Psychiatric Rehabilitation: Definition, Benefits, History, Theory, Principles, Process
Psychiatric rehabilitation helps individuals with severe mental health conditions regain independence, develop coping skills, and reintegrate into society. Psychiatric rehabilitation focuses on improving emotional, social, and vocational functioning through structured interventions, combining therapy, medication management, and life skills training to enhance overall well-being.
Psychiatric rehabilitation helps individuals with severe mental health conditions regain independence, develop coping skills, and reintegrate into society. Psychiatric rehabilitation focuses on improving emotional, social, and vocational functioning through structured interventions, combining therapy, medication management, and life skills training to enhance overall well-being.
According to a study by Dalton-Locke C, Marston L, McPherson P, Killaspy H., et al. 2021, titled “The Effectiveness of Mental Health Rehabilitation Services: A Systematic Review and Narrative Synthesis,” the success rate of psychiatric rehabilitation varies by program type, with studies showing 50% to 74% of patients achieving stable housing, avoiding rehospitalization, or maintaining community placement within follow-up periods of one to five years.
The benefits of psychiatric rehabilitation include improved daily functioning, enhanced social skills, and increased self-sufficiency. By promoting recovery-oriented care, it helps reduce hospitalizations, strengthen coping strategies, and support independent living. A study by Physiopedia titled “Mental Health Issues and Rehabilitation” shows that individuals who engage in rehabilitation experience better employment outcomes, stronger relationships, and improved quality of life.
The history of psychiatric rehabilitation dates back to the deinstitutionalization movement of the mid-20th century, shifting care from asylums to community-based settings. Over time, advances in therapy, medication, and psychosocial support systems have shaped modern rehabilitation programs, emphasizing recovery, empowerment, and person-centered care.
The theories behind psychiatric rehabilitation are grounded in the belief that recovery is possible with the right support. It integrates psychological, social, and medical models, including cognitive-behavioral approaches and recovery-oriented frameworks, to help individuals build resilience, manage symptoms, and achieve meaningful life goals.
The principles of psychiatric rehabilitation emphasize person-centered care, empowerment, and community integration. Programs focus on strengths-based approaches, shared decision-making, and cultural relevance, ensuring that treatment is individualized, holistic, and responsive to each person’s unique recovery journey.
The process of psychiatric rehabilitation involves comprehensive assessment, symptom stabilization, skill development, and ongoing support. It includes therapy, vocational training, medication management, and coordination with healthcare providers to help individuals achieve long-term stability and reintegrate into their communities.
What Is Psychiatric Rehabilitation?
Psychiatric rehabilitation, also known as psychosocial rehabilitation, is a therapeutic approach aimed at assisting individuals with mental health conditions in restoring their functional abilities and enhancing their quality of life. This process focuses on helping individuals develop the necessary skills and support to live independently and participate meaningfully in their communities.
The rehabilitation process encompasses a variety of services tailored to meet the unique needs of each individual. These services include medication management, independent living, social skills training, psychological support for clients and their families, housing assistance, vocational rehabilitation and employment support, social network enhancement, and access to leisure activities. The goal is to address both the clinical and personal recovery needs of individuals, promoting social inclusion and empowerment.
Statistics by Killaspy H, Dalton-Locke C., et al. 2023, titled “The growing evidence for mental health rehabilitation services and directions for future research,” indicate that up to 20% of individuals newly diagnosed with psychosis develop complex problems requiring rehabilitation services. On average, individuals referred for rehabilitation have been engaged with mental health services for over 13 years and have experienced multiple admissions.
Is Psychiatric Rehabilitation Offered in Inpatient or Outpatient Settings?
Yes, psychiatric rehabilitation is offered in both inpatient and outpatient settings, depending on the severity of the individual’s condition, level of functional impairment, and required support. Inpatient rehabilitation is provided for individuals with severe mental health conditions who need intensive, 24-hour care in a structured environment, such as those recovering from acute psychiatric episodes or those with complex, long-term disorders. Outpatient rehabilitation, on the other hand, is designed for individuals who live in the community but still need ongoing support through therapy, vocational training, and social skills development.
The choice between inpatient and outpatient rehabilitation is determined by several factors, including the individual’s psychiatric diagnosis, level of independence, risk of relapse, availability of family or community support, and response to previous treatments. Those with high-risk conditions, severe functional impairments, or inadequate social support are more likely to require inpatient care, whereas individuals with stable conditions and strong support networks benefit from outpatient programs that allow them to maintain daily responsibilities while receiving treatment.
What Types of Professionals Provide Psychiatric Rehabilitation Services?
Types of professionals that provide psychiatric rehabilitation services include psychiatrists, clinical psychologists, licensed therapists, psychiatric nurses, and case managers, among others. These professionals work together to help individuals with mental health conditions regain independence, improve social functioning, and enhance their overall well-being through personalized rehabilitation programs. Their roles vary from medical treatment and therapy to skill development, case management, and community support.
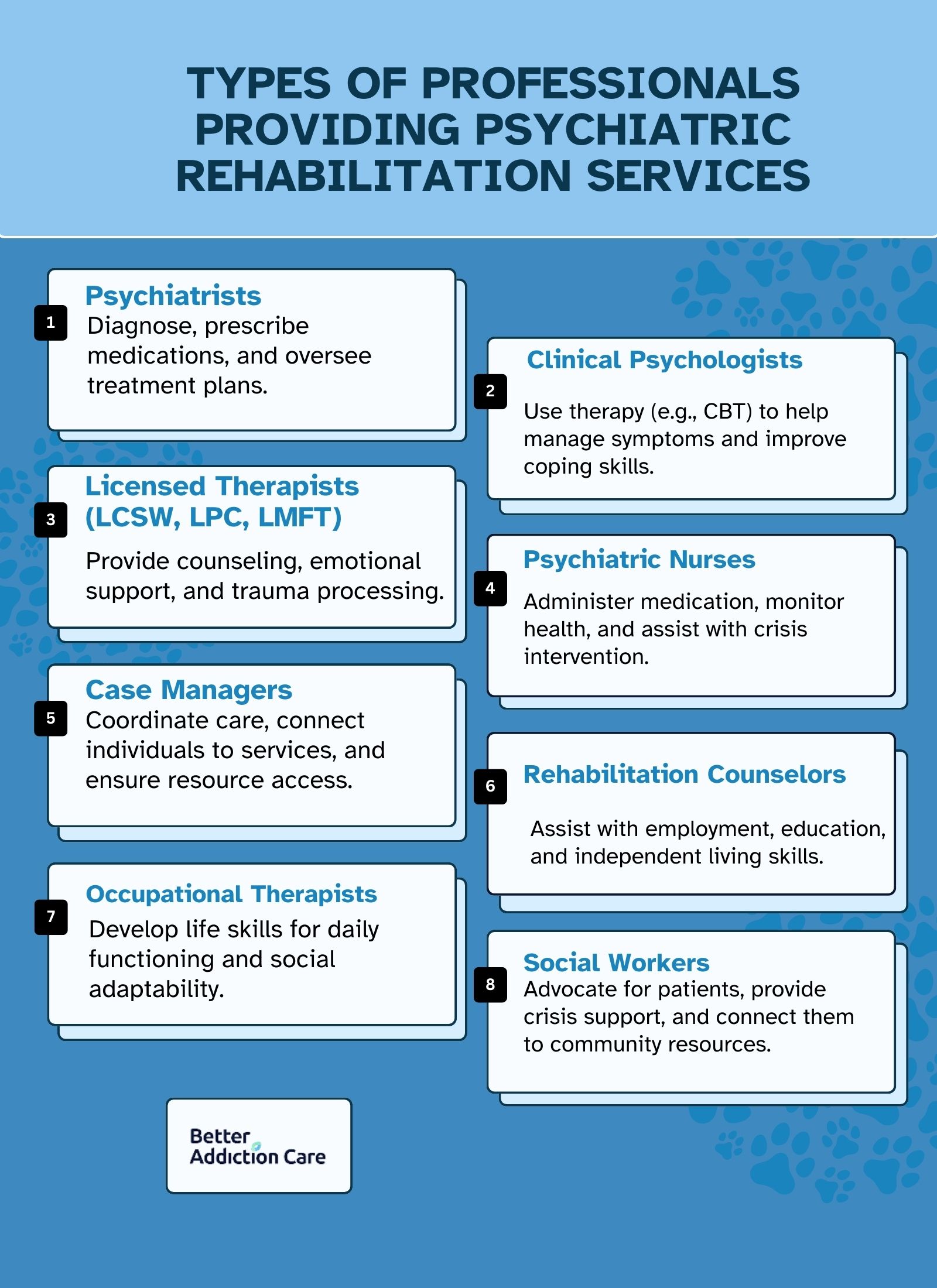
The following types of professionals provide psychiatric rehabilitation services:
-
Psychiatrists: Psychiatrists are medical doctors who specialize in mental health and diagnose and treat psychiatric disorders. They prescribe medications, monitor treatment progress, and oversee rehabilitation plans, ensuring individuals receive appropriate psychiatric care tailored to their needs.
-
Clinical Psychologists: Clinical psychologists assess, diagnose, and provide therapy for individuals with mental health conditions. They use evidence-based psychological interventions such as cognitive-behavioral therapy (CBT) to help individuals manage symptoms and develop coping strategies for independent living.
-
Licensed Therapists (LCSW, LPC, LMFT): Licensed therapists, including Licensed Clinical Social Workers (LCSW), Licensed Professional Counselors (LPC), and Licensed Marriage and Family Therapists (LMFT), offer psychotherapy, counseling, and emotional support. They help individuals process trauma, develop problem-solving skills, and improve relationships.
-
Psychiatric Nurses: Psychiatric nurses provide medical and emotional support to rehabilitation individuals. They administer medications, monitor mental and physical health, educate patients on self-care, and assist in crisis intervention to stabilize symptoms and promote recovery.
-
Case Managers: Case managers coordinate psychiatric rehabilitation services by connecting individuals to healthcare providers, community programs, and social support systems. They assess needs, develop treatment plans, and ensure individuals receive the necessary resources to reintegrate into society.
-
Rehabilitation Counselors: Rehabilitation counselors assist individuals with mental health conditions develop skills for employment, education, and independent living. They provide vocational training, job placement support, and career counseling to improve long-term success.
-
Occupational Therapists: Occupational therapists help individuals develop vital life skills, such as self-care, time management, and social interaction. They create personalized strategies to improve daily functioning and adaptability in various environments.
-
Social Workers: Social workers advocate for individuals with mental health conditions by providing support services, connecting them with housing, employment, and community resources, and assisting with crisis management. They play a key role in long-term rehabilitation and social integration.
What Are the Benefits of Psychiatric Rehabilitation?
The benefits of psychiatric rehabilitation include improved daily functioning, enhanced social skills, and increased self-esteem. This rehabilitation approach helps individuals with mental health conditions regain control over their lives, integrate into society, and work toward long-term recovery. Psychiatric rehabilitation promotes independence and overall well-being through structured therapy, skill-building, and community support.
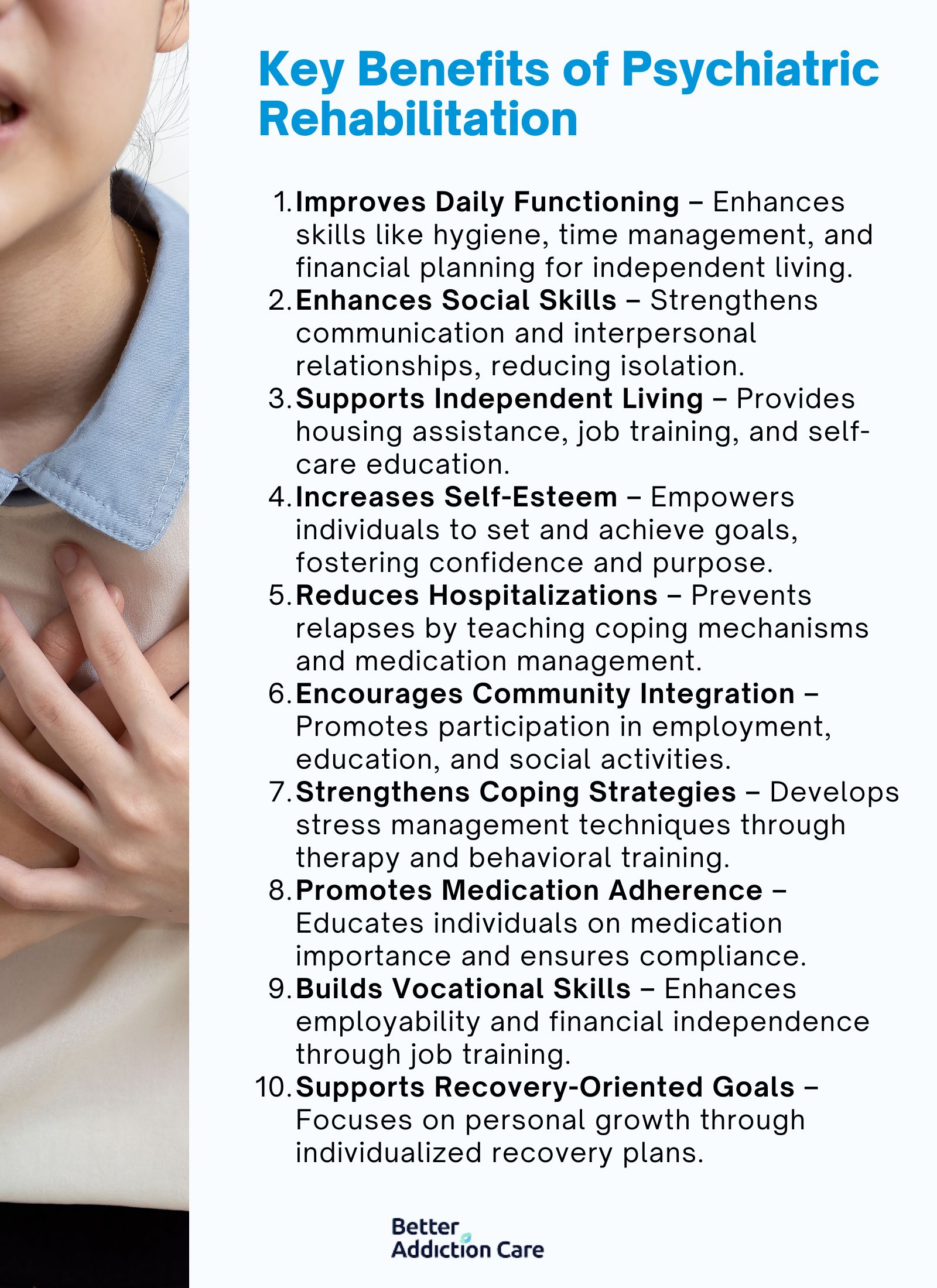
The benefits of psychiatric rehabilitation are as follows:
-
Improves Daily Functioning: Psychiatric rehabilitation helps individuals develop critical life skills, such as personal hygiene, time management, and financial planning, to maintain a stable and productive lifestyle. According to a study by Pratt CW et al. 2014, titled “Psychiatric Rehabilitation: Third Edition,” addressing cognitive and functional impairments enables individuals to manage daily tasks independently, reducing their reliance on caregivers.
-
Enhances Social Skills: Many individuals with mental health conditions struggle with communication and interpersonal relationships. Psychiatric rehabilitation provides structured training in social skills, improving interactions with family, friends, and coworkers. According to a study by Farkas M et al. 2016, titled "Person-Centered Psychiatric Rehabilitation," psychiatric rehabilitation facilitates better relationships and reduces isolation, which is necessary for mental well-being.
-
Supports Independent Living: Psychiatric rehabilitation programs focus on helping individuals live autonomously by offering housing assistance, job training, and self-care education. This promotes confidence and self-sufficiency, allowing individuals to reintegrate into society with minimal external support, as the World Health Organization studied.
-
Increases Self-Esteem: By empowering individuals to set and achieve personal goals, psychiatric rehabilitation improves self-worth and confidence. Engaging in meaningful activities, such as employment or volunteer work, contributes to a sense of purpose and achievement, which plays an integral role in recovery.
-
Reduces Hospitalizations: Psychiatric rehabilitation decreases the likelihood of psychiatric hospital admissions by providing ongoing support and intervention. By teaching coping mechanisms and medication management, these programs help individuals maintain stability and prevent relapses.
-
Encourages Community Integration: Many people with psychiatric conditions experience social exclusion. Rehabilitation programs facilitate participation in community activities, employment, and education, allowing individuals to rebuild social connections and lead fulfilling lives, according to a study by Tiu MMH et al. 2020, titled “Experience of Drug Abusers Participating in Community-Based Drug Rehabilitation Services Provided by the Counselling Centres for Psychotropic Substance Abusers (CCPSAs) in Hong Kong.”
-
Strengthens Coping Strategies: Psychiatric rehabilitation teaches individuals how to handle stress, anxiety, and other mental health challenges through therapy, mindfulness, and behavioral techniques. Strengthening coping skills enhances resilience and reduces the impact of psychiatric symptoms.
-
Promotes Medication Adherence: One of the major challenges in psychiatric treatment is medication non-compliance. Rehabilitation programs provide education on the importance of medication, monitor adherence, and address side effects, ensuring that individuals remain on their prescribed treatment plans.
-
Builds Vocational Skills: Workplace training and job placement services are key components of psychiatric rehabilitation. These programs improve employability and financial independence by equipping individuals with vocational skills, contributing to overall mental stability.
-
Supports Recovery-Oriented Goals: Psychiatric rehabilitation is centered on personalized recovery goals, whether they involve employment, education, or relationships. By focusing on an individual’s strengths and aspirations, these programs foster long-term personal growth and sustained mental health improvement.
What Are the Psychiatric Disorders Treated in Psychiatric Rehab?
The psychiatric disorders that are treated in psychiatric rehab include schizophrenia, bipolar disorder, major depressive disorder, and co-occurring substance use disorders, among others. These conditions require long-term management, and psychiatric rehabilitation provides structured therapy, skill-building, and community support to help individuals achieve stability and improve their quality of life. By focusing on recovery-oriented care, psychiatric rehab helps patients reintegrate into society and lead independent, fulfilling lives.
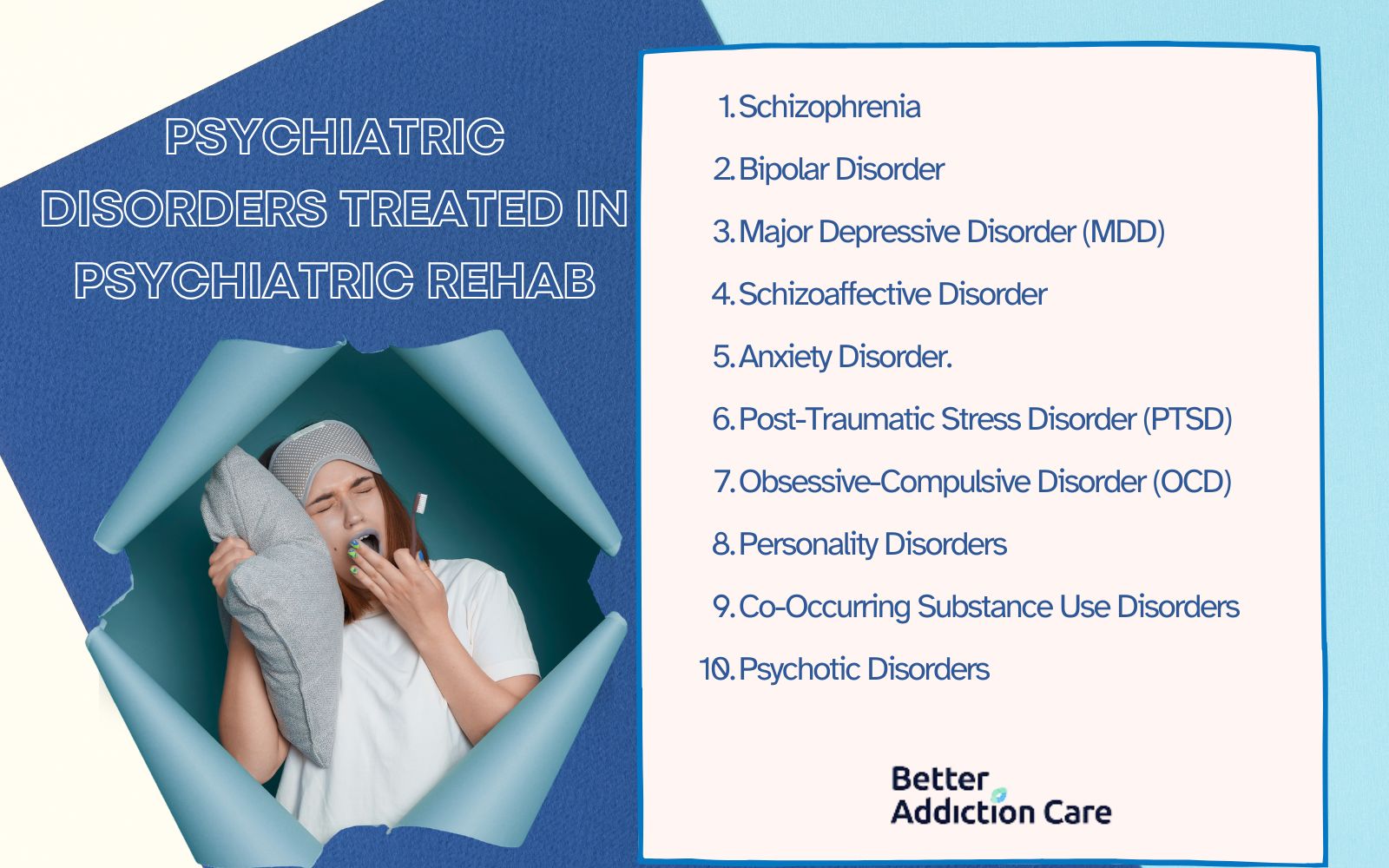
The following psychiatric disorders are treated in psychiatric rehab:
-
Schizophrenia: Schizophrenia is a chronic mental disorder characterized by hallucinations, delusions, disorganized thinking, and impaired social functioning. It affects approximately 0.32% of the global population, according to the World Health Organization (WHO). Psychiatric rehabilitation helps individuals with schizophrenia develop coping mechanisms, adhere to medication, and improve daily functioning through structured programs.
-
Bipolar Disorder: Bipolar disorder causes extreme mood swings, ranging from depressive episodes to manic highs. It affects about 2.4% of the population worldwide, according to a study by Bonnín CDM, Reinares M, Martínez-Arán A, et al. 2019, titled “Improving Functioning, Quality of Life, and Well-being in Patients with Bipolar Disorder.” Psychiatric rehab assists individuals in managing mood stability, developing routines, and engaging in vocational training to enhance their ability to function in society.
-
Major Depressive Disorder (MDD): MDD is a severe form of depression that impacts mood, behavior, and physical health. It affects approximately 5% of adults globally, according to the World Health Organization (WHO). Psychiatric rehab provides structured therapy, medication management, and lifestyle interventions to help individuals regain motivation and restore daily functioning.
-
Schizoaffective Disorder: This condition combines symptoms of schizophrenia and mood disorders (either bipolar or depressive types). It is relatively rare, affecting about 0.3% of the population, as reported by the National Alliance on Mental Illness (NAMI). Psychiatric rehabilitation helps individuals manage both psychotic and mood symptoms, ensuring stability through therapy, medication, and skill-building programs.
-
Anxiety Disorders: Anxiety disorders, including generalized anxiety disorder (GAD), panic disorder, and social anxiety, are among the most common psychiatric conditions, affecting about 31% of adults at some point in their lives, according to the National Institute of Mental Health (NIMH). Psychiatric rehabilitation programs teach stress management techniques, cognitive-behavioral strategies, and exposure therapy to help individuals regain control over their anxiety.
-
Post-Traumatic Stress Disorder (PTSD): PTSD develops after exposure to traumatic events and affects about 3.9% of people worldwide, as studied by Koenen KC et al. 2017, titled “Posttraumatic stress disorder in the World Mental Health Surveys.” Symptoms include flashbacks, hypervigilance, and emotional numbness. Psychiatric rehab provides trauma-focused therapy, coping skills training, and community support to help individuals process their experiences and improve emotional regulation.
-
Obsessive-Compulsive Disorder (OCD): OCD is a disorder marked by persistent, intrusive thoughts (obsessions) and repetitive behaviors (compulsions). It affects around 1.2% of U.S. adults annually, according to the American Psychiatric Association. Rehabilitation programs use cognitive-behavioral therapy (CBT) and exposure-response prevention (ERP) to help individuals manage compulsions and reduce distress.
-
Personality Disorders: Personality disorders, such as borderline personality disorder (BPD) and antisocial personality disorder, affect emotional regulation, relationships, and self-image. BPD alone affects about 1.6% of the population, according to PsychCentral, “Borderline Personality Disorder and Self-Isolation: What’s the Link?” Psychiatric rehab uses dialectical behavior therapy (DBT), social skills training, and structured support to help individuals develop healthier interpersonal relationships.
-
Co-Occurring Substance Use Disorders: Many individuals with psychiatric disorders also struggle with addiction, a condition known as dual diagnosis. About 50% of people with a severe mental illness experience a co-occurring substance use disorder, as studied by the National Institute on Drug Abuse. Psychiatric rehab integrates addiction treatment with mental health care, offering counseling, medication-assisted treatment (MAT), and relapse prevention strategies.
-
Psychotic Disorders: Psychotic disorders, including brief psychotic disorder and delusional disorder, involve a loss of contact with reality. These conditions affect approximately 3 in 100 people over their lifetime, according to NIDA. Psychiatric rehab provides therapy, structured routines, and community integration programs to help individuals regain stability and function independently.
What is the History of Psychiatric Rehabilitation?
The history of psychiatric rehabilitation is rooted in the deinstitutionalization movement of the mid-20th century, which sought to transition individuals with mental illnesses from asylums to community-based care. Initially, mental health treatment was custodial, with psychiatric hospitals isolating patients rather than rehabilitating them. In the 1960s and 1970s, policies such as the U.S. Community Mental Health Act (1963) and advancements in psychotropic medications led to a shift toward recovery-oriented care. The psychosocial rehabilitation model emerged, emphasizing skills training, vocational support, and social reintegration. Today, psychiatric rehabilitation is an evidence-based practice incorporated into global mental health systems, with studies showing that structured rehab programs significantly improve social functioning and reduce hospitalizations for individuals with severe mental illnesses.
What Is the Theory Behind Psychiatric Rehabilitation?
The theory behind psychiatric rehabilitation is based on the belief that individuals with mental illnesses achieve meaningful recovery and lead independent lives with the right support. This model integrates principles of psychosocial rehabilitation, emphasizing skill development, social integration, and empowerment. Rooted in person-centered care, it aligns with the "recovery movement," which gained traction in the late 20th century. Research by Abidin MA et al. 2021, titled “Employment programmes for schizophrenia and other severe mental illness in psychosocial rehabilitation: a systematic review,” indicates that psychiatric rehabilitation enhances the quality of life and reduces relapse rates, with studies showing that supported employment programs improve work outcomes for individuals with schizophrenia. The approach is guided by cognitive-behavioral, social learning, and strengths-based theories, reinforcing that mental illness management is not solely about symptom reduction but also about fostering self-sufficiency and resilience.
What are the Principles of Psychiatric Rehabilitation?
The principles of psychiatric rehabilitation include person-centered care, empowerment, hope and respect, and a strengths-based approach. These principles form the foundation of effective mental health recovery, ensuring individuals receive holistic, individualized, and community-integrated support. By emphasizing recovery-oriented, culturally relevant, and evidence-based strategies, psychiatric rehabilitation helps individuals regain independence, improve their quality of life, and reduce relapse rates.
The principles of psychiatric rehabilitation are as follows:
-
Person-Centered Care: Person-centered care focuses on tailoring treatment to individual needs, preferences, and goals rather than applying a one-size-fits-all approach. This principle ensures that people with mental illnesses actively participate in their recovery, leading to improved adherence to treatment and better long-term outcomes.
-
Empowerment: Empowerment in psychiatric rehabilitation means giving individuals control over their own recovery process. By fostering self-efficacy, individuals gain confidence in managing their mental health, which has been linked to increased social engagement and improved quality of life.
-
Hope and Respect: Hope is a necessary element of recovery, as individuals need to believe that improvement is possible. Respect ensures that people with mental illnesses are treated with dignity, reducing stigma and promoting engagement in therapy and social activities.
-
Strengths-Based Approach: This principle focuses on identifying and building upon an individual’s existing strengths rather than solely addressing deficits. By utilizing personal skills, psychiatric rehabilitation enhances self-sufficiency and resilience, leading to better-coping mechanisms.
-
Recovery-Oriented: Recovery-oriented care emphasizes long-term well-being rather than just symptom management. It supports individuals in setting and achieving life goals, such as employment, education, and independent living, which contribute to overall mental health stability.
-
Culturally Relevant: Mental health recovery includes cultural beliefs, values, and traditions. A culturally relevant approach ensures that individuals from diverse backgrounds receive care that respects their identity, leading to better engagement and outcomes.
-
Informed and Shared Decision-Making: In this approach, individuals work collaboratively with mental health professionals to make treatment decisions. Shared decision-making leads to higher treatment satisfaction and improved adherence to therapy.>
-
Integration into the Community: Psychiatric rehabilitation promotes social inclusion by facilitating reintegration into work, education, and community life. Community-based programs help individuals build relationships and reduce isolation, which is necessary for sustained recovery.
-
Comprehensive Approach: A comprehensive approach combines medical, psychological, and social support to address all aspects of an individual’s well-being. This holistic care model improves overall functioning and reduces relapse risks.
How Does Psychiatric Rehabilitation Differ from Drug Rehab?
Psychiatric rehabilitation differs from drug rehab in its primary focus. Psychiatric rehabilitation addresses mental health conditions like schizophrenia, bipolar disorder, and major depression, while drug rehab focuses on treating substance use disorders through detox, therapy, and relapse prevention. However, both programs share similarities, such as structured therapy, life skills training, and community support, as they aim to improve overall well-being and independence.
Psychiatric rehabilitation primarily supports individuals with severe and persistent mental illnesses, emphasizing medication management, psychosocial therapy, and skill development for independent living. It is offered in inpatient psychiatric hospitals, community-based programs, or outpatient mental health clinics. Treatment is long-term and aims to help individuals reintegrate into society while managing their conditions effectively.
In contrast, drug rehab focuses on treating substance use disorders through detoxification, behavioral therapies like cognitive-behavioral therapy (CBT), medication-assisted treatment (MAT), and relapse prevention strategies. Programs range from short-term inpatient treatment to long-term outpatient recovery plans involving support groups like Narcotics Anonymous (NA) or Alcoholics Anonymous (AA).
Both psychiatric rehabilitation and drug rehab emphasize structured therapy, individualized treatment plans, and community reintegration. Dual diagnosis programs exist for individuals struggling with both mental illness and substance use disorders, integrating psychiatric rehabilitation with addiction treatment for comprehensive recovery.
What Is the Process During Psychiatric Rehabilitation?
The process during psychiatric rehabilitation is a structured, multi-step approach designed to help individuals with mental illnesses regain independence, improve daily functioning, and reintegrate into the community. This involves assessment, treatment planning, skill development, and ongoing monitoring to ensure long-term recovery and stability. Each step is personalized to meet the individual's unique needs, emphasizing a combination of medical, psychological, and social support strategies.
The process during psychiatric rehabilitation includes the following steps:
-
Comprehensive Psychiatric Evaluation: A thorough evaluation assesses the individual’s mental health condition, medical history, and psychosocial needs. This includes clinical interviews, diagnostic tests, and observations to determine the severity of symptoms and their impact on daily life.
-
Functional Assessment and Diagnosis: A functional assessment identifies the individual’s cognitive, emotional, and behavioral abilities and any challenges affecting their daily activities. The diagnosis helps in designing a targeted rehabilitation plan to enhance self-sufficiency.
-
Development of an Individualized Rehabilitation Plan (IRP): Based on the evaluation and assessment, a personalized plan is created, outlining specific treatment goals, interventions, and support systems required for recovery. The plan is continuously updated as progress is made.
-
Symptom Stabilization and Medication Management: Medications such as antipsychotics, mood stabilizers, and antidepressants are prescribed to manage symptoms. Regular monitoring ensures effectiveness, reduces side effects, and prevents relapse.
-
Cognitive and Behavioral Skill Training: Cognitive-behavioral strategies are used to help individuals develop coping mechanisms, improve decision-making, and regulate emotions, promoting mental resilience and daily functioning.
-
Psychotherapeutic Interventions (Individual and Group Therapy): Therapeutic sessions, including cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and group therapy, address emotional struggles, enhance self-awareness, and foster social support networks.
-
Occupational and Vocational Rehabilitation: Programs focus on job training, skill-building, and employment assistance, helping individuals gain financial independence and integrate into the workforce while managing their condition.
-
Social and Communication Skills Development: Training in interpersonal communication, conflict resolution, and social interactions enhances confidence and reduces isolation, supporting reintegration into social and family life.
-
Coordination with Primary Care and Support Services: Collaboration with healthcare providers, social workers, and community support programs ensures holistic care, addressing both mental and physical health needs.
-
Continuous Clinical Monitoring and Treatment Adjustment: Regular assessments and follow-ups allow healthcare providers to track progress, modify treatment plans, and ensure long-term stability, preventing relapses and hospitalizations.
Is Psychiatric Rehabilitation the Same as an Inpatient Mental Health Program?
No, psychiatric rehabilitation is not the same as an inpatient mental health program because they serve different purposes and have distinct treatment approaches. Psychiatric rehabilitation focuses on long-term recovery, skill development, and reintegration into the community, provided in outpatient or residential settings. In contrast, inpatient mental health programs are short-term, intensive treatments designed to stabilize individuals experiencing severe psychiatric crises, involving hospitalization with round-the-clock medical supervision. While both aim to improve mental health, psychiatric rehabilitation emphasizes long-term functional recovery, whereas inpatient programs focus on immediate crisis management.
What Treatment Approaches Are Used During Psychiatric Rehabilitation?
Treatment approaches used during psychiatric rehabilitation are Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and medication management. These approaches are diverse and tailored to support individuals with severe psychiatric disorders by addressing symptoms, improving daily functioning, and promoting long-term recovery. These methods incorporate evidence-based therapies, medication strategies, and skill-building programs to enhance independence and quality of life. By focusing on cognitive, behavioral, social, and vocational aspects, psychiatric rehabilitation helps individuals reintegrate into society and lead fulfilling lives.

Treatment approaches used during psychiatric rehabilitation are as follows:
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a structured, evidence-based approach that helps individuals identify and change negative thought patterns and behaviors contributing to their psychiatric symptoms. It is widely used for disorders such as schizophrenia, major depression, and anxiety disorders. CBT enhances coping mechanisms, improves emotional regulation, and reduces distressing symptoms, helping individuals regain control over their thoughts and actions. According to Verywell Mind, approximately 60% of people who are treated with cognitive behavioral therapy (CBT) for a substance use problem are able to maintain their recovery for a year.
Dialectical Behavior Therapy (DBT)
Dialectical Behavior Therapy (DBT) is particularly effective for individuals with borderline personality disorder and co-occurring conditions. It focuses on building emotional regulation, distress tolerance, mindfulness, and interpersonal effectiveness. DBT is helpful in psychiatric rehabilitation as it teaches individuals how to manage extreme emotions, reduce self-harm behaviors, and improve social interactions, fostering long-term stability. According to a study by Dimeff LA, Linehan MM. et al. 2008, titled “Dialectical behavior therapy for substance abusers,” individuals who received Dialectical Behavior Therapy had significantly higher treatment retention (64% vs. 27%), showed greater reductions in drug use based on interviews and urinalyses, and attended more individual therapy sessions compared to those receiving standard treatment.
Medication Management
Medication management ensures that individuals receive the appropriate psychiatric medications, such as antipsychotics, mood stabilizers, or antidepressants, in the correct dosages. Regular monitoring by psychiatrists or psychiatric nurses helps adjust medications to optimize effectiveness while minimizing side effects. This approach is crucial for stabilizing symptoms of conditions like schizophrenia, bipolar disorder, and severe depression. According to SAMHSA, 68% of people who complete drug and alcohol detox programs report their treatment to be successful.
Psychoeducation
Psychoeducation provides individuals and their families with knowledge about mental illness, treatment options, and coping strategies. By understanding their conditions, patients make informed decisions about their care and actively participate in their rehabilitation process. Psychoeducation reduces stigma, enhances adherence to treatment, and empowers individuals to manage their symptoms effectively.
Cognitive Remediation Therapy
Cognitive remediation therapy is designed to improve cognitive deficits such as memory, attention, and problem-solving skills in individuals with psychiatric disorders like schizophrenia. By engaging in structured exercises and computerized tasks, patients develop stronger cognitive abilities, which help them function better in daily life, work, and social interactions.
Social Skills Training
Social skills training helps individuals develop effective communication, relationship-building, and problem-solving skills necessary for daily interactions. This approach is especially beneficial for those with schizophrenia, autism spectrum disorders, or severe anxiety, as it enhances their ability to form and maintain relationships, navigate social situations, and improve their overall quality of life.
Vocational Rehabilitation
Vocational rehabilitation provides individuals with training, job placement, and employment support tailored to their abilities and interests. People with psychiatric disorders face challenges in securing and maintaining employment, and this approach helps them develop work-related skills, build confidence, and achieve financial independence, contributing to their overall recovery.
Occupational Therapy
Occupational therapy focuses on helping individuals regain fundamental life skills and daily functioning. Through structured activities, patients learn how to manage tasks like cooking, cleaning, and financial management. This therapy is particularly beneficial for those recovering from severe mental illness, as it promotes independence and self-sufficiency.
Case Management
Case management ensures coordinated care by connecting individuals with mental health services, housing assistance, medical care, and community resources. Case managers advocate for their clients, monitor progress, and provide continuous support, ensuring that patients receive comprehensive care that meets their specific needs.
Group Therapy
Group therapy provides a supportive environment where individuals with similar psychiatric conditions share experiences, learn coping strategies, and build social connections. This approach is particularly useful for people with depression, PTSD, and substance use disorders, as it fosters peer support and reduces feelings of isolation. A Lancet journal estimates that only 5% to 8% of people who attend AA successfully maintain abstinence.
Family Therapy
Family therapy involves the participation of family members in the rehabilitation process to improve communication, address conflicts, and educate loved ones about mental illness. This approach helps create a supportive home environment, which is important for long-term recovery and relapse prevention, according to Hogue A. et al. 2021, titled “Family involvement in treatment and recovery for substance use disorders among transition-age youth: Research bedrocks and opportunities.”
Motivational Interviewing
Motivational interviewing is a counseling technique designed to enhance an individual's motivation to change harmful behaviors, such as substance abuse or medication non-adherence. By using a non-confrontational approach, therapists help patients explore their goals, resolve ambivalence, and commit to healthier choices.
Supported Employment and Housing Services
Supported employment and housing services assist individuals in securing stable jobs and safe living environments, both of which are necessary for psychiatric rehabilitation. Stable housing reduces stress and provides a foundation for recovery, while supported employment programs offer guidance and accommodations to help individuals succeed in the workforce.
How to Find a Psychiatric Rehab Near Me?
To find a psychiatric rehab near you, use online directories and rehab locators that list accredited facilities based on location and treatment needs. To find a psychiatric rehab near you, trust Better Addiction Care to help guide you to the right treatment. We provide a free rehab locator tool that connects you with facilities in our database across the country. Whether you're looking for rehabs in California, Illinois, Texas, New York, Florida, Massachusetts, Oklahoma, Georgia, or Pennsylvania, explore inpatient, outpatient, and dual diagnosis programs tailored to your mental health and addiction needs. Let us help you verify insurance coverage, compare program options, and find the care that works best for you.
How Long Does Psychiatric Rehabilitation Last?
Psychiatric rehabilitation lasts for varying durations depending on the severity of the condition, treatment goals, and individual progress. Programs range from a few months to several years, with some individuals requiring lifelong support. A study published in Psychiatric Services found that long-term rehabilitation programs significantly improve outcomes for those with severe mental illnesses, reducing hospital readmissions and improving independent living skills. The duration is personalized, with continuous assessments guiding the length of care.
How Do You Qualify for Psychiatric Rehabilitation?
You qualify for psychiatric rehabilitation if you have a diagnosed mental health condition that affects your daily functioning and requires structured support for recovery. Eligibility depends on factors such as the severity of symptoms, history of hospitalizations, and inability to maintain employment or independent living. Many programs require a referral from a psychiatrist or healthcare provider. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), psychiatric rehabilitation services are provided to individuals with schizophrenia, bipolar disorder, and severe depression to help them reintegrate into society.
Is Psychiatric Rehabilitation Covered by Insurance?
Yes, psychiatric rehabilitation is covered by insurance, but coverage varies by provider, policy, and location. Under the Mental Health Parity and Addiction Equity Act (MHPAEA) in the U.S., insurance plans must provide mental health services at the same level as physical health care. Many private insurance plans, Medicaid and Medicare cover psychiatric rehabilitation services, including therapy, medication management, and social skills training. However, some programs require pre-authorization or out-of-pocket expenses, making it necessary to verify benefits with the insurance provider.
Can Psychiatric Rehabilitation Help with Employment or Housing?
Yes, psychiatric rehabilitation can help with employment and housing by providing job training, supported employment programs, and assistance with independent living skills. Many rehab programs collaborate with vocational services to help individuals find and maintain jobs suited to their abilities. The National Alliance on Mental Illness (NAMI) states that supported employment programs improve job retention rates for individuals with severe mental illnesses. Similarly, housing assistance programs, such as transitional housing or permanent supportive housing, are integrated into psychiatric rehabilitation to promote stability.
What is the Role of Family in Psychiatric Rehabilitation?
The role of family in psychiatric rehabilitation is important, as family members provide emotional support, encourage treatment adherence, and help create a stable home environment. Studies by Thomas PA, Liu H, Umberson D., et al. 2017, titled “Family Relationships and Well-Being,” show that individuals with strong family support experience better outcomes, including reduced hospitalizations and improved symptom management. Family psychoeducation programs help relatives understand mental health conditions, teaching coping strategies to improve communication and problem-solving. According to SAMHSA, involving family members in psychiatric rehabilitation enhances recovery and promotes long-term well-being.
What is the Success Rate of Psychiatric Rehabilitation?
The success rate of psychiatric rehabilitation varies between 60% and 80% based on individual conditions, treatment engagement, and support systems. Research published in the Psychiatric Rehabilitation Journal suggests that structured rehab programs lead to significant improvements in social functioning, employment, and independent living, as studied by Volkow, N. D., & Blanco, C. et al. 2023, titled “Substance use disorders: a comprehensive update of classification, epidemiology, neurobiology, clinical aspects, treatment and prevention.” Success is measured by reduced hospital readmissions, increased employment rates, and improved quality of life. While not a cure, psychiatric rehabilitation provides individuals with tools to manage symptoms and achieve long-term stability.
Related Articles
Treatment Centers in Texas








