Prescription Drug addiction: Definition, Types, signs and symptoms, Effects, Treatment
Prescription drug addiction occurs when individuals misuse medications like opioids, benzodiazepines, or stimulants, leading to compulsive use despite harmful consequences. Drugs such as oxycodone, hydrocodone, and fentanyl are involved, and misuse escalates into seeking out street drugs when prescriptions are unavailable. According to the National Institute on Drug Abuse (NIDA, 2018), an estimated 18 million people in the United States misused prescription medications in the past year.

Prescription drug addiction occurs when individuals misuse medications like opioids, benzodiazepines, or stimulants, leading to compulsive use despite harmful consequences. Drugs such as oxycodone, hydrocodone, and fentanyl are involved, and misuse escalates into seeking out street drugs when prescriptions are unavailable. According to the National Institute on Drug Abuse (NIDA, 2018), an estimated 18 million people in the United States misused prescription medications in the past year.
The main signs and symptoms of prescription drug addiction include physical changes like drowsiness, nausea, and weight fluctuations, as well as behavioral shifts such as mood swings, anxiety, irritability, and isolation. Symptoms vary depending on the type of drug misused, with opioids, depressants, and stimulants showing distinct patterns.
The effects of prescription drug addiction are both immediate and long-term, ranging from impaired judgment and organ damage to severe brain changes and cardiovascular issues. Families and communities suffer emotional and financial burdens, with public health systems bearing rising costs due to widespread misuse of prescription and street drugs.
Effective treatment methods for prescription drug addiction include medical detox under supervision, behavioral therapies like CBT and DBT, medication-assisted treatment (MAT) with drugs like buprenorphine, and peer support programs. Relapse prevention strategies and ongoing recovery support are critical to maintaining long-term sobriety and reducing the risk of returning to drug use.
What Is Prescription Drug Addiction?
Prescription drug addiction is a chronic, relapsing disorder characterized by the compulsive misuse of medications that a healthcare provider legally prescribes. Medically, it is defined as the development of dependence on a drug, where individuals continue to use the substance despite harmful consequences. This condition involves changes to the brain chemistry, particularly affecting the central nervous system pathways that regulate reward and pleasure.
Many prescription drugs, such as opioids, benzodiazepines, and stimulants, alter dopamine levels, a neurotransmitter important for feelings of pleasure and reinforcement, leading to intense cravings and loss of control over use. Prescription drugs become addictive not only because of their ability to relieve pain, anxiety, or attention problems but also due to their pharmacological action on the brain's reward system.
According to the 2022 National Survey on Drug Use and Health (NSDUH), approximately 5.5 million people aged 12 and older in the United States reported misusing prescription pain relievers within the past year. Repeated misuse of these prescription drug medications disrupts normal neural function, creating a cycle of dependence that requires professional intervention to break.
Which Prescription Medications Are Most Commonly Misused?
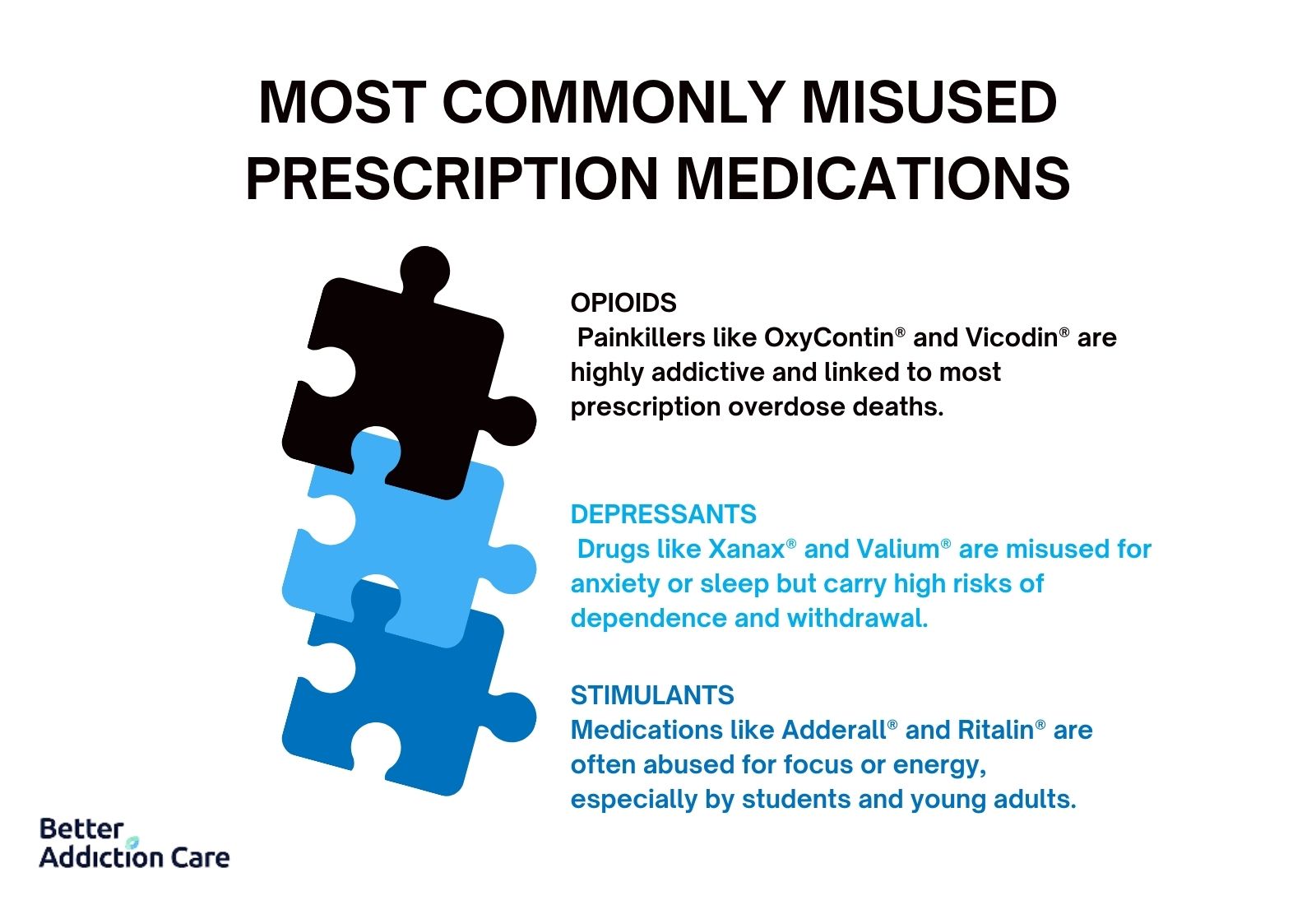
Prescription medications that are most commonly misused include opioids, depressants like benzodiazepines, and stimulants. These drugs, while effective when used appropriately under medical supervision, have a high potential for misuse due to their powerful effects on the central nervous system. Misuse involves taking higher doses than prescribed, using someone else's medication, or using the drug for the euphoric effects rather than for medical reasons. According to the 2022 National Survey on Drug Use and Health (NSDUH), opioids, benzodiazepines, and stimulants rank among the top classes of prescription drugs most frequently misused in the United States. Overdose deaths involving prescription opioids, including medications like oxycodone and hydrocodone, accounted for more than 16,700 fatalities nationwide in 2021, as reported by the Centers for Disease Control and Prevention (CDC).
The following prescription medications are most commonly misused:
-
Opioids/Narcotics/Pain Relievers: Opioids are powerful medications used primarily to manage moderate to severe pain. They work by binding to opioid receptors in the brain and spinal cord, reducing the perception of pain and triggering feelings of euphoria. Common examples include oxycodone (OxyContin®) and hydrocodone (Vicodin®). Due to their intense effects on the brain's reward system, opioids have a high potential for misuse and addiction. According to the Drug Enforcement Administration (DEA), prescription opioids are involved in nearly 70% of all drug overdose deaths related to prescription medications.
-
Depressants (Benzodiazepines, Tranquilizers, Barbiturates, Sedatives): Depressants slow down brain activity and are commonly prescribed to treat anxiety, panic disorders, and sleep disturbances. This category includes benzodiazepines like alprazolam (Xanax®), diazepam (Valium®), and clonazepam (Klonopin®), as well as barbiturates and other sedatives. While these medications are effective for short-term use, they are easily misused, leading to dependence and life-threatening withdrawal symptoms. SAMHSA data show that over 4.8 million people reported the misuse of benzodiazepines in the past year, making them one of the most misused prescription drug categories in the U.S.
-
Stimulants: Stimulants are prescribed to treat attention-deficit/hyperactivity disorder (ADHD) and certain sleep disorders like narcolepsy. These drugs increase alertness, energy, and attention by boosting levels of dopamine and norepinephrine in the brain. Commonly misused stimulants include amphetamine (Adderall®) and methylphenidate (Ritalin®). The DEA reports that stimulant misuse is especially prevalent among young adults and college students seeking enhanced academic performance or recreational highs. In 2021, nearly 2 million people aged 12 and older reported misusing prescription stimulants, highlighting a growing concern about non-medical use and overdose risks tied to this class.
How Can Prescription Medication Use Turn Into Addiction?
Prescription medication use turns into addiction when repeated misuse alters the brain's reward pathways, leading to compulsive drug-seeking behavior and loss of control over use. Chronic exposure to certain medications, particularly opioids, benzodiazepines, and stimulants, changes how the brain processes dopamine, causing intense cravings, reduced sensitivity to natural rewards, and eventually dependence. Dependency develops within just a few weeks of misuse, especially when high doses are taken regularly without medical supervision.
Prescription medication use turns into addiction in the following ways:
-
Disruption of Dopamine and Reward Pathways: When prescription drugs like opioids or stimulants are misused, they cause a surge in dopamine levels, overstimulating the brain's natural reward pathways. This creates powerful feelings of pleasure and reinforcement, encouraging repeated use. According to a 2021 study published in Frontiers in Behavioral Neuroscience, opioids rapidly hijack the brain's reward system, making it increasingly difficult for natural rewards like food or social interaction to produce the same pleasure.
-
Development of Tolerance: Over time, the brain adapts to the presence of the drug by reducing its natural dopamine production or receptor sensitivity, leading to tolerance. This means larger or more frequent doses are needed to achieve the same effect. A study by Dumas EO, Pollack GM. et al. 2008, titled "Opioid tolerance development: a pharmacokinetic/pharmacodynamic perspective," shows that tolerance to opioids develops within a few weeks of daily use, dramatically increasing the risk of overdose and addiction. A study in Addiction Science & Clinical Practice by Davis 2015 found that "tolerance and dependence develop in over 60% of chronic opioid users."
-
Onset of Dependence: With continued use, the brain and body become so accustomed to the presence of the medication that normal function is impaired without it, resulting in dependence. Individuals experience withdrawal symptoms when the drug is not taken, reinforcing the cycle of use. Benzodiazepine use for as little as three to six weeks, even when taken strictly at therapeutic doses, has been associated with the development of physical dependence. According to a study by Petursson H. and Lader M.H. (1981), titled "Withdrawal from long-term benzodiazepine treatment," between 15% and 44% of chronic benzodiazepine users experience protracted, moderate to severe withdrawal symptoms upon cessation, including the emergence of anxiety and depressive symptoms.
-
Psychological Reinforcement and Craving: Beyond biological changes, psychological factors also contribute to addiction. Individuals start to misuse prescription drugs to cope with stress, trauma, or mental health issues, further entrenching addictive behavior. Research from the Journal of Substance Abuse Treatment emphasizes how stimulants like Adderall® increase dopamine in brain areas responsible for motivation and habit formation, making emotional and behavioral cravings particularly strong.
What Are the Key Causes of Prescription Drug Addiction?
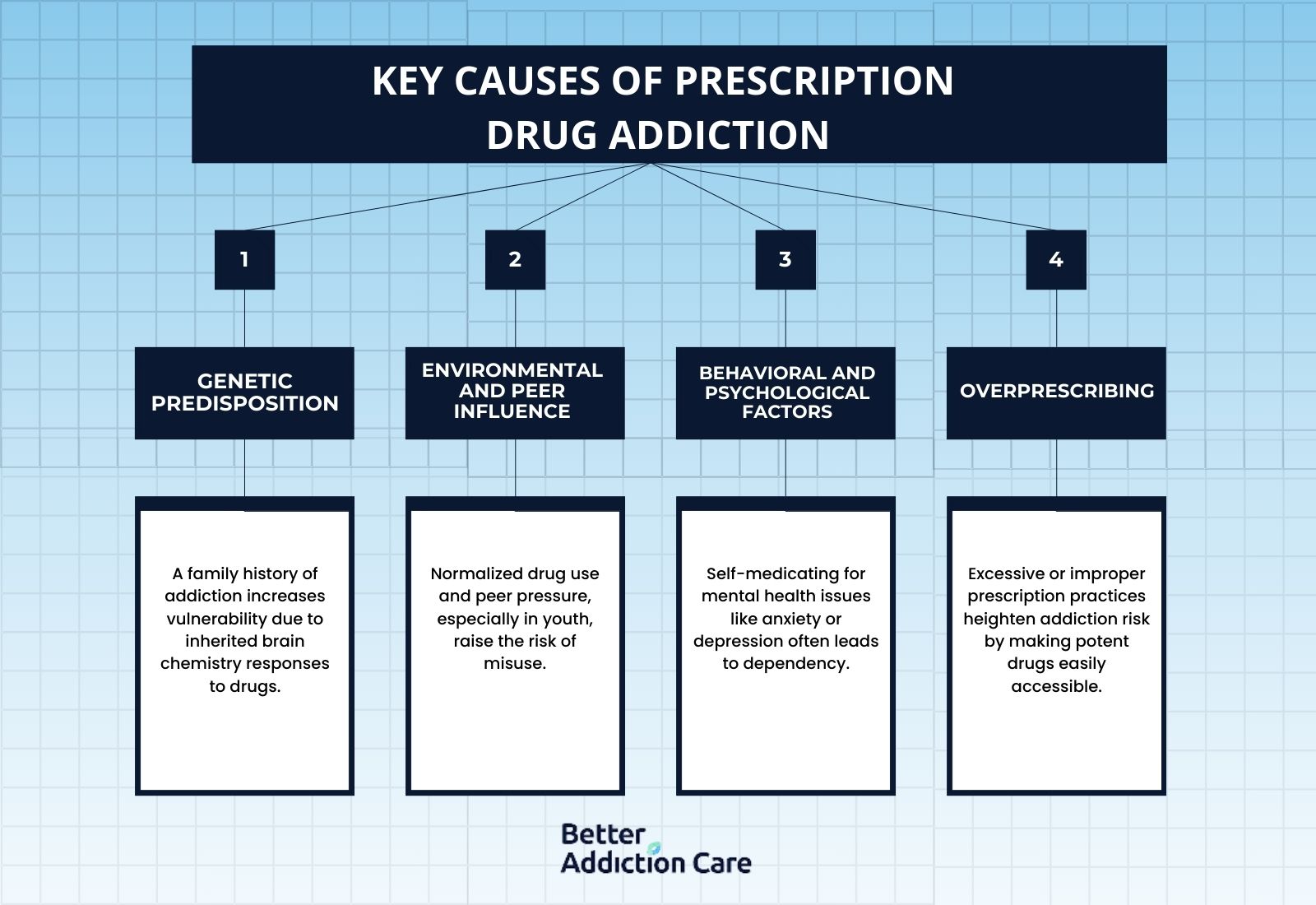
The key causes of prescription drug addiction are genetic vulnerability, environmental influences, behavioral factors, and medical practices such as overprescribing. Addiction results from a complex interplay of these factors, where both biological susceptibility and life experiences shape an individual's risk.
The key causes of prescription drug addiction are as follows:
-
Genetic Predisposition: Genetics plays a significant role in determining an individual's susceptibility to prescription drug addiction. According to the "Genetic Influence on Addiction" by the National Institute on Drug Abuse (NIDA, 2016), people with a family history of substance use disorders are at a much higher risk of developing dependence themselves. Genetic factors influence how the brain's reward pathways respond to drugs, making some individuals more vulnerable to the reinforcing effects of opioids, benzodiazepines, and stimulants.
-
Environmental Factors and Peer Influence: Social environments heavily influence the likelihood of prescription drug misuse. Exposure to environments where drug use is normalized, peer influence encourages misuse, and high levels of stress or trauma all increase the risk. Adolescents and young adults are particularly susceptible to peer-driven misuse, as highlighted by numerous behavioral studies in addiction science.
-
Behavioral and Psychological Factors: Certain behavioral patterns, such as using substances to cope with anxiety, depression, or stress, also contribute to the risk of developing an addiction. Individuals with untreated mental health disorders are significantly more likely to misuse prescription drugs as a form of self-medication, according to data from the Substance Abuse and Mental Health Services Administration (SAMHSA).
-
Prescription Practices and Overprescribing: Medical practices significantly impact addiction development. Overprescribing of opioids, benzodiazepines, and stimulants has been directly linked to rising addiction rates. A landmark study in The New England Journal of Medicine found that patients exposed to longer and higher-dose opioid prescriptions after surgeries had a substantially increased risk of long-term use and addiction. Inappropriate or excessive prescribing practices create easy access to high-risk medications, setting the stage for misuse and eventual dependence.
What Are the Risk Factors That Increase The Chances of Prescription Drug Addiction?
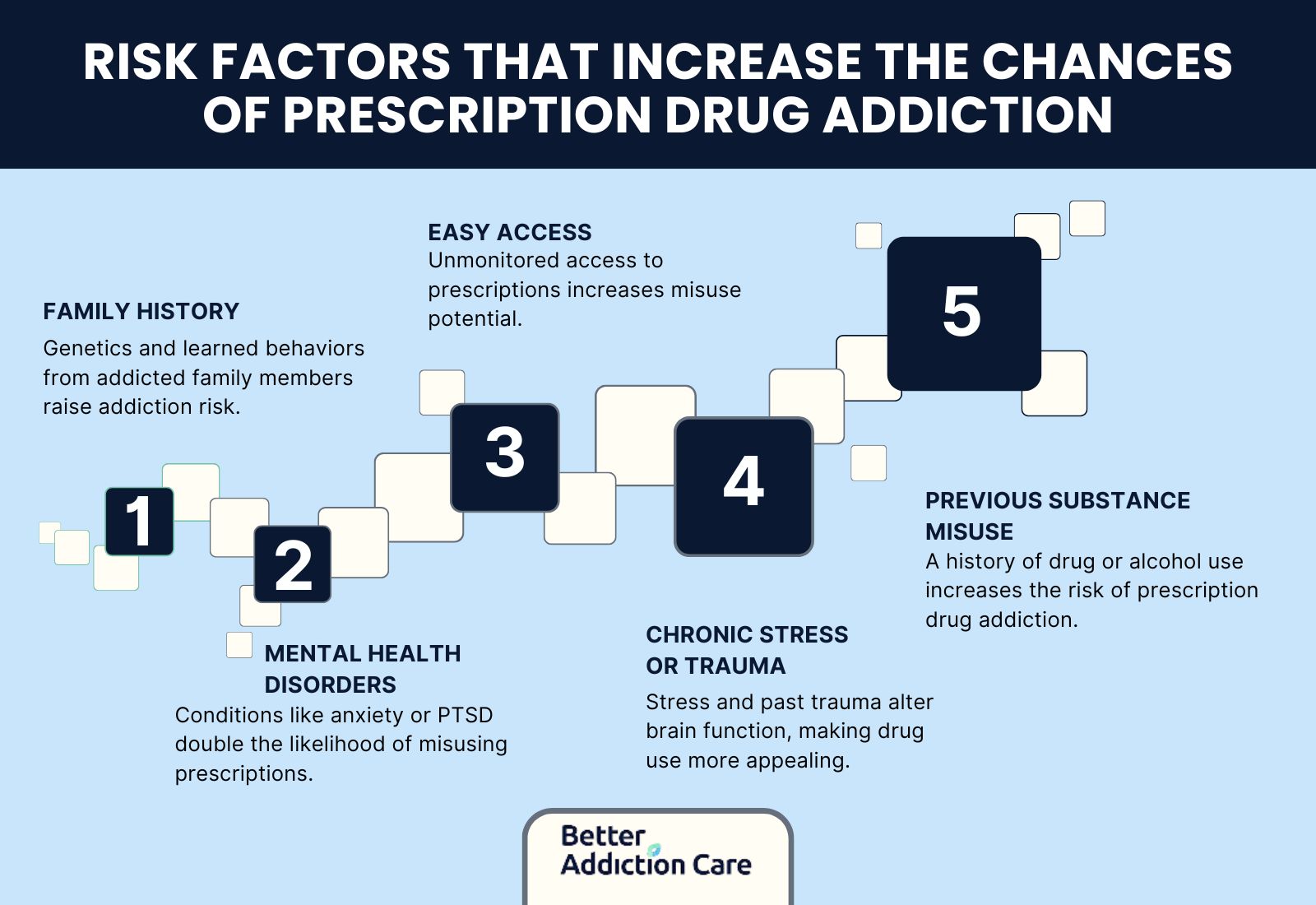
The risk factors that increase the chances of prescription drug addiction are genetic susceptibility, mental health comorbidities, chronic exposure to prescription medications, and environmental stressors. Individuals with overlapping vulnerabilities face a significantly higher risk, and national studies have confirmed that these factors interact to create complex pathways toward addiction.
The risk factors that increase the chances of prescription drug addiction are as follows:
-
Family History of Substance Use Disorders: A strong family history of addiction greatly increases the risk of prescription drug misuse. According to data from the Centers for Disease Control and Prevention (CDC), individuals with immediate family members who have struggled with substance abuse are more likely to develop addictive patterns themselves, due to both genetic and behavioral influences.
-
Presence of Mental Health Conditions (Comorbidities): Mental health comorbidities such as anxiety, depression, post-traumatic stress disorder (PTSD), and bipolar disorder elevate the risk of prescription drug addiction. Research published in NIDA indicates that individuals with mood or anxiety disorders are twice as likely to misuse prescription medications compared to those without psychiatric conditions.
-
Easy Access to Prescription Medications: Having frequent or unsupervised access to prescription drugs, whether through personal prescriptions, family members, or social circles, is a significant risk factor.
-
Chronic Stress and Trauma: Experiencing chronic stress, adverse childhood experiences (ACEs), or trauma increases vulnerability to addiction. Stress-related changes in brain chemistry heighten the appeal of prescription drugs as coping mechanisms, as noted in a study by the Center for Substance Abuse Treatment (US), titled "Trauma-Informed Care in Behavioral Health Services," on the biological impact of trauma and addiction pathways.
-
History of Substance Misuse: Individuals who have previously misused alcohol, tobacco, or illicit drugs are at higher risk of prescription drug addiction. Patterns of earlier substance misuse suggest underlying behavioral tendencies toward compulsive drug-seeking, making prescription drugs another accessible outlet.
What Are the Signs and Symptoms of Prescription Drug Addiction?
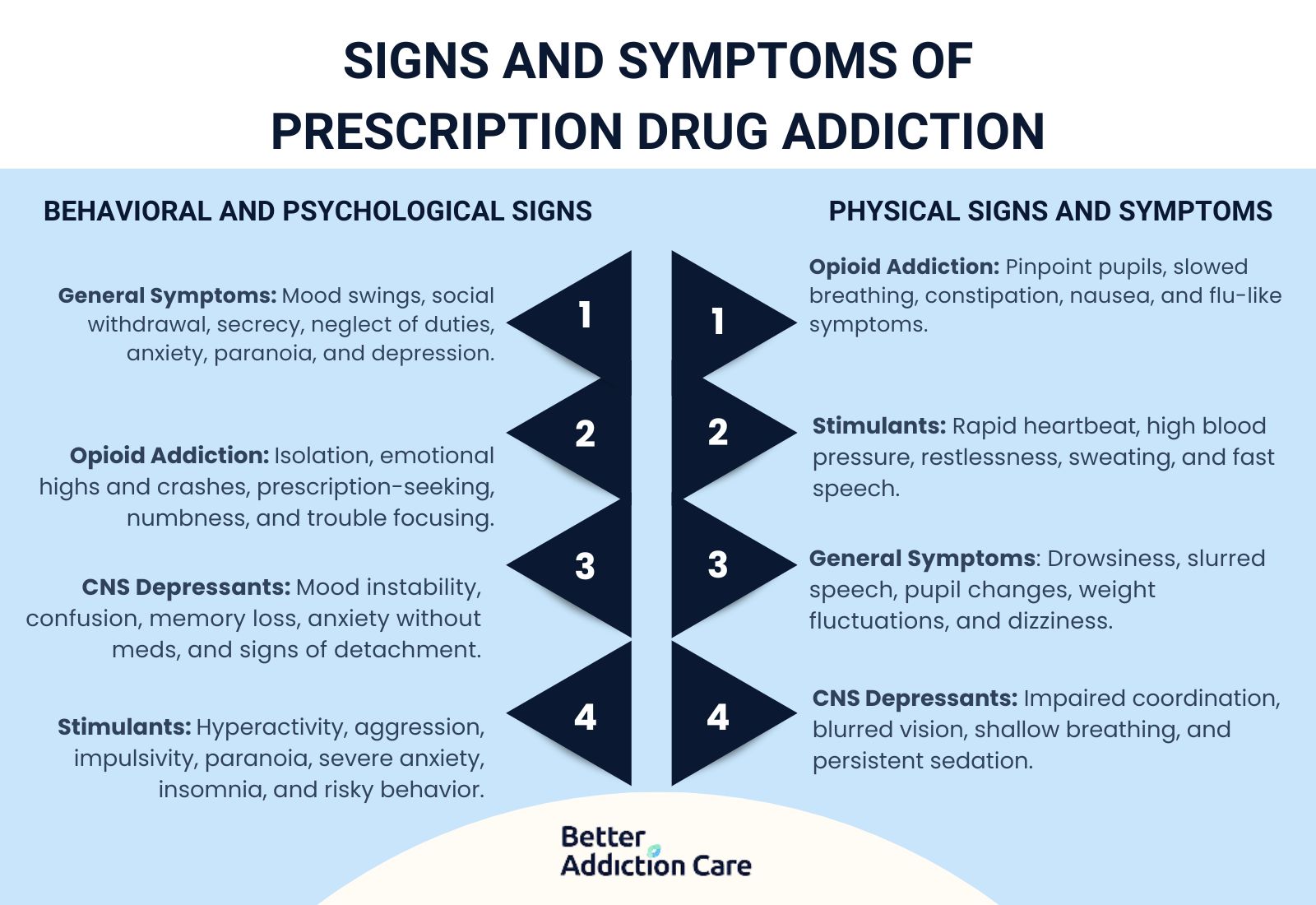
The signs and symptoms of prescription drug addiction are persistent drowsiness, slowed or slurred speech, constricted or dilated pupils, frequent mood swings, withdrawal from social activities, sudden secrecy, and neglect of responsibilities. These symptoms vary significantly depending on the type of medication being misused. Whether it involves opioids, central nervous system (CNS) depressants, or stimulants, each class of drug produces distinct physical and psychological effects. Early identification of these symptoms greatly improves the chances of timely intervention and successful treatment.
Physical Signs and Symptoms of Prescription Drug Addiction
Physical signs of prescription drug addiction manifest differently based on the substance being misused, but all forms of addiction cause noticeable changes in bodily functions and appearance. Individuals exhibit declining health, impaired coordination, or changes in sleep patterns. Spotting these physical indicators early helps friends, family, and healthcare providers intervene before the addiction deepens.
The common physical signs and symptoms of prescription drug addiction include:
-
General Physical Symptoms: Persistent drowsiness, slowed or slurred speech, constricted or dilated pupils, unexplained weight changes, and frequent dizziness are general physical symptoms seen across various types of prescription drug addiction, as studied by the Cleveland Clinic.
-
Opioid Addiction Physical Symptoms: Misuse of opioids such as oxycodone and hydrocodone leads to noticeable drowsiness, slowed breathing, constipation, and nausea. Individuals also show pinpoint pupils and frequent complaints of flu-like symptoms. According to a study by Fox LM, Hoffman RS, Vlahov D, Manini AF. et al. (2018) titled "Risk factors for severe respiratory depression from prescription opioid overdose," out of 307 patients studied, 109 (35.5%) suffered severe respiratory depression (SRD), with SRD rates highest for fentanyl users (83.3%) and lowest for codeine users (3.6%).
-
CNS Depressants (Benzodiazepines, Tranquilizers) Physical Symptoms: Addiction to CNS depressants like benzodiazepines results in impaired motor coordination, slowed reflexes, blurred vision, and shallow breathing. Chronic users experience persistent lethargy and noticeable sedation. According to a study in the Journal of Respiratory Medicine by Johnson, 2016, opioid-induced respiratory depression occurs in 50 to 70% of patients who overdose on these medications.
-
Stimulant Addiction Physical Symptoms: People addicted to stimulants display increased heart rate, high blood pressure, decreased appetite, and excessive sweating. Symptoms like twitching, restlessness, and rapid speech are particularly associated with stimulant misuse.
Behavioral and Psychological Signs of Prescription Drug Addiction
Behavioral and psychological symptoms of prescription drug addiction are just as revealing as physical changes. A person's mood, priorities, and social behaviors shift drastically under the influence of addiction. Recognizing these changes, such as rising irritability, increasing anxiety, or sudden isolation, is important for timely support and intervention.
The common behavioral and psychological signs and symptoms of prescription drug addiction include:
-
General Behavioral and Psychological Symptoms: Frequent mood swings, withdrawal from social activities, sudden secrecy, neglect of responsibilities, and dramatic changes in social circles are typical behavioral warning signs. Psychological symptoms include heightened anxiety, paranoia, and depressive episodes. According to a study in the American Journal of Psychiatry written by Harrison, 2019, paranoia and psychosis occur in 20 to 40% of chronic stimulant users.
-
Opioid Addiction Behavioral and Psychological Symptoms: Opioid misuse causes individuals to isolate themselves, display unusual euphoria followed by severe depression, and show desperation for obtaining prescriptions or drugs. Emotional numbness and difficulty concentrating are also common.
-
CNS Depressants Addiction Behavioral and Psychological Symptoms: Addiction to CNS depressants results in pronounced mood swings, persistent irritability, confusion, and memory problems, as studied by Medical News Today. Users appear detached, indifferent to previously important activities, or overly anxious without their medication. A study by Adams, 2017, published in the Journal of Substance Abuse Treatment, reported that suicidal ideation is present in 10 to 20% of individuals with severe prescription drug addiction.
-
Stimulant Addiction Behavioral and Psychological Symptoms: Individuals addicted to stimulants show hyperactivity, aggression, impulsive behavior, and paranoia. According to Lumen Learning, prolonged stimulant misuse leads to severe anxiety disorders, insomnia, and a tendency toward risky or erratic behavior. A study in the Journal of Clinical Psychiatry, written by Garcia, 2017, found that cognitive impairment occurs in 30 to 50% of individuals with long-term prescription drug addiction.
What Are the Effects of Prescription Drug Addiction?
The effects of prescription drug addiction are euphoria, sedation, dizziness, and significant damage to the brain and body. These wide-ranging effects seriously impact physical health, mental well-being, and social stability. Short-term effects include immediate changes in mood, perception, and behavior, while long-term misuse causes irreversible health damage and increased mortality. Beyond individual consequences, prescription drug addiction also deeply affects families, workplaces, and communities.
Immediate Effects of Prescription Drug Abuse
The immediate effects of prescription drug abuse vary depending on the type of drug used, but they include rapid changes in mood, impaired thinking, and dangerous physical symptoms. These short-term effects increase the risk of accidents, risky behaviors, and acute health crises.
The immediate effects of prescription drug abuse include:
-
Euphoria and sedation: Opioids like oxycodone and hydrocodone cause an intense sense of pleasure followed by drowsiness, impairing judgment and reaction times, as studied by Kosten TR, George TP et al. 2002, titled "The neurobiology of opioid dependence: implications for treatment."
-
Dizziness and slowed breathing: CNS depressants, such as benzodiazepines (e.g., diazepam, lorazepam), lead to relaxation, reduced anxiety, and sedation but dangerously slow breathing and heart rates, as studied by WebMD.
-
Increased alertness and risky behavior: Stimulants, including prescription amphetamines like Adderall, cause heightened energy, euphoria, and reduced need for sleep, but also trigger impulsivity, paranoia, and cardiovascular strain, as studied by Medscape in "Amphetamine-Related Psychiatric Disorders."
Long-Term Health Risks of Prescription Drug Addiction
Over time, prescription drug addiction causes significant damage to the body and brain. Chronic use of opioids results in liver damage, hormonal imbalances, and brain changes that alter emotional regulation and pain perception. A review in the American Journal of Gastroenterology by Williams, 2018 noted that "opioid-induced constipation affects up to 40-80% of patients on long-term opioid therapy." Prolonged misuse of CNS depressants is linked to cognitive decline, memory impairment, and persistent anxiety.
Long-term stimulant abuse leads to severe cardiovascular issues such as hypertension, stroke, and heart failure. According to the World Health Organization, 2017, "infections related to needle sharing occur in up to 30% of individuals who inject prescription drugs." Similarly, a study in the Journal of Clinical Psychiatry written by Garcia, 2017, found that "cognitive impairment occurs in 30-50% of individuals with long-term prescription drug addiction."
According to data from the CDC, long-term prescription drug misuse significantly increases the risk of overdose death, with opioids being a leading cause of unintentional injury deaths in the U.S. According to a study by Smith, 2017, published in the Journal of Hepatology, "chronic opioid use lead to liver damage in 20-30% of long-term users."
Effects on Family Life and the Broader Community
Prescription drug addiction has profound emotional, financial, and societal effects on both the individual and their loved ones. Families experience stress, anxiety, and fractured relationships due to the erratic behaviors and emotional instability of an addicted family member. Financially, the cost of supporting someone through addiction is significant, leading to loss of income, depleted savings, and increased healthcare costs.
Prescription drug misuse places a heavy burden on society, with rising healthcare costs, law enforcement expenses, and lost productivity. According to the CDC, the economic cost of prescription opioid misuse alone is estimated at $78.5 billion annually in the U.S., which includes healthcare expenses, lost productivity, and criminal justice costs.
What Are Treatment Options for Prescription Drug Addiction?
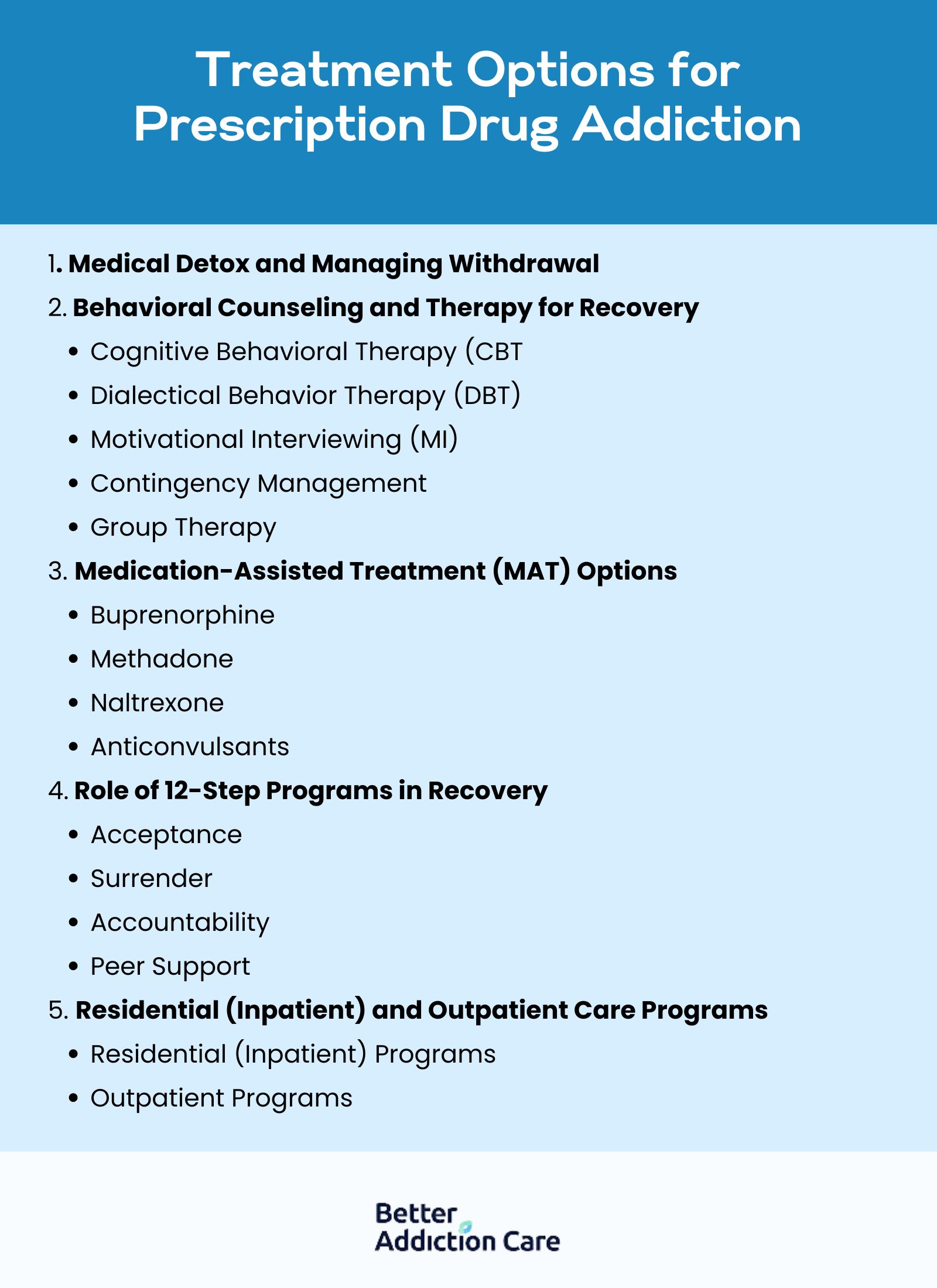
The treatment options for prescription drug addiction are medical detox, behavioral counseling, medication-assisted treatment (MAT), participation in 12-step programs, and residential or outpatient care programs. Successful recovery usually requires a combination of these approaches tailored to the individual's needs to address the physical, psychological, and behavioral aspects of addiction.
The treatment options for prescription drug addiction are as follows:
1. Medical Detox and Managing Withdrawal
Detoxification is the initial phase of addiction treatment, focused on safely removing the drug from the individual's body under medical supervision. Withdrawal symptoms are severe, ranging from nausea and sweating to seizures or hallucinations, depending on the substance misused. Drug detox centers provide round-the-clock medical care to manage these symptoms and minimize health risks, offering a safer and more comfortable start to recovery.
According to "The Importance of Medically Assisted Withdrawal (Detoxification) for Prescription Drug Abuse" by the Substance Abuse and Mental Health Services Administration (SAMHSA, 2019), medically supervised detox is important for safely managing withdrawal symptoms and reducing the risk of complications.
2. Behavioral Counseling and Therapy for Recovery
Behavioral counseling plays an important role in treating prescription drug addiction by helping individuals understand and change the thoughts and behaviors that fuel substance misuse.
The common therapy types include:
-
Cognitive Behavioral Therapy (CBT): Cognitive Behavioral Therapy helps patients recognize and change negative thinking and behavior patterns linked to drug use. It teaches individuals to develop healthier coping mechanisms when facing cravings or triggers. CBT is widely regarded as one of the most effective evidence-based treatments for substance use disorders, helping to prevent relapse through skill-building and self-monitoring. According to the UCLA Addictions Lab, CBT is more effective than no treatment or minimal treatment, with outcomes roughly 15% to 26% better.
-
Dialectical Behavior Therapy (DBT): Dialectical Behavior Therapy focuses on emotional regulation and coping mechanisms, particularly beneficial for individuals with co-occurring mental health disorders. DBT incorporates mindfulness practices that help patients manage intense emotions without resorting to substance use. It is especially effective for those struggling with self-destructive behaviors, promoting stability and emotional resilience during recovery.
-
Motivational Interviewing (MI): Motivational Interviewing strengthens a person's motivation and commitment to change by addressing ambivalence toward quitting drug use. It uses empathetic, non-confrontational dialogue to help individuals articulate their reasons for seeking recovery. MI significantly improves engagement and outcomes when integrated into broader addiction treatment programs.
-
Contingency Management: Contingency Management provides tangible rewards for positive behavior, such as maintaining sobriety, as drug-free urine tests confirm. It uses incentives to reinforce healthy behavior changes, promoting abstinence during the early, most vulnerable stages of recovery. Contingency management strategies enhance treatment retention and short-term abstinence rates.
-
Group Therapy: Group Therapy offers peer support and shared experiences, helping individuals feel less isolated in their recovery journey. It fosters a sense of community, accountability, and hope as members encourage one another to stay committed to sobriety. Group settings also provide opportunities to practice social skills and learn from others' coping strategies and successes.
3. Medication-Assisted Treatment (MAT) Options
Medication-Assisted Treatment (MAT) combines medications with counseling to address both the physical and psychological sides of addiction. MAT helps stabilize brain chemistry, block euphoric effects, relieve physiological cravings, and normalize body functions without the harmful effects of the abused drug.
Examples include:
-
Buprenorphine: Buprenorphine is a partial opioid agonist that reduces cravings and withdrawal symptoms with a lower risk of misuse. It is prescribed by certified physicians and taken at home.
-
Methadone: It is a long-acting opioid agonist used in medication-assisted treatment to reduce cravings and withdrawal symptoms. It is administered in a controlled clinical setting to prevent misuse.
-
Naltrexone: Naltrexone is an opioid antagonist that blocks the effects of opioids, preventing relapse. It is available as an oral medication or a monthly injection.
-
Anticonvulsants: These are medications used to prevent seizures during the withdrawal process from certain drugs. Medications such as carbamazepine or valproate are used to manage withdrawal symptoms and prevent seizures.
4. Role of 12-Step Programs in Recovery
The 12-step model, first developed by Alcoholics Anonymous (AA), remains a cornerstone in addiction recovery, including for prescription drug addiction. It emphasizes peer support, accountability, and spiritual growth. Key principles of the 12-step program include:
-
Acceptance: Recognizing addiction as a chronic, progressive disease.
-
Surrender: Trusting a higher power or the support of the community.
-
Accountability: Taking personal responsibility for past actions and making amends.
-
Peer Support: Participating in meetings through groups like Narcotics Anonymous (NA) to stay connected and encouraged during recovery.
5. Residential (Inpatient) and Outpatient Care Programs
Both residential (inpatient) and outpatient care programs offer structured treatment environments but differ in intensity and flexibility.
-
Residential (Inpatient) Programs: Provide 24/7 care at rehabilitation centers, ideal for individuals with severe addiction or co-occurring disorders. They offer a highly immersive environment away from everyday triggers.
-
Outpatient Programs: Allow individuals to live at home while attending therapy sessions and support groups. Outpatient care is more affordable and flexible, making it suitable for those with milder addictions or strong home support systems.
What Is the Typical Recovery Timeline for Prescription Drug Addiction?
The typical recovery timeline for prescription drug addiction varies depending on the individual's substance use history, the type of drug misused, and personal health factors. Recovery unfolds in several phases, beginning with detoxification, which lasts from a few days to about two weeks, depending on the drug type and severity of dependence. Inpatient rehabilitation programs range from 30 to 90 days, offering structured care and intensive therapy.
Outpatient drug rehab programs extend from several months to over a year, providing ongoing support while individuals reintegrate into daily life. According to the National Institute on Drug Abuse (NIDA), longer treatment durations, specifically programs lasting at least 90 days, are associated with significantly better outcomes. Still, recovery is a lifelong process requiring continuous support and personal commitment.
Is Relapse a Normal Part of Prescription Drug Addiction Recovery?
Yes, relapse is a regular part of prescription drug addiction recovery. Relapse rates for substance use disorders, including prescription drug addiction, are comparable to those of other chronic illnesses such as diabetes and hypertension, with approximately 40% to 60% of individuals experiencing relapse after treatment.
Relapse prevention involves building coping skills, establishing recovery support networks, and engaging in ongoing care such as therapy, medication management, and peer support groups. Recognizing relapse as a potential hurdle rather than a failure encourages individuals to seek immediate support and continue progressing in their long-term recovery journey.
What Are the Strategies to Prevent Prescription Drug Addiction?
The strategies to prevent prescription drug addiction include safe prescribing practices, public education efforts, and encouraging personal responsibility in medication use. Prevention requires a collaborative approach involving healthcare providers, policymakers, families, and individuals to reduce misuse before it begins and promote healthier behaviors.
The strategies to prevent prescription drug addiction are as follows:
-
Safe Prescribing Practices: Healthcare providers play an important role in prevention by following guidelines for prescribing opioids, benzodiazepines, and stimulants. This includes prescribing the lowest effective dose for the shortest necessary duration, using prescription drug monitoring programs (PDMPs), and educating patients about the risks of dependence and misuse.
-
Public Education Campaigns: Widespread education about the dangers of prescription drug misuse helps change public perceptions and reduce stigma. Community initiatives, school programs, and media campaigns increase awareness about how quickly dependence develops and promote safe medication habits.
-
Secure Storage and Proper Disposal: Individuals prevent misuse by securely storing prescription medications away from others, especially children and teens, and properly disposing unused drugs through authorized take-back programs to prevent unauthorized access.
-
Screening and Early Intervention: Regular screening for substance misuse in primary care and mental health settings helps identify at-risk individuals early. Early interventions, such as brief counseling or referral to addiction specialists, prevent misuse from escalating into addiction.
-
Promoting Alternative Pain Management: Encouraging non-opioid pain treatments like physical therapy, acupuncture, or cognitive behavioral therapy for pain management reduces the reliance on addictive prescription drugs and minimizes the risk of developing dependence.
Are Support Resources Available for Prescription Drug Addiction?
Yes, support resources are widely available for individuals struggling with prescription drug addiction, offering both emotional assistance and structured recovery programs. Access to support groups, state initiatives, and community services significantly boosts recovery outcomes by providing peer connection, accountability, and ongoing encouragement.
Examples of available support resources include:
-
Narcotics Anonymous (NA): NA is a global, peer-led support group that follows the 12-step model, welcoming individuals recovering from all types of drug addiction, including prescription drugs. According to NA World Services, over 70,000 weekly meetings are held worldwide.
-
State-Sponsored Programs: Many states offer substance abuse helplines, treatment locators, and recovery programs. For example, North Carolina's Department of Health and Human Services provides resources through the Alcohol/Drug Council of North Carolina at 1-800-688-4232.
-
SAMHSA's National Helpline: The Substance Abuse and Mental Health Services Administration (SAMHSA) offers a confidential, 24/7 helpline (1-800-662-HELP) that connects callers to local treatment and support services.
-
Prescription Drug Abuse Support Groups: Some communities offer specialized support groups focused specifically on prescription medication addiction, hosted at local rehab centers or hospitals.
-
Online Recovery Communities: Websites like SMART Recovery offer virtual meetings and resources for individuals seeking a science-based alternative to traditional 12-step groups, with options tailored for prescription drug recovery.
What Are the Ways to Support a Loved One Struggling with Prescription Drug Addiction?
The ways to support a loved one struggling with prescription drug addiction include offering emotional encouragement, setting healthy boundaries, and helping them access professional treatment. Compassionate support, clear communication, and timely intervention make an important difference in their recovery journey.
The ways to support a loved one struggling with prescription drug addiction are as follows:
-
Plan a Thoughtful Intervention: Organizing a carefully planned intervention helps your loved one recognize the impact of their addiction. This approach, guided by a professional, creates a structured and nonjudgmental environment to encourage them to seek help.
-
Communicate with Compassion and Honesty: Open, honest conversations grounded in compassionate support help reduce feelings of shame and defensiveness. Express concern using "I" statements, emphasizing your care rather than blame.
-
Educate Yourself About Prescription Drug Addiction: Learning about the nature of addiction and the specific challenges related to prescription drug misuse helps you better understand your loved one's behavior and the complexity of their struggle.
-
Encourage Professional Treatment: Supporting your loved one in finding qualified addiction treatment services, such as detox programs, therapy, or outpatient rehab, is instrumental. Offer to help with research, attend consultations, or assist with logistics if needed.
-
Set Healthy Boundaries: Establishing and maintaining clear, healthy boundaries protects both you and your loved one. It reinforces accountability while preventing enabling behaviors that could worsen their addiction.
-
Participate in Family Therapy or Support Groups: Joining family-focused therapy sessions or groups like Al-Anon provides you with coping strategies and emotional support. These environments also help families rebuild trust and communication strained by addiction.
Where to Find Prescription Drug Addiction Treatment?
Finding prescription drug addiction treatment involves reaching out to specialized rehabilitation centers, hospitals, outpatient clinics, or community-based programs. Many reputable facilities offer medical detox, behavioral therapy, medication-assisted treatment, and long-term recovery support tailored to individual needs. Resources like SAMHSA's National Helpline (1-800-662-HELP) or online treatment center locators assist in locating local treatment options. Primary care providers and mental health professionals also provide referrals to trusted addiction specialists.
Does Insurance Cover Prescription Drug Addiction Treatment?
Insurance covers prescription drug addiction treatment, including services like detox, therapy, medication-assisted treatment (MAT), and outpatient or inpatient rehab programs. Under the Affordable Care Act (ACA), substance use disorder services are considered essential health benefits, meaning most private insurance plans, Medicaid, and Medicare offer some level of coverage. However, the extent of coverage varies depending on the provider and specific plan, so it's important to verify benefits directly with the insurance company or the treatment facility's admissions team.
Do All Prescription Drug Addictions Require Inpatient Rehab?
No, not all prescription drug addictions require inpatient rehab. The decision depends on the severity of the addiction, the presence of co-occurring mental health conditions, and the individual's environment and support system. Some people succeed with outpatient care, especially if their addiction is identified early and they have strong external support.
Can You Detox from Prescription Drugs at Home Safely?
Yes, you can detox from prescription drugs at home, but it is not considered safe, especially for substances like opioids, benzodiazepines, and stimulants, which cause severe withdrawal symptoms. Medical supervision during detox is significant to manage health risks, prevent complications, and increase the likelihood of a successful transition into recovery.
What Happens After Completing Prescription Drug Addiction Treatment?
After completing prescription drug addiction treatment, individuals continue with aftercare plans that include outpatient therapy, 12-step programs, relapse prevention strategies, and ongoing medical support. Building a strong support network, maintaining healthy habits, and staying connected with recovery communities are important steps in sustaining long-term sobriety.





