Medication-Assisted Therapy (MAT): Definition, Applications, Components, Medications, Risks
Medication-assisted treatment (MAT) combines FDA-approved medications with behavioral therapies to address both the physical and psychological aspects of addiction. The goal of MAT is relapse prevention, withdrawal management, and sustained recovery, providing a whole-patient approach that supports individuals through detoxification, cravings, and long-term sobriety.

Medication-assisted treatment (MAT) combines FDA-approved medications with behavioral therapies to address both the physical and psychological aspects of addiction. The goal of MAT is relapse prevention, withdrawal management, and sustained recovery, providing a whole-patient approach that supports individuals through detoxification, cravings, and long-term sobriety.
According to the National Institute on Drug Abuse (NIDA, 2023), MAT significantly improves treatment retention rates and reduces the risk of overdose by stabilizing brain chemistry and providing therapeutic support.
MAT is used in addiction treatment programs by offering medication management in conjunction with therapeutic interventions like cognitive-behavioral therapy (CBT) and group therapy to address the root causes of addiction.
According to the Substance Abuse and Mental Health Services Administration (SAMHSA) in 2022, MAT is a highly effective treatment strategy for opioid and alcohol use disorders, significantly improving patient engagement and long-term recovery success.
The components of MAT include FDA-approved medications, behavioral therapies, and medical supervision, providing a holistic approach to managing addiction. According to the National Institute on Drug Abuse (NIDA, 2023), MAT patients are up to 70% more likely to stay in treatment and maintain long-term sobriety.
Medications used in MAT include methadone, buprenorphine, naltrexone, acamprosate, and disulfiram, which help stabilize brain chemistry, reduce cravings, and manage withdrawal symptoms. The National Institute on Drug Abuse (NIDA, 2023) reports that MAT medications significantly lower relapse rates and prevent opioid overdose deaths.
The risks of MAT include dependency on medications, potential side effects such as nausea or dizziness, and the misuse or diversion of medications like methadone and buprenorphine if not monitored properly. MAT requires careful medical supervision to reduce the risk of complications, including overdose and withdrawal symptoms if medication is stopped abruptly.
What Is Medication-Assisted Treatment (MAT)?
Medication-assisted treatment (MAT) is a comprehensive approach to addiction treatment that combines FDA-approved medications with behavioral therapies and counseling to support individuals struggling with opioid use disorder (OUD), alcohol use disorder (AUD), and other substance dependencies.
The primary goal of MAT is to reduce cravings, alleviate withdrawal symptoms, and improve long-term recovery outcomes by addressing both the physical and psychological aspects of addiction.
According to a study by the Substance Abuse and Mental Health Services Administration (SAMHSA) titled "Medication-Assisted Treatment for Opioid Use Disorder," published in 2021, over 1.6 million Americans received MAT for opioid use disorder in that year alone, demonstrating its widespread application.
Additionally, research from the National Institute on Drug Abuse (NIDA) in 2023 found that MAT reduces the risk of opioid overdose deaths by up to 50% and improves treatment retention rates by 70%.
MAT is not a one-size-fits-all solution; instead, it is customized based on the patient’s substance use history, medical condition, and psychological needs. The therapy component of MAT helps individuals identify triggers, develop coping mechanisms, and work toward sustainable recovery. By addressing both the biological and behavioral factors of addiction, MAT has become a key strategy in modern addiction treatment programs across inpatient and outpatient settings.
How Does Medication-Assisted Treatment Work in Addiction Treatment?
Medication-assisted treatment (MAT) works by targeting brain receptors affected by substance use while integrating behavioral therapy to address the psychological aspects of addiction.
The medications used in MAT help to stabilize brain chemistry, reduce withdrawal symptoms, and manage cravings, making it easier for individuals to engage in counseling and long-term recovery.
Substances such as opioids and alcohol alter the brain’s reward system by binding to specific receptors, leading to dependency. When a person stops using these substances, they experience withdrawal, which includes severe discomfort, anxiety, and cravings.
According to a study by the National Institute on Drug Abuse (NIDA) titled "The Science of Medication-Assisted Treatment," published in 2022, MAT medications act on the same brain receptors as addictive substances but in a controlled manner, preventing withdrawal without producing a high.
Different medications play unique roles in craving management and relapse prevention. For instance, buprenorphine and methadone are partial and full opioid agonists, which help stabilize opioid-dependent individuals by occupying opioid receptors without causing euphoria.
Naltrexone, an opioid antagonist, works by blocking opioid receptors, preventing the effects of opioids altogether. In alcohol use disorder (AUD), acamprosate restores the neurochemical balance disrupted by chronic alcohol consumption, reducing post-withdrawal cravings.
Beyond medication, therapy is a critical component of MAT, ensuring individuals develop coping mechanisms, behavioral changes, and emotional resilience. Cognitive-behavioral therapy (CBT), motivational interviewing (MI), and group counseling are commonly integrated into MAT programs to address the underlying triggers of addiction
According to research published in the Journal of Addiction Medicine (2021), patients receiving MAT combined with therapy have a 60% greater chance of maintaining long-term sobriety compared to those who rely on medication alone.
How Is MAT Applied in Addiction Treatment Programs?
Medication-assisted treatment (MAT) is applied in addiction programs through a structured, step-by-step approach that ensures patients receive both medical and psychological support.
While medication helps stabilize brain function and control withdrawal symptoms, therapy addresses behavioral and emotional triggers, making MAT an essential component of comprehensive addiction treatment.

Ways MAT is applied in addiction treatment programs include:
Step 1: Comprehensive Assessment and Diagnosis: Before starting MAT, patients undergo a medical and psychological evaluation to determine their substance use history, mental health status, and overall physical condition. According to the Substance Abuse and Mental Health Services Administration (SAMHSA) in 2022, structured assessments help clinicians tailor MAT to the individual's needs, ensuring that the right medication and dosage are prescribed.
Step 2: Medication Selection and Stabilization: Once evaluated, a healthcare provider prescribes an FDA-approved medication based on the type of addiction, including:
-
Opioid Use Disorder (OUD): Methadone, Buprenorphine, or Naltrexone.
-
Alcohol Use Disorder (AUD): Acamprosate, Disulfiram, or Naltrexone.
During stabilization, patients receive closely monitored dosages to ensure the medication effectively reduces withdrawal symptoms and craving management without unwanted side effects. According to the National Institute on Drug Abuse (NIDA, 2023), patients stabilized on MAT experience up to 50% fewer withdrawal symptoms than those undergoing non-medicated detox.
Step 3: Behavioral Therapy Integration: MAT is not a stand-alone treatment—it is most effective when combined with evidence-based therapies, including:
-
Cognitive-behavioral therapy (CBT) to help patients identify and manage triggers
-
Motivational Interviewing (MI) to strengthen commitment to recovery
-
Group and Family Therapy to build a support system and improve coping strategies
A study published by the National Institute on Drug Abuse (2021) found that patients who receive MAT alongside therapy have a 70% higher treatment retention rate compared to those relying on medication alone.
Step 4: Long-Term Maintenance and Monitoring: Recovery is an ongoing process. Patients on MAT continue with regular medical check-ups and adjustments to their treatment plan as needed. Many transition to outpatient programs where they receive continued medication while engaging in counseling, employment support, and lifestyle changes to maintain sobriety.
How Does MAT Combine With Behavioral Therapies?
MAT combines with behavioral therapies through Cognitive-Behavioral Therapy (CBT), Motivational Interviewing (MI), and Group Counseling to provide a comprehensive approach to addiction recovery.
CBT helps individuals identify triggers and develop coping strategies, while MI strengthens motivation for change. Group therapy fosters peer support and accountability, improving long-term recovery outcomes.
According to the National Institute on Drug Abuse (NIDA, 2023), combining MAT with therapy increases treatment retention rates by up to 70% and reduces relapse risk by 50%. This dual approach addresses both the biological and psychological aspects of addiction, ensuring sustainable recovery.
Is it Possible For MAT to Be a Stand-Alone Treatment?
No, MAT is most effective when combined with behavioral therapies, but it still provides benefits as a standalone treatment. While MAT reduces withdrawal symptoms, stabilizes brain receptors, and helps with craving management, it does not address the behavioral and psychological factors that contribute to addiction.
According to a study by the National Institute on Drug Abuse (NIDA) published in 2022, patients who receive MAT without therapy have a 40% lower long-term recovery rate compared to those who combine MAT with counseling.
However, in cases where therapy is inaccessible, MAT alone has been shown to reduce opioid overdose deaths by up to 50% and improve treatment retention according to the National Institute on Drug Abuse. This suggests that while standalone MAT helps prevent relapse and stabilize individuals, it does not provide the comprehensive support needed for sustained recovery.
What are the Components of Medication-Assisted Therapy?
The components of Medication-Assisted Therapy are FDA-approved medications, behavioral therapies, and medical supervision. Medications help manage withdrawal and cravings, therapy addresses the psychological aspects of addiction, and medical supervision ensures safe and effective treatment adjustments for long-term recovery.

The components of medication-assisted therapy are explained below:
-
Medications: MAT utilizes FDA-approved medications such as methadone, buprenorphine, naltrexone, disulfiram, and acamprosate to help stabilize brain receptors, reduce withdrawal symptoms, and manage cravings. These medications prevent the euphoric effects of substances, restore chemical balance, and improve treatment retention. According to the National Institute on Drug Abuse (NIDA, 2023), MAT medications reduce the risk of opioid overdose deaths by 50% and increase patient retention rates by up to 70%.
-
Therapies: MAT is most effective when combined with evidence-based therapies like Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), Motivational Interviewing (MI), and Contingency Management (CM). These approaches help individuals understand triggers, develop coping skills, and build motivation for recovery. A study published in the Journal of Addiction Medicine (2021) found that patients receiving MAT with therapy have a 60% higher chance of long-term sobriety compared to those relying on medication alone.
-
Support Services: Comprehensive MAT programs include peer support, case management, vocational training, and housing assistance to address social determinants of recovery. Peer support groups provide accountability and encouragement, while case management ensures access to healthcare and employment resources. According to the Substance Abuse and Mental Health Services Administration (SAMHSA, 2022), patients with integrated support services are 50% more likely to maintain long-term recovery than those without.
Which Medications Are Used in MAT?
The medications used in MAT are methadone, buprenorphine, naltrexone, disulfiram, and acamprosate, each targeting different substance use disorders. Methadone and buprenorphine help manage opioid withdrawal and cravings by acting on brain receptors without producing a high, while naltrexone blocks opioid effects and reduces alcohol cravings.
Disulfiram creates unpleasant reactions to alcohol consumption, discouraging relapse, and acamprosate helps restore brain balance in individuals recovering from alcohol dependence. According to the National Institute on Drug Abuse (NIDA, 2023), MAT medications improve treatment retention rates by 70% and significantly lower relapse risks.
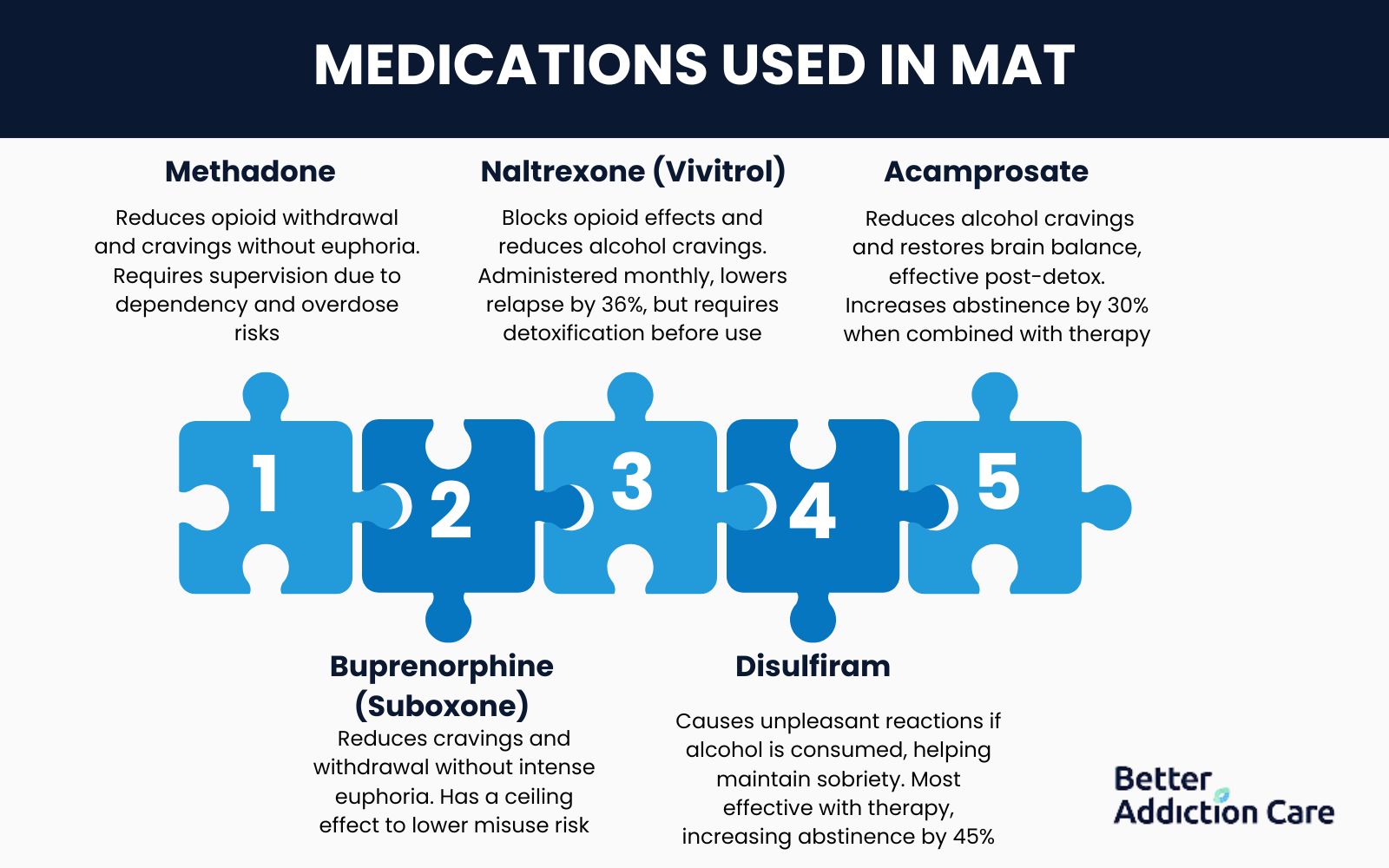
Medications used in MAT are explained below:
1. Methadone
Methadone is a long-acting opioid agonist used in Medication-Assisted Treatment (MAT) for opioid addiction to reduce withdrawal symptoms and cravings without producing euphoria. It works by binding to opioid receptors in the brain, stabilizing individuals recovering from heroin or prescription opioid dependence.
Methadone is administered once daily in liquid, tablet, or wafer form under supervision at specialized treatment clinics. According to the Substance Abuse and Mental Health Services Administration (SAMHSA, 2022), methadone treatment has been shown to decrease opioid-related deaths by over 50% when used consistently.
However, as a full opioid agonist, methadone carries risks of dependency, respiratory depression, and overdose if not carefully monitored, making medical supervision essential for safe use.
2. Buprenorphine (Suboxone)
Buprenorphine is a partial opioid agonist used in Medication-Assisted Treatment (MAT) for opioid addiction, providing withdrawal management and craving reduction without producing the intense euphoria associated with full opioids.
Unlike methadone, buprenorphine has a ceiling effect, meaning its opioid effects plateau at higher doses, reducing the risk of misuse and overdose. It is commonly prescribed as Suboxone, a combination of buprenorphine and naloxone, which further prevents abuse by triggering withdrawal if injected.
According to the National Institute on Drug Abuse (NIDA, 2023), patients receiving buprenorphine for opioid addiction are twice as likely to remain in treatment compared to those without MAT. With its strong safety profile, buprenorphine is prescribed in outpatient settings, allowing greater accessibility for individuals seeking opioid recovery.
3. Naltrexone (Vivitrol)
Naltrexone is an opioid antagonist used in relapse prevention for both opioid and alcohol dependence by blocking opioid receptors in the brain. Unlike methadone or buprenorphine, naltrexone is non-addictive and does not produce euphoric effects, making it a safer long-term option for recovery.
It is commonly administered as a once-monthly injection (Vivitrol) to ensure adherence and prevent relapse, though it is also available in oral tablet form. According to the National Institute on Drug Abuse (NIDA, 2023), individuals receiving naltrexone injections have a 36% lower relapse rate compared to those without MAT.
However, naltrexone requires complete detoxification before use, as taking it while opioids are still in the system triggers severe withdrawal symptoms.
4. Disulfiram
Disulfiram is an FDA-approved medication used in Medication-Assisted Treatment (MAT) for alcohol addiction. It works by blocking the enzyme aldehyde dehydrogenase, which is responsible for metabolizing alcohol, causing severe nausea, vomiting, headaches, and flushing if alcohol is consumed.
This deterrent effect helps individuals avoid alcohol use and maintain sobriety. According to the Substance Abuse and Mental Health Services Administration (SAMHSA, 2022), patients using disulfiram as part of a structured treatment program have a 45% higher alcohol abstinence rate than those without medication support.
Because of its strong aversive reaction, disulfiram is most effective when combined with behavioral therapy and counseling to reinforce long-term alcohol recovery.
5. Acamprosate
Acamprosate is an FDA-approved medication used in Medication-Assisted Treatment (MAT) for alcohol addiction to help individuals maintain long-term sobriety. It works by stabilizing brain chemistry disrupted by chronic alcohol use and reducing post-withdrawal cravings and emotional distress associated with alcohol dependence.
Unlike disulfiram, acamprosate does not cause an aversive reaction to alcohol but instead helps restore neurotransmitter balance, making it particularly beneficial for individuals experiencing persistent cravings after detox.
According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA, 2023), patients taking acamprosate have a 30% higher alcohol abstinence rate compared to those in therapy alone. Acamprosate is most effective when used alongside counseling and behavioral therapy to support sustained recovery.
What are the Risks of MAT?
The risks of MAT are dependency on medications, potential side effects, and misuse in unsupervised settings. While MAT significantly reduces withdrawal symptoms and relapse rates, medications like methadone and buprenorphine require careful monitoring to prevent overuse, dependence, or diversion into illegal use.

The risks of MAT are explained below:
-
Dependence on medication: Some MAT medications, such as methadone and buprenorphine, are opioids themselves and lead to physical dependence if not carefully managed. However, they are prescribed in controlled doses to minimize misuse while supporting recovery. According to the National Institute on Drug Abuse (NIDA, 2023), approximately 10-15% of patients on long-term MAT require gradual tapering to avoid dependence.
-
Potential for misuse or diversion: Medications like buprenorphine are misused if taken inappropriately, particularly when obtained without medical supervision. To prevent this, combination formulations such as Suboxone (buprenorphine + naloxone) are designed to reduce abuse potential. The Substance Abuse and Mental Health Services Administration (SAMHSA, 2022) reports that MAT programs with strict monitoring reduce medication diversion by 60%.
-
Side effects from medications: MAT drugs cause nausea, drowsiness, dizziness, or constipation, depending on the individual’s response. Methadone, for example, leads to respiratory depression if taken in high doses, while naltrexone causes liver issues in some patients. The FDA (2023) recommends regular monitoring to adjust dosages and minimize adverse effects.
-
Long-term medication costs: MAT requires years of continuous treatment, leading to significant financial strain, particularly for uninsured individuals. Methadone maintenance therapy, for instance, costs approximately $126 per week per patient when provided in federally regulated clinics. According to SAMHSA (2022), only 54% of individuals in need of MAT have full insurance coverage for long-term treatment.
-
Withdrawal symptoms if stopped abruptly: Discontinuing MAT without proper tapering leads to severe withdrawal symptoms, increasing the risk of relapse. Methadone and buprenorphine require gradual dose reduction to avoid complications. The National Institute on Drug Abuse (NIDA, 2023) states that patients who taper off MAT under medical supervision have a 35% higher chance of maintaining sobriety compared to those who stop suddenly.
-
Limited access in certain areas: Many rural or underserved communities lack MAT providers, making treatment inaccessible for those in need. Methadone, in particular, is only available through federally regulated clinics, restricting its reach.
-
The stigma surrounding MAT use: Despite its proven effectiveness, MAT faces stigma from the public and even some healthcare providers, leading to hesitancy in seeking treatment. Many falsely believe that MAT is merely replacing one addiction with another, despite scientific evidence proving otherwise.
-
Need for continuous medical supervision: MAT requires ongoing medical oversight to ensure safe dosing, therapy adherence, and progress evaluation. Patients must attend regular check-ins, urine screenings, and counseling sessions, which feel burdensome.
-
Potential interactions with other medications: MAT medications interact with antidepressants, benzodiazepines, and certain painkillers, leading to adverse effects or overdose risk. For example, combining methadone with sedatives causes dangerous respiratory depression. The FDA (2023) advises careful medication management to prevent dangerous drug interactions.
-
Not addressing underlying psychological issues: While MAT helps with physical withdrawal and cravings, it does not directly treat co-occurring mental health disorders like depression or PTSD. Without integrated therapy, individuals struggle with unresolved emotional triggers, increasing the risk of relapse.
What are the Benefits of Using Mat in Addiction Recovery?
The benefits of using MAT in addiction recovery are reduced withdrawal symptoms, improved treatment retention, and lower relapse rates. According to the National Institute on Drug Abuse (NIDA, 2023), patients receiving MAT are 70% more likely to remain in treatment and have a 50% lower risk of overdose compared to those who attempt recovery without medication support.
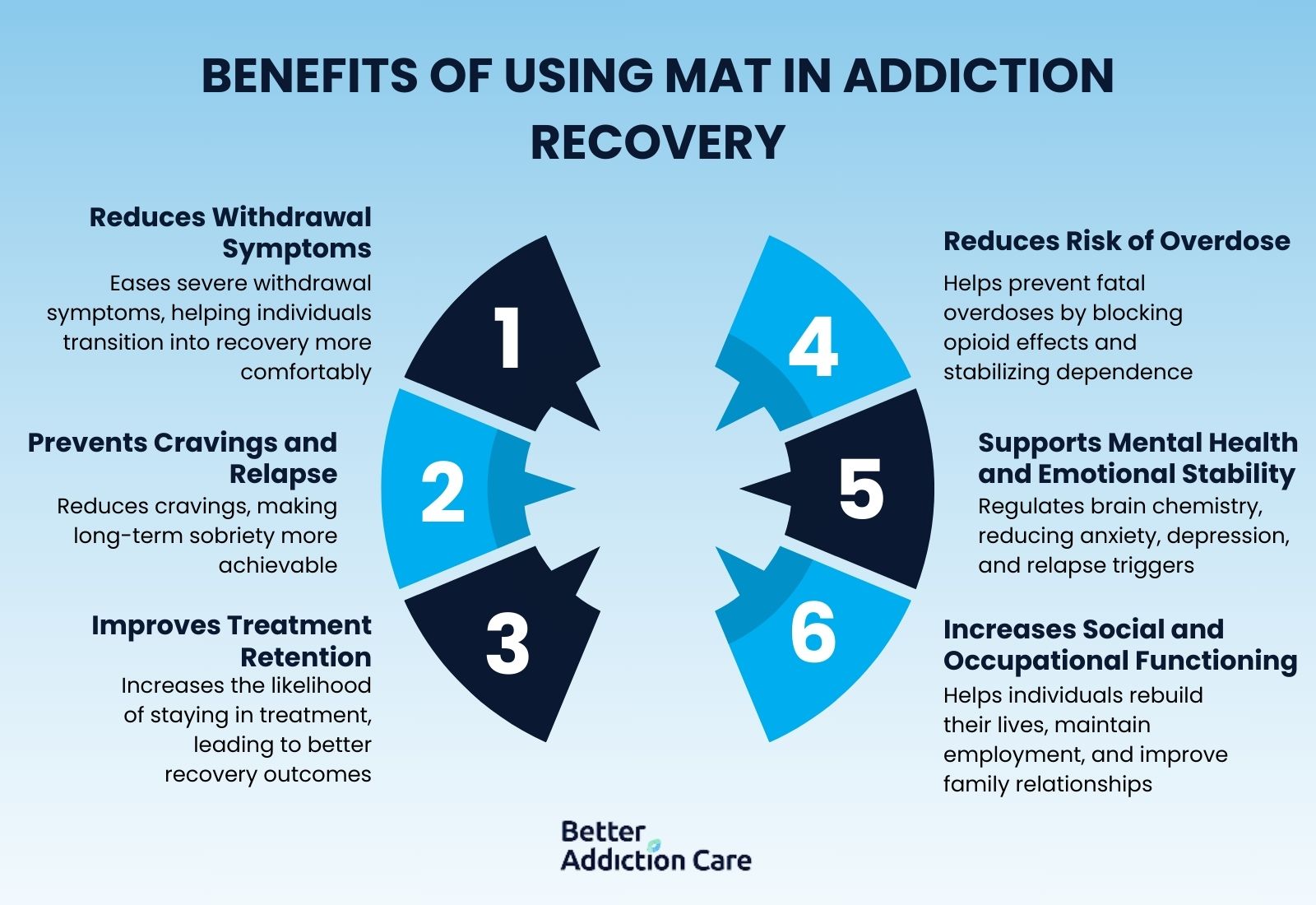
The benefits of using MAT in addiction recovery are explained below:
-
Reduces withdrawal symptoms: MAT helps ease severe withdrawal symptoms, allowing individuals to transition into recovery more comfortably. Medications like methadone and buprenorphine stabilize brain receptors, reducing the physical distress associated with opioid and alcohol detoxification. According to the National Institute on Drug Abuse (NIDA, 2023), MAT reduces acute withdrawal severity by up to 60%, improving early treatment engagement.
-
Prevents cravings and relapse: MAT reduces intense cravings that lead to relapse, making long-term sobriety more achievable. Naltrexone blocks opioid receptors, preventing users from experiencing any euphoric effects, while acamprosate stabilizes brain chemistry to minimize alcohol cravings.
-
Improves treatment retention: Individuals receiving MAT are more likely to stay in treatment longer, leading to better recovery outcomes. Medications help reduce the discomfort that causes people to drop out of rehabilitation early, allowing them to fully engage in therapy and counseling. According to SAMHSA (2022), MAT increases treatment retention rates by 70%, significantly improving long-term recovery success.
-
Reduces the risk of overdose: MAT helps prevent fatal overdoses by blocking the effects of opioids and stabilizing opioid dependence. Naltrexone prevents opioids from binding to brain receptors, and methadone/buprenorphine reduces the urge for illicit opioid use, lowering the risk of accidental overdose. The Centers for Disease Control and Prevention (CDC, 2023) reports that MAT reduces opioid-related overdose deaths by 50% among individuals in recovery.
-
Supports mental health and emotional stability: Many people with substance use disorders struggle with co-occurring mental health conditions, and MAT provides stability to engage in therapy and address emotional health. By regulating brain chemistry, MAT reduces anxiety, depression, and impulsivity, which are common relapse triggers. The National Institute of Mental Health (NIMH) in 2023 states that patients using MAT alongside therapy have a 65% improvement in mental health outcomes compared to those in non-medicated treatment.
-
Increases social and occupational functioning: MAT allows individuals to focus on rebuilding their lives and improving employment stability, family relationships, and overall well-being. By reducing withdrawal symptoms and cravings, patients return to work, education, and social activities without constant fear of relapse. According to SAMHSA in 2022, MAT patients are twice as likely to maintain employment and stable housing compared to those who go through detox without medication support.
Who Needs Medication-Assisted Treatment?
People experiencing severe withdrawal symptoms, those with a history of relapse, and individuals at high risk of overdose need Medication-Assisted Treatment (MAT). MAT is recommended for individuals who struggle with intense cravings, do not maintain sobriety with therapy alone, or have co-occurring mental health disorders.
It is also beneficial for patients transitioning from detox to long-term recovery and those requiring medical stabilization to safely manage their addiction. According to the National Institute on Drug Abuse (NIDA, 2023), individuals receiving MAT are 50% more likely to complete treatment successfully than those who attempt abstinence-only recovery.
The people who need medication-assisted treatment are explained below:
-
People experiencing severe withdrawal symptoms: MAT helps manage intense withdrawal effects, reducing discomfort and preventing complications that arise from stopping substance use abruptly.
-
Those with a history of relapse: Individuals who have repeatedly relapsed benefit from MAT as it provides long-term craving control and relapse prevention.
-
Individuals at high risk of overdose: MAT, especially with naltrexone or buprenorphine, blocks opioid effects and reduces the likelihood of a fatal overdose, making it critical for individuals who have previously overdosed.
-
People struggling with intense cravings: MAT modifies brain chemistry to reduce persistent cravings, allowing individuals to focus on recovery without constant urges to use substances.
-
Those unable to maintain sobriety with therapy alone: While therapy helps address the psychological aspects of addiction, some individuals require medication support to maintain sobriety and prevent relapse.
-
Individuals with co-occurring mental health disorders: MAT supports individuals with dual diagnoses, such as depression or anxiety, by stabilizing mood and reducing impulsivity.
-
Patients transitioning from detox to long-term recovery: After detox, MAT helps smooth the transition into rehabilitation programs, preventing early relapse due to residual cravings or withdrawal symptoms.
-
People requiring medical stabilization for addiction: Some individuals need structured, medically supervised care to manage their addiction safely and effectively, making MAT an essential treatment option.
What Are the Main Addictions that Need MAT?
The main addictions that need MAT are opioid use disorder (OUD) and alcohol use disorder (AUD) because both involve severe withdrawal symptoms, high relapse rates, and significant risks of overdose or long-term health complications.
Individuals with OUD benefit from medications like methadone, buprenorphine, and naltrexone, which help reduce cravings, stabilize brain receptors, and prevent opioid-induced euphoria, lowering the risk of fatal overdoses.
Similarly, those with AUD require acamprosate, disulfiram, or naltrexone to manage cravings, block alcohol’s pleasurable effects, and prevent relapse. According to the National Institute on Drug Abuse (NIDA, 2023), MAT reduces opioid overdose deaths by 50% and increases long-term abstinence rates for alcohol addiction by 30%. By addressing both physical dependence and behavioral triggers, MAT is a critical tool in the treatment of these substance use disorders.
Is MAT the Same as Drug Detox?
No, MAT is not the same as drug detox. Detox is a short-term process focused on eliminating substances from the body, while MAT is a long-term treatment approach that manages cravings and supports recovery.
Detox lasts a few days to weeks and addresses acute withdrawal symptoms, but it does not provide ongoing support to prevent relapse. MAT, on the other hand, continues beyond drug detox, using medications like methadone, buprenorphine, and naltrexone to stabilize brain chemistry and reduce the risk of returning to substance use.
According to the Substance Abuse and Mental Health Services Administration (SAMHSA, 2023), individuals who complete detox without MAT have a relapse rate of over 80%, whereas MAT significantly improves long-term recovery outcomes.
Can MAT be Used in Outpatient Rehab?
Yes, MAT can be used in outpatient rehab because it allows individuals to receive medication-assisted support while continuing their daily responsibilities. Unlike inpatient treatment, where patients stay at a facility, outpatient MAT provides structured medical supervision and counseling while enabling individuals to live at home and maintain work or family obligations.
Medications like buprenorphine and naltrexone are commonly prescribed in outpatient settings, reducing cravings and preventing relapse without requiring hospitalization. According to the National Institute on Drug Abuse (NIDA, 2023), outpatient MAT programs have been shown to increase treatment adherence by 65% and lower relapse rates compared to non-medicated outpatient approaches.
How Is MAT Used During Inpatient Drug Rehab?
MAT is used in inpatient drug rehab to provide 24/7 medical supervision, manage withdrawal symptoms, and support long-term recovery through structured therapy and medication management.
In residential treatment centers, individuals receive FDA-approved medications such as methadone, buprenorphine, and naltrexone in combination with behavioral therapy, counseling, and peer support programs. This approach ensures that patients are stabilized before transitioning into outpatient care, reducing the likelihood of early relapse due to severe cravings or untreated withdrawal symptoms.
According to the Substance Abuse and Mental Health Services Administration (SAMHSA, 2023), inpatient MAT programs increase early recovery success rates by 60% compared to non-medicated inpatient treatment. These programs also allow close monitoring of medication adherence, reducing the risk of misuse or diversion.
Additionally, MAT in inpatient settings is especially beneficial for individuals with severe opioid use disorder (OUD) or alcohol use disorder (AUD), as it provides structured support and immediate medical intervention when needed. By integrating MAT into inpatient rehab, individuals have a higher chance of long-term recovery, better engagement in therapy, and improved overall treatment outcomes.
What are the Typical Costs and Insurance Coverage for MAT?
The typical costs and insurance coverage for MAT are dependent on the medication used, the treatment setting, and whether the individual has insurance or qualifies for financial assistance.
Methadone treatment at a federally regulated clinic costs $126 per week or around $6,500 annually, while buprenorphine-based treatments like Suboxone range from $300 to $600 per month without insurance. Naltrexone (Vivitrol) injections, used for opioid and alcohol addiction, cost up to $1,500 per dose if paid out of pocket.
Many private insurance plans, Medicaid, and Medicare cover MAT, but coverage levels vary by state and provider. According to the Substance Abuse and Mental Health Services Administration (SAMHSA, 2023), Medicaid covers MAT in all 50 states, although copayments and prior authorization requirements differ.
Some treatment centers also offer sliding-scale payment options, grants, and state-funded programs to assist individuals who cannot afford MAT. Expanding insurance coverage for MAT has been a key strategy in reducing opioid-related deaths, as research from the National Institute on Drug Abuse (NIDA, 2023) shows that patients with insurance-covered MAT are 50% more likely to complete treatment compared to those without financial support.
Is MAT Covered by Insurance?
Yes, MAT is covered by insurance, but coverage varies depending on the provider, state, and specific treatment plan. Medicaid, Medicare, and most private insurance plans cover FDA-approved medications like methadone, buprenorphine, and naltrexone, along with counseling and therapy services.
However, some insurers require prior authorization, copayments, or proof of medical necessity, which creates barriers to access. According to the Substance Abuse and Mental Health Services Administration (SAMHSA, 2023), Medicaid covers at least one form of MAT in all 50 states, and the Affordable Care Act mandates coverage for substance use treatment, including MAT.
Despite this, gaps in insurance coverage still exist, leaving some individuals reliant on state-funded programs, grants, or sliding-scale payment options to afford treatment.
Where Can I Find Reliable MAT Rehab Programs Near Me?
You can find reliable MAT rehab programs near you through the SAMHSA provider directory, which lists licensed treatment centers that offer FDA-approved MAT medications and behavioral therapies.
When evaluating providers, ensure they are accredited by recognized organizations such as the Joint Commission and that they meet state-specific licensing requirements. Patient reviews and testimonials also provide valuable insights into the quality of care and success rates at each rehab facility.
According to the National Institute on Drug Abuse (NIDA, 2023), facilities with positive reviews and certifications are more likely to provide safe, effective MAT services. Additionally, consulting your healthcare provider or insurance company for recommendations helps narrow down reliable MAT programs near you.
How Is MAT Regulated?
MAT is regulated through federal and state regulations, including the Drug Addiction Treatment Act of 2000 (DATA 2000) Waiver, which allows qualified physicians to prescribe buprenorphine for opioid use disorder.
The FDA also provides guidelines for the approval and use of MAT medications like methadone, buprenorphine, and naltrexone, ensuring they meet safety and efficacy standards. Our comprehensive treatment finder helps you locate state-licensed MAT providers across Georgia, Massachusetts, Oklahoma, Illinois, New York, Pennsylvania, California, Texas, and Florida that comply with both federal regulations and local monitoring requirements for evidence-based addiction care.
Does MAT Address Co-Occurring Mental Health Conditions?
Yes, MAT addresses co-occurring mental health conditions like depression or anxiety through integrated treatment approaches. Medications like buprenorphine and naltrexone not only help manage opioid or alcohol dependence but also improve mood stability and reduce anxiety by stabilizing brain chemistry.
Dual diagnosis treatment combines MAT with therapy to address both substance use and mental health issues simultaneously, improving overall recovery outcomes.
Does MAT Replace One Addiction With Another?
No, MAT does not replace one addiction with another; it helps individuals stabilize their addiction and work toward long-term recovery. While some medications used in MAT, such as methadone and buprenorphine, are opioids themselves, they are prescribed in controlled doses to prevent withdrawal symptoms and cravings without causing euphoria or a high.
Unlike illicit drugs or alcohol, MAT medications are used in a medically supervised, structured treatment plan to provide gradual recovery and reduce the risk of relapse. The Substance Abuse and Mental Health Services Administration (SAMHSA, 2022) states that MAT helps individuals gradually rebuild their lives without the intense physical dependency associated with untreated addiction.
MAT also works best when combined with therapy to address underlying psychological factors, making it a comprehensive treatment rather than a substitution of one dependency for another.
What Happens if MAT Is Stopped?
If MAT is stopped individuals experience cravings and a high risk of relapse. Medications like methadone and buprenorphine help stabilize brain chemistry and reduce cravings, making it easier for individuals to stay sober and engage in therapy.
If MAT is stopped suddenly, individuals experience intense withdrawal symptoms, including muscle pain, anxiety, and nausea, as the brain adjusts to functioning without the medication. According to the National Institute on Drug Abuse (NIDA, 2023), patients who stop MAT abruptly are more likely to relapse, as withdrawal symptoms lead to a return to substance use.
It is always recommended that MAT be tapered off gradually, under medical supervision, to prevent these adverse effects and ensure a smooth transition into sustained recovery.
Is MAT Safe During Pregnancy?
Yes, MAT is safe during pregnancy and is an essential tool for managing opioid use disorder (OUD) in pregnant women. Medications like methadone and buprenorphine are FDA-approved and have been shown to reduce the risk of complications associated with opioid withdrawal, such as miscarriage, premature labor, and neonatal abstinence syndrome (NAS).
According to the National Institute on Drug Abuse (NIDA, 2023), MAT significantly improves maternal health outcomes and reduces the risk of adverse pregnancy outcomes compared to untreated opioid use disorder. Buprenorphine is preferred in pregnancy due to its lower risk of overdose and safer profile, but methadone remains a widely used option under medical supervision.
It's important to note that MAT should always be administered and monitored by healthcare providers experienced in managing addiction during pregnancy.
How Effective Is MAT for Addiction Recovery?
MAT is highly effective for addiction recovery, particularly for opioid and alcohol use disorders. MAT improves treatment retention, reduces the risk of relapse, and lowers the likelihood of overdose.
MAT also addresses both the physical dependence on substances and the psychological triggers for addiction by combining medication with therapy, ensuring a comprehensive recovery plan.
The National Institute on Drug Abuse (NIDA, 2023) shows that MAT increases long-term sobriety rates by 60% and significantly improves the quality of life for individuals in recovery.
Can MAT Prevent Relapse?
Yes, MAT can prevent relapse by managing cravings and withdrawal symptoms, allowing individuals to focus on long-term recovery. Medications such as methadone, buprenorphine, and naltrexone help stabilize brain chemistry and prevent the physical triggers that lead to relapse.
According to the National Institute on Drug Abuse (NIDA, 2023), MAT reduces relapse rates by up to 50% for individuals recovering from opioid and alcohol addiction. Additionally, when combined with behavioral therapies, MAT helps address the psychological aspects of addiction, providing individuals with the tools and coping mechanisms they need to maintain sobriety over time.
Related Articles
Treatment Centers in Virginia