment plans, and loans or government programs also provide support.
-
Payment plans with monthly installments through rehab centers.
-
Medical or personal loans for upfront treatment costs.
-
State and federal assistance programs for addiction treatment.
Do I have to pay anything out-of-pocket?
Yes, you have to pay some out-of-pocket costs such as copays, deductibles, or fees for services not fully covered by your insurance. The exact amount depends on your specific plan and the rehab facility you choose.
Can I go to rehab without insurance?
Yes, you can go to rehab without insurance. Many treatment centers offer sliding scale fees, payment plans, or financial assistance programs to help make care affordable even if you don’t have insurance coverage.





