6 Stages of Addiction
The six stages of addiction describe how substance use develops into a compulsive and chronic disorder. Each stage reflects increasing involvement with drugs and behavioral changes that contribute to long-term addiction. Understanding these stages helps in recognizing early signs and seeking treatment before addiction becomes severe.

The six stages of addiction describe how substance use develops into a compulsive and chronic disorder. Each stage reflects increasing involvement with drugs and behavioral changes that contribute to long-term addiction. Understanding these stages helps in recognizing early signs and seeking treatment before addiction becomes severe.
Experimentation is the first stage of addiction, where a person tries a substance out of curiosity, peer pressure, or to escape stress. At this stage, drug use is voluntary, and there are no significant consequences. Individuals who begin drinking alcohol before the age of 15 are more likely to develop alcohol dependence compared to those who start at 21 or older. According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), early initiation of alcohol use is associated with an increased likelihood of developing alcohol use disorders later in life.
Regular use/behavior occurs when a person begins using a substance consistently, such as on weekends or in specific social settings. Although they still have control over their usage, patterns of reliance start forming. Psychological dependence begins to develop, and the risk of progressing to more dangerous use increases.
Risky use/behavior is the stage where substance use leads to negative consequences, such as health problems, impaired judgment, or trouble at work and in relationships. Despite experiencing harm, the person continues using the substance, showing early signs of losing control. As noted by Liu and Li (2018) in "Drug Addiction: A Curable Mental Disorder," addiction disrupts multiple brain systems, including those responsible for stress regulation and decision-making.
Dependence is when the brain and body adapt to the drug, requiring higher doses to achieve the same effects. Withdrawal symptoms emerge when the person stops using, reinforcing continued use to avoid discomfort. This stage signals a deeper level of involvement, where quitting without medical help becomes increasingly difficult.
Addiction is the stage where substance use becomes compulsive, and the person loses control despite harmful consequences. The brain’s reward system is altered, making drug use feel necessary for survival. Addiction is classified as a chronic mental disorder that requires treatment, including behavioral therapy, medication, or other interventions. Addiction affects both substance users and those with behavioral addictions, demonstrating its complexity across different domains.
Relapse occurs when a person returns to substance use after attempting to quit. It is a common part of addiction, triggered by stress, environmental cues, or exposure to the substance. Relapse does not mean treatment has failed, but it highlights the need for long-term support and relapse prevention strategies. Addiction involves complex neural mechanisms, making sustained recovery a challenge that requires ongoing management.
Stage #1: Experimentation
Experimentation is the initial stage of addiction, characterized by occasional, socially driven use, such as at parties. Individuals in this stage are driven by curiosity or peer pressure, with no immediate negative consequences. Adolescents are particularly vulnerable due to ongoing brain development. The physical effects include an initial dopamine release that reinforces pleasurable associations. Emotionally, individuals experience euphoria or stress relief. Socially, there is positive reinforcement from peers. Financially, the impact is minimal at this stage. Early exposure increases susceptibility to progressing to regular use. According to the National Academies of Sciences, Engineering, and Medicine (2016) in "The Neurobiology of Substance Use, Misuse, and Addiction," adolescence is an important risk period for initiation, with addictive substances causing disproportionate harm to developing brains.
Stage #2: Regular Use/Behavior
Regular use involves integrating substance use into daily or weekly routines. Individuals begin planning activities around substance use, develop increased tolerance, and start consuming substances alone. Physically, there is reduced natural dopamine production. Emotionally, there is a reliance on substances to manage stress. Socially, individuals shift their social circles to include other users. Financially, there are early expenditures on substances. Tolerance develops, requiring larger doses for the same effect. According to the 2021 National Survey on Drug Use and Health (NSDUH), approximately 61.6 million people aged 12 or older reported binge drinking in the past month, indicating regular alcohol use.
Stage #3: Risky Use/Behavior
Risky use is marked by persistent substance use despite negative consequences. Individuals engage in impaired decision-making, such as driving under the influence, experiencing strained relationships, and neglecting responsibilities. The Centers for Disease Control and Prevention (CDC) reports that in 2023, 28.3% of all traffic-related deaths in the United States were due to alcohol-impaired driving, highlighting the dangers associated with risky use. Physically, there is an increased risk of accidents or injury. Emotionally, individuals face mood swings, irritability, and anxiety. Socially, conflicts with loved ones arise. Financially, there is job instability or legal fines. Prefrontal cortex dysfunction reduces risk assessment capacity. Verdejo-Garcia et al. (2017) in "Stages of Dysfunctional Decision-Making in Addiction" found that risky use correlates with prefrontal cortex impairment, prioritizing immediate rewards over long-term consequences.
Stage #4: Dependence
Dependence involves daily substance use to avoid withdrawal symptoms. Individuals develop physical and psychological reliance, experience withdrawal symptoms such as nausea and anxiety, and have failed attempts to quit. Physically, withdrawal symptoms emerge upon cessation. Emotionally, there are severe cravings and emotional instability. Socially, individuals experience isolation and neglect in relationships. Financially, there are increased costs to sustain addiction. Brain stress systems become hyperactive, perpetuating use. The National Institute on Drug Abuse (NIDA) reports that 75% of individuals with substance use disorders experience moderate-to-severe withdrawal.
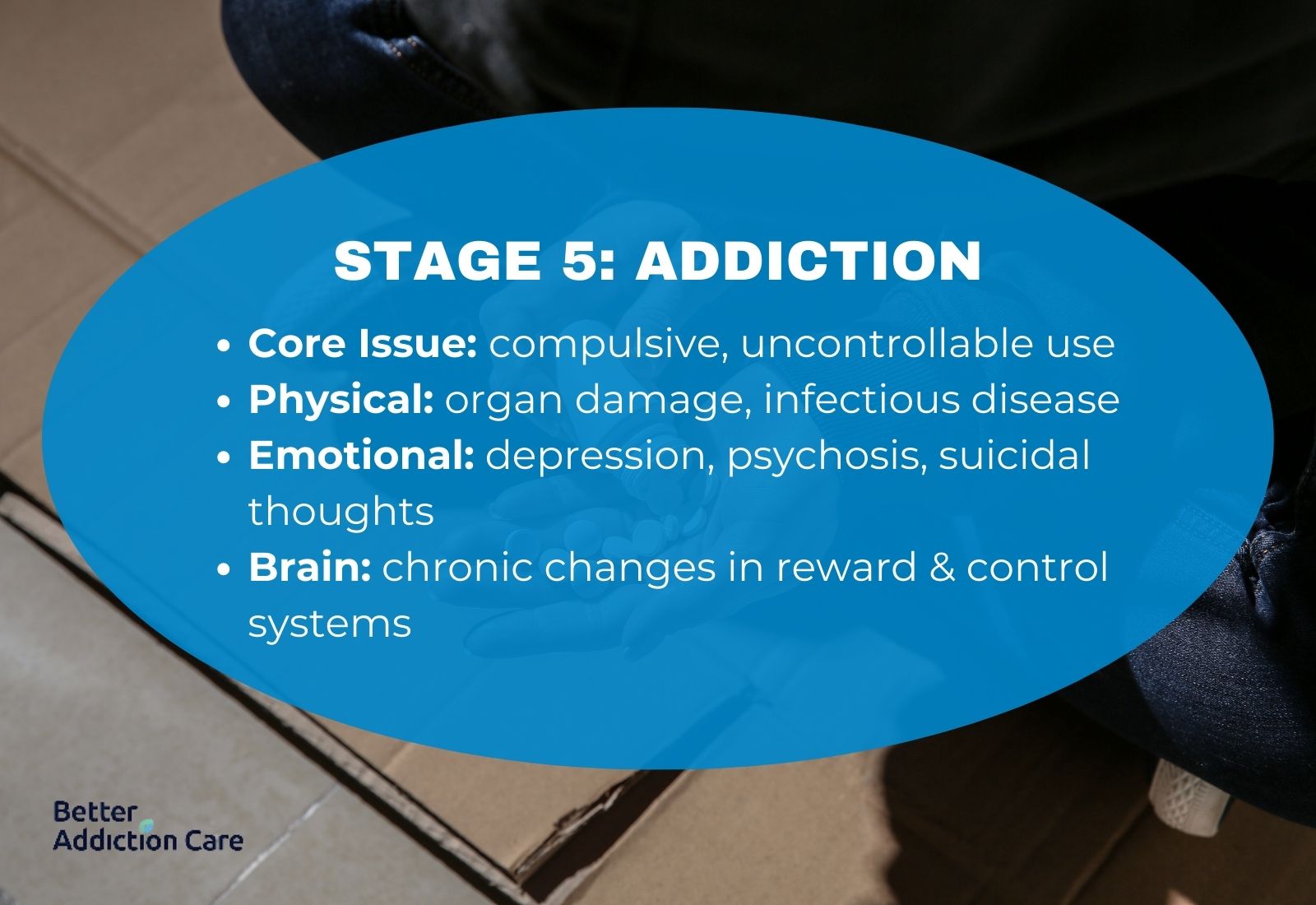
Stage #5: Addiction
Addiction is characterized by compulsive, uncontrollable substance use. Individuals prioritize substances over health, work, or family. Physically, there is organ damage or infectious diseases. Emotionally, individuals suffer from depression, psychosis, or suicidal ideation. Socially, there are broken relationships or child neglect. Financially, individuals face bankruptcy or homelessness. Chronic brain changes occur in reward, stress, and executive function systems. In the United States, approximately 14.5% of individuals aged 12 or older had a substance use disorder (SUD) in the past year, according to the 2020 National Survey on Drug Use and Health, thus showing how serious this stage is and how important it is that we understand how to treat it.
Stage #6: Relapse
Relapse refers to the resumption of substance use after attempting to quit. Individuals return to substance use due to triggers such as stress or environmental cues. Physically, there is an increased risk of overdose due to reduced tolerance. Emotionally, individuals feel shame or hopelessness. Socially, there is stigmatization. Financially, recurring treatment costs arise. Relapse rates for substance use disorders are 40–60%, comparable to other chronic diseases. The National Institute on Drug Abuse (NIDA) in "Drugs, Brains, and Behavior: The Science of Addiction" highlights that brain changes persist post-recovery, increasing relapse susceptibility.

How Long Does It Take to Progress Through the Six Stages of Addiction?
It takes weeks or years to progress through the six stages of addiction, depending on the substance, frequency of use, and individual vulnerability. Someone using heroin daily develops dependence in weeks, while a person drinking alcohol socially takes years before withdrawal symptoms appear. The method of use also affects the timeline, as injecting a drug delivers faster effects than swallowing a pill. Genetic factors influence addiction risk, with 40–60% of a person’s susceptibility linked to inherited traits. According to the National Institute on Drug Abuse (NIDA) in "Drugs, Brains, and Behavior: The Science of Addiction," about 10% of people who try addictive substances develop a substance use disorder, though not everyone linearly progresses through all six stages.
Are the Six Stages of Addiction the Same for All Substances?
The six stages of addiction apply to all substances and behaviors, but the speed and severity of progression depend on the drug or addictive activity. Someone using heroin or methamphetamine reaches dependence quickly due to their intense effects on the brain, while a person engaging in behavioral addictions like gambling or internet use takes longer to experience compulsive patterns. Nicotine and alcohol addiction develop gradually but are difficult to overcome due to social acceptance and withdrawal symptoms. According to the National Academies of Sciences, Engineering, and Medicine (2016) in "The Neurobiology of Substance Use, Misuse, and Addiction," different substances affect the brain in distinct ways, making some addictions harder to treat than others.
How Does Early Intervention Affect the Stages of Addiction?
Early intervention affects the stages of addiction by preventing substance use from escalating into dependence and severe addiction. Catching early signs, such as behavioral changes or neglecting responsibilities, allows for timely action. According to Volkow (2022) in “Time To Start Talking About Pre-Addiction” (NIDA), addressing substance use in early stages increases recovery success, while waiting for “rock bottom” worsens outcomes.
Programs like SBIRT identify substance misuse early, reducing the progression to addiction. The Surgeon General’s Report on Alcohol, Drugs, and Health (2016) found that brief interventions in healthcare settings significantly lower substance use. Early support in adolescents reduces long-term drug dependence risk by 40-60%, according to NIDA (2016) in “Preventing Drug Use Among Children and Adolescents”.
What Is Addiction?
Addiction is a chronic disorder characterized by compulsive substance use despite harmful consequences. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), classifies addiction under "Substance-Related and Addictive Disorders," encompassing both substance use disorders and behavioral addictions such as gambling disorder. In the United States, approximately 20.4 million people aged 12 or older had a substance use disorder in 2019, according to the National Survey on Drug Use and Health.
What Does It Mean to Have an Addictive Personality?
Having an addictive personality means a set of traits that increase an individual's susceptibility to developing addictions. These traits include impulsivity, sensation-seeking, and difficulty delaying gratification. While the concept is debated, individuals with these characteristics are more prone to substance use disorders.
What Is the Difference Between Psychological Dependence and Physical Dependence?
The difference between psychological dependence and physical dependence is that psychological dependence involves emotional and mental preoccupation with a substance, leading to cravings and compulsive use. Physical dependence refers to the body's adaptation to a substance, resulting in tolerance and withdrawal symptoms upon cessation. Both forms of dependence occur simultaneously but are distinct aspects of addiction.
What Are the Causes of Addiction?
The causes of addiction are genetics, social environments, demographics, peer pressure, chronic pain, and mental health conditions. Genetic factors influence how the brain processes substances, with 40–60% of addiction risk linked to inherited traits. Social factors, such as poverty and exposure to trauma, contribute to substance use initiation. Demographics, including age and gender, affect susceptibility, with adolescents being at higher risk due to brain development. Peer pressure increases experimentation, particularly among young people. Chronic pain leads to prescription drug misuse, while mental health conditions like depression and anxiety drive self-medication. According to the National Institute on Drug Abuse (2020) in “Drugs, Brains, and Behavior: The Science of Addiction,” early substance use and environmental stressors significantly raise addiction risk.
How Is Addiction Diagnosed?
Addiction is diagnosed using the DSM-5 criteria for Substance Use Disorders (SUD). The DSM-5 outlines 11 symptoms, including tolerance, withdrawal, cravings, continued use despite harm, and neglect of responsibilities. A person meeting 2–3 criteria is diagnosed with mild SUD, 4–5 indicates moderate SUD, and 6 or more signals severe addiction. Diagnosis requires a clinical assessment over 12 months to evaluate compulsive behavior and its impact on daily life. According to the National Institute on Drug Abuse (NIDA), approximately 20 million Americans have met the DSM-5 criteria for SUD in recent years.
What Are the Treatments for Addiction?
The primary treatments for addiction are detox, medication-assisted treatment (MAT), behavioral therapies, and support groups. Addiction treatment approaches vary depending on the substance used and the severity of addiction, with a combination of medical and psychological interventions offering the best outcomes.
The treatments for addiction are given below:
-
Detox: This process helps individuals safely withdraw from substances under medical supervision. It reduces withdrawal symptoms and prevents dangerous complications, making it the first step in treatment. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), approximately 68% of individuals who complete drug and alcohol detox programs report their treatment as successful.
-
Medication-Assisted Treatment (MAT): This approach combines medications like methadone or buprenorphine with therapy to reduce cravings and prevent relapse. Patients on methadone had 33% fewer opioid-positive drug tests and were 4.44 times more likely to stay in treatment than those without medication, as noted by the National Institute on Drug Abuse (2018) in "How effective are medications to treat opioid use disorder?"
-
Behavioral Therapies: These include cognitive-behavioral therapy (CBT), contingency management, and motivational interviewing to change harmful thought patterns and behaviors. A meta-analysis titled titled "Cognitive-Behavioral Treatment with Adult Alcohol and Illicit Drug Users: A Meta-Analysis of Randomized Controlled Trials," by Magill and Ray in 2009, published in the Journal of Studies on Alcohol and Drugs found that CBT had a moderate effect size for substance use disorders, with 60% of patients maintaining abstinence at a 52-week follow-up.
-
Support Groups: Programs such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) provide peer support, accountability, and long-term relapse prevention strategies. Many individuals benefit from ongoing participation in these groups alongside formal treatment.
How Does Treatment Differ Depending on the Stage of Addiction?
Treatment differs depending on the stage of addiction, with more intensive programs required as severity increases. Early stages, such as experimentation and regular use, benefit from outpatient counseling and educational programs to address substance use before dependence forms. Moderate addiction, marked by risky use and withdrawal symptoms, requires intensive outpatient programs (IOP) or partial hospitalization programs (PHP) that provide structured therapy while allowing patients to maintain daily responsibilities. Severe addiction, involving compulsive use and relapse, requires inpatient rehabilitation or residential treatment, where individuals receive 24-hour medical and psychological care. According to the National Institute on Drug Abuse (NIDA) in "The Science of Addiction," long-term treatment increases recovery success, with structured programs reducing relapse rates.
How to Prevent Addiction?
To prevent addiction requires early intervention, education, and lifestyle changes that reduce substance use risk. Avoiding environments where substance use is common helps limit exposure, especially for adolescents and young adults. Building strong social connections and engaging in healthy activities, such as exercise and hobbies, reduces the likelihood of seeking substances for stress relief. Access to mental health care and coping strategies for anxiety and depression lowers the risk of self-medicating with drugs or alcohol. According to the National Institute on Drug Abuse (NIDA), early prevention programs in schools and communities significantly decrease the likelihood of substance use disorders later in life.
What Are Gateway Drugs?
Gateway drugs are substances like alcohol, nicotine, and cannabis that increase the likelihood of using more addictive substances. Adolescents who smoke cigarettes are more likely to experiment with drugs like cocaine or heroin later in life. Cannabis use has been linked to a higher risk of opioid misuse due to its effects on brain chemistry and decision-making. According to the National Institute on Drug Abuse (NIDA) in the study "Monitoring the Future," individuals who use cannabis are 44.7% more likely to try other illicit substances, highlighting its role as a gateway drug.
What Is the Difference Between the Stages of Addiction and the Addiction Cycle?
The difference between the stages of addiction and the addiction cycle is that the stages show how addiction develops over time, while the cycle explains the repeated pattern that fuels substance use. The stages of addiction progress from experimentation to regular use, risky use, dependence, and eventually, compulsive addiction. The addiction cycle follows a repetitive loop, beginning with emotional triggers such as stress or trauma that create a need for relief. This leads to craving, where the brain associates substances with a temporary escape. The ritual phase involves behaviors or routines that prepare for use, followed by substance use, which provides short-term relief. The cycle ends in guilt, where feelings of regret and shame reinforce emotional distress, restarting the pattern. According to the National Institute on Drug Abuse (NIDA) in the study "The Science of Addiction," breaking this cycle requires interventions that address both psychological triggers and physical dependence.





