Paying for Rehab with the Affordable Care Act - ACA Plans
Paying for addiction treatment is a major concern for many individuals and families, but the Affordable Care Act (ACA) makes it possible to access high-quality rehab without facing overwhelming costs. As of the 2024 enrollment period, approximately 21.3 million individuals signed up for health insurance coverage through the Affordable Care Act (ACA) marketplaces, marking a record high in enrollment numbers according to the Centers for Medicare and Medicaid Services. The ACA is a federal law that expanded health insurance options across the country and requires all marketplace plans to include coverage for substance use disorder treatment.

For people struggling with addiction, ACA insurance offers a clear path to recovery. Instead of delaying treatment because of cost, individuals are able to begin the process with the support of a structured plan that covers a wide range of clinical services like detox, residential rehab, outpatient care, and therapy for drug or alcohol addiction.
If you're ready to start treatment or helping a loved one find care, understanding how ACA plans work for rehab is a powerful first step. With the right coverage in place, recovery becomes more than a possibility; it becomes a priority.
How to Pay for Rehab with the Affordable Care Act Insurance?
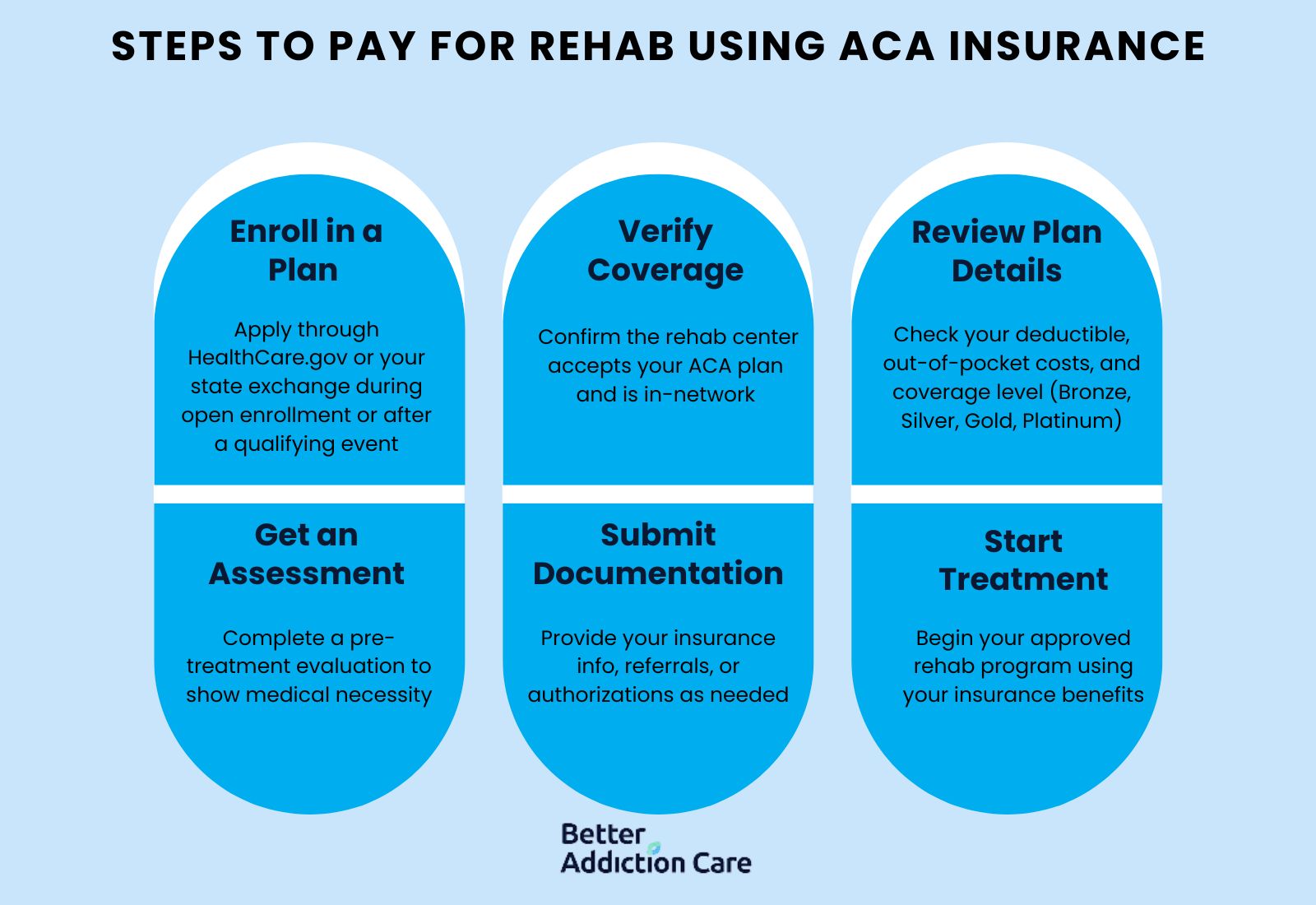
To pay for addiction treatment through an Affordable Care Act (ACA) plan involves a structured process that gives individuals access to evidence-based rehab services without the burden of paying full cost. Once enrolled in a plan through the Health Insurance Marketplace, individuals use their benefits to offset the cost of care at an in-network treatment facility. Understanding your plan’s deductible, coinsurance, and covered services is key to managing expenses and getting the help you need.
Steps to pay for rehab using ACA insurance:
-
Enroll in an ACA Marketplace Plan: Visit HealthCare.gov or your state’s exchange to apply during open enrollment or a qualifying life event.
-
Verify Coverage: Contact your selected treatment center to confirm they accept your ACA plan and are in-network.
-
Review Plan Details: Understand your plan’s deductible, out-of-pocket maximum, and what percentage of costs are covered (Bronze, Silver, Gold, or Platinum level).
-
Get a Pre-Treatment Assessment: Most plans require an assessment to confirm medical necessity for rehab services.
-
Submit Required Documentation: Provide your insurance ID and any necessary referrals or prior authorizations as requested by the treatment provider.
-
Start Treatment: Once approved, begin your detox, inpatient, or outpatient care using your ACA plan benefits.
As of the 2025 Open Enrollment Period, over 24 million consumers selected health coverage through the ACA Marketplaces, marking a significant increase from previous years according to the Centers for Medicare and Medicaid. Thus showing how many people use this type of insurance.
How Does the Affordable Care Act Improve Access to Addiction Treatment?
The Affordable Care Act (ACA) improves access to addiction treatment by requiring all marketplace insurance plans to cover substance use disorder (SUD) services as part of essential health benefits. This federal policy integrates mental health and addiction care into standard medical coverage, removing the financial and legal barriers that once made treatment inaccessible for many.
According to the Center for Children and Families at Georgetown University, Medicaid, expanded under the ACA, has become the largest single payer of behavioral health services in the country, offering support to children, teens, and adults with substance use disorders. Additionally, the Centers for Medicare & Medicaid Services (CMS) reported that in 2021, 45% of Medicaid expansion enrollees received treatment for a substance use disorder. These numbers reflect the ACA’s role in delivering real care to vulnerable populations.
Expanded coverage through ACA plans ensures that more individuals struggling with addiction receive detox, residential care, outpatient treatment, and dual diagnosis support without facing insurmountable costs.
What is the Affordable Care Act?
The Affordable Care Act (ACA) is a federal healthcare law enacted in 2010 to increase access to affordable health insurance for Americans. Commonly known as “Obamacare,” the ACA expanded Medicaid, created health insurance marketplaces, and required insurance plans to cover a core set of health services including substance use disorder and mental health treatment.
One of the ACA’s most significant features is that it prohibits insurance companies from denying coverage based on pre-existing conditions, such as a history of addiction. It also allows young adults to remain on their parents’ insurance plans until age 26 and provides income-based subsidies to help individuals and families afford coverage.
As of the latest reports, 38 states and the District of Columbia have adopted Medicaid expansion under the ACA, broadening access to healthcare for low-income individuals. The ACA mandates that insurance companies spend at least 80% of premium dollars on medical care and health care quality improvement, ensuring value for consumers according to the Centers for Medicare and Medicaid.
By making addiction treatment a covered benefit under most plans, the ACA has opened the door for millions of Americans to receive detox, inpatient rehab, outpatient services, and behavioral therapy as part of their recovery.
What Does ACA Insurance Cover for Addiction Treatment?

The Affordable Care Act (ACA) requires all health insurance plans offered through the Health Insurance Marketplace to include coverage for substance use disorder (SUD) services, treating addiction the same as any other medical condition. This includes a wide range of services necessary for both short-term stabilization and long-term recovery.
Covered addiction treatment services under ACA-compliant plans include:
-
Comprehensive addiction assessments and evaluations
-
Brief intervention and early treatment services
-
Medication-assisted treatment (MAT)
-
Outpatient clinic visits
-
Inpatient and residential rehabilitation
-
Drug and alcohol testing
-
Family and individual counseling
-
Anti-craving medications
-
Home health services when medically necessary
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), ACA plans must follow mental health parity, ensuring addiction treatment is just as accessible and thorough as care for physical health conditions.
Inpatient services such as medical detox programs are also covered when deemed medically necessary, depending on the plan and provider network.
How Much Does the Affordable Care Act Insurance Cover for Addiction Treatment?
The affordable care act covers different amounts depending on your plan. There are five types of Marketplace plans under the ACA, each covering a different percentage of healthcare costs. The breakdown is as follows:
-
Bronze Plan: Covers approximately 60% of treatment costs
-
Silver Plan: Covers approximately 70%
-
Gold Plan: Covers approximately 80%
-
Platinum Plan: Covers approximately 90%
-
Catastrophic Plan: Covers around 60%, available only to individuals under 30 or with qualifying hardships
Each plan type affects how much you’ll pay out-of-pocket for addiction care, including co-pays, deductibles, and coinsurance. Choosing the right plan depends on your health needs and financial situation.
Some states operate their own Health Insurance Marketplace instead of using HealthCare.gov, and coverage levels vary slightly depending on your state's implementation of Medicaid expansion and addiction treatment funding. It is important to verify your benefits and ensure what your plan offers.
Who Is Eligible for Coverage with the Affordable Care Act?
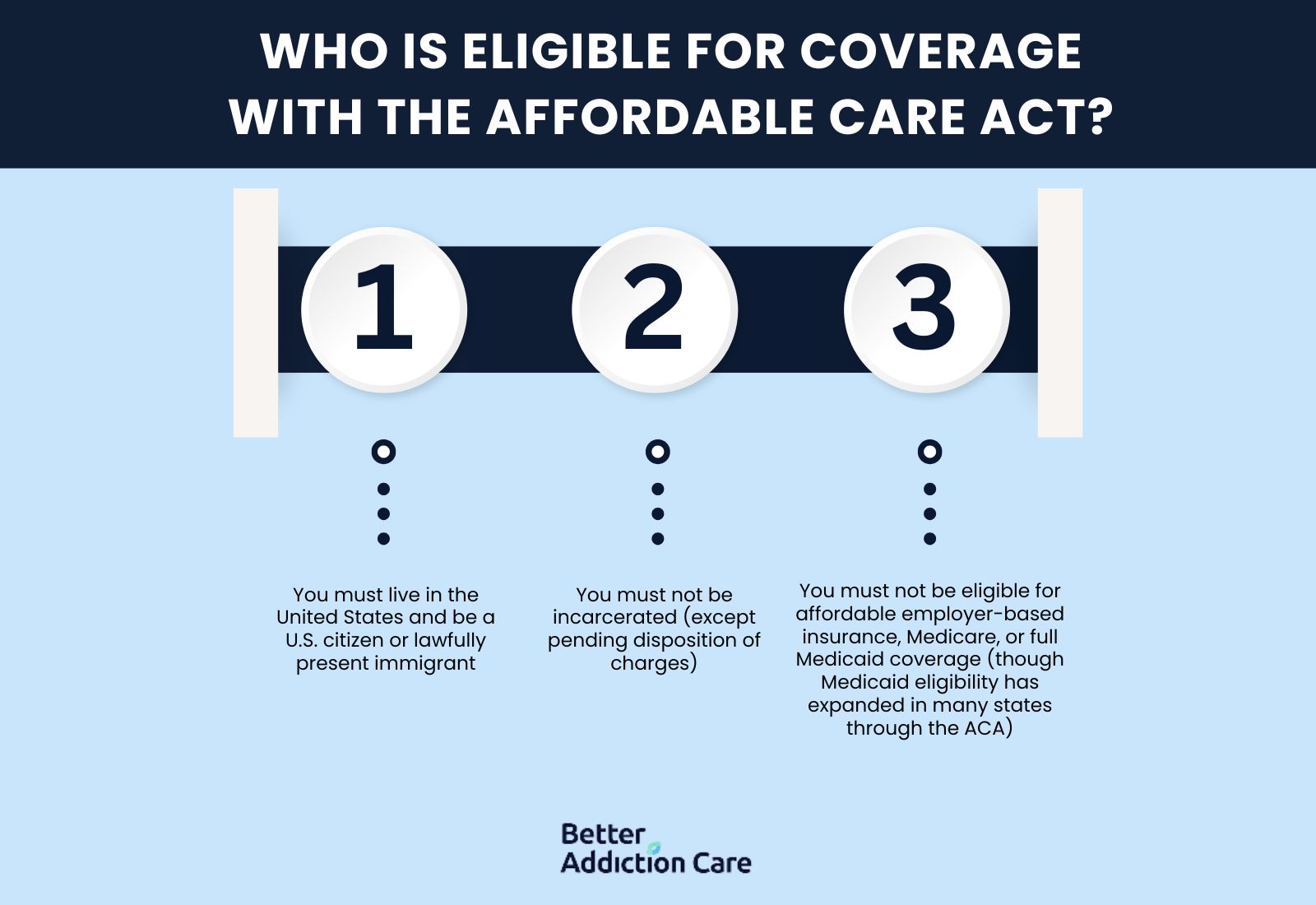
The people eligible for coverage with the Affordable Care Act (ACA) Marketplace include anyone who is a US citizen and doesn’t have employer based insurance. Eligibility is primarily based on income, residency status, and whether the applicant has access to other forms of health coverage, such as an employer-sponsored plan or Medicaid.
To qualify for ACA coverage:
-
You must live in the United States and be a U.S. citizen or lawfully present immigrant.
-
You must not be incarcerated (except pending disposition of charges).
-
You must not be eligible for affordable employer-based insurance, Medicare, or full Medicaid coverage (though Medicaid eligibility has expanded in many states through the ACA).
Financial help is available for many applicants. According to the Centers for Medicare & Medicaid Services (CMS), more than 87% of people enrolled through the ACA Marketplace receive premium subsidies to reduce monthly insurance costs.
For individuals and families struggling with addiction, these benefits make accessing professional substance use disorder treatment more affordable and realistic.
What Providers Are Included in the Affordable Care Act?
The providers included in the Affordable Care Act include a wide range of private health insurance companies that participate depending on your state. These providers offer ACA-compliant plans that include coverage for substance use disorder treatment, mental health care, preventive services, and more.
While availability varies by state, many of the largest and most recognized providers offer ACA plans, including:
-
Blue Cross Blue Shield (BCBS)
-
Aetna
-
Cigna
-
Ambetter
-
UnitedHealthcare
-
Molina Healthcare
-
Oscar Health
-
Kaiser Permanente
Many of these plans are widely accepted by treatment centers and rehabs all over the United States.
How to Find a Rehab Center that Accepts ACA Insurance?
To find a rehab center that accepts ACA Marketplace insurance, you can use online resources and websites like Better Addiction Care that provide a rehab locator tool to help you filter rehabs near you. These resources provide listings that include what programs are available at specific centers and what insurances are accepted.
Does the Affordable Care Act cover drug and alcohol rehab?
Yes. According to the U.S. Department of Health and Human Services, all ACA-compliant health insurance plans must include coverage for drug and alcohol rehab, which includes detox, inpatient rehab, outpatient care, counseling, and medication-assisted treatment.
When can I enroll in an ACA plan to cover rehab costs?
You can enroll in an ACA plan during the Open Enrollment Period, which typically runs from November to January each year. If you miss that window, you still qualify for a Special Enrollment Period due to a major life change, such as loss of job-based coverage or a recent diagnosis.
Can I use ACA insurance for both mental health and addiction treatment?
Yes. The Affordable Care Act requires all marketplace plans to cover mental health and substance use disorder services as part of their essential health benefits. This includes treatment for co-occurring conditions like depression, anxiety, PTSD, and addiction, all under the same plan.
Related Articles
Treatment Centers in New Jersey








